CH50: The Patient with a Neurodevelopmental Disorder
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
46 Terms
Learning objectives
• Define and describe neurodevelopmental disorders
• Give examples of the characteristics, oral findings, and health problems significant for providing dental hygiene care for patients with neurodevelopment disorders, including intellectual disabilities, Down syndrome, and autism spectrum disorder
• Recognize adaptations necessary for providing dental hygiene care for a patient with a neurodevelopmental disorder
Overview
Neurodevelopmental disorders are a diverse group of chronic and potentially severe conditions that:
• Typically manifest in the early developmental period
• Usually last throughout a person’s lifetime
• Lead to intellectual, social, and/or physical impairments
• Create problems with major life activities such as language, mobility, learning, self-help, and independent living
Down syndrome (DS) and autism spectrum disorder (ASD) are two major categories of patients with neurodevelopmental disorders that dental professionals encounter in standard dental settings
Major Diagnostic Categories of Neurodevelopmental disorders
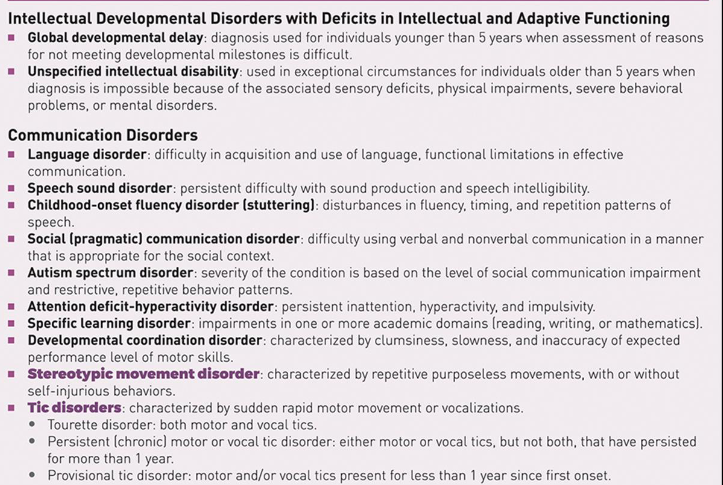
Intellectual disability
When limitations in your mental abilities affect intelligence, learning and everyday life skills.
Characterized by
Intelligence-related symptoms
Delayed or slowed learning (school or real-life experiences), difficulties with reasoning and logic, problems with judgment and critical thinking, distractibility and difficulty focusing
Limitations in adaptive behavior
slower learning of self-care activities, slower social development, need help managing time, money, medications, etc.
Symptoms may begin at birth, but include any intellectual disability before the age of 18
Disabilities related to IDs are a symptom in well over 200 different conditions
Depending on the severity, people may experience minor effects but still live independent lives while others may have severe effects and need lifelong assistance and support
Causes of ID
Prebirth
•Genetics and inheritance
•Infections
•Teratogens
During Birth
•Lack of oxygen (hypoxia)
•Premature birth
•Brain injury during birth
Early Childhood
•Injuries or accidents
•Toxic exposures (lead, mercury)
•Infections that spread to the nervous system
•Tumors or growths in brain
•Medical conditions (seizures/epilepsy)
Models of human functioning and disability
Diagnosis based on 3 criteria
◦ Intelligence testing (problem solving, abstract thinking, judgment, academic learning abilities, ability to plan ahead, etc.)
◦ Assessment of adaptive behaviors
◦ Age of onset
Assessment of functioning: establish baseline information for behavioral, social, and functional problems
Assessment of support needs
Planning and developing individual supports
Assessment of personal outcomes including quality of life
Supportive Services
◦ Avoid preventable causes of ID (e.g. fetal alcohol syndrome (FAS)) and limit negative effects of conditions resulting in ID
◦ Early intervention to support the development and growth of the individual as well as the family
◦ Individualized education plans to support development of autonomy, self-determination, and self-advocacy
◦ Positive behavioral supports to improve quality of life and reduce negative behaviors
◦ Identify and provide individual supports like assistive technology and community participation
◦ Provide long-term family and individual support to help individuals with ID transition to community living
Dental care is one of the supportive services needed for the individual with ID to ensure
◦ Freedom from oral discomfort and pain
◦ Attain and maintain oral health
◦ Improved quality of life
Classification of intellectual disabilities
Multiple steps-involves assessing intelligence (IQ) and adaptive behavior capabilities. Generally, can’t identify severity until old enough for IQ testing and full adaptive assessment.
◦ Mild
◦ Moderate
◦ Severe
◦ Profound
◦ Provisional-ID exists, but individual is infant or child <4 years old so assessment is not possible
◦ Unspecified-used when standardized tests cannot be performed due to lack of cooperation, severe impairment, or infancy
Mild intellectual disability
◦ Average mental age of between 9-12 years
◦ Disability may interfere with learning or complex tasks, but individual can often work around these issues
◦ Often work and live independently
◦ About 85% of people with ID are at this level
Moderate Intellectual Disability
◦ Average mental age of 6-9 years
◦ Ability to communicate using simple language
◦ Basic capacity for language and academic skills-about elementary school level
◦ Can live independently to some degree but will need help and support, such as a group home
Severe Intellectual Disability
◦ Average mental age of 3-6 years
◦ Language/communication is limited to single words, phrases and/or gestures
◦ Can develop basic self-care skills with extensive training
◦ Benefit from daily care and support with activities and daily life
Profound intellectual disability
◦ Average mental age of 3 years and below
◦ Severe limitation in self-care, continence, communications, and mobility
◦ Usually communicate nonverbally, understanding of some gestures and emotional cues
◦ Benefit from 24/7 medical care and support for all activities and aspects of life
◦ Unable to live independently
Management and treatment
No way to cure or treat ID directly, but treatments that focus on helping with adaptive behaviors and life skills can improve the individual’s good quality of life
◦ Education and support interventions
◦ Behavioral support and interventions
◦ Vocational training
◦ Education for the family of a person with an ID
◦ Various medications can help with some symptoms
◦ Community support
Components of support
Early diagnosis is essential
Professional interventions
Special education and psychosocial support
Inclusive environments
Support individuals’ growth and development
Supported living, work, and inclusive education
Support strategies
Assistive devices and technology
Reasonable accommodations
Build on personal strengths
Treatment with dignity and respect
General characteristics
Physical
◦ Many do not have unusual physical characteristics
◦ Delays in physical and motor functioning such as walking, running, and jumping
Oral Findings
◦ Higher levels of dental biofilm
◦ Gingivitis more common than in those without ID, more than ½ adults with ID have more severe periodontal disease
◦ Dental caries
◦ Oral development malformations (e.g. macroglossia, short and narrow palate, delayed tooth development)
◦ Oral habits of clenching, bruxing, mouth breathing, or tongue thrusting
◦ Oral hypersensitivities, hyperactive bite or gag reflex
Factors significant for DH care
Often experience significant barriers to accessing dental care
Personal and lifestyle factors impacting oral care
◦ Cognitive impairment may impact understanding of oral self-care procedures
◦ Oral motor conditions make self-care difficult for the individual or caregiver
◦ Oral tactile sensitivity such as gagging
◦ Challenging or obstructive behaviors
◦ Mood, fear, or distress when performing oral care
◦ Increased caries risk due to high sugar foods or medications
Social and environmental factors affecting oral care
◦ Caregiver education and support
◦ Oral care equipment and/or assistive devices
◦ Transportation for professional care
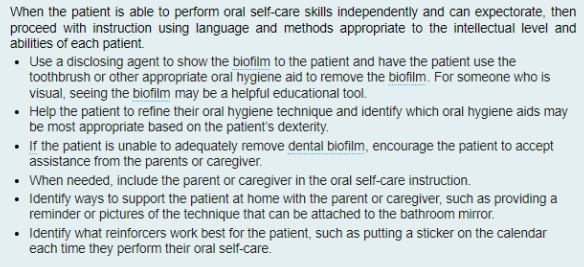
DH Care
◦ Appointments for dental health care may be overwhelming because of the unfamiliar stimuli
◦ Dental care may have been neglected due to problems with social interactions, language and communication problems, or difficult behaviors
◦ Severity of symptoms dictates appropriate setting for delivery of dental care services
◦ Patients with mild-moderate symptoms of ID may be treated successfully in the general dental setting with modifications to treatment/implementation
◦ Patients with more severe symptoms may require sedation, general anesthesia, or immobilization in a hospital or specialized setting
Oral Health Problems
◦ Previous dental care needs not met-child behavior/parent embarrassment or reluctance
◦ Dental caries-high level of oral sensory sensitivity can make for difficulty in maintaining health diet, brushing and flossing can be uncomfortable or even painful
◦ Oral Hygiene-difficulty providing good oral hygiene care with uncooperative individuals, OT may need to be utilized
DH Care Plan
Plan four-handed dental hygiene for the resistant patient
More frequent appointments to prevent oral disease
As cooperation increases, increase preventive services
◦ Biofilm removal
◦ Debridement if needed
◦ Fluoride treatments (flavor or texture could be an issue)
◦ Sealants
Appointment considerations
Provide predictable and consistent experiences
Create a quiet environment and limit stimuli
Avoid unnecessary touching, provide sunglasses, lead apron or weighted blanket
Desensitization/practice
Introductory appointment, move slow, tell-show-do and repeat, patience and firmness, give caregiver tools to help practice at home
Use behavior guidance procedures
Involve caregivers in prevention guidance, provide immediate positive reinforcement, rewards (non-food)
Protective stabilization
Requires additional training to be used safely and should not be used until after less-restrictive approaches have been attempted
Risks and benefits must be explained and written informed consent is required
Parental presence may be helpful for both parent and child
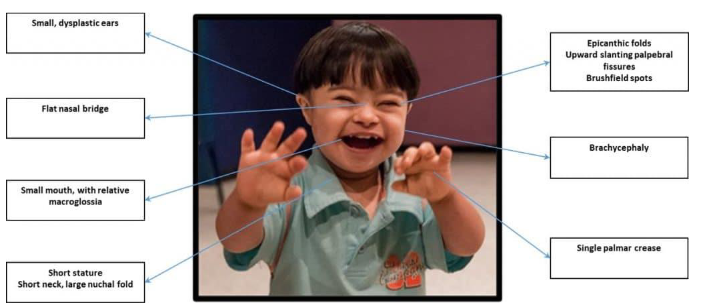
Down syndrome
◦ Trisomy 21
◦ Most common chromosomal condition
◦ According to CDC, approximately 1 in every 775 babies in the US is born with Down syndrome
◦ About 5,000 babies with Down syndrome are born in the US each year
◦ Life Expectancy has increased dramatically due to advancements in medical treatment and social support
◦ As many as 80% of adults with Down syndrome reach age 60, and many live longer
◦ Most live with family in private homes or settings such as group residential homes and access health care as well as dental care services within their communities
DS: How you Speak Matters!
Should always be referred to as people first
Instead of “a Down syndrome child”, refer to as “a child with Down syndrome”
Avoid “Down’s child” and describing the condition as “Down’s” as in, “He has Down’s.”
Down syndrome is a condition or a syndrome, not a disease
People “have” Down syndrome, they do not “suffer from” it and are not “afflicted by it”
Typically developing” or “typical” is preferred over “normal.”
“Intellectual disability” or “cognitive disability” has replaced “mental retardation” as the appropriate term
The National Down Syndrome Society (NDSS) strongly condemns the use of the word “retarded” in any derogatory context
Using this word is hurtful and suggests that people with disabilities are not competent
DS: Physical Characteristics
◦ Poor muscle tone and altered gait
◦ Short neck
◦ Flat facial features
◦ Slanted eyes with epicanthic fold (from upper eyelid over inner angle of eye)
◦ Small mouth and macroglossia
◦ Small ears
◦ Small hands with short fingers and one crease in the palm of their hand (palmar crease)
◦ Shorter than average height
DS: Cognitive and behavioral characteristics
◦ Need to be kept in mind as approach to dental/dental hygiene appointments may need to be altered
◦ Short attention span
◦ Stubbornness and tantrums
◦ Delayed language and speech development
◦ Impaired executive functioning
◦ Slower to gain new skills and more difficulty maintaining them
◦ Higher nonverbal reasoning and ability to solve problems using visual reasoning
◦ High risk of Alzheimer’s disease
DS: Other Medical Complications
◦ Heart problems
congenital heart disease
◦ Thyroid disease
◦ GI problems
constipation, GERD, celiac disease
◦ Neurological conditions
epilepsy, autism
◦ Vision impairment
◦Hearing impairment
(high prevalence); chronic ear infections
◦ Early-onset Alzheimer’s disease
◦ Osteopenia-osteoporosis
◦ Respiratory problems (sleep apnea, prone to respiratory tract infections)
◦ Obesity
DS: Oral findings
◦ Macroglossia with protruding tongue
◦ Narrow, vaulted palate
◦ Delayed or irregular sequence of eruption
◦ Congenitally missing teeth
◦ Malocclusion
◦ TMJ dysfunction in about 77% of DS patients
◦ Mouth breathing
◦ Periodontal disease (infections more prevalent and more severe)
◦ Poor oral hygiene
◦ Bruxism
Children and young adults have a lower prevalence of dental caries
Delayed eruption, congenitally missing teeth and microdontia resulting in wider interdental spaces and less food accumulation
DS: Factors significant for DH care
Individual factors:
Review med history and medications with caregiver
Communicate effectively by using simple, clear language along with visual aids, repetition due to memory issues
Behavior is not typically an issue but discuss with the caregiver beforehand
Minimize stimuli (excess noise)
Chair positioning may need to be adjusted due to dysphagia or respiratory problems
More frequent periodontal maintenance may be necessary
Social factors:
May have access to occupational therapy (OT) –could assist with oral hygiene skills
Caregiver education for prevention and management of oral disease
Environmental factors:
Those living in a residential center may have difficulty finding transportation for routine dental care
Patients with Down syndrome present with additional special needs and health concerns including all of the following except which one?
A. Ear infections and hearing loss
B. Seizures
C. Ventricular septum defects
D. Congenital heart disease
E. Diabetes
E) Diabetes
Which of the following is a dental anomaly NOT commonly associated with Down syndrome?
A. Microdontia fused teeth
B. Supernumerary teeth
C. Hypoplastic enamel
D. Irregular sequence of eruption
B) supernumerary teeth
Fragile X Syndrome
◦ Genetic condition that can cause a range of learning and developmental problems
◦ Leading cause of inherited intellectual disabilities
◦ More common in boys than girls, and boys usually have more severe symptoms
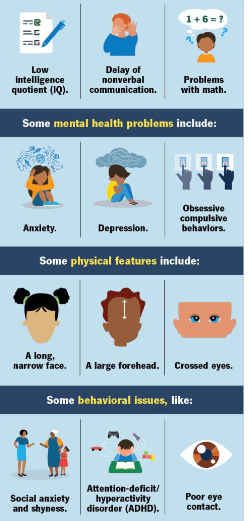
FXS: physical characteristics
◦ Long, narrow face
◦ Large forehead
◦ Large jaw
◦ Large, protruding ears
◦ Crossed eyes
◦ Hyperflexibility of joints due to connective tissue dysplasia
◦ Flat feet
◦ High-arched palate
◦ Low muscle tone (hypotonia)
FXS: Cognitive and Behavioral Characteristics
◦ Intellectual disabilities
◦ Hyperactivity disorder (ADHD)
◦ Autism spectrum disorder
◦ Social anxiety and shyness
◦ Poor eye contact
◦ Difficulty picking up social cues
◦ Weak short-term and working memory-limited ability to retain and process new information
◦ Impairment of executive functioning
◦ Language processing disorders
FXS: medical complications
◦ Over ½ experience recurrent otitis media (collapsible Eustachian tubes)
◦ Neurologic conditions-seizures, hand flapping
◦ GI issues-GERD, diarrhea
◦ Vision problems
◦ Sleep issues-difficulty sleeping, sleep apnea
◦ Aggressiveness or irritability
◦ Self-injury behaviors
◦ Obesity
FXS: oral findings
◦ High arched palate
◦ Mandibular prognathism
◦ Macroglossia
◦ Enamel hypoplasia
◦ Malocclusion
◦ Gingivitis
◦ Poor oral hygiene
◦ Medication-induced xerostomia

FMX: Factors Significant for DH Care
Individual factors:
◦ Review med history and medications as well as behavioral considerations with caregiver
◦ Gather information regarding cognitive and behavioral limitations as well as vision or hearing issues before first visit
◦ Behavior may result in lack of cooperation with caregivers during oral care
◦ Short=term and working memory issues need to be considered when providing education
◦ Visual-motor coordination may make it difficult for patient to learn self-care techniques
◦ GERD with medication-induced xerostomia can result in high caries risk-consider fluoride treatments
Social factors:
◦ Caregiver education and support for routine oral care will be vital in prevention and management of oral disease
Autism Spectrum Disorder
◦ Complex spectrum of developmental disorders, varies in severity
◦ Characterized by impaired social skills, communication problems, and repetitive actions
◦ Symptoms can begin before age 2, usually diagnosed between2-4
◦ Comorbidity with other disabling and medical conditions is common
Prevalence
◦ Rapidly increasing in the past few decades
◦ Year 2018 estimated 1 in 44 children, 2000 1 in 150 children-may be attributable to increase in awareness and better diagnostic testing
◦ Occurs in all racial, ethnic, and social groups worldwide
◦ More than 4x as common in boys than girls
Etiology
◦ Multifactorial, genetic and environmental factors (genetic factors 30% of risk)
◦ About 40 prenatal, perinatal, and postnatal risk factors that may increase risk, more research needed
◦ Tendency to run in families, but inheritance pattern is usually unknown
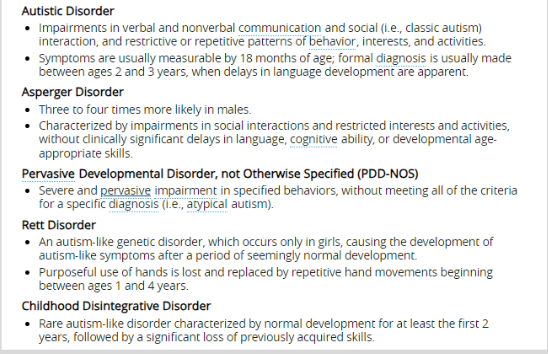
Main characteristics of Autism

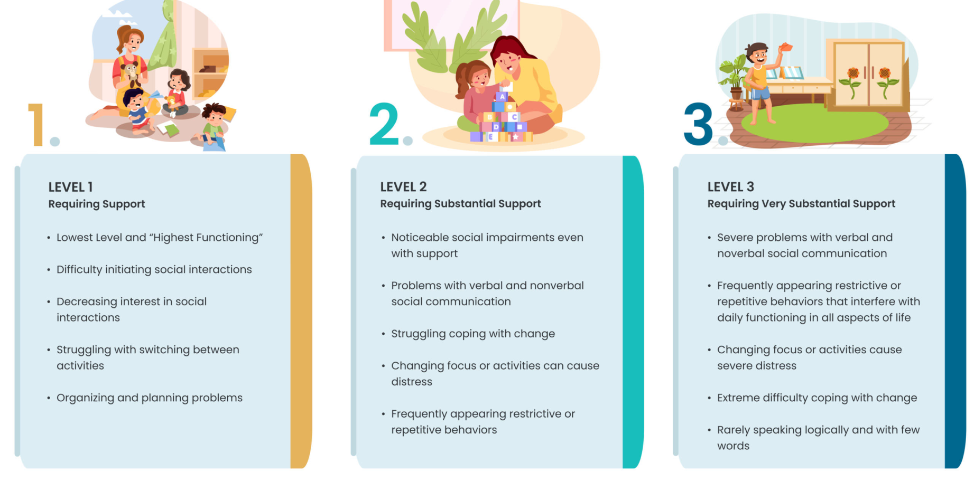
The Three Levels of Autism
Treatment with Peeps with Autism
◦ No “cure”
◦ Individualized treatment using multiple approaches
◦ Behavioral
◦ Developmental
◦ Educational
◦ Social
◦ Pharmacologic
◦ Psychological
◦ Complementary and alternative
Autism: Factors significant for DH Care
◦ Patience, a consistent approach, and patient preparation prior to the appointment can increase probability of a successful dental visit
◦ Careful investigation of med history and medication along with questions regarding behavioral considerations
◦ Poor oral hygiene and gingivitis are common
◦ Impairment in social interaction and difficulty in shifting focus of attention make traditional oral health education approaches difficult
◦ Repetitive body movements and mannerisms may compromise patient safety and impact infection control protocols
Next up: programs to help improve outcomes of dental visit for patients with ASD
D-Termined Program (DTP) of Familiarization and Repetitive Tasking
◦ Training program for dentists
◦ System gradually introduces children with ASD to the expectations of a dental visit so that they can successfully receive treatment in a normal dental office
The five “D” steps for learning cooperation skills
1) Divide the skill into smaller parts: the key for people with autism is to take each small step of a dental appointment one at a time, and master it before moving ahead
2) Demonstrate the skill: use the tell-show-do technique
3) Drill the skill: repeat/practice the skill many times until it becomes second nature
4) Delight the learner: reward successful attainment of any small portion of the task with reinforcement
5) Delegate the repetition: involve other members of the dental staff in reinforcing the skills and have parents/caregivers rehearse/practice at home
Autism speaks dental tool kit
◦ Tips for caregivers to work on oral health at home and prepare for visits to the dentist. Includes information on selecting the right tooth brush, flossing tools and schedule aids to help keep autistic children and adolescents on track.
◦ Autistic perspective with tips for autistic people, parents and dental professionals to make dental visits more comfortable.
◦ Tried-and-tested tips from parents of autistic children on everything from selecting a tooth brush to scheduling dental appointments based on what an autistic loved one's preferences.
◦ Information for dental professions to better understand autism, the autistic patient, and how to better accommodate autistic patients.
◦ Visual schedule for parents to use with their autistic loved one to help them better understand the steps of a routine dental exam.
◦ Standard dental form for parents to fill out ahead of a first visit with a dentist to help them better understand their loved one.
Autism: Additional strats for dental care
◦ Desensitization through short familiarization visits-“get to know you” appointment to build trust and learn of patient’s capabilities, break down the appointment into smaller steps
◦ Provide a sensory-friendly environment-turn down lights and music, noise-canceling headphones, weighted blankets or lap pads
◦ Use simple, clear, and brief language or use of visual aids
◦ Be understanding-anxiety or overstimulation and result in negative behavior such as yelling, head banging, combativeness, or defiance and is not typically something the patient can control
◦ Educate caregivers-visual aids/books and “take-home kits” to allow for familiarization and preparation at home
◦ Provide a calm and supportive environment to reduce anxiety and fear associated with the dental visit and to increase chances of a successful visit!
Which of the following is NOT a consideration for dental hygiene care of a person with autism?
A. Avoid unnecessary touching
B. Minimize sensory stimuli
C. Provide a consistent and predictable experience
D. Schedule morning appointments after a meal
D. Schedule morning appointments after a meal
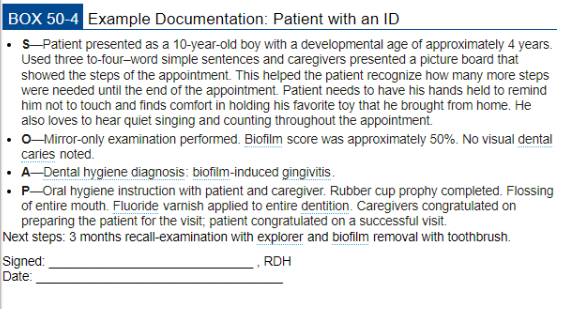
Documentation for a patient with a neurodevelopmental disorder
◦ Chronologic age versus developmental age
◦ Communication strengths and weaknesses with patient and caregiver
◦ Helpful behavioral supports and guidance techniques
◦ Treatment completed and helpful modifications
◦ Recommended home oral hygiene teachniques
Factors to teach patient