Fetal Circulation
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
16 Terms
Where are pharyngeal arches developed from?
How many pairs are they?
Describe the linings of these pharyngeal arches
What migrates to these pharyngeal arches and what is the result of this?
Development of Pharyngeal Arches:
@ 4th-5th week, series of bulges @ future face and anterior neck appear → Pharyngeal Arches (6 pairs)
Characteristics of Pharyngeal Arches:
lined by ectoderm and endoderm
Neural crest cells migrate into pharyngeal arches to surround cores of paraxial mesoderm
together: forms most structures in the pharyngeal arches.
Define Pharyngeal Arches
How many are them?
Where are they and why are they important?
What do they contain/have? What do they recruit and what does this develops?
Pharyngeal Arches:
Def: (5) paired transient swellings
Location: surrounds foregut; btw developing brain and heart;
Importance: critical for dev. of head and neck structures.
Contents:
Contain all 3 germ layers & has own artery, nerve, cartilage, and muscles
recruit neural crest cells → cartilages, bones, muscles, nerves, arteries of the head and neck
What is the first structure to develop in each pharyngeal arch?
Describe this structure
Where does this structure terminate? What does this form?
Describe the temporal property of this developmental step
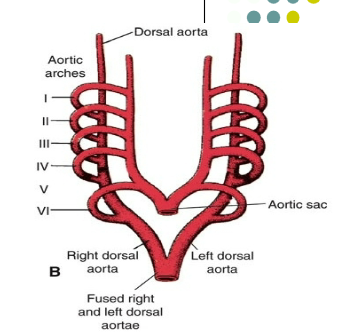
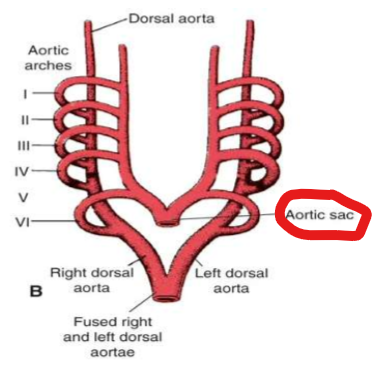
Aortic (Pharyngeal) Arch Artery:
first structure to develop in each pharyngeal arch
Communicating blood vessel btw dorsal aorta and ventral aorta (aortic sac in humans)
Termination:
Each arch terminates in R/L dorsal aorta
R/L dorsal aorta → fuse @ caudal → descending aorta
Temporal Property:
Transient; appear in a cranial-to-caudal sequence and are not all present simultaneously
Where does the Ventral Aorta (aortic sac) developed from? Describe its initial structure
What does the aortic sac develops into?
Development of the Aortic Sac (ventral aorta)
develops from the truncus arteriosus
initially exists as paired structures → fusion → aortic sac
What the Aortic Sac Forms:
forms right and left horns
R: brachiocephalic artery
L: proximal ascending aorta
Describe what the Six aortic arches develops into
Development of the 6 Aortic Arches:
First arch → maxillary A.
Second Arch → hyoid and stapedial A. (temporary embryonic structures ) → orbital, dural or maxillary branches
Third Arch → Common/External/Internal (first part) Carotid A.
rest of the internal carotid is formed by the dorsal aorta
Fourth Arch
L: aortic arch
R: proximal right subclavian artery
Distal segment from 7th intersegmental artery
Fifth Arch → nothing develops here
Sixth Arch
R: proximal right pulmonary artery
L: proximal left pulmonary artery and ductus arteriosus
Where does the recurrent laryngeal nerve hook around? What is the function of this nerve?
Recurrent Laryngeal N. hooks/function:
Left Side: hooks around the ductus arteriosus
Right Side: subclavian artery
due to absence of the distal part of the right sixth arch.
Function: main nerve supply to the larynx
What are Vitelline Arteries?
What happens when these Arteries Fuses and the function of these structures
What does the vitilline Veins form before entering the sinus venosus?
How do Vitilline veins relate to liver development?
What are the Vitilline veins a precursor of?
Vitelline Arteries:
paired branches of the dorsal aorta that supply the yolk sac
Fusion of Vitilline Arteries:
Fusion → three unpaired arteries in the dorsal mesentery of the gut
celiac (foregut)
superior mesenteric (midgut)
inferior mesenteric (hindgut).
supply the parts of the gastrointestinal tract derived from each part of the primitive gut.
Vitelline Veins:
Before entering sinus venosus → forms plexus around duodenum and passes through septum transversum
Form hepatic sinusoids when liver cords grow into the septum transversum
Vitelline Veins Development:
Right Side:
hepatocardiac portion of IVC
superior mesenteric vein
Left Side:
Nothing
Plexus around duodenum → portal vein
What are Umbilical Arteries?
What does it become?
Describe what happens to it after birth
Initially, where are the Umbilical Veins? What happen to these veins ?
What is the Ductus Venosus?
What happens to these veins after Birth?
Umbilical Arteries:
paired ventral branches of the dorsal aortae
shift to become branches of the common iliac arteries
Umbilical Arteries After Birth:
persist as internal iliac and umbilical arteries
distal umbilical arteries → obliterated → medial umbilical ligaments
Umbilical Veins:
Initially pass on each side of the liver, connecting with hepatic sinusoids
Right umbilical V. and Prox. Left Umbilical V. disappears
left umbilical vein will carry blood from placenta to liver
Ductus Venosus:
forms btw L Umbilical V. and right hepatocardiac channel (IVC)
shunts oxygenated blood from placenta past the liver into the heart
Umbilical V. After Birth
left umbilical vein → ligamentum teres hepatis
ductus venosus → ligamentum venosum
What three major pairs of veins forms the venous systems
Vitelline (omphalo-mesenteric) veins: carry blood from the yolk sac
Umbilical veins: carry oxygenated blood to the embryo from chorionic villi
Cardinal veins: drain the body of the embryo proper
What are the Cardinal Veins consists of?
What happens when these veins fuse
Cardinal Veins:
Consists of Anterior/Posterior Cardinal Veins
A: Drains cephalic part
P: Drains rest of the embryo
Anterior and Posterior Cardinal Veins will fuse → common cardinal vein and will drain into the sinus horn
What forms the SVC?
How does the left brachiocephalic vein form?
How does the left superior intercostal vein form?
SVC: Right anterior cardinal v. + common cardinal v.
Left Brachiocephalic v.: anastomosis between the anterior cardinal veins
Left Superior Intercostal v.: terminal portion of the left posterior cardinal veins
Describe Fetal Circulation
Placenta → fetus via umbilical vein → bypasses liver via ductus venosus → IVC
@ IVC: placental blood mixes with deoxygenated blood
IVC → RA → LA via foramen Ovale
Small portion of blood @ enters RV → Pulmonary trunk → Aorta via ductus arteriosus
LA → LV → Systemic circulation → Placenta via 2 umbilical veins
NOTE: at all stages, deoxygenated and oxygentated blood mixes
Describe the circulatory changes @ birth
Describe what happen to some vasculatures
Circulatory Changes at Birth:
Baby’s First Breath → Lung caps are filled w/ blood → O2 blood from Lungs → LA
this causes LA > RA in pressure → holds the valves of foramen ovale shut
Foramen Ovale Valve + septum secundum → fossa ovalis
Probe patency: in 20% of peeps; fusion does not occur
Changes @ vasculature:
ductus arteriosus → ligamentum arteriosum
distal umbilical arteries → medial umbilical ligaments
umbilical vein → ligamentum teres hepatis (round ligament of the liver)
ductus venosus → Ligamentum venosum
After birth, what normally closes the Ductus Arteriosus?
What is the consequences of patent ductus arteriosus (PDA)?
How can you detect PDA in a patient
Ductus Arteriosus Closure due to:
Increased O2 Content
decreased prostaglandin levels (constriction of DA)
Symptoms/consequences of PDA:
L → R shunt due to higher pressure in aorta
increased pulmonary artery (PA) pressure → right
ventricular hypertrophy (RVH) → R →L shunt →late cyanosis
Detection:
murmur at first intercostal space left parasternal border
Define Coarctation of the Aorta
What are the two types and describe the differences between the two of them
Symptoms/Consequences?
Coarctation of the Aorta:
Def: congenital narrowing of the aorta
Two Types:
Preductal coarctation
usually associated w/ patent ductus arteriosus (PDA)
Surgery in infancy is required for survival
Postductal coarctation
not usually associated w/ PDA
collateral circulation develops and patients typically survive into adulthood (but not beyond 50 w/o surgery)
Symptoms/consequences:
Higher blood pressure in upper vs. lower extremities
Weak pulses in lower extremities
Compensatory development of collateral circulation
Describe the collateral circulation created during Coarticulation of the Aorta
Anterior and posterior intercostal arteries:
Supplies intercostal muscles or the thoracic aorta
Increased size of collaterals present as “notching of the ribs” in CXRs
***These collateral is also used to maintain blood supply to anterior intercostal spaces in surgery when internal thoracic
artery is used for cardiac bypass surgery.***
Superior/Inferior epigastric artery:
Superior from internal thoracic artery and Inferior from external iliac
Provides collateral circulation from Upper limb (subclavian A.) to the Lower Limb (Femoral A.)
***These collaterals could be used to bypass obstruction of abdominal aortic aneurysm or atherosclerotic plaques in the common iliac, external iliac arteries***