Safety & TeamSTEPPS - NUR 337
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
46 Terms
True or false: teamwork cannot occur in the absence of a clearly defined team
TRUE
What is a critical part of TeamSTEPPS for implementation planning?
understanding a team’s structure and how multiple teams interact
Definition of a team
Two or more people who interact dynamically, interdependently, and adaptively toward a common and valued goal, have specific roles or functions, and have a time-limited membership.
True or false: teams are only considered in-person, permanent positions.
FALSE - teams can be in-person or virtual, temporary or permanent, and frequently changing due to staff scheduling.
True or false: patients are members of the core team.
TRUE → a family caregiver also may be!
What are some strategies for involving patients and family caregivers in teams?
include the pts in bedside rounds
conduct handoffs at the pts bedside
provide pts and family caregivers with tools for communicating with their care team (email, phone #, etc)
involve pts on key committees (ex: stroke survivors)
actively encourage pt and family caregiver participation
How can we foster pt and family caregiver involvement?
embrace pts and family as separate, valuable, and contributing partners
listen and ask for feedback
assess preference regarding involvement
ask about concerns
speak in layman terms
allow them time
treat pts and family as distinct
help them have access to relevant info on a pt portal
How can pts and family caregivers function effectively in teams?
provide accurate info
collaborating to create a care plan they will follow
asking questions + voicing concerns about their care
monitoring + reporting changes in the pts condition
coordinating & communicating with other family
encouraging + showing appreciation to other team members
Who all is included in the multi-team system for pt care?
core team + pt
contingency teams
coordinating teams
ancillary + support services
administration
Core team
A group of care providers who work interdependently to manage a set of assigned patients from point of assessment to disposition.
True or false: core team members have the closest contact with the pt
TRUE
Contingency team
a time-limited team formed for emergent or specific events and composed of members from various teams.
ex: rapid response
Ancillary Services
Provide direct, task-specific, time-limited care to patients.
ex: pt or dieticians
Support Services
Provide indirect service-focused tasks that help facilitate the optimal healthcare experience for pts and their families.
Role of Administration
establish + communicate vision
develop policies and set expectations for staff related to teamwork
support & encourage staff during implementation + culture change
hold teams accountable for team performance
define the culture of the organization
Leadership
ensures the patient remains the focus for all team decisions
holds a teamwork system together
ensures a plan is conveyed, reviewed, and updated
is facilitated by communicating, continuously monitoring the situation, and fostering an environment of mutual support
Designated (Formal) Team Leader
The person assigned to lead and organize a team, establish clear goals, and facilitate open communication + teamwork among team members
ex: charge nurse
Situational Team Leader
Any team member with the skills to manage the situation at hand
ex: BLS-trained individual helps heart attack pt
What do effective team leaders do?
ensure the pts needs and preferences are understood and prioritized
define, assign, share, monitor, & modify a plan
review the team’s performance
establish “rules of engagement”
manage + allocate resources effectively (prioritize telemetry monitors)
provide feedback regarding assigned responsibilities + progress toward the goal
facilitate information sharing
encourage team members to assist one another
facilitate conflict resolution (ex: crucial conversations)
model effective teamwork
What should team members consider when developing a plan?
Patient: What does the pt need and how can the team best provide it?
Time: How much time is available to complete all the necessary tasks and activities?
People: Do available staff have the necessary knowledge and skills to perform their roles?
Equipment: Is the needed equipment available and working?
Information: Has all the needed information been collected and reviewed?
What must be done to properly assign tasks & responsibilities?
determine the tasks + roles to be assigned
determine which roles must be filled and allocate tasks appropriately
communicate clear expectations of what team members need to do
request feedback
True or false: a team brief is an effective strategy for sharing the plan
TRUE
ex: pt has an MI in the community. ER nurse will pre-brief everyone and gather a team for the incoming pt.
What is the purpose of briefs?
form the team
designate team roles + responsibilities
establish climate + goals
engage team in short and long-term planning
What is covered in the brief checklist tool?
who is on the team?
do all members understand and agree upon goals?
are roles and responsibilities understood?
what is our plan of care?
what is provider availability throughout the shift?
how is workload shared among team members?
what resources are available?
When is a TeamSTEPPS huddle called?
DURING THE EVENT!
when we monitor and modify the plan to re-establish goals
What problem solving occurs during a TeamSTEPPS huddle?
ad hoc “touch base” meeting to regain situational awareness
discuss critical issues
anticipate outcomes + likely contingencies
assign resources
express concerns
elicit input + answer pt questions when appropriate
When does a TeamSTEPPS debrief occur?
following the event!
review the team’s performance
How do debriefs foster process improvement?
brief, informal information exchange + feedback sessions
occur after an event or shift
designed to improve teamwork skills
designed to improve outcomes:
accurate recount of key events
analysis of why the event occurred
discussion of lessons learned + reinforcement of success
revised plan to incorporate lessons learned
What is part of the debrief checklist?
was communication clear?
were roles and responsibilities understood?
was situational awareness maintained?
was workload distribution equitable?
was task assistance requested or offered?
were errors made or avoided?
were resources available?
what went well?
what is one thing that should improve?
How do effective leaders facilitate conflict resolution?
facilitate conflict resolution to avoid compromising patient safety + quality of care
do not allow interpersonal or irrelevant issues to negatively affect the team
help team members master conflict resolution techniques
How do effective leaders cultivate desired team behaviors and skills?
open information sharing
role modeling + effective cuing of team members to use prescribed teamwork behaviors & skills
constructive and timely feedback
facilitation of briefs, huddles, debriefs, and conflict resolution
mitigation of conflict within the team
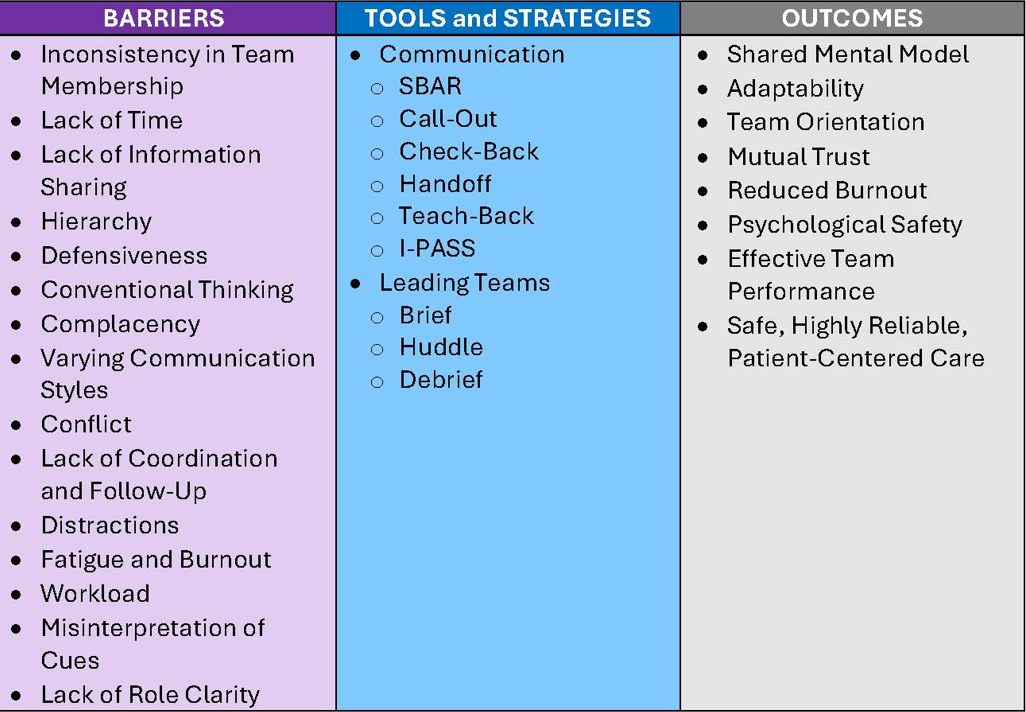
Tools & Team Strategies Summary
True or false: hand hygiene is the number 1 way that we can prevent the spread of disease
TRUE
True or false: we wear gloves at all times around the pt
FALSE - only when we may come in contact with bodily fluids
True or false: in standard precautions, you may use additional PPE if performing certain procedures to avoid bodily fluids
TRUE → gown/face shield during NG tube application to avoid emesis
True or false: all patients in the hospital at baseline are on standard precautions
TRUE
When do we need to wash our hands during standard precautions?
when entering the room
as needed in the room
when leaving the room
Contact precautions
Where spores can attach to the clothes you are wearing.
PPE = gown, gloves
Ex = C-Diff
Droplet Precautions
PPE = surgical mask
Ex = meningitis, influenza, COVID-19
True or false: influenza & COVID-19 can become airborne during some procedures
TRUE
Airborne Precautions
Finer particles that can remain airborne for a longer period of time
PPE = N95 surgical mask
Ex = TB
Environmental Awareness for Nurses
across room assessment
bed in lowest position + locked
non-skid footwear
room free of clutter
top 2 side rails up (NOT bottom 2)
good lighting
call light + tray table in reach
bed/chair alarm on if necessary
O2 and suction available and working
infection control risks
get report from RN + check white board
ANY SAFETY PRECAUTIONS?
Identify if the pt is NPO
Any limb restrictions? (mastectomy)!
Trust your gut!
What can a pt be at risk for?
aspiration
falls
injuries
seizures
suicide/self-harm (1:1 sitter)
PI (nutrition → protein)
What occurs during a transition to an inpatient unit from the emergency department?
systems for communication vary
receiving RN’s responsibilities → understand patho behind admitting diagnosis, review assessment for appropriate admission to unit, clarify unclear issues, welcome + communicate with pt
begin admission procedures → safety screening, orientation to room, assessment of IV access, assessment, history
What do we use to determine risk for injury with fall?
ABCS -
A = Age > 85
B = Bone health (Fx risk or history → osteoporosis, bone mets, steroid use)
C = Coagulation (coagulopathy or on anticoagulant meds)
S = Surgery (within 14 days)
Where do failures occur with risk for injury with falls?
failure to communicate changes in assessments
failure to implement and document prevention interventions
unclear handoffs
insufficient safety instructions
pt or family confusion from nurse teaching
assuming it is only important to teach the pt
education that fails to be individualized