1037DOH - Oral Cariology
1/174
Earn XP
Description and Tags
cariology for dental hygiene (week 4 onwards)
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
175 Terms
what is the definition of dental caries?
localised, progressively destructive tooth disease that starts at the external surface (usually enamel) with apparent dissolution of the inorganic components by organic acids that are produced by the enzymatic action of masses of microorganisms (in bacterial plaque) on carbohydrates
key components of the definition of dental caries
bacteria required to produce disease
bacteria use metabolise-refined carbs
when metabolism anaerobic, acids are produced
acids dissolve inorganic phase of teeth
dental caries aren’t just holes in teeth. the process of bacteria fermenting foods to produce _____ and dissolving tooth mineral
acids
what are some of the acids produced by bacteria?
lactic
acetic
formic
propionic acids
dental caries is a ________ _________ disease
transmissible bacterial disease
describe the transmission of bacteria causing dental caries from mother to child
bacteria transferred to babies from mothers or caregivers in very early life
colonisation of soft tissues possible before tooth eruption
teeth erupt, cariogenic bacteria colonise surface, establish dental plaque
cycle of destruction begins if plaque accumulates
4 factors according to the Jordan diagram to have dental caries
(BSST)
biofilm/plaque presence
susceptible tooth surface
sugars (food for bacteria)
time (to allow acid to demineralise the tooth)
these factors without any protective factors or with multiple risk factors will result in dental caries
list some of the primary modifying factors (main influence)
tooth anatomy
saliva
biofilm pH and composition
fluoride use
diet
oral hygiene
immune system
genetic factors
meds
list some secondary modifying factors (these modify the primary modifying factors)
socioeconomic status
education
lifestyle
environment
age
ethnic group
occupation
acidogenic vs aciduric bacteria
genic) produce acid
uric) live in an acidic environment
the normal protection for caries on the tooth surface is regular _____ ________ ______
mechanical biofilm removal (toothbrushing and interdental cleaning)
factors on the tooth surface that influence caries position (yk like where the caries are more present on the tooth surface)
pits/fissures
below contact points
cervical area of tooth
developmental defects (grooves etc, encourages plaque accumulation and makes it harder to clean
poor restorations (if ledges/edges, encourages plaque accumulation, inc. risk of caries developing between margin of restoration and tooth)
iatrogenic damage (areas the dentist damaged lol)
areas of hypomineralisation (less mineralisation, so more susceptible to damage)
mineral content ____ in different areas of teeth. substitution of ______ in tooth structure for ______ increases susceptibility of an acid attack (solubility)
varies
carbonate
phosphate
fluoride applied during which two moments reduces solubility (susceptibility to acid attacks)?
systemically before eruption
topically after eruption
how does biofilm start and how does it evolve?
highly organised sequence of events
starts as initial pellicle of enzymes, glycoproteins and immunoglobulins
turns into complex colonies of many bacteria (strep and actinomyces species)
aciduric bacteria tend to arise later because the environment they need to live in arises later too
higher maternal salivary levels of bacteria leads to higher WHAT in the child
salivary levels of bacteria
4 steps of plaque formation on tooth surface
acquired pellicle formation
initial adhesion of bacteria on pellicle surface
co-aggregation (more bacteria of different types, extracellular polysaccharides come that form the visible portion of plaque)
maturation and diffusion (gets thicker, saliva prevented to getting to tooth surface and areas where bulk of acid is produced)
diet and dental caries - you need a _______ substrate within the diet. what other factors do you need to consider? in the absence of the above substrate, what happens?
need a fermentable substrate
factors:
amount
frequency
how consumed (held in the mouth for how long, when consumed (with or after meal?)
formulation (boiled sweet vs fluid vs sticky)
temperature (enzymatic reaction to produce acid (metabolic process) so its rate is temp dependent, colder = slower, therefore less cariogenic than something hot)
in the absence of a fermentable carbohydrate, caries don’t develop
elaborate on the primary modifying factors:
tooth anatomy
saliva
biofilm pH
biofilm composition
tooth anatomy
sites that are more difficult to clean
saliva
flow rate, buffering capacity
natural defence against caries
biofilm pH
directly related to thickness and amount/frequency of sugar consumed
composition
depends on bacterial flora
how long undisturbed
and presence of sugars
all these influence the development of extracellular polysaccharides (what you see clinically)
elaborate on the primary modifying factors of:
fluoride use
oral hygiene
fluoride use
decreases solubility of dental hard tissue when incorporated into enamel
antibacterial effect
oral hygiene
acid production requires anaerobic metabolism
needs good thickness of plaque (anaerobic respiration so it can do this)
regular removal necessary
elaborate on the primary modifying factors of:
immune system (affects…)
genetic factors (affects…)
meds/radiotherapy
immune system
affects the number and type of microorganisms in the mouth
genetic factors
can affect the structure of teeth and salivary function
meds/radiotherapy
many medications (incl. side effects) reduce salivary flow
previous radiotherapy around head and neck can damage salivary glands
xerostomia can be part of medical syndromes
elaborate on the secondary modifying factors of:
socioeconomic status
age
socioeconomic status
increasing evidence caries are more prevalent in more socio-economically deprived families
diet (greater reliance on processed foods)
oral hygiene (irregular dentist visits, or not having a toothbrush)
self-motivation (unemployed, feeling devalued etc)
age
teeth more susceptible to caries shortly after eruption (before absorbing fluoride)
old age - medication that could cause xerostomia etc, intercurrent disease
initial mineral loss affects the ________ tissue
subsurface
describe the state of the outer and inner surfaces of a tooth during an early carious lesion
outer surface is intact
layer below the surface is demineralised
thus possible to reverse this in this stage
list the caries classification by site
class 1
pits/fissures of occlusal 1/3 of molars/premolars
occlusal 2/3 of molars/premolars
linguals of anterior teeth
class 2
proximal surface of molars and premolars
just below contact point
class 3
proximal surfaces of central/lateral incisors
canines (not incisal angles)
just below contact point
class 4
proximal including incisal angles of anterior teeth
class 5
gingival 1/3 of facial/lingual surfaces of all teeth
below max convexity and just above ging. margin
class 6
cusp tip of molars/premolars + canines
naturally cleansed areas so caries here is super bad
what is common about classes 1-5 of the caries classification sites? what about class 6?
1-5) all these areas are where plaque stagnation occurs as they’re not self-cleansing
6) normally self-cleansing so caries here indicates high caries risk (eg cusp tip caries)
what are:
primary caries?
recurrent (secondary) caries?
residual caries?
primary caries
new lesion on unrestored surfaces
secondary (recurrent) caries
adjacent to a restoration (margin)
residual caries
caries left under a restoration (intentionally or unintentionally)
dentist has left some caries while treating it
cannot be seen clinically and usually seen in a radiograph
what is pathogenesis?
biological mechanism that leads to a diseased state
can also be used to describe origin + development of disease
whether acute (quick onset), chronic (slow onset) or recurrent
what is the extended ecological plaque theory (EEPT)?
composition of the plaque is important
plaque adapts
as it matures, the species that inhabit the plaque change
if pH is habitually acidic, plaque favours aciduric and acidogenic bacteria
find it easier to inhabit the plaque
the tooth surface is unique as its not protected by ____-______ _______
self-shedding mechanisms
things like new skin, nails, hair, etc
describe the tooth habitats for cariogenic biofilm (plaque)
pellicle ideal surface for bacterial colonisation
undisturbed plaque rapidly builds - produce an anaerobic environment
important to break chain early - frequent tooth cleaning (early plaque might not contribute much to caries but mature plaque much more likely to)
note about plaque
(it isnt necessarily…. but its an accumulation of…)
it isnt necessarily food debris - could be found in patients who don’t clean often
plaque is accumulation of extracellular polysaccharides that are produced by bacteria (product of metabolising sugars)
list 4 key components of the dental caries definition
bacteria required to produce disease
bacteria metabolise sugars
when metabolism is anaerobic, acids are produced
acids dissolve inorganic phase of the teeth (enamel)
list the first 3 steps of demineralisation
bacteria metabolise fermentable carbohydrates (organic acids which diffuse into the tooth structure through water between crystals)
acid reaches susceptible site on crystal surface, calcium and phosphate dissolve into aqueous phase between crystals
occurs at atomic level long before it’s visible with magnification
____________ is a natural repair process for subsurface non-cavitated carious lesions
remineralisation
explain remineralisation
calcium and phosphate ions diffuse into tooth structure
attaches to and rebuilds crystal remnants (doesn’t build new ones)
recreate not repair
primarily saliva-sourced and some from topical sources
fluoride aids remineralisation process
absorbed into tooth structure
fluorapatite
need the surface layer to be intact for this to work!
once absorbed into the crystal surface, fluoride attracts _______ and ______ ions attracted to calcium
calcium
phosphate
fluoride is a negatively charged ion and calcium is a positively charged ion, then the calcium attracts phosphate
role of saliva in caries
acts as a buffer
neutralise extreme pH fluctuation
calcium and phosphate in saliva inhibit dissolution (promote remineralisation)
has antibacterial components (enzymes etc)
effect depends on flow rate, buffering capacity (how much, how good at neutralising acids, how long tooth bathed in it) fluoride availability and time
why is saliva nature’s anticaries agent?
bacterial clearance
when you swallow you swallow the flora too which die in the stomach
direct antibacterial activity
assorted enzymes produced
buffers
remineralisation
how much saliva do adults produce?
around 1-1.5 litres per day
when is salivary flushing most effective?
during mastication/stimulation of flow
(as theres a greater amount of saliva produced)
is saliva part of the immune system? why or why not?
not part of the immune system
saliva holds no memory (no specific response to certain agents)
non specific so washes away bacteria equally
describe what salivary enzyme amylase does (action and effect)
breaks down sucrose, depriving bacteria of its energy source
describe the action and effect of lactoperoxidase
action) catalyses H2O2 mediated oxidation
effect) bactericidal. suppresses biofilm formation
describe the action and effect of lysozymes
action) lyses cells by attacking cell walls
effect) bactericidal. suppresses biofilm formation
describe the action and effect of lipases
action) breaks down triglycerides
effect) free fatty acids inhibit attachment and growth of some bacteria
describe the action and effect of lactoferrin
action) binds free iron
effect) inhibits growth of some iron-dependent microbes
describe the action and effect of secretory immunoglobulin (predominantly IgA)
action) agglutination of bacteria inhibits bacterial enzymes
effect) reduced numbers in saliva and inhibits growth
describe the action and effect of glycoproteins (mucins)
action) agglutination of bacteria
effect) reduces numbers in saliva by precipitation
_______ capacity has a major impact on caries (along with flow rate). why?
buffering
reduces the potential for acid production
encourages return to neutral pH when sugar intake stops
generally speaking, where do caries commonly appear on teeth?
in sites that are difficult to clean
unless there is a significant risk factor to produce dental caries, how long (generally) does it take to form caries?
months or years
what do remineralised enamel lesions look like?
intact
smooth white
black or brown (trapped organic material)
contour is still same but structure not fulllly restored ykwim
describe the progression of an enamel lesion
surface breakdown
surface becomes rough and plaque retentive
easily damaged by probing, soft/easily disturbed
further progess leads to cavitation
colour can vary but usually light
describe the histological appearance of an enamel lesion
widest near surface
tapers toward dentino-enamel junction
caries can reach dentin without cavitation
describe progression of an enamel lesion (caries) in pits and fissures
often appears as if there are 2 lesions on opposing surfaces
same triangular shape
deepest in the middle
the cavitated lesions become ______ _______ which means it is an ideal environment for ________ and favours ________ progression.
plaque retentive
biofilm
caries
describe a lesion at the dentino-enamel junction
may precede cavitation
defence reactions in pulp
reparative dentin (dentin tries to wall itself from the bacteria invasion - cant renew surface but dentin can be made more impervious so more is put down)
sclerosis of tubules (part of reparative is put inside the tubules to make it sclerotic)
tertiary dentin in pulp (within pulp, reduces size of pulp chamber to make it further from the bacteria)
still asymptomatic (if precedes cavitation then can be remineralised)
describe the spread of caries at the dentino-enamel junction
spreads laterally (mushroom shaped) along the path of least resistance
if early, can remineralise (especially if no enamel cavitation)
so dentin is compromised but enamel isnt. dentin acts as a cushion for enamel so when its compromised the brittle enamel breaks off (collapses)
cavitation is delayed where theres high fluoride (fluorapatite is stronger than hydroxyapatite)
still asymptomatic (but may be sensitive)
describe sensitivity, reversible and irreversible pulpitis
SENSITIVITY
sharp pain
seconds
seen in things like sensodyne adverts
hot/cold causes fluid to move to the dentinal tubules and pulp underneath still normal so the stim. disappears
REVERSIBLE
seconds to minutes
cold more than hot
pulp becomes inflamed and responds more to stimuli
IRREVERSIBLE
minutes to hours
spontaneous
hot worse than cold
worse lying down
infected vs affected dentin
infected: damaged beyond repair
colonised by bacteria
affected: can be saved
typically demin. but structure still intact so can remin.
describe dentinal caries
infected dentin - most superficial part of the lesion
softened/demineralised infected with bacteria
collagen denatured
cannot remineralise
appears as soft necrotic tissue - comes off in layers
stains with caries detection dye
if you remove the ________ dentin, you reach the ________ dentin
infected
affected
describe affected dentin
softened/demineralised and not infected with bacteria
collagen cross-linking remains (structure)
template for remin.
comes off in chips quite easily
doesn’t stain
may be varying shades of colour
why are pulp caries painful?
the pulp tries to extend with the inflammation like get bigger but bc its enclosed in hard tissue it cant so it elicits a pain response (pulp necrosis)
can be destructive - cuts of blood supply and dies
while the pulp is still alive and can respond, it produces a number of _____ _______ against caries
defence mechanisms
describe the 4 pulp complex reparative response against caries
reparative dentin
sclerotic dentin
tubules filled with mineral crystals
called whitlockite (different structure to hydroxy.)
appears glassy
tertiary dentin
different than secondary dentin (normal aging)
this one is in response to a bad (noxious) stimulus
structure varies according to rate of deposition
reactionary dentin - mild stim
reparative - stronger stim
pulp inflammation
brings with it (along with blood flow) resources to fight infection
types of progression of caries
slow progression
rapidly progressing lesion + rampant caries
arrested caries
describe a slowly progressing lesion
takes around 18 months to do
unsupported enamel collapses eventually
wide open cavity
cleansable sometimes
saliva bathed sometimes
darker and less active
describe arrested caries
stopped progressing and are inactive
usually self cleaning
no food impaction
hard and glossy
dark brown/black in colour
mainly buccal/lingual
interproximal adjacent to extracted teeth (molars)
define root surface caries
primary caries on an exposed root surface (often after gingival recession)
penetrates dentin more easily (no enamel barrier over the surface)
cementum is softer (less minerals)
pathological process is the same as primary enamel caries
key differences between enamel and root caries
THINK! colour, minerals, extents of lesion, time
initial lesions are minimal (no colour change)
reduced surface hardness/texture
different than enamel where it appears as white spot lesions
lower mineral content in dentin/cementum
therefore collagen matrix rapidly exposed (demineralisation)
collagen susceptible to physical damage (esp in early stages of demin)
structure maintained if hydrated
collagen matrix easily remineralised
enamel not involved
may be undermined as lesion progresses
difficult to define extent of lesion
still has affected and infected zones tho (margins less easy to identify)
darkens with time
result of bacterial activity
also result of collagen matrix uptaking dyes from food
critical pH of enamel and dentin
enamel: 5.5
dentin 6.2-6.7
root caries progresses at _x the rate of enamel caries
2
risk factors are conditions that…
increase risk of developing disease
modifiable or non-modifiable (changed or can’t be changed)
risk factors for root caries
gingival recession
poor oral hygiene
cariogenic diet
presence of multiple restorations/missing teeth
existing caries
xerostomic medications
compromised salivary flow rate/buffering capacity
explain gingival recession risk factor for root caries (more common in and happens when you have previous what?)
exposed root surface required
more common in old age
previous periodontal disease
explain poor oral hygiene risk factor for root caries
biofilm is a necessary component
impaired dexterity as you age
medical compromise (cant floss/brush etc)
complexity
multiple restorations - can be more difficult to clean (eg under bridge harder than natural teeth)
gingival recession
explain cariogenic diet risk factor for root caries
same as primary enamel caries
elderly less inclined to cook
ready meals have more sugar
elderly more prone to snacking - boredom
dry mouth can lead to sweet sucking
presence of multiple restorations/missing teeth
increases difficulty of cleaning
FPDs (fixed partial denture)
RPDs (removable partial denture)
explain existing caries risk factor for root caries
caries risk is a factor for caries
having caries means you have the right conditions to harbour more
part of risk assessment
explain xerostomic medications AND compromised salivary flow rate/buffering capacity risk factors for root caries
XM
most of most prescribed meds cause dry mouth
nearly half of meds taken by institutionalised elderly cause xerostomia
70% of institutionalised elderly take at least 1 med that causes xerostomia
SFL/BC
saliva flow and buffering may decrease with age although unclear how
management of root caries
(i’m lad urp)
improve salivary flow and buffering
modulate cariogenic biofilm
limit cariogenic food/drinks
attempt to remineralise lesions
discuss meds with GP
use of ETB/water irrigation (if poor manual dexterity)
restorations that release fluoride (glass ionomer types)
patient education (patient based preventive measures)
rampant/rapidly progressing caries
rampant caries
presence of extensive and multiple cavitated and active caries lesions in the same person
baby bottle caries
bottle feeding
radiation therapy caries
radiotherapy of head and neck
meth-mouth caries
misuse of meth (but can occur w. other stuff too)
definition of rampant caries
suddenly appearing, widespread, rapidly burrowing caries resulting in early pulp involvement
can affect teeth (or surfaces) regarded as immune to ordinary decay (class 3 and 6)
more than 10 lesions
causes of rampant caries (XTREME)
extremes of diet
extreme compromise of salivary function
drug/radiation induced xerostomia
increased virulence of strep mutans
bottle caries (early childhood caries)
caused by excessive feeding bottle use
particularly at night
prolonged contact
bottles used as pacifiers
pacifiers coated in sugary solutions
risk factors for early childhood caries
evolving immune system and bacterial micobiota
hypoplastic defects (newly erupted teeth)
breast/bottle diet
more prevalent among children from low-income families
parents seek restorative (not preventive) treatment, lack of motivation and knowledge of prevention
radiation therapy caries
results from radiation to major salivary glands, not to individual teeth
challenging bc of increasing treatment costs and higher risk of osteoradionecrosis
xerostomia + diet changes may influence development
resin composites with fluoride application seems to be ideal management approach
radiation related caries continued
hyposalivation + xerostomia caused by salivary gland damage are indirect effects mostly associated with RRC
loss of salivary buffer capacity lowers oral pH
biofilm accumulation
shift to a more cariogenic oral microbiota mainly composed of lactobacillus sp. and strep mutans
difficulties in performing adequate oral hygiene practices
trismus, pain and oral mucositis
diet changes with radiation related caries
highly cariogenic food
softer
carb rich
combat weight loss
poor eating dysphagia, pain and oral/oropharangeal mucositis
shift to sweet foods
last taste to disappear during treatment
meth-mouth caries
(reduces?
how it looks?
users more likely to have?)
meth reduces salivary flow and buffering capacity
teeth are blackened, stained and falling apart
meth users are more likely to have untreated decay, missing/filled teeth and caries compared to non-users
meth mouth pt caries description
long-acting
dehydration (low saliva)
hyperactivity (bad lifestyle, so no oral hygiene)
increase intake of carbonated beverages (dry mouth)
poor OH
methadone caries
opioid used to manage opioid addiction
frequently given as suspension high in sugar
presents as:
rampant caries
periodontal disease
xerostomia
poor OH
hypoglycaemia
frequent sugar ingestion
dental management of methadone/meth caries
oral hygiene
diet
other preventive methods
treatment
many illicit drug users are dental phobic
when thinking about the impact of the pattern of sugar consumption, what do you need to consider (as it affects the balance of demineralisation and remineralisation?)
amount of sugar consumed
type of sugar consumed
can it be washed away? sticky? takes time to dissolve in the mouth?
frequency of sugar consumption
what is the importance of the critical pH?
altering pH alters the saturation point of things
the critical pH means the saliva and plaque fluid cease to be saturated with calcium and phosphate, and the hydroxyapatite in the dental enamel can now dissolve
what factors lower the plaque pH?
acid production (by acidogenic bacteria)
food source available for the bacteria
what factors raise the plaque pH?
saliva flow
fluids in the mouth (above neutral and no sugar in them) - wash away acid
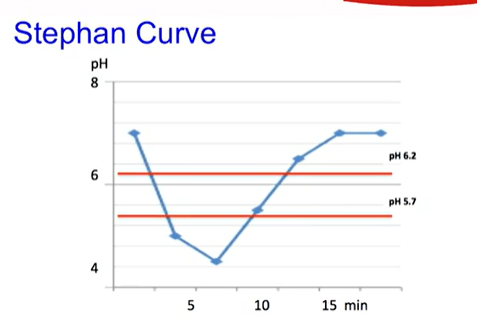
what did Stephan do?
(they didnt give me a last name lol)
first measured plaque pH and published it in 1944
did seminal work on plaque pH (pattern of sugar intake on dental caries)
stephan’s curve!
flip over for visualiser of stephan’s curve