Cardiac function
1/29
Earn XP
Description and Tags
part 1, lecture 2
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
What are the phases of the cardiac cycle?
atrial systole
isovolumetric contraction
ventricular ejection
isovolumetric relaxation
late diastole
phase 1 - Atrial systole
last 20% of filling occurs when the atria contract
additional flow of blood called the atrial kick or boost
small backflow into venae cavae as no one-way valves - used to diagnose high right atrial blood pressure.
phase 2 - Isovolumetric contraction
ventricular contraction with no change in ventricular volume
spiral bands of ventricular muscle contract and squeeze blood upwards
blood pushes on underside of AV valves and forces them closed
AV and semilunar valves are closed, therefore blood has nowhere to go
pressure builds up quickly without changing ventricular volume
phase 3 - ventricular ejection
contraction of ventricles creates enough pressure to open semi-lunar valves
blood ejected into arteries
pressure generated by ventricles is driving force for blood flow
high pressure blood forced into arteries displaces the low pressure blood that fills them and pushes it further into the vessels
phase 4 - isovolumetric relaxation
ventricles begin to relax, leading to a rapid fall in ventricular pressure
ventricular pressure falls below aortic pressure
small volume of blood flows backwards and closes aortic valve —→ brief rise in arterial pressure (dicrotic notch)
phase 5 - late diastole
both chambers are relaxed
ventricle begins to fill with blood passively before atrial systole & start of another cycle
What is occurring during the 2 sounds that make up the heartbeat?
“lub” - closure of AV valves
“dub” - closure of semi-lunar valves
Abnormal sounds heard during auscultation of the heart.
gallops - third sound is heard
clicking - abnormal movement of the valves
whoosh - murmurs caused by valvular incompetance
EMG
burst of electrical activity measured when a muscle is contracted.
ECG
small changes in potential detected between different locations on the skin
potentials caused by the spread of electrical currents through underlying structures.
3 main waves on an ECG
P wave - atrial depolarisation
QRS complex - ventricular depolarisation
T wave - ventricular repolarisation
*NB - atrial repolarisation masked by QRS complex and therefore not represented
What is the R-R interval an accurate measurement of?
heart rate
What is a long Q-T interval indicative of?
long Q-T syndrome - channelopathies where there are mutations in myocardial Na+ & K+ channels
can sometimes occur because of drug side-effects
aortic stenosis
reduction in valve orifice area for left ventricle when opened
high outflow resistance
large pressure gradient across aortic valve during ejection
peak systolic pressure in ventricle greatly increased
increase in cardiac afterload, decrease in stroke volume, increase in cardiac muscle mass
risk of heart faliure
end diastolic volume
volume of blood in the heart at the end of the cardiac filling phase
end systolic volume
volume of blood left in the heart at the end of the ejection phase
Describe experiment 1 (increased preload and the Starling law) done by Starling.
peripheral resistance (therefore afterload) and heart rate were kept constant. Cardiac filling pressure (therefore preload) was increased.
cardiac output increased under these conditions
Increased cardiac output must be due to increased stroke volume as heart rate was kept constant
left ventricular and aortic pressures increased - greater amount of blood ejected against the same resistance.
increased filling pressure lead to ventricular stretch to accommodate for the increased end diastolic volume.
stimulates intrinsic property to increase the force of contraction in response to elongation/stretch
“energy of contraction is a function of the length of the muscle fibre” - Starling law of the Heart
TL;DR - put more blood in, get more blood out so heart volume remains the same.
Describe experiment 2 (increased afterload and the Starling law) done by Starling.
Heart rate and filling pressures are kept constant
peripheral resistance (therefore afterload) is increased. Heart finds it harder to force blood through the system.
increase in aortic & left ventricular pressures
increase in end systolic volume as less complete emptying of the heart
initial fall in stroke volume & cardiac output as pumping against an increased resistance
increased afterload promotes increase in end diastolic volume - ventricle walls stretched more
cardiac output increased by Frank-Starling mechanism
*NB - biphasic response: 1st a small decrease in cardiac output then a recovery of cardiac output
The Anrep effect
Autoregulation method where myocardial contractility increases with afterload
Sustained myocardial stretch activates Na+/H+ exchangers
Na+ enters the sarcolemma
Na+ gradient reduces
Na+/Ca2+ exchanger that exploits this gradient stops working as effectively
Ca2+ accumulates inside the sarcolemma and taken up by sarcoplasmic reticulum SERCA pumps as a result
CICR from sarcoplasmic reticulum increased upon stimulation of cardiac myocyte by action potential
increase in force of contraction
increase stroke volume & cardiac output to try to maintain tissue perfusion.
What are sympathetic influences on the heart?
cardiac accelerator nerves extends to SAN, AVN & portions of myocardium
releases noradrenaline
binds to beta-1 receptors
SAN - positive chronotropic effect
fibres in ventricles - positive inotropic effect
Positive chronotropic effect
increases frequency of contraction
positive inotropic effect
increased strength of contraction
What are the parasympathetic influences on the heart?
right & left vagus nerves release acetylcholine
acts on muscarinic receptors in SAN, AVN & atrial myocardium
negative chronotropic effect but no ionotropic effect
What are the endocrine influences on the heart?
adrenaline is both positively chronotropic & positively ionotropic.
What is the pacemaker potential?
spontaneous, slow depolarisation of the SAN from -60mV to threshold at -40mV
Why is the slope of the pacemaker potential especially important?
determines the time to reach threshold value
sympathetic influences increase slope
parasympathetic influences decrease slope
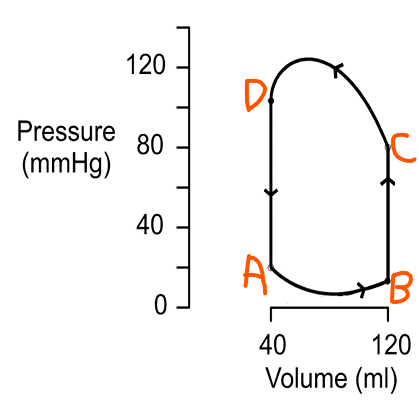
What happens at point A of the cardiac pressure-volume loop?
ventricle has completed a contraction
contains minimum amount of blood
pressure at a minimum
blood flows into atria from pulmonary veins
mitral valve opens
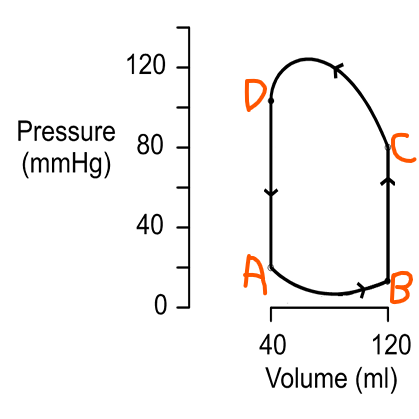
What happens at point B of the cardiac pressure-volume loop?
ventricles fill
contain maximum volume of blood
end diastolic volume
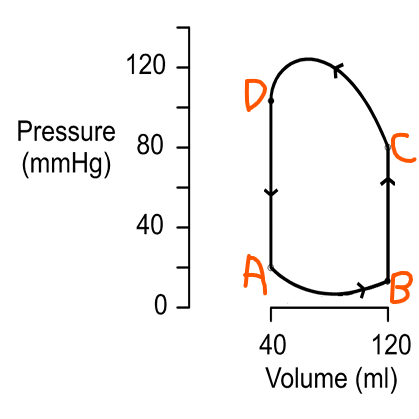
What happens at point C of the cardiac pressure-volume loop?
mitral valves close
ventricular pressure increases
no change in volume (isovolumetric contraction)
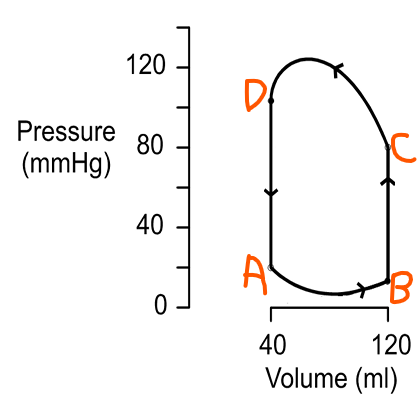
What happens at point D of the cardiac pressure-volume loop?
ventricular pressure exceeds aortic pressure
aortic valves open
ejection takes place
rapid fall in ventricular volume to reach D
heart not completely emptied of blood