Physiology Unit 3 Discussion Quiz 2
0.0(0)
Card Sorting
1/110
There's no tags or description
Looks like no tags are added yet.
Last updated 5:39 AM on 3/29/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
111 Terms
1
New cards
What is the cardiovascular system’s role in homeostasis?
main transport system for integrating homeostasis
2
New cards
Why is the cardiovascular system necessary?
diffusion only supports life when the source is less than 100 um away
3
New cards
Every cell in the body is __________ um away from a capillary
1-10 um
\
The exception is the cornea, but the rest are located this close so that capillaries can quickly deliver oxygen and nutrients to cells via the plasma and so that CO2 and wastes can be returned via the plasma
\
The exception is the cornea, but the rest are located this close so that capillaries can quickly deliver oxygen and nutrients to cells via the plasma and so that CO2 and wastes can be returned via the plasma
4
New cards
What are the components of the cardiovascular system?
heart
blood
blood vessels
blood
blood vessels
5
New cards
What is the function of the heart in the CV system?
biological pump that generates force to move blood
6
New cards
What is the function of the blood in the CV system?
medium for O2, CO2, waste, nutrients, and messengers like hormones to be transported in
7
New cards
What is the function of blood vessels in the CV system?
the tubing through which the blood flows (play an active role in the movement of blood, not passive, they make messengers and are capable of responding to messengers)
8
New cards
What is circulation out of the heart and into the lungs called?
pulmonary circulation
(unoxygenated blood is pumped to the lungs)
(unoxygenated blood is pumped to the lungs)
9
New cards
What is circulation out of the heart and into the rest of the body called?
systemic circulation
(oxygenated blood is pumped to the rest of the body to deliver nutrients)
(oxygenated blood is pumped to the rest of the body to deliver nutrients)
10
New cards
What is circulation returning to the heart from the lungs called?
pulmonary circulation
(oxygenated blood from the lungs enters the heart ready to be distributed)
(oxygenated blood from the lungs enters the heart ready to be distributed)
11
New cards
What is circulation returning to the heart from the rest of the body called?
systemic circulation
(deoxygenated blood from the body returns to the heart to be pumped to the lungs and become oxygenated again)
(deoxygenated blood from the body returns to the heart to be pumped to the lungs and become oxygenated again)
12
New cards
What fraction of blood does plasma make up?
55%
(plasma is part of the ECF)
(plasma is part of the ECF)
13
New cards
What fraction of the blood does erythrocytes (hematocrit) make up?
45%
(RBC or hematocrit is mainly for gas transport)
(RBC or hematocrit is mainly for gas transport)
14
New cards
What is the buffy coat in blood?
contains leukocytes (WBC) and platelets
\
insignificant volume in blood
\
insignificant volume in blood
15
New cards
if an individual has more testosterone, what happens to the expected fraction of hematocrit in their blood?
it goes up
(because more testosterone = more RBC)
(because more testosterone = more RBC)
16
New cards
All blood cells start out as ______________
a multipotent uncommitted hematopoietic stem cell
17
New cards
What are the 4 commitments of blood cells?
1. reticulocyte (develops into redblood cell and is used for oxygen transport)
2. megakaryocyte (fragments into platelets for clotting)
3. collectively WBC (monocytes become macrophages and are used for immunity defense)
4. B and T lymphocytes (also about immunity)
18
New cards
What are the characteristics of red blood cells?
biconcave discs
large surface area, small volume (good for diffusing o2)
lots of hemoglobin (oxygen binding protein)
organelles are extruded (no DNA, DNA only in buffy coat)
large surface area, small volume (good for diffusing o2)
lots of hemoglobin (oxygen binding protein)
organelles are extruded (no DNA, DNA only in buffy coat)
19
New cards
What is sickle cell disease?
an inherited blood disorder that causes a change in the primary structure of the hemoglobin chain, making the cells look like sickles and causing blockages of capillaries, leading to tissue damage/pain/consequent anemia
20
New cards
What is the cause of sickle cell disease?
a mutation to one amino acid in the hemoglobin chain
(people with the disease must be homozygous for the mutant allele)
(people with the disease must be homozygous for the mutant allele)
21
New cards
What is sickle cell trait?
when individuals are heterozygous for the mutant allele, and thus have both normal hemoglobin and abnormal hemoglobin
\
(symptoms for people with sickle cell trait are only observed when the oxygen level is unusually low, such as when they experience high altitude)
\
(symptoms for people with sickle cell trait are only observed when the oxygen level is unusually low, such as when they experience high altitude)
22
New cards
What removes deformed sickle-like RBC from circulation?
the spleen
(this is why the spleen can become overfilled and painfully enlarged in the event of a large increase in sickled cells)
(the sickled cells can also block blood vessels in the spleen, causing pain and damage to it)
(this is why the spleen can become overfilled and painfully enlarged in the event of a large increase in sickled cells)
(the sickled cells can also block blood vessels in the spleen, causing pain and damage to it)
23
New cards
How do kidneys respond to low O2 delivery?
they increase erythropoietin secretion
which is then transported by CV system to bone marrow
bone marrow responds by increasing production of erythrocytes (which are red blood cells)
this results in increased hemoglobin concentration and thus an increased O2 carrying capacity
and overall results in a restored O2 delivery
which is then transported by CV system to bone marrow
bone marrow responds by increasing production of erythrocytes (which are red blood cells)
this results in increased hemoglobin concentration and thus an increased O2 carrying capacity
and overall results in a restored O2 delivery
24
New cards
the heart is actually composed of
2 separate pumps and circulatory systems
25
New cards
What is the definition of an artery?
carries blood away from the heart
26
New cards
What is the definition of a vein?
carries blood towards the heart
27
New cards
artery
carries blood away from the heart
28
New cards
vein
carries blood to the heart
29
New cards
Which side of the heart is thicker?
the left side has a thicker wall of muscle because a greater generation of pressure is required to get blood into the systemic circulation
30
New cards
What is perfusion?
blood flow through capillary beds (arterioles, capillaries, and venules in all organs and tissues except the lungs)
31
New cards
Walk through the path of a blood cell starting in the right atrium?
right atrium (d)
passes through AV valve in to the right ventricle (d)
passes through semilunar valve into the pulmonary artery/trunk (d)
is oxygenated at pulmonary capillaries located at lungs
traveling back towards heart in pulmonary veins (o)
enters left atrium (o)
passes through AV valve into the left ventricle (o)
passes through semilunar valve into the aorta (o)
travels through systemic arteries and delivers oxygen to body via systemic vascular beds (now deoxygenated)
traveling back toward heart in systemic veins (d)
enters vena cava and continues traveling back to heart (d)
returns to right atria (d)
\
passes through AV valve in to the right ventricle (d)
passes through semilunar valve into the pulmonary artery/trunk (d)
is oxygenated at pulmonary capillaries located at lungs
traveling back towards heart in pulmonary veins (o)
enters left atrium (o)
passes through AV valve into the left ventricle (o)
passes through semilunar valve into the aorta (o)
travels through systemic arteries and delivers oxygen to body via systemic vascular beds (now deoxygenated)
traveling back toward heart in systemic veins (d)
enters vena cava and continues traveling back to heart (d)
returns to right atria (d)
\
32
New cards
How are vascular beds arranged in the body?
in parallel
(they can’t be arranged in series, or else too much blood pressure would be required to get oxygen to the last organs in the series - additionally, most of the nutrients and oxygen would be depleted by the end of the series)
(they can’t be arranged in series, or else too much blood pressure would be required to get oxygen to the last organs in the series - additionally, most of the nutrients and oxygen would be depleted by the end of the series)
33
New cards
What are the key implications of having capillary beds (organs) arranged in a parallel fashion
1. Blood quality to all organs (all organs get good quality blood)
2. flow regulation to individual organs (can easily regulate flow to single organs without affecting others)
3. Amount of initial pressure required (don’t need as much initial pressure when they are arranged in a parallel fashion)
34
New cards
in systemic circulation, capillary beds are ________
in parallel
35
New cards
what happens to blood flow during strenuous exercise?
large increase in blood flow goes to skeletal muscle
decrease in blood to kidneys and abdominal organs in GI
decrease in blood to kidneys and abdominal organs in GI
36
New cards
What is resting blood flow?
5 L/min
37
New cards
What can blood flow get to at its max?
around 20 L/min
38
New cards
What is the equation for blood flow?
F = (delta P)/R
\
F: flow (L/min) - note: not velocity
delta P: pressure gradient
R: resistance to flow
\
F: flow (L/min) - note: not velocity
delta P: pressure gradient
R: resistance to flow
39
New cards
Why is chronic high blood pressure dangerous?
although high blood pressure might be occurring, a person doesn’t experience many symptoms early on because the pressure gradient is all that matters, and not the actual magnitude of the values
\
the body can only sense when blood flow is off, so if flow is still normal, high blood pressure will go unnoticed until it’s too late
\
the body can only sense when blood flow is off, so if flow is still normal, high blood pressure will go unnoticed until it’s too late
40
New cards
What is the equation of blood flow that we must know?
F = (delta P x pi x r^4) / (8 x L x n)
\
L: vessel length (longer the vessel, more R)
n: viscosity of fluid (blood thickness, thicker blood, more R)
r: radius of vessel (raised to 4th power)
\
L: vessel length (longer the vessel, more R)
n: viscosity of fluid (blood thickness, thicker blood, more R)
r: radius of vessel (raised to 4th power)
41
New cards
What does resistance come from in blood vessels?
from blood scraping against vessel walls, hence why the radius of the vessel is so important
(large radius = less resistance = more flow)
always look at cross sectional area when considering equivalence of different blood vessels
(large radius = less resistance = more flow)
always look at cross sectional area when considering equivalence of different blood vessels
42
New cards
Which AV valve is tricuspid?
right AV valve
43
New cards
Which AV valve is bicuspid?
left AV valve
(also called mitral valve)
(also called mitral valve)
44
New cards
What is endocardium?
the inner lining of the heart
45
New cards
What is the myocardium?
cardiac muscle (makes up vast majority of ventricle)
46
New cards
What is the epicardium?
secretory epithelium on top of myocardium
47
New cards
What is the pericardium?
a folding over of the epicardium that creates an even more external layer of the heart
48
New cards
What is the chordae tendinae
white fibrous connective tissue
49
New cards
In the heart, where there is more volume,
there is more pressure
50
New cards
What happens when the atrium pressure is higher than the ventricle pressure?
the AV valve is open and flow of blood is favored to move from atrium into ventricle
51
New cards
What happens when the ventricle pressure is greater than the atrium pressure?
the ventricles start to contract, squeezing the volume of blood in the ventricle, thus raising the ventricular pressure
\
this causes the cusps of the AV valve to swing up and the AV valve closes
\
this causes the cusps of the AV valve to swing up and the AV valve closes
52
New cards
What is prolapse?
when the cusps flip up into the atrium, the AV valve is called a prolapsed valve, as it allows blood to flow backwards from the ventricle into the atrium
53
New cards
What structures help prevent prolapse?
chordae tendinae and papillary muscles
\
they accompish this by chordae tendinae being attached to the cusps and the chordae tendinae are being pulled down by papillary muscles
\
they accompish this by chordae tendinae being attached to the cusps and the chordae tendinae are being pulled down by papillary muscles
54
New cards
What is the overall purpose of heart valves?
to promote one way direction of blood flow
55
New cards
What are the four valves?
right AV valve (tricuspid valve)
left AV valve (bicuspid or mitral valve)
pulmonary semilunar valve
aortic semilunar valve
left AV valve (bicuspid or mitral valve)
pulmonary semilunar valve
aortic semilunar valve
56
New cards
What opens and closes heart valves?
pressure gradients
57
New cards
Where does coronary circulation start?
right outside the aortic semilunar valve
(coronary arteries are the very first branch of circulation driven out of the left ventricle)
(coronary arteries are the very first branch of circulation driven out of the left ventricle)
58
New cards
What is the purpose of the coronaries?
supply blood to the myocardium
59
New cards
Why are the coronary arteries required?
the myocardium is too thick to supply via diffusion from the chamber lumen
60
New cards
What determine the heart rate?
a small fraction of cardiac muscle cells called autorhythmic cells (aka pacemaker cells)
\
(spontaneously active)
\
(spontaneously active)
61
New cards
What are responsible for rapidly spreading the electrical stimulus throughout the chambers?
a small fraction of cardiac cells called conducting cells
62
New cards
What constitutes the majority of cardiac cells?
contractile cells
63
New cards
What is the role of the SA node?
the true pacemaker (starts each heart beat by oscillating to threshold first)
\
sits in right atrium
\
sits in right atrium
64
New cards
What is the AV node?
a chain of cells that slowly conducts excitation from the atria into the ventricles
\
the AV node delays propagation, as the AP propagation is slow
(this delay is important because we don’t want the atria and ventricles to contract at the same time)
\
the AV node delays propagation, as the AP propagation is slow
(this delay is important because we don’t want the atria and ventricles to contract at the same time)
65
New cards
What are the reasons for the AV node delay?
it is a chain of cells
ion channel density
ion channel density
66
New cards
What is the role of the bundle of his and Purkinje fibers?
conducting cells
get signal to ventricular contractile cells
\
AP propagation is fast
get signal to ventricular contractile cells
\
AP propagation is fast
67
New cards
What is the only expected electrical connection between atria and ventricle?
AV node
68
New cards
What is the base?
where the valves are attached
69
New cards
What is the apex?
the point of the heart at the bottom
70
New cards
Can cusps of valves conduct electrical signals?
no, they are insulators
71
New cards
What is the conduction pathway?
1. SA node
2. Atrial contractile cells
3. AV node
4. Bundle of His
5. Bundle branches
6. Purkinje fibers
7. Ventricular contractile cells
72
New cards
What are the four implications of the conduction pathway?
1. Everything in the conduction pathway is joined by gap junctions, so you only need 1 SA node cell to get to threshold and the whole thing will go
2. You only need one bad cell to mess the whole thing up
3. We can insert external pacemakers to overcome cells that have gone bad
4. Every cell must participate (nobody gets a rest)
73
New cards
What is the setup of ECG lead 1?
recording electrode on left arm (+)
reference electrode on right arm (-)
reference electrode on right arm (-)
74
New cards
What occurs during the P wave?
the SA node gets to threshold and atria start to depolarize and contract
75
New cards
What happens gives rise to the isopotential period during the P-R segment?
1. atria contractile cells are uniformly depolarized
2. AV nodal delay
76
New cards
What does the R wave show?
evidence of ventricular depolarization
77
New cards
What happens during the T wave?
ventricular repolarization and relaxation
78
New cards
Where is atrial relaxation?
atrial relaxation is buried in the R wave, we can’t see it and can’t measure it because of this
79
New cards
Where do the Bundle of His and Purkinje fibers of the conducting system deliver the excitation to?
to the apex of the heart so that ventricular contraction occurs in an upward sweep
80
New cards
What is automaticity?
capable of spontaneous, rhythmical self excitation
81
New cards
List the intrinsic depolarization rates?
SA node: 100-120 APs/min
AV node: 60-80 APs/min
Purkinjie fiber: 30-50 APs/min
\
This shows that the AV node and purkinjie fibers are capable of pacemaking, but it’s not their primary role, so they are called latent pacemakers
AV node: 60-80 APs/min
Purkinjie fiber: 30-50 APs/min
\
This shows that the AV node and purkinjie fibers are capable of pacemaking, but it’s not their primary role, so they are called latent pacemakers
82
New cards
Sinus rhythm
normal cardiac excitation-contraction sequence beginning at the SA node
83
New cards
What is a latent pacemaker?
lying quiet or hidden, not active potential pacemakers
\
includes AV node and conducting cells
\
includes AV node and conducting cells
84
New cards
What is an ectopic pacemaker?
abnormal, any site driving ventricular excitation-contraction sequence that isn’t the sA node
\
(when a latent pacemaker has to take over, it becomes an ectopic pacemaker)
\
(when a latent pacemaker has to take over, it becomes an ectopic pacemaker)
85
New cards
What is tachycardia
HR greater than 100 bpm
86
New cards
What is bradycardia
HR slower than 60 bpm
87
New cards
What is fibrillation
totally irregular and chaotic AP propagation
\
totally dysfunctional pump with no organized sequence or pattern of excitation (doesn’t send blood to the body or the brain)
\
totally dysfunctional pump with no organized sequence or pattern of excitation (doesn’t send blood to the body or the brain)
88
New cards
How do AED devices correct for fibrillation?
applies massive depolarization that stops cells in misrhythm, and then hopefully the SA node is able to take over again
89
New cards
What are the 3 different kinds of Action Potentials in the heart?
1. nodal cell AP
2. conducting cell AP
3. contractile cell AP
90
New cards
What is the basis of difference in the 3 different AP types in the heart?
the different types of ion channels present for each
91
New cards
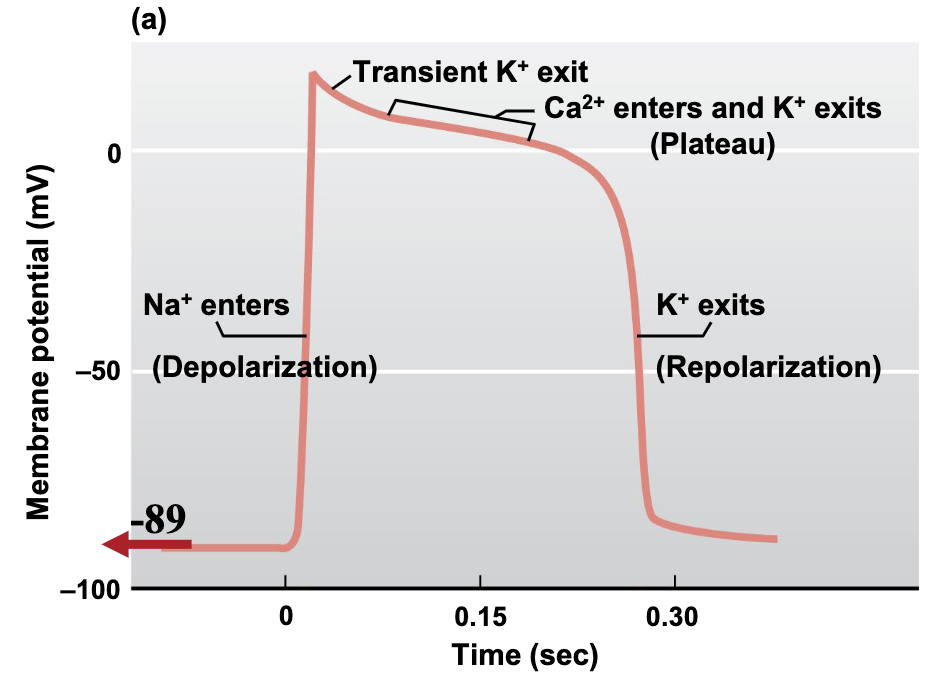
Characteristics of contractile cell AP
RMP is -89 mv and is completely flat/unchanging
current injection from gap junction from nearby depolarized cells is what kicks off depolarization
rapid depolarization caused by opening of voltage gated Na+ channels
prolonged plateau of depolarization is due to the slow but prolonged opening of voltage gated Ca2+ channels (L-type channels aka DHPRs)
Unique K+ channels transiently open for a moment at peak causing very slight repolarization
CICR leads to mechanical contraction we know
current injection from gap junction from nearby depolarized cells is what kicks off depolarization
rapid depolarization caused by opening of voltage gated Na+ channels
prolonged plateau of depolarization is due to the slow but prolonged opening of voltage gated Ca2+ channels (L-type channels aka DHPRs)
Unique K+ channels transiently open for a moment at peak causing very slight repolarization
CICR leads to mechanical contraction we know
92
New cards
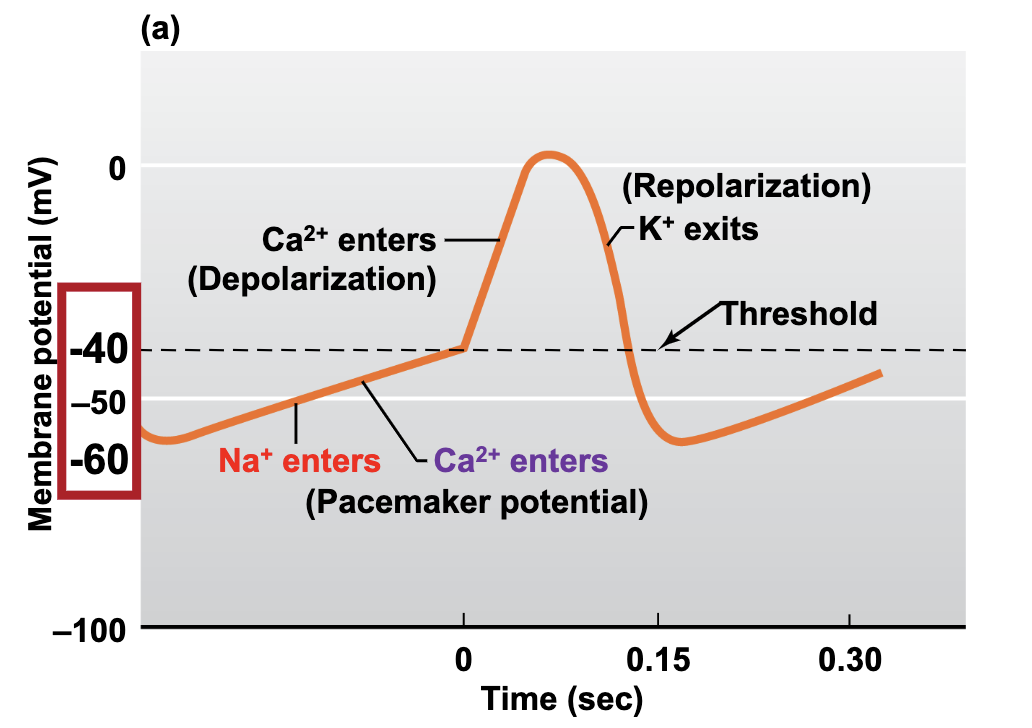
Characteristics of nodal cell AP
RMP is never flat! Always oscillating
\
self depolarizing pacemaker potential:
\-Closing K+ channels
\-Opening of funny f-type Na+ channels depolarize the cell from -60 to -50 mv
\-Opening of transient T-type Ca2+ channels gets us to threshold of -40 mv
\
The AP upstroke occurs due to opening of voltage gated L-type calcium channels at threshold
\
Peak is slightly more positive than 0
\
Reopening of K+ channels plus inactivation of L-type Ca2+ channels are responsible for repolarization
\
This repolarization back to -60 mv by K+ channels is what opens the funny Na+ channels, thus starting the cycle over again
\
Maximum diastolic hyperpolarization is -60 millivolts (the most negative value that the oscillation makes)
threshold is -40 mv
\
self depolarizing pacemaker potential:
\-Closing K+ channels
\-Opening of funny f-type Na+ channels depolarize the cell from -60 to -50 mv
\-Opening of transient T-type Ca2+ channels gets us to threshold of -40 mv
\
The AP upstroke occurs due to opening of voltage gated L-type calcium channels at threshold
\
Peak is slightly more positive than 0
\
Reopening of K+ channels plus inactivation of L-type Ca2+ channels are responsible for repolarization
\
This repolarization back to -60 mv by K+ channels is what opens the funny Na+ channels, thus starting the cycle over again
\
Maximum diastolic hyperpolarization is -60 millivolts (the most negative value that the oscillation makes)
threshold is -40 mv
93
New cards
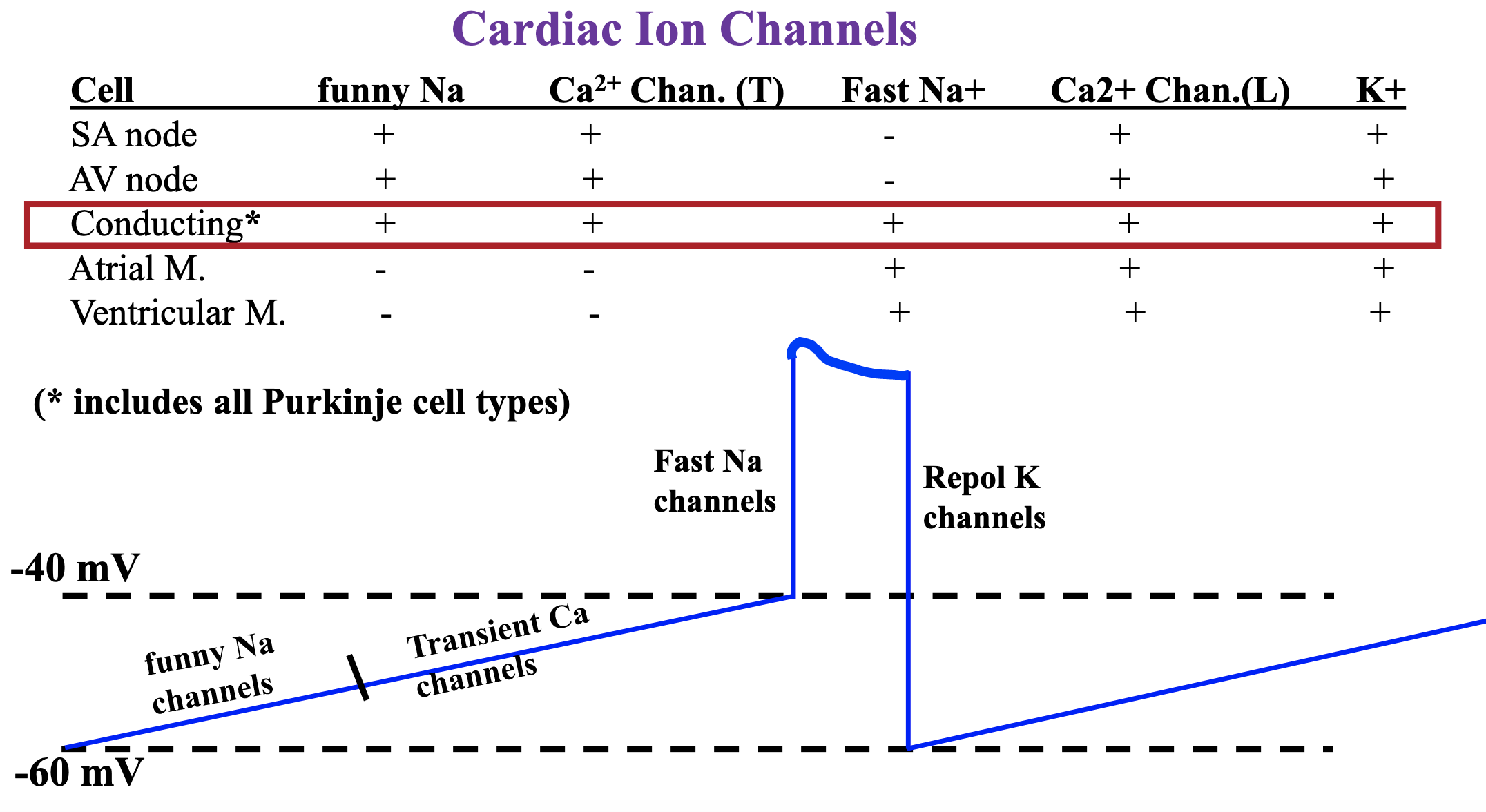
What type of channels do Purkinje fiber cell APs utilize?
all of them
funny Na
transverse Ca2+
Fast Na+
L type Ca2+ channels
K+ channels
funny Na
transverse Ca2+
Fast Na+
L type Ca2+ channels
K+ channels
94
New cards
characteristics of conducting cell AP
conducting cell is oscillating, it is a latent pacemaker
\
threshold is -40 mv
\
Funny Na+ channels kick of depolarization to -50 mv from -60 mv
\
Transient Ca2+ channels get cell to threshold of -40 mV
\
Fast Na+ channels give rise to upstroke
\
long plateau caused by L-type Ca2+ channels
\
Repolarization caused by opening of K+ channels
\
threshold is -40 mv
\
Funny Na+ channels kick of depolarization to -50 mv from -60 mv
\
Transient Ca2+ channels get cell to threshold of -40 mV
\
Fast Na+ channels give rise to upstroke
\
long plateau caused by L-type Ca2+ channels
\
Repolarization caused by opening of K+ channels
95
New cards
What does the plateau of atrium action potential align with?
P-Q segment
96
New cards
What does the plateau of contractile cell AP align with?
S-T or R-T segment
97
New cards
Go through slides 23&24 of lecture 2
98
New cards
systole
ventricular excitation (contraction)
99
New cards
diastole
ventricular relaxation (filling)
100
New cards
What fraction of time are we in diastole?
2/3 of the cardiac cycle
\
we spend more time filling in diastole than we do in systole contracting
\
we spend more time filling in diastole than we do in systole contracting