Section 3 7 Mass transport
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
22 Terms
Structure of heamoglobin
Primary structure (sequence of amino acids), to secondary structure (into a helix) to tertiary structure (bonds between R-groups) to quaternatary structure bonds between the four polypeptide strands.
There are two alpha and two beta polypeptide
Each polypeptide contains a heam group that contains Fe 2+ ion that bonds to O2
The different properties of heamoglobin
Gas exchange (lungs): high oxygen concentration, low carbon dioxide, high oxygen affinity, Oxygen associated (more oxygen loaded than unloaded)
Respiring cells (muscle cells): low oxygen concentration, high carbon dioxide, low oxygen affinity, Oxygen dissociated (more oxygen unloaded than loaded)
Key point: with higher levels of CO2 it causes an acidic environment, lowers PH and changes the Quaternary structure of the hemoglobin so oxygen is loaded less easily
Explain the oxygen dissociation curve:
This is a graph that compares saturation of heamoglobin with oxygen and the partial pressure of oxygen.
1st oxygen to bind: At low partial pressures it is hard for the first oxygen to bind because the polypeptide subunits are closely linked together.
2nd and 3rd oxygen: Once the first O2, it causes the quaternatary structure to change making it easier for the other molecules of oxygen to bind. Therefore, it requires less oxygen pressure increase for greater oxygen saturation (positive cooperativity)
4th oxygen: Once the 2nd and 3rd oxygen bind, there is only one binding space left for oxygen molecule so less probability for last oxygen to bind.
What does left shift and right shift of the oxygen curves mean?
Left shift: the greater the affinity of heamoglobin for oxygen (so loads oxygen more readily and unloads less easily) because at lower partial pressures greater oxygen saturation
Right shift: the lower the affinity of heamoglobin (so loads oxygen less readily but unloads more oxygen) because at lower partial pressures smaller oxygen saturation
Why mammals have double circulatory system?
They have a small surface area to volume ratio
They are active organisms
Double circulatory system ensures that blood is transported at high pressures around the body for example lower pressure required to the lungs, but higher pressure for body cells.
So, blood does not mix, so we don’t have partial oxygen concentration in blood so not steep diffusion path.
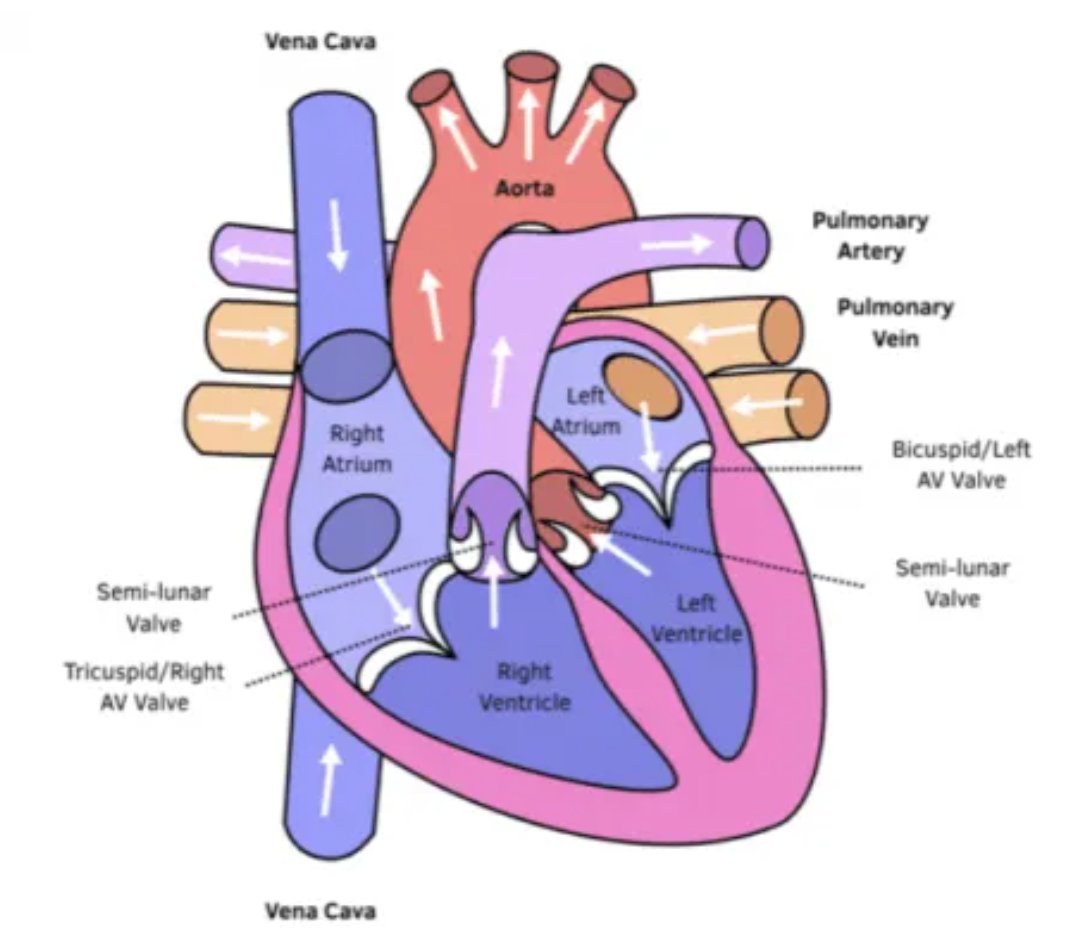
The structure of the heart:
Atrium and ventricles: Atria walls are thinnner (less muscle tissue) than Ventricle, as ventricles pump blood with more pressure to further places in body.
Left atrioventricular valves (Tricuspid) // Right atrioventricular valves (Bicuspid)
Semi-lunar valve: between the ventricles and (pulmonary artery or aorta)
Aorta: Oxygenated blood from the heart to the rest of the body cells (under high pressure)
Vena cava: Deoxygenated blood from the body cells into the heart
Pulmonary artery: deoxygenated blood from the heart into the lungs
Pulmonary vein: Oxygenated blood from the lungs to the heart
What are the blood vessels that carry oxygenated and deoxygenated blood into the kidneys?
Oxygenated blood into the kidney’s: Renal artery
Deoxygenated-blood out of kidneys: Renal vein
A comes first then V
The cardiac cycle simple stages:
Diastole (relaxation of the heart): Blood enters the heart via the vena cava and pulmonary vein, the relaxation of the ventricles allow blood to enter from the atria. Semi-lunar valves closed, atrioventricular valves are open.
Atrial systole (Atria contraction): Atria contract pushing blood into the ventricles. Semi lunar valves are closed, atrioventricular valves are open.
Ventricular systole (Ventricles contract): Ventricles contract to pump blood into the aorta. The pressure of ventricles increases which causes semi-lunar valves open, atrioventricular valves to close.
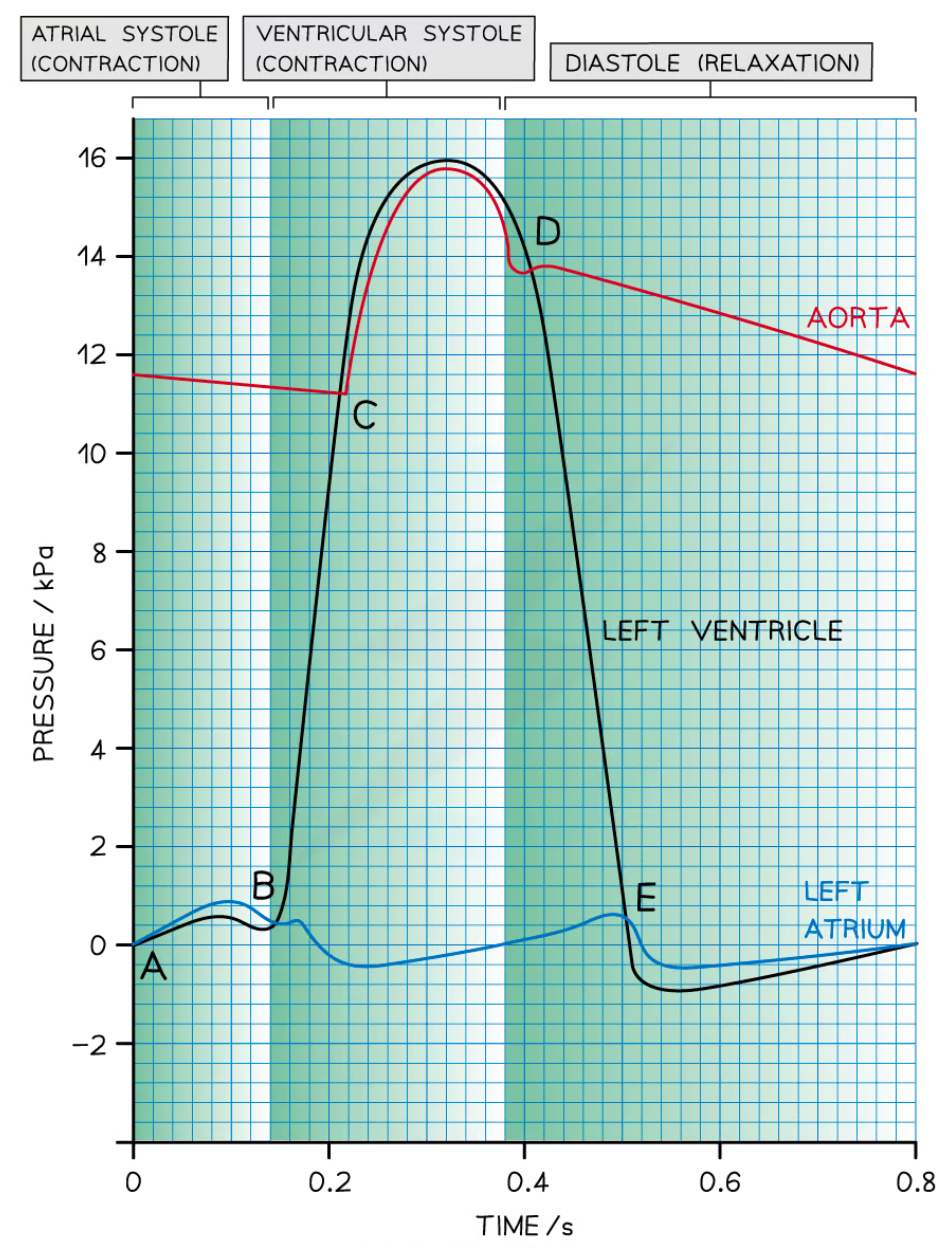
Explain the cardiac cycle graph:
A => The end of diastole: Atrium filled with blood, pressure is higher in atrium than ventricle so AV open.
Between A and B => atrial systole: Left atrium contracts, increases in atrial pressure and forces blood into the left ventricle, ventricular pressure increases as it is filled with blood. Pressure is higher in atrium than in ventricle, so the AV valve open.
Point B => Beginning of ventricular systole: Left ventricle contracts which causes the ventricular pressure to increase, pressure in left atrium drops as the muscle relaxes, pressure in the ventricle exceeds pressure in the atrium so AV valves are closed.
Point C => Ventricular systole: Ventricle continues to contract, pressure in left ventricle exceeds that in the aorta, SL valves opens
Point D => beginning of diastole: left ventricle has been emptied of blood, muscles in the walls of the left ventricle relax and pressure falls bellow that in the newly filled aorta, SL valves closes.
Between points D and E => early diastole: Ventricle remains relaxed and ventricular pressure continues to decrease, blood flows into the relaxed atrium from pulmonary vein, causes increased pressure.
Point E => diastole: Relaxed left atrium fills with blood, causing pressure in atrium to exceed the ventricle. AV valves opens
After point E => late diastole: short period of left ventricle expanding (relaxed muscles), increases internal volume of left ventricle and decrease in ventricle pressure. Blood flows slowly into the newly opened AV valves into ventricle, brief decrease in pressure of atrium. The pressure of both atrium and ventricle increases slowly as they continue to fill with blood.
How to calculate Cardiac output?
Cardiac output (dm cubed /min) = heart rate (BPM) x stroke volume (dm cubed)
Arteries and their function
They transport blood under high pressure from the heart to tissues.
Thicker muscle layer than veins: they can constrict and dilate to control the volume of blood flowing through them.
Elastic layer thicker than veins: they stretch and recoil to maintain blood under high pressure.
Thick walls: to prevent the vessels bursting under pressure
No valves: blood is under high pressure, so doesn’t tend to flow backwards
Arterioles and their function:
Aterioles are similar to Arteries, but they are smaller in diameter, larger muscle layer and lumen.
The muscle layer is thicker than arteries: restricts the flow of blood into the capillaries
Elastic layer is thinner than arteries: Blood is at lower pressure
Veins and their function:
Muscle layer is thinner compared to arteries: carry blood away from heart so contraction and dilation cannot control the flow of blood.
Elastic layer is thinner compared to arteries: The blood pressure is too low.
Overall thickness of wall is thin as pressure is too low, there is no risk of bursting.
Valves are present to prevent the backflow of blood// Veins can be flattened easily which compresses blood within them to one direction
Capillaries and their function:
Walls consist of lining layer: extremely thin, so distance for diffusion of substances is short for rapid diffusion.
Numerous and highly branched: Large SA:V for exchange
Narrow diameter + narrow lumen: Short diffusion pathway
Spaces between lining: White blood cells can escape to deal with infections
The route of blood through the blood vessels:
Oxygenated blood exists the heart through the aorta (artery) which enters the arterioles which are smaller in diameter to control the flow of blood and reduce pressure so not to damage the capillary network.
Once in capillaries exchange of materials takes place
Then deoxygenated blood is transported from the veins into the heart
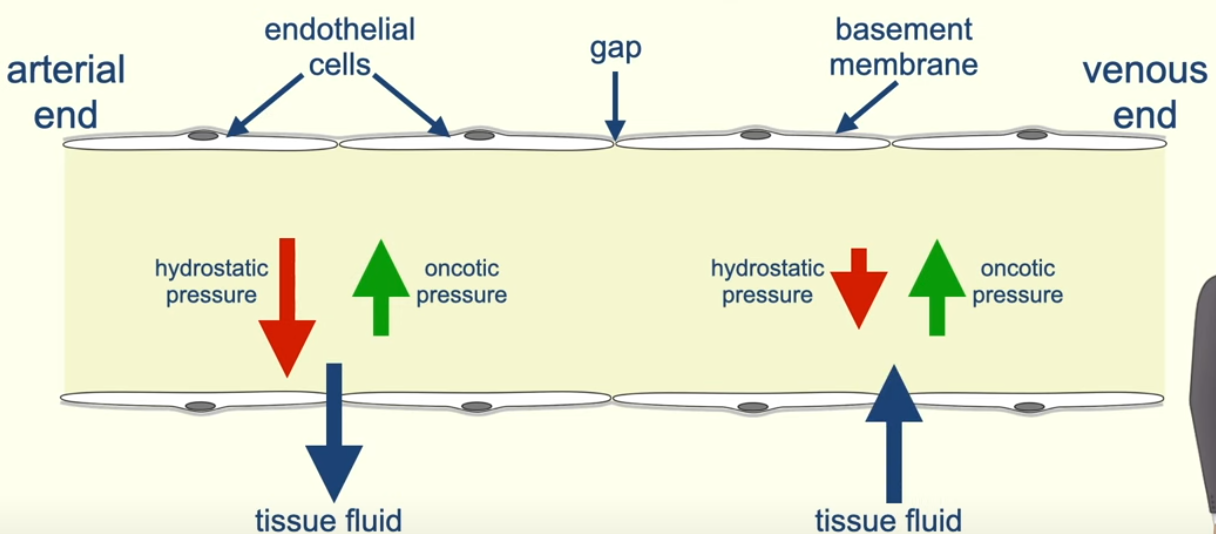
What is tissue fluid?
It is a watery liquid that contains: glucose, amino acids, fatty acids, ions in solution and oxygen.
Tissue fluid exchanges materials between the blood and the cells.
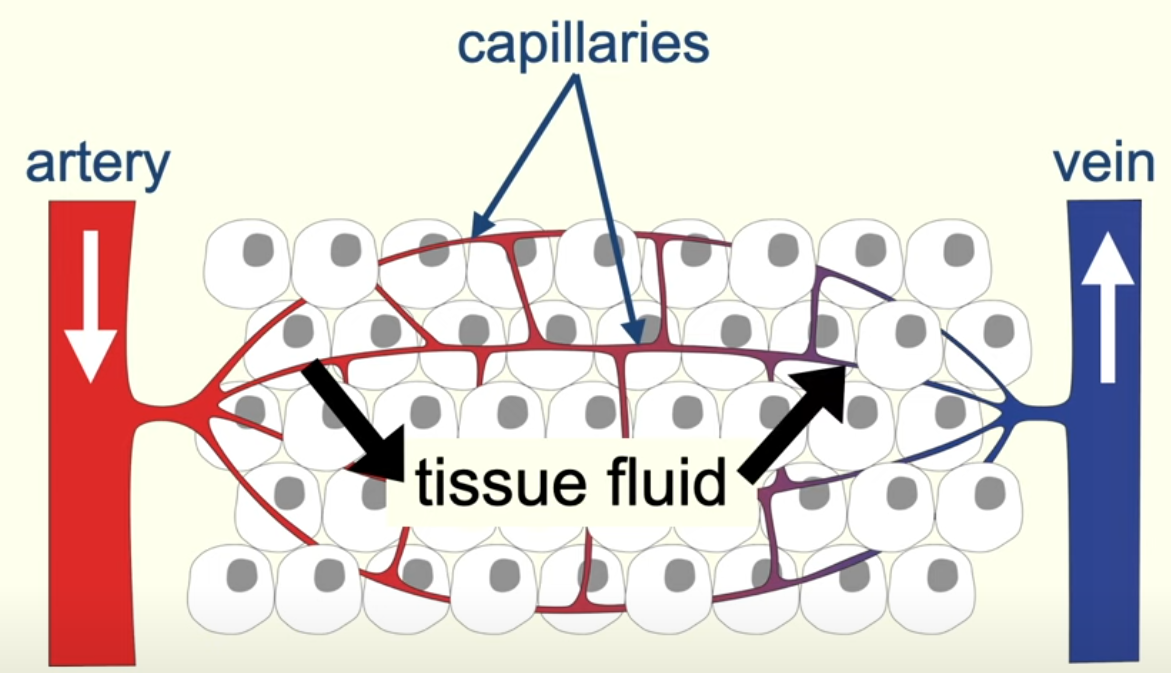
The journey of tissue fluid in blood vessels:
The blood pumped by the heart causes hydrostatic pressure at the arteriole end, which causes the tissue fluid to move out of the blood and into the tissue.
As the tissue fluid leaves the capillaries (contains plasma proteins) they lower water potential of blood plasma, so water moves down the concentration gradient into the capillaries.
Near the arterial end the hydrostatic pressure is greater than the water pressure, which forces the tissue fluid out of capillaries.
At the venous end of capillaries the hydrostatic pressure is much lower than the water pressure so tissue fluid enters back into the capillaries. This is because large amount of water has left the blood in the capillaries.
When there is a 4 mark question on how tissue fluid is returned back:
The proteins remain in the blood
This causes a water potential gradient
So, water returns via osmosis
Some tissue fluid returns via lymphatic system
Xylem function and cohesion-tension theory:
Properties of Xylem:
Lignin: which spiral structure to withstand the tension of water being pulled.
Bidirectional
Transpiration stream
How water is moved through the plant?
Known as the cohesion-tension theory => water molecules experience cohesion through hydrogen bonding. The column of water doesn’t break because there is adhesion of water molecules with the xylem walls.
Water is lost through the stomata via evaporation, and water is absorbed through roots by absorption (transpiration stream)
Water molecules form hydrogen bonds and stick together (cohesion)
Water molecules stick to other substances known as tension.
Due to the transpiration stream, xylem is under tension so pulling water molecules upwards.
Structure related to function:
No organelles, so less obstruction to the flow of water.
Hollow tube with lignin to withstand the force of water
Pores in cellulose walls, so water can be moved to adjacent cells such as phloem
Waterproof to resist tension
Phloem and translocation steps:
Properties of Phloem:
Sieve tubes: long-thin structures at end to end of the phloem tubes
Companion cells: contain mitochondria to release energy and ATP for active transport of molecules
Translocation, unidirectional
Translocation:
The plant transports sucrose and dissolved substances from the source (leaf where photosynthesis occurs) to the sink (Root hair cells, where no photosynthesis takes place).
Glucose is formed in leaf cells via photosynthesis which gets converted to sucrose.
H+ ions are actively transported out of the companion cells, which increases concentration gradient of H+ ions, so they move down the concentration gradient into the companion cells coupled with sucrose molecule (co-transport)
The sucrose can now diffuse through the plasmodesmata and into the sieve tube element cells, so high concentration of sucrose, which lowers the water potential in sieve tube element cells, causing water to move into the sieve tubes from xylem via osmosis.
There is now hydrostatic pressure inside the sieve tube, causing the dissolved minerals to move up or down.
As the sap moves down, the sucrose gets diffused into the root cells, increasing water potential, so water moves into the xylem via osmosis.
Mass flow hypothesis and evidence:
The mass flow hypothesis is the transport of sucrose (cell sap = dissolved sucrose in water) from the source to the sink, via the phloem.
Evidence supporting: The concentration of sucrose is higher in the leaves than the roots, companion cells contain many mitochondria and releases ATP, increase levels of sucrose in leaf follows increase sucrose in phloem, lack of oxygen reduced translocation of sucrose in phloem.
Evidence against: Function of sieve tubes are still unclear they have evidence as to prevent bursting at high pressure, not all the solutes move at same rate they should if mass flowing, sucrose delivered at same rate but they should go to areas with low sucrose conc first.
Ringing experiement
A circular ring of bark removed, where phloem present, so transport of sucrose is inhibited, and is found at these locations high concentration of sucrose
Observations:
the bark above is swelled with high sucrose concentration
death of cells bellow the ring as sucrose transportation is inhibited
Conclusion: that phloem transports dissolved sucrose.
Tracer experiments
Radioactive carbon is used, which are incorporated into the glucose during photosynthesis converted to sucrose.
The radioactive carbon can be traced and found that travels from the source to the sink evidence for mass flow.