Sonographic and Doppler Evaluation of the Female Pelvis
1/106
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
107 Terms
LMP
Date of last menstrual period for assessment.
Gravidity
Number of times a woman has been pregnant.
Parity
Number of pregnancies carried to viable gestation.
Hormone regimen
Hormonal treatments affecting pelvic health.
Pelvic examination
Clinical assessment of pelvic organs.
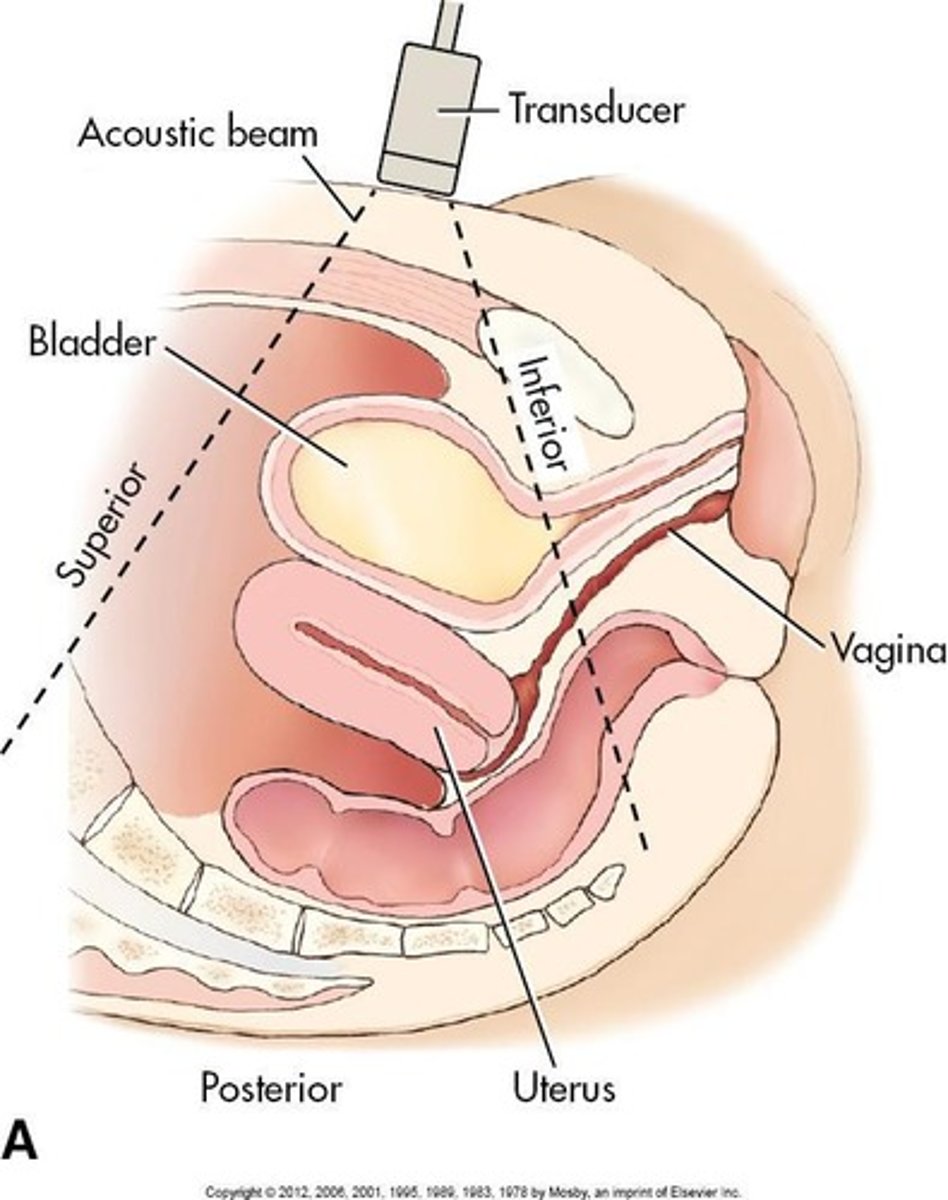
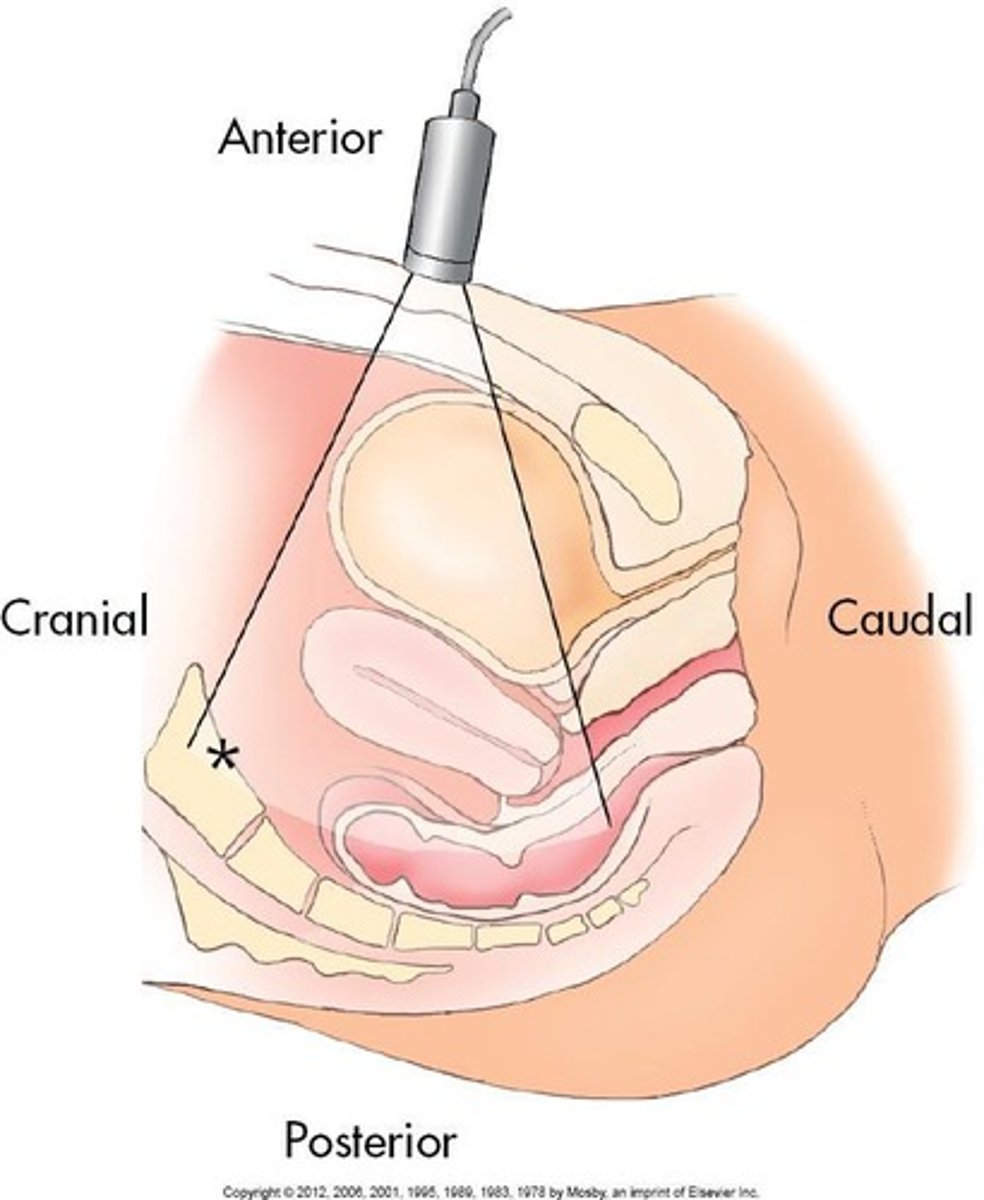
Transabdominal approach
External ultrasound scanning across the abdomen.
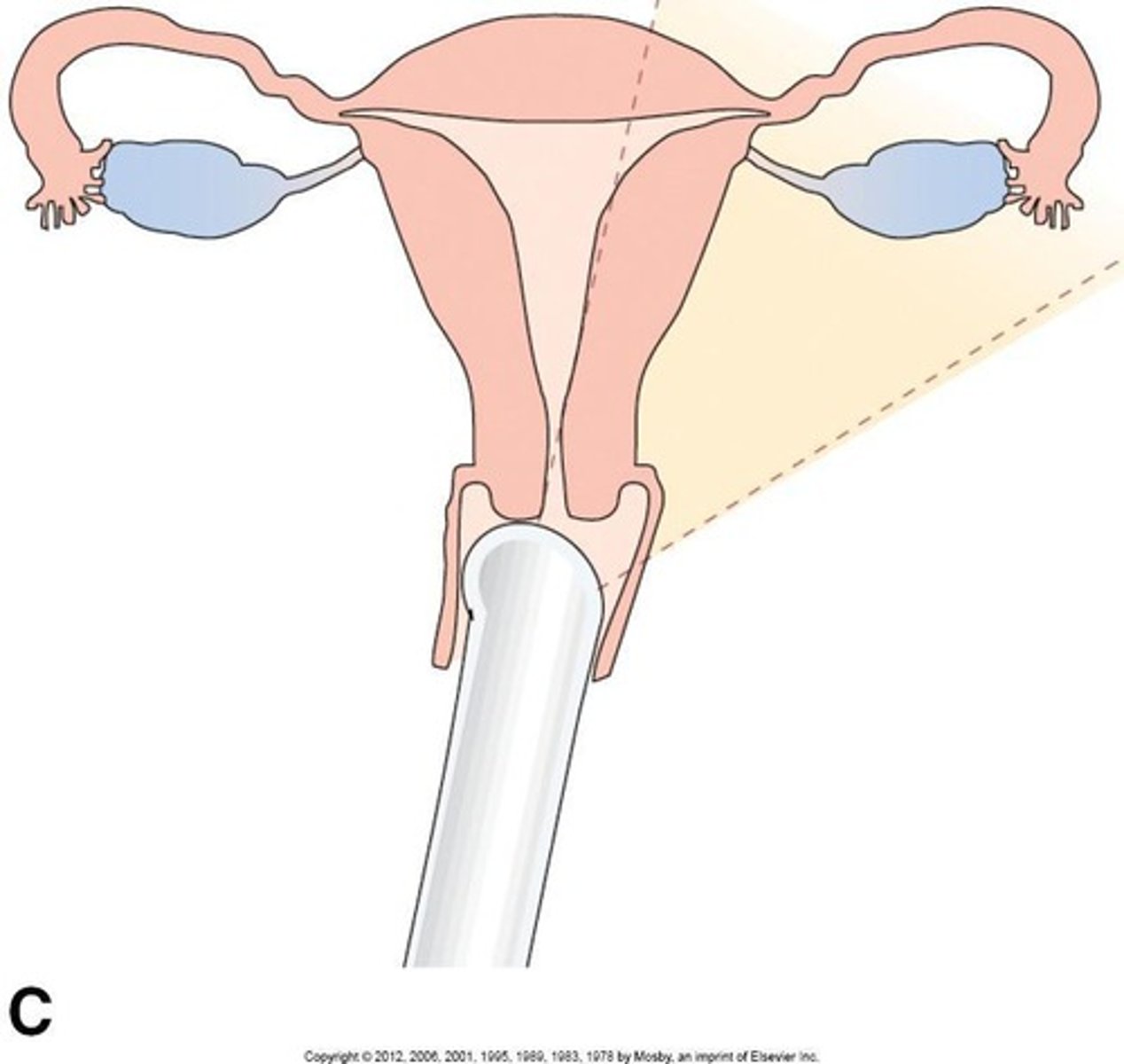
Transvaginal approach
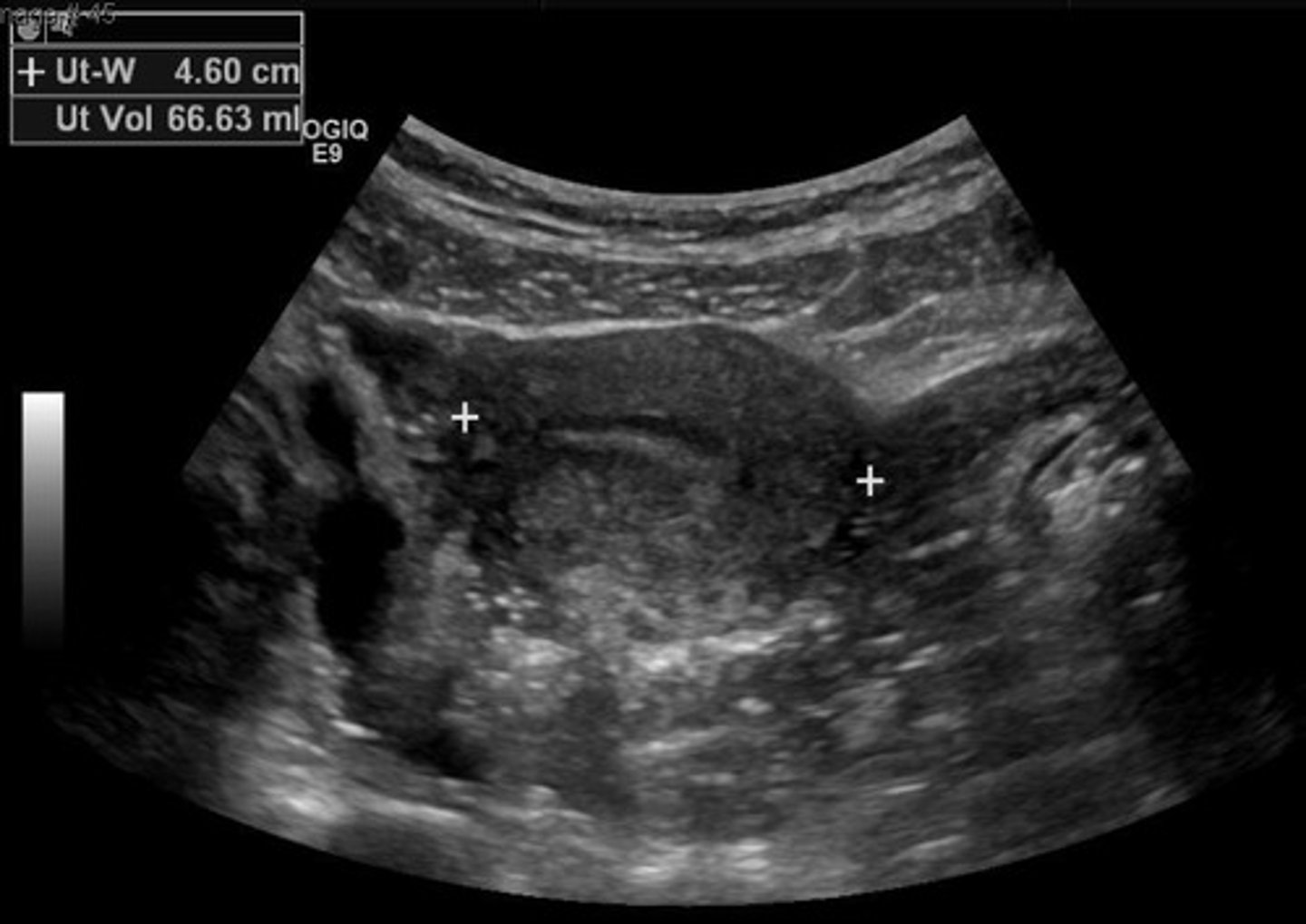
Internal ultrasound examination via the vagina.
Uterine size
Measured dimensions of the uterus.
Endometrium
Inner lining of the uterus, analyzed for thickness.
Myometrium
Muscular layer of the uterus, evaluated for masses.
Cervix
Lower part of the uterus, assessed for dimensions.
Cul-de-sac
Space in the pelvis evaluated for fluid or masses.
Ovarian size
Measured by length and AP dimensions.
Ovarian volume
Calculated from ovarian dimensions.
Sonographic technique
Methodology for performing ultrasound examinations.
Mass characterization
Features to assess when a mass is found.
Location of mass
Determines if mass is uterine or extrauterine.
Size of mass
Overall dimensions of the detected mass.
External contour
Shape and borders of the mass.
Internal consistency
Composition of the mass: cystic or solid.
Pelvic ultrasound protocol
Standardized steps for conducting pelvic ultrasound.
Adnexa
Refers to ovaries and fallopian tubes.
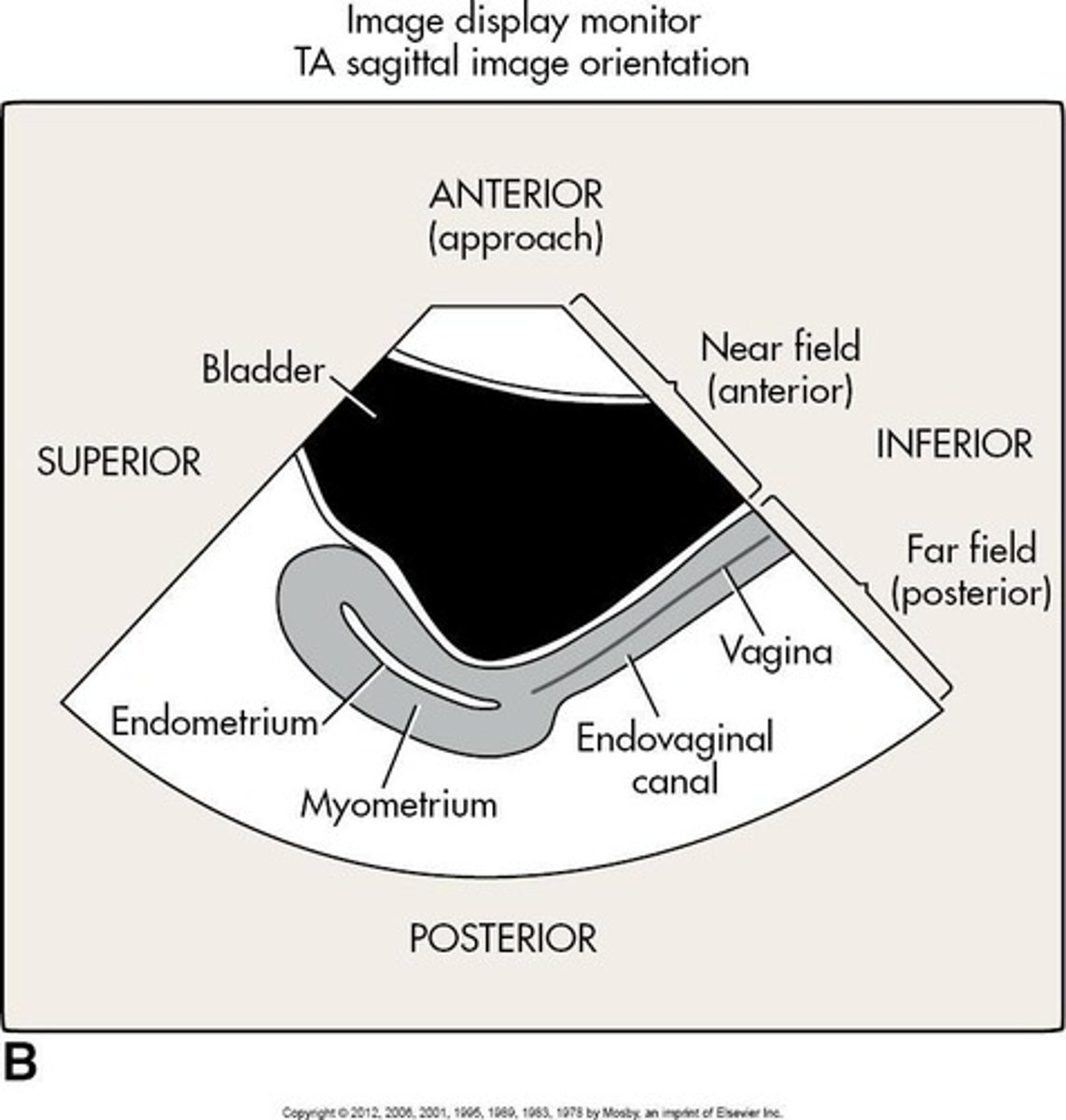
Transabdominal Pelvic Ultrasound
Ultrasound technique using abdominal approach.
Transverse View
Imaging bladder, uterus, and ovaries in cross-section.
Low Transverse View
Visualizes distended bladder, vagina, cervix.
Mid Transverse View
Shows bladder, uterus body, endometrium, and ovaries.
High Transverse View
Focuses on fundus of uterus and lateral ovaries.
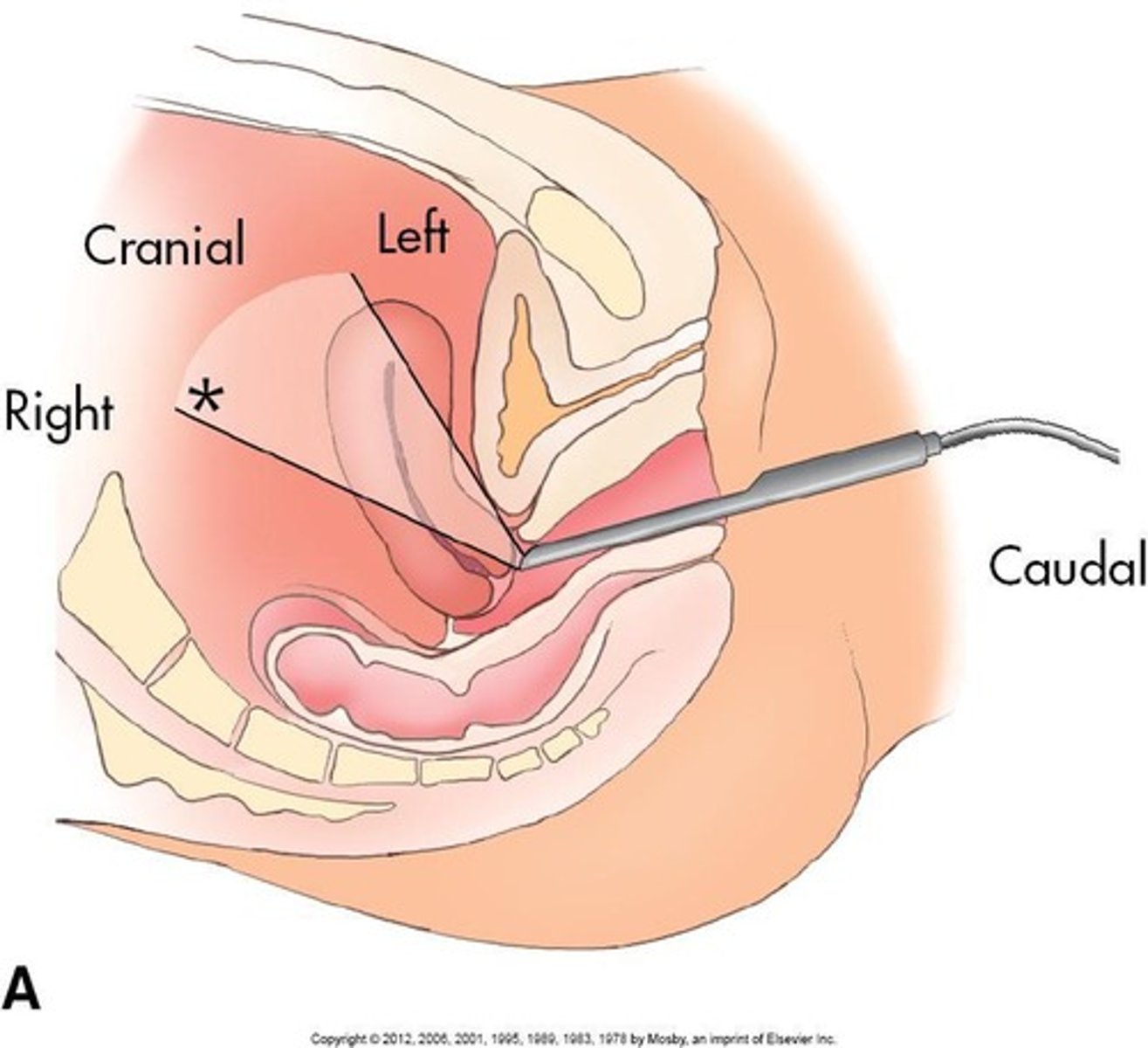
Transvaginal Sonography
Ultrasound technique using vaginal probe.
Patient Instructions
Guidelines provided to patients before procedure.
Probe Preparation
Steps to ready ultrasound probe for use.
Examination Technique
Methodology for conducting the ultrasound examination.

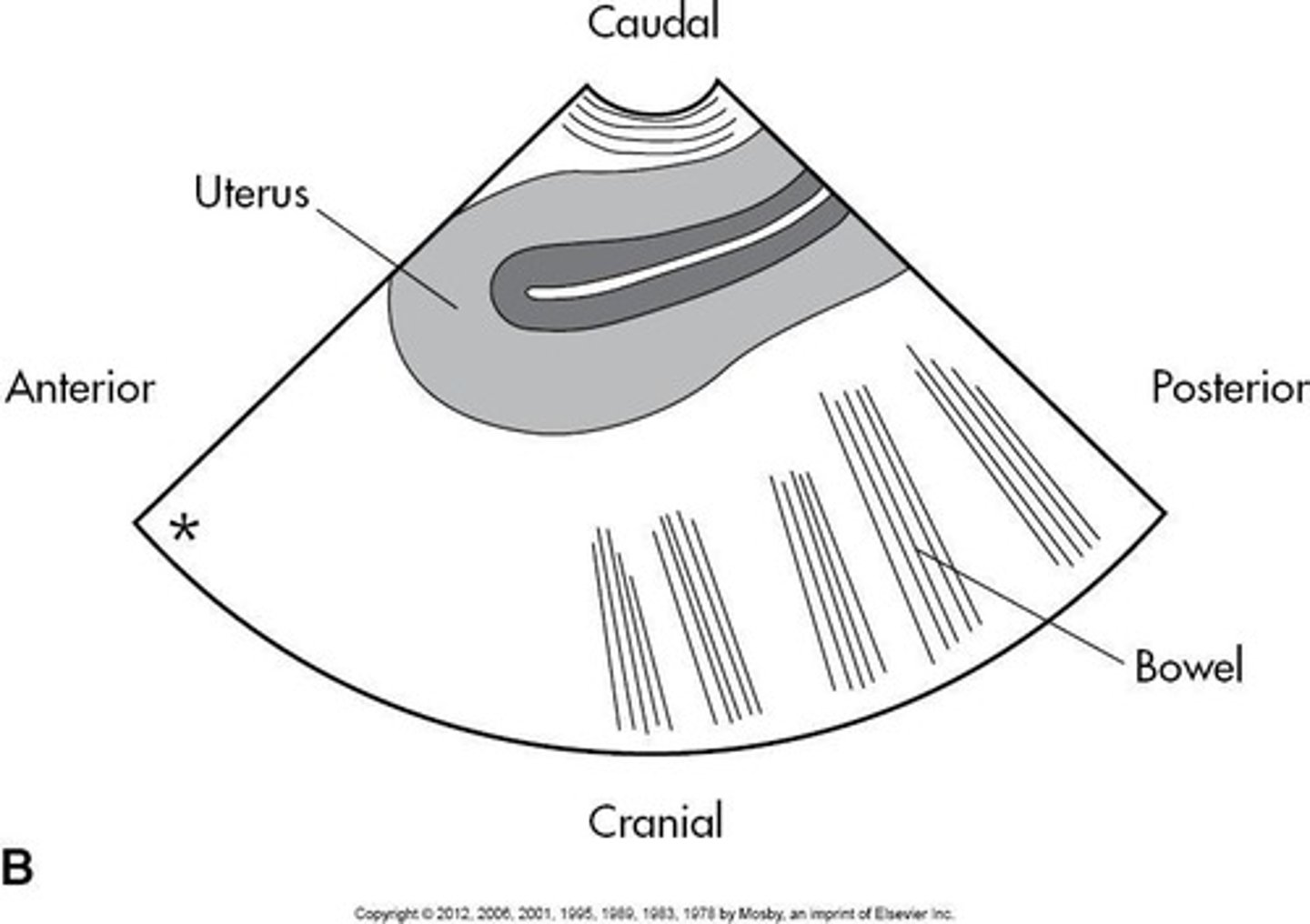
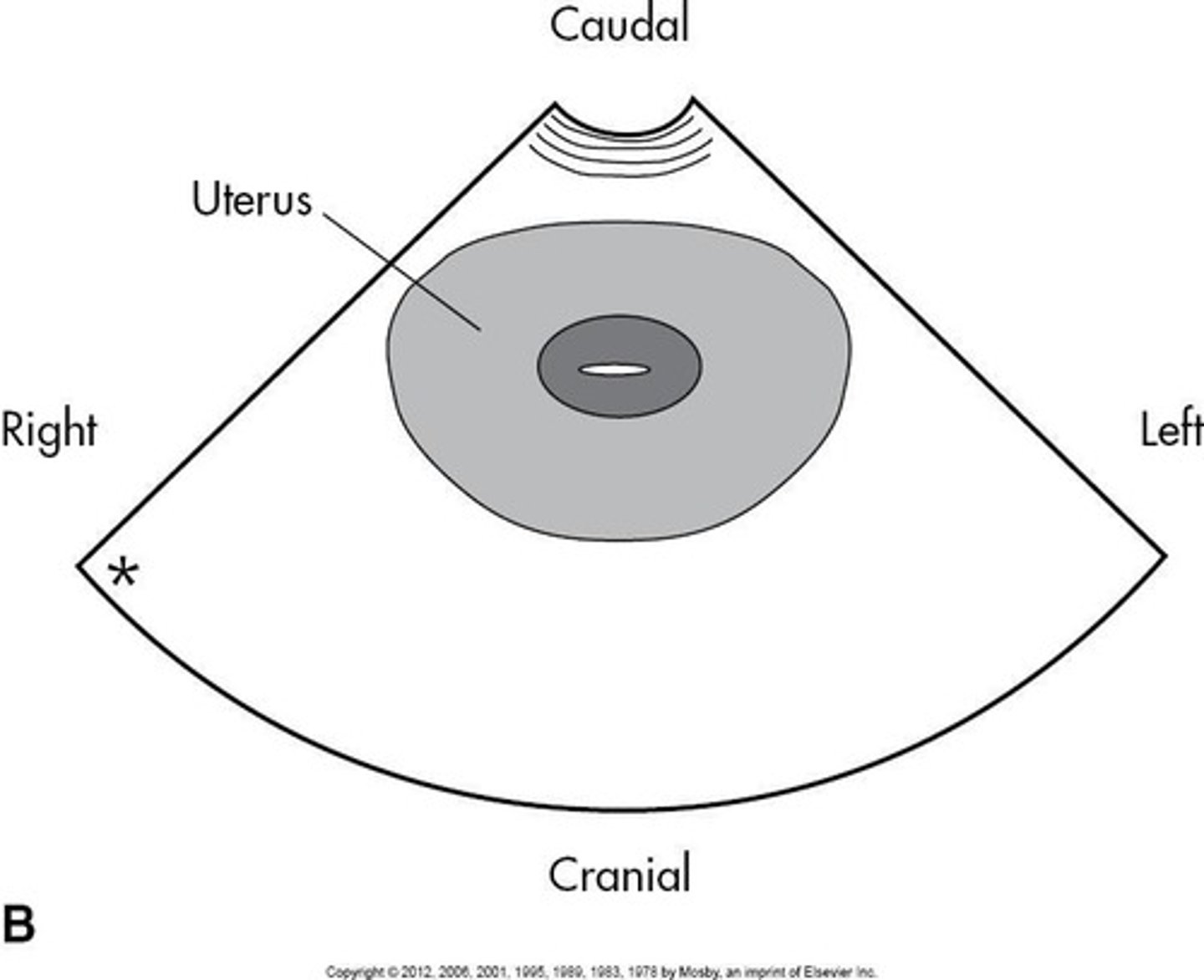
Scan Orientation
Positioning of ultrasound images for accurate assessment.
Scanning Planes
Different planes used for imaging pelvic structures.
Sagittal Plane
Vertical plane dividing body into left and right.
Coronal Plane
Vertical plane dividing body into anterior and posterior.
Scan Protocol
Standardized procedure for conducting ultrasound exams.
Sagittal Protocol for Uterus
Images cervix to fundus; measures long axis.
Coronal Protocol for Uterus
Images uterine fundus, body, and cervix.
Sagittal Protocol for Ovaries
Images ovaries; measures long axis and follicles.
Coronal Protocol for Ovaries
Images ovaries; measures width and depth.
Free Fluid Assessment
Checking for fluid around uterine cavity.
Color Imaging
Technique to differentiate vascular structures from ovaries.
Disinfectant Technique
Method to sanitize equipment before procedures.
Bony Pelvis
Sacrum appears as a bright line sonographically.
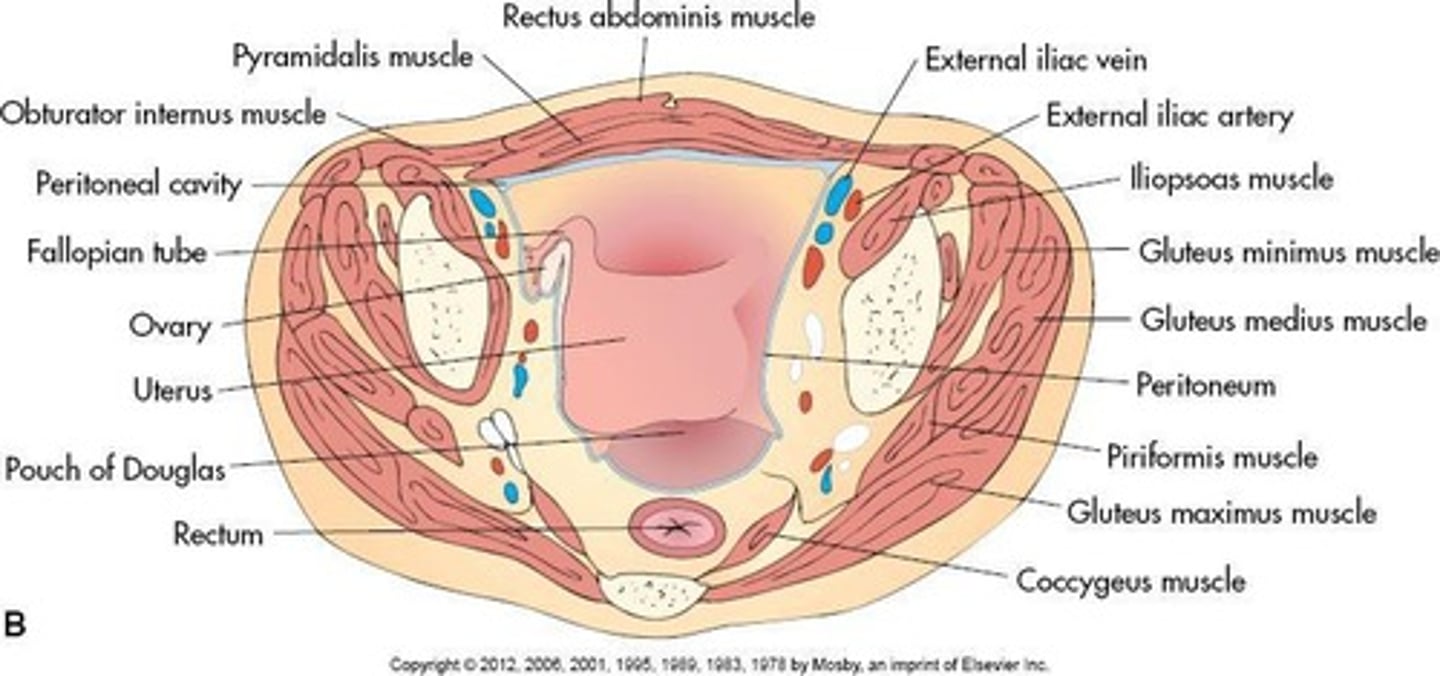
Rectus Abdominis Muscles
Paired muscles inserting on pubic rami.
Hypoechoic Structures
Muscles appear darker on ultrasound images.
Rectus Sheath
Bright linear echogenic reflector separating muscles.
Obturator Internus Muscles
Located at posterior lateral corners of bladder.
Obturator Fascia
Surrounds obturator internus muscle in pelvis.
Levator Ani Muscle
Hammock-shaped muscle visualized in transverse plane.
Coccygeus Muscle
Located deep and cranially in pelvic cavity.
Piriformis Muscle
Posterior muscle not routinely visualized sonographically.
Iliopsoas Muscle
Combination of iliacus and psoas major muscles.
S/D Ratio
Peak systolic to end diastolic ratio in vascularity.
Pourcelot Resistive Index (RI)
Calculated as (A − B)/A for vascular assessment.
Pulsatility Index (PI)
Calculated as (A − B)/mean for blood flow.
Uterine Muscle Layers
Three layers: serosa, myometrium, and endometrium.
Myometrium
Middle layer with homogeneous echotexture and smooth borders.
Endometrium
Inner layer, thin and relatively hypovascular.
Subendometrial Halo
Hypoechoic area surrounding echogenic endometrial stripe.
Arcuate Vessels
Normal vessels in periphery, not pathological.
Radial Arteries
Branches supplying deeper layers of uterus.
Straight and Spiral Arteries
Arise from radial arteries before endometrium.
Uterus
Female reproductive organ for fetal development.
Cervix
Narrow lower part of the uterus.
Isthmus
Narrow section between uterus body and cervix.
Cervical inclusion cysts
Also known as nabothian cysts.
Nabothian cysts
Anechoic cysts near endocervical canal.
Echogenicity
Tissue's ability to reflect ultrasound waves.
Anechoic
Absence of internal echoes on ultrasound.
Acoustic enhancement
Increased echogenicity posterior to fluid-filled structures.
Anteverted uterus
Uterus tilted forward towards the bladder.
Retroflexed uterus
Uterus tilted backward towards the spine.
Flexion
Uterine body axis relative to cervix.
Version
Cervix axis relative to vagina.
Endometrium
Inner lining of the uterus.
Functional layer
Superficial layer of the endometrium.
Basal layer
Deep layer of the endometrium.
Menstrual phase
Days 1 to 4 of the menstrual cycle.
Hypoechoic
Lower echogenicity compared to surrounding tissues.
Proliferative phase
Days 5 to 14 of the menstrual cycle.
Secretory phase
Days 15 to 28 of the menstrual cycle.
Three-line sign
Ultrasound appearance of endometrial layers.
Endometrial thickness
Varies from 6 mm to 10 mm pre-ovulation.
Posterior enhancement
Increased echogenicity due to vascularity.
Secretory Phase
Phase of menstrual cycle with endometrial changes.
Endometrial Complex Measurement
Normal thickness is 7 to 14 mm.
Endometrial Thickness Measurement
Measured from basalis to myometrium interface.
Fallopian Tubes Identification
Difficult unless surrounded or filled with fluid.
Ovaries Mobility
Ovaries move based on bladder volume and pregnancy.
Ovarian Shape
Elliptical, with long axis oriented vertically.
Transvaginal Scanning
Superior for assessing ovarian texture.
Ovary Location
Lateral to uterus, medial to internal iliac vessels.
Ovary Localization
Easiest in coronal plane lateral to cornua.
Ovary Position Variability
Can be above uterus or in rectouterine area.
Normal Ovary Appearance
Ovoid, medium-level echogenic structure.
Follicular Cysts
May appear peripherally in ovarian cortex.
Ovary Measurement
Measured in sagittal and transverse planes.
Ovary Volume Calculation
Volume = 0.523 × length × thickness × width.
Rectouterine Recess
Most posterior peritoneal cavity reflection.