Dermatology 7
1/12
Earn XP
Description and Tags
28/05 - 29/05
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
13 Terms
Define PAPULES and list the names of 10 diseases that appear with these lesions
PAPULE: circumscribed, raised or depressed lesion <1cm in diameter, it may be solid or cystic.
Acne vulgaris
Keratosis pilaris
Angioma
Melanoma
BCC
Molluscum contagiosum
Primary syphiloma (primary spyphilis)
Secondary manifestations (condyloma piano and secondary palmoplantar syphylis)
Merkel cell carcinoma
Trichoepithelioma
Describe the signaling pathway involved in BCC and its mutations
The Hedgehog (Hh) signaling pathway is a key molecular pathway during embryonic development.
In adults, however, this pathway is normally inactive or significantly downregulated. It is crucial in the pathogenesis of basal cell carcinoma (BCC).
Normally, the PTCH1 receptor inhibits SMO, preventing downstream activation. When the Hedgehog ligand (SHH) binds to PTCH1, this inhibition is lifted, allowing SMO to activate GLI transcription factors, which translocate into the nucleus and activate genes involved in cell proliferation.
In basal cell carcinoma (BCC), this pathway becomes aberrantly activated, even in the absence of SHH, due to genetic mutations, resulting in uncontrolled cell growth and tumour formation.
The most common mutations include:
Loss-of-function mutations in PTCH1, which prevent it from inhibiting SMO
Gain-of-function mutations in SMO, allowing it to activate the pathway independently of PTCH1.
Describe urticaria lesions
Urticaria lesions, also known as wheals or hives, are characterized by the following features:
Raised, well-circumscribed areas of skin (wheals) that are Erythematous (red), Edematous (swollen), often pale in the center with a red flare at the edges. They may occur anywhere in the body, vary in size, shape (rounded, annular and serpiginous) and number, and usually disappear within 24 hours (transient).

Describe the role of C1INH involved with angioedema
C1INH inhibits plasma kallikrein and Factor XIIa. These enzymes are involved in the production of bradykinin, a potent vasodilator at the base of angioedema’s pathology.
In C1INH deficiency or dysfunction, bradykinin levels rise excessively, leading to:
Vasodilation
Increased vascular permeability
Fluid leakage into tissues → swelling (angioedema).
This is the primary mechanism in hereditary angioedema (HAE) types I and II and in acquired angioedema related to C1INH alterations.
John is a 38-year-old male who presents with complaints of intermittent facial redness and visible blood vessels on his cheeks and nose with no involvement of nasogenial sulcus for the past 2 years. He states that the redness is more noticeable after drinking alcohol, exposure to hot weather, or physical exertion. He denies any significant pain but mentions occasional burning or stinging sensations. John does not have a history of acne vulgaris or other dermatologic conditions. His mother had similar symptoms, which were attributed to "rosy cheeks." He tried using moisturizers and sunscreens, but without improvement. What is the most likely diagnosis?
ACNE ROSACEA
Anna, a 32-year-old woman complains of sudden patchy hair loss. On examination, there are round, non-scarring alopecic areas without scaling or erythema, exclamation mark hairs and yellow dots. Short, tapered hairs are visible at the margins of the patches. She reports no itching or pain. What is the most likely diagnosis?
ALOPECIA AREATA
Luisa, a 62-year-old postmenopausal Caucasian woman, presents to the dermatology clinic with a 6-month history of progressive hairline recession. She describes a gradual loss of hair along the frontal scalp, accompanied by mild itching in the affected areas. She denies any systemic symptoms, recent illness, or new medications. On examination, there is a band-like area of scarring alopecia along the frontotemporal hairline, with perifollicular erythema and scaling. The eyebrows appear thinned, especially laterally. A “lonely hair sign” is observed—single terminal hairs remaining in otherwise bald, scarred skin. The remainder of the scalp appears unaffected. There is no nail or mucosal involvement. What is the most likely diagnosis? How do you make a definitive diagnosis?
FRONTAL FIBROSING ALOPECIA. Diagnosis is made by biopsy of the scalp.
Describe anonychia and name 2 pathologies that can cause it
ANONYCHIA is complete absence of the nail plate or of all the nail unit.
Epidermolysis Bullosa Dystrophica
Lichen Ruber Planus
Nail-Patella syndrome
Define onichodynia and list 4 causes of this condition
Pain, which can be acute or chronic, anywhere in the nail system.
Subungual tumors, especially glomic tumor
Vasoconstrictive/ischemic events
Psoriasis
Pachyonychia
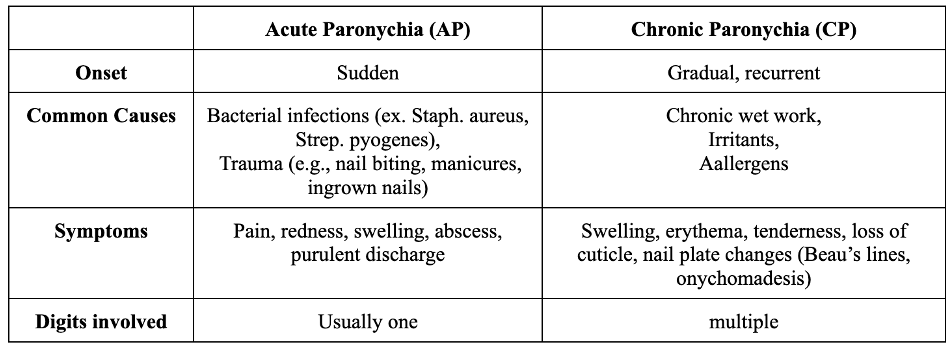
Differences between acute and chronic paronychia
ACUTE PARONYCHIA has a sudden onset. It is usually caused by bacterial infections (Staph. Aureus, Strep. Pyogenes) or by trauma (nail biting, manicures, ingrown nails). Symptoms include pain, redness, swelling, abscess, purulent discharge. It involves usually only 1 digit.
CHRONIC PARONYCHIA has a gradual onset, and it can also recur. It is usually caused by chronic wet work, irritants, allergens. Symptoms include swelling, erythema, tenderness, loss of cuticle, nail plate changes (Beau’s lines, onychomadesis). It can involve multiple digits.
Define CRUSTS and list the names of 5 diseases that appear with this lesion
Dried fluid on the skin’s surface, usually serum, blood, pus or a combination. Easier to remove than scales.
Impetigo
Crusted scabies
Eczema herpeticum
Pemphigus vulgaris
Pemphigus foliaceus

Define VESICLES and BULLAE (or BLISTERS) and list the names of 6 diseases that appear with these lesions
VESICLE: fluid-filled papule <1cm in diameter
BULLA: papule that is >1cm in diameter
Pemphigus vulgaris
Bullous pemphigoid
Epidermolysis bullosa
Eczema herpeticum
Dermatitis herpetiformis
Hailey Hailey disease
Define PLAQUES and NODULES and list the names of 10 diseases that appear with these lesions
PLAQUE: circumscribed, superficial, elevated or depressed plateu area >1cm in diameter
NODULE: palpable, ovoid/dome-shaped lesion >1cm in diameter, may be solid or cystic.
Psoriasis
Lipoma
Keloids
Cysts
Erythema nodosum
Neurofibromatosis
BCC
Cutaneous tuberculosis
Erysipelas
Classic Kaposi sarcoma