PN exam 2: sleep disorders
1/93
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
94 Terms
What are disorders of sleep in children and adolescents?
Common conditions affecting children and adolescents; most are benign and remit over time but can highly disrupt family life.
What is sleep an underappreciated contributor to?
Health and behavior.
What does evaluation of sleep disorders in children require?
Interviewing caregivers, the child, and reviewing sleep diaries.
What is true about diagnostic tests for sleep problems in children?
They are available but difficult to access and not all that useful.
How can most sleep problems in children be improved?
With improved sleep hygiene.
Medical causes of sleep problems are ___ but benefit from ___.
Medical causes of sleep problems are rare but benefit from treatment.
What is SIDS?
Sudden Infant Death Syndrome — occurs in very young infants.
What age group is affected by obstructive sleep apnea?
Older children.
What are night terrors and when are they common?
A common parasomnia occurring in ages 2–4 years.
What are nightmares and when do they occur most often?
Frightening dreams, common in ages 3–5 years
When does sleep walking typically begin?
Between ages 4 and 8 years.
What is restless legs syndrome in children?
Night-time leg discomfort in about 1% of children.
How common is enuresis?
10% of normal 6-year-olds; 1% of 15-year-olds.
Who does delayed sleep-phase syndrome affect?
A common condition in teens.
What are the key features of narcolepsy?
Cataplexy (abrupt falls)
Hypnogogic hallucinations
Sleep paralysis
Daytime somnolence(excessive sleepiness).
How long are normal sleep cycles in children?
Cycles every 60–90 minutes
What are the stages of non-rapid eye movement (NREM) sleep?
N1–3; progressively deeper stages of sleep — N3 is the deepest.
What are characteristics of rapid eye movement (REM) sleep?
Decreased EEG amplitude, muscle atonia, autonomic variability, and rapid eye movements.
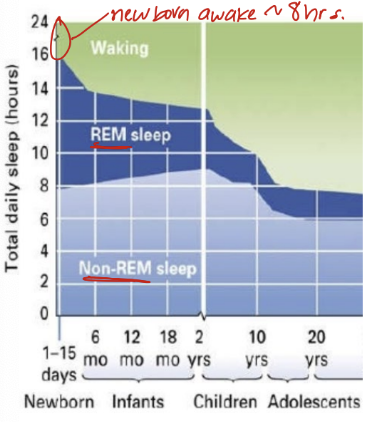
Describe proportion of REM to non REM sleep by age.
Equal no matter age, but actual # of hours between non-REM, REM, and waking is different
CASE:
A 2-month-old boy presents to ED via ambulance in full arrest. On that day, his mother had left him with a babysitter, who put him down to sleep after feeding. When she checked 30 minutes later, she found him pale, not breathing, and limp. She called 911 and began CPR. En route, patient was intubated, an intraosseous line was placed and epinephrine administered.
Past Medical History: The patient was born at term with birth weight of 7 lbs 7 oz. He was discharged home from hospital on day of life 2. Since then he had been well.
Exam: Vital Signs T 95 F, without CPR apneic and pulseless. The infant is mottled without spontaneous movements. Pupils are fixed and dilated.
Resuscitation is continued in ED but there is no response. He is pronounced dead after 30 minutes
SIDS
(if it was abuse, would need 1. encephalopathy 2. R Subarachnoid Hematoma 3. Retinal Hemorrhage)
What is SIDS?
The unexpected and silent death of a sleeping infant who seemed healthy
SIDS is the leading cause of death among what age group?
Babies 1 month to 1 year old
About how many babies die of SIDS each year in the U.S.?
About 4,000 babies yearly (≈1 per 1,000 births)
What are the ABC’s of Safe Sleep?
A – Alone: Not with people, pillows, or blankets
B – on my Back: Not on the stomach or side
C – in my Crib: Not on an adult bed, sofa, or soft surface
What are the three main factors thought to cause SIDS?
Vulnerable infant
Critical developmental period
Outside stressors
What does it mean when a baby is a vulnerable infant?
The baby has an underlying brain defect or abnormality that affects control of breathing, heart rate, or arousal during sleep.
What are examples of outside stressors that increase SIDS risk?
Sleeping on the stomach, overheating, secondhand smoke, or a upper respiratory infection.
Why does SIDS occur specifically in infants?
During an infant's first 6 months of life, changes in homeostatic controls occur, including breathing
t/f SIDS is most likely to occur when a vulnerable infant is in a critical developmental period and exposed to an outside stressor.
True
CASE:
Devontay is a 9-year-old boy, who presents for his yearly check-up at your office. His mom comments that he snores during sleep, and sometimes she hears him gasp
He has started taking naps during the day, has poor concentration in school; his grades have dropped. Mom is concerned about his sleep and asks if you know what to do next
(2 below are correct)
1) Could be ADD
2) Can’t be ADD – we did that last month
3) Maybe he has a sleep disorder. Did you say he snores?
4) IDK. I fell asleep during this lecture
5) He needs a polysomnogram
6) He needs a brain MRI
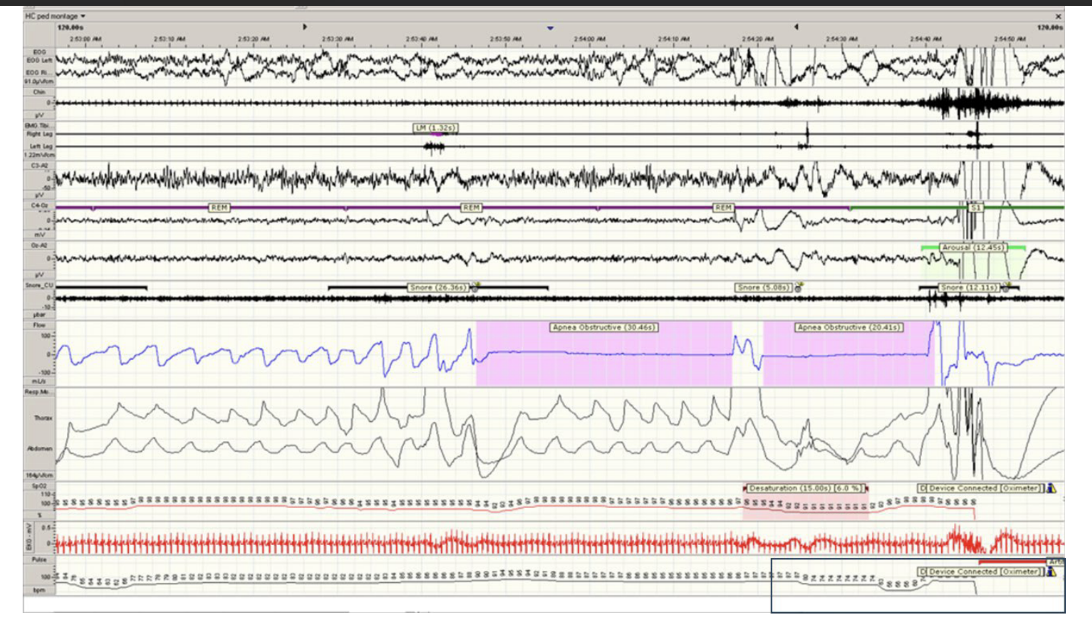
3) Maybe he has a sleep disorder. Did you say he snores?
5) He needs a polysomnogram
What does Devontay have?
OSA:
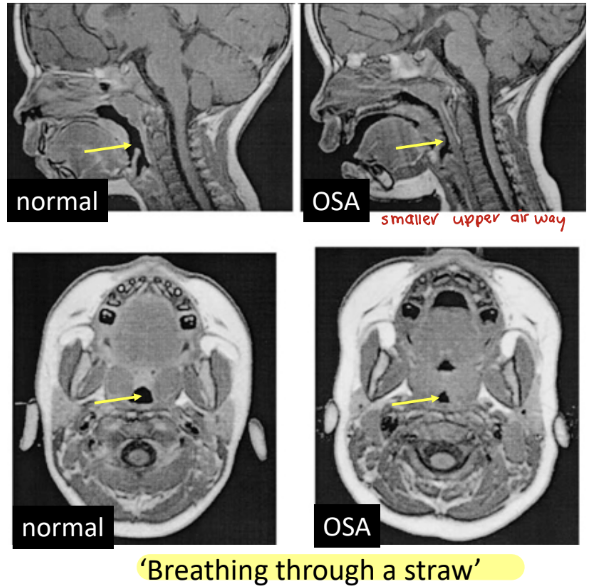
What happens in obstructive sleep apnea (OSA)?
Airway becomes blocked during sleep.
How common is OSA in kids?
OSA is common. Affects about 3% of kids.
What are symptoms of OSA in children?
Snoring, with snorts or gasps, and night-time arousals, daytime sleepiness, headache, hyperactivity, impaired school performance
What is the diagnostic test for OSA?
Begin with a diagnostic polysomnogram.
What are the main treatments for OSA in children?
Adenectomy (removal of adenoids/tonsils) or weight loss if overweight
What treatment is used for severe OSA?
Night-time continuous positive airway pressure (CPAP)
What does CPAP do?
It pushes air continuously into the airway through a mask to keep it open during sleep
Does CPAP deliver oxygen?
No — it provides air pressure, not oxygen
Treat OSA by treating ______.
Upper airawy obstruction. Remove tissue to increase airway size(upper central airway extraction), but if there’s muscle weakness pt’s tissue removal won’t help
CASE: A healthy 4-year-old boy awakens 90 minutes after falling asleep. His parents find him screaming, sweaty, and standing up wide-eyed in bed. After several minutes he calms, parents put him back in bed, and he sleeps the rest of the night.
He wakes up in his usual good mood and does not remember the episode. They occur 3 or 4 times a week.
DX?
DX: Night terror
90 minutes is the same length as average sleep cycle
What are night terrors?
Episodes where a child appears awake and frightened but is actually still asleep.
How long do night terror episodes usually last?
Several minutes, after which the child calms down.
Is the child easy to wake up during a night terror?
No — they are difficult to wake and may be disoriented or confused if awakened.
Does the child remember the event the next morning?
No, unlike nightmares, they do not recall the incident or any dreams.
During which type and time of sleep do night terrors occur?
Non REM sleep, typically between midnight and 2 AM.
What are common triggers of night terrors?
Change in sleep schedule
Extreme tiredness or lack of sleep
Stress
CASE
Since junior high school Chris’ usual sleep hours got progressively later, and it became extremely difficult to wake him up for school. He slept during morning classes and his grades deteriorated
He graduated from high school, but his achievements were lower than his potential. He managed to complete undergraduate and graduate studies by taking afternoon / evening courses. He is now a university professor, thus able to sleep between 5 AM and 1 PM
Over the years he tried sleeping pills, anxiety medications, and psychotherapy, which didn't help
dx?
Chris has Delayed Sleep Phase disorder
Case
Since junior high school Chris’ usual sleep hours got progressively later, and it became extremely difficult to wake him up for school. He slept during morning classes and his grades deteriorated
He graduated from high school, but his achievements were lower than his potential. He managed to complete undergraduate and graduate studies by taking afternoon / evening courses. He is now a university professor, thus able to sleep between 5 AM and 1 PM
Over the years he tried sleeping pills, anxiety medications, and psychotherapy, which didn't help
dx?
Delayed Sleep Phase disorder
What causes circadian rhythm dyssomnias?
Inappropriate timing of sleep due to melatonin release delay
Inappropriate timing of sleep due to melatonin release delay causes what?
circadian rhythm dyssomnias
What is the specific condition where sleep and wake times are shifted later than normal?
Delayed Sleep Phase Disorder (DSPD
What are the main symptoms of Delayed Sleep Phase Disorder?
Insomnia or excessive sleepiness
Inability to fall asleep at the desired time
Inability to wake up at the desired time
How long must this delayed sleep pattern persist to diagnose DSPD?
For 3–6 months
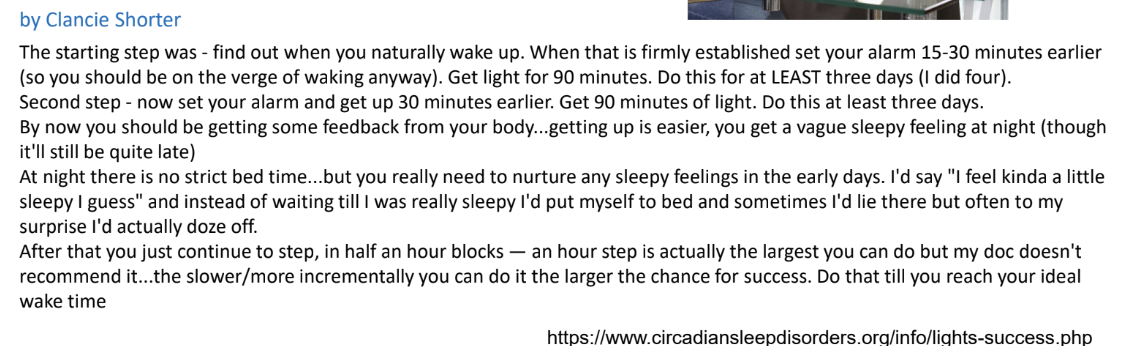
What is the main treatment for Delayed Sleep Phase Disorder (DSPD)?
Bright Light Therapy
How does Bright Light Therapy help treat DSPD?
It gradually resets the biological clock to match the normal daytime schedule.
When should Bright Light Therapy be used for DSPD?
In the morning, shortly after waking up, to signal the body that it’s daytime.
Case - Amanda’s story ‘When I was a sophomore in high school, I started passing out up to 5 times a day. I would be in the middle of a conversation, or walking to the bathroom, and just fall over, and be unknown to the world for about 3 minutes.
Eventually, I had to be taken out of school. Up until then, I had been an honors student and on the JV softball team. My life was in shambles. My mother was a complete wreck and wouldn’t let me out of her sight, or even out of the house. When I went to the bathroom I had to keep the door open. When I showered my mom sat on the toilet. Since I could never go out, my friends stopped talking to me.
My mother always knew I had a problem with sleep (when I was little I would sit up in my crib playing with my toys until about 2 in the morning). When I could walk, I would go out into the living room and watch TV in the middle of the night without my mother’s knowledge. She would even have to wake me up on Christmas morning’
dx?
Narcolepsy
What causes narcolepsy?
Autoimmune attack on orexin receptors, which normally stabilize sleep–wake transitions
What is the peak incidence of narcolepsy?
15–25 years of age
What are the four key clinical features (tetrad) of narcolepsy?
1) Sleep attacks: irresistible urge to sleep for 5-20 minutes
2) Cataplexy (intrusion of REM atonia while awake): abrupt total loss of body muscle tone triggered by strong emotions such as anger (the patient is awake, but unable to move)
3) Sleep paralysis (REM atonia) at sleep-wake transition when patient briefly cannot move
4) Hypnagogic hallucinations: dreams continue into waking as illusions or hallucinations
Whats the normal vs narcolepsy order of turning off paralysis and waking up?
normal: 1. turn off paralysis 2. wake up
narcolepsy: 1. wake up 2. turn off paralysis
Main symptom of narcolepsy
daytime sleepiness
emotionally triggered loss of voluntary muscle tone
hypnagonic hallucinations
sleep paralysis
For narcolepsy diagnosis ___ is needed.
PSG (polysomnography)
Alongside PSG what can be used to diagnose narcolepsy?
Multiple Sleep Latency Test
What is Multiple Sleep Latency Test? What is it’s critical measurement?
5 successive naps
Critical measurement: time to REM Sleep
**go to slide 25 to look at pic (unable to upload rn)
Narcolepsy treatment is mostly ______.
symptomatic
For narcolepsy treatment, what is recommended?
Regular sleeping and rising times are recommended with scheduled naps 2-3 times a day
For narcolepsy ______ may help excessive daytime sleepiness
stimulants
What is used to treat cataplexy?
SSRI antidepressants
What is most common REM parasomnia?
Nightmares
Nightmares, often that your safety is in danger, occur in ___.
REM sleep
What is Nightmare disorder (dream anxiety disorder?
frequent nightmares
Nightmare disorder (dream anxiety disorder)’s onset is what ages?
3-6 years of age
For pt’s w/Nightmare disorder what percent have nightmares severe enough to worry their parents?
50%
How are nightmares different from sleep terrors?
Unlike sleep terrors, a child with nightmares can recall the event in the morning
Treatment for nightmares?
Treatment is reassurance during the incident and reducing daytime stress
______ is a dramatic parasomnia.
Sleepwalking is a dramatic parasomnia.
Sleepwalking affects ____% of children, usually between ages of ____.
Sleepwalking is a dramatic parasomnia in 10% of children, usually between ages 4-8 years
Symptoms of sleepwalking:
Sitting up in bed, sleep talking, walking, etc., all while asleepn
Do sleepwalkers remember their incidents?
Sleepwalkers have no memory of the incident.
What does sleepwalking look like and how long does it last?
Although their eyes are open, their expression is glazed.Typically last a few minutes
PSG in a child with sleep walking would show arousal from ____.
deep sleep (stage N3)
Management for sleepwalking:
door alarms, child-proof locks
_____: Urge to move the legs, usually accompanied by unpleasant sensations
Restless leg syndrom
What is apathesia?
urge to move
apathesia
urge to move
Restless leg syndrome:
Urge to move the legs and accompanying unpleasant sensations begin during periods of rest such as lying down or sitting
Relieved by ____
Worse in the ____
Urge to move the legs and accompanying unpleasant sensations begin during periods of rest such as lying down or sitting
Relieved by movement
Worse in the evening or night
Restless leg syndrome causes:
• Low serum iron level
• A genetic link in some cases
• Drugs may cause RLS as a side effect
• Unknown
What is enuresis?
Bed wetting
Enuresis can occur _____, _____ of sleep stage or depth of sleep
Enuresis can occur day or night, independent of sleep stage or depth of sleep
T/F Punishing a child for wetting nor ignoring is not helpful
Tru
Treatments for Enuresis:
Parents may reward a child for nights without bedwetting, and praise efforts to try
A bedwetting alarm can alert a child who begins to urinate to go to the bathroom
Preferred medication for treating children with enuresis
Desmopression