Pulmonary Ventilation Flashcards
1/40
Earn XP
Description and Tags
Flashcards about Pulmonary Ventilation, created from lecture notes.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
41 Terms
What are the four major functions of respiration?
Pulmonary ventilation
Diffusion of oxygen and carbon dioxide (they will always go together)
Transport of oxygen and carbon dioxide
Regulation of ventilation (based on tissue needs)
What are the two main mechanics of pulmonary ventilation?
Downward or upward movement of the diaphragm and elevation or depression of the ribs.
Describe the muscles of inspiration
Diaphragm - forces abd contents down and forward
External intercostals, pectoralis minor, sternocleidomastoid, and scalenes - lift ribs up and outward pulling the individual alveoli along with contraction to energy being used
Describe how pressure changes as air flows into the lungs.
When alveoli are pulled open, pressure decreases in alveoli and air flows in, making pressure less than 760 mmHg following the pressure gradient
What mechanism forces air into the lungs?
Explain the relationship between atmospheric pressure and lung pressure for air to flow into the lungs.
differences in pressure
Air flows into the lungs when atmospheric pressure becomes greater than the pressure within the lungs called bulk flow
Describe the muscles of expiration.
Rectus abdominis, internal obliques - push diaphragm up
internal intercostals - pull ribs downward
T/F - expiration at rest is passive
True - no ATP (energy) is requried because of the elasticity (recoil of the lungs, chest wall, and abd structures
What is the average number of breaths a minute at rest?
12
Describe the lung's position in the thoracic cavity.
The lungs “float” in the thoracic cavity and are surrounded by a thin layer of pleural fluid which lubricates the lungs.
Lungs are 'attached' to the chest wall via suction between the visceral surface of the lung and parietal pleura surface of the thoracic cavity
Distinguish between visceral and parietal pleura.
Visceral pleura adheres to the outer surface of the lungs, and parietal pleura adheres to the thoracic wall.
What is pleural pressure?
Pressure of the fluid in the thin space between the lung pleura and chest wall pleura
What is the role of the interpleural space in lung function?
Has fluid to lubricate the pleura
A low pressure (-5 cm H2O) area that is required to hold the lungs open to their resting level = lungs will be able to inflate with normal inspiration and pressure becomes more negative (-7.5)
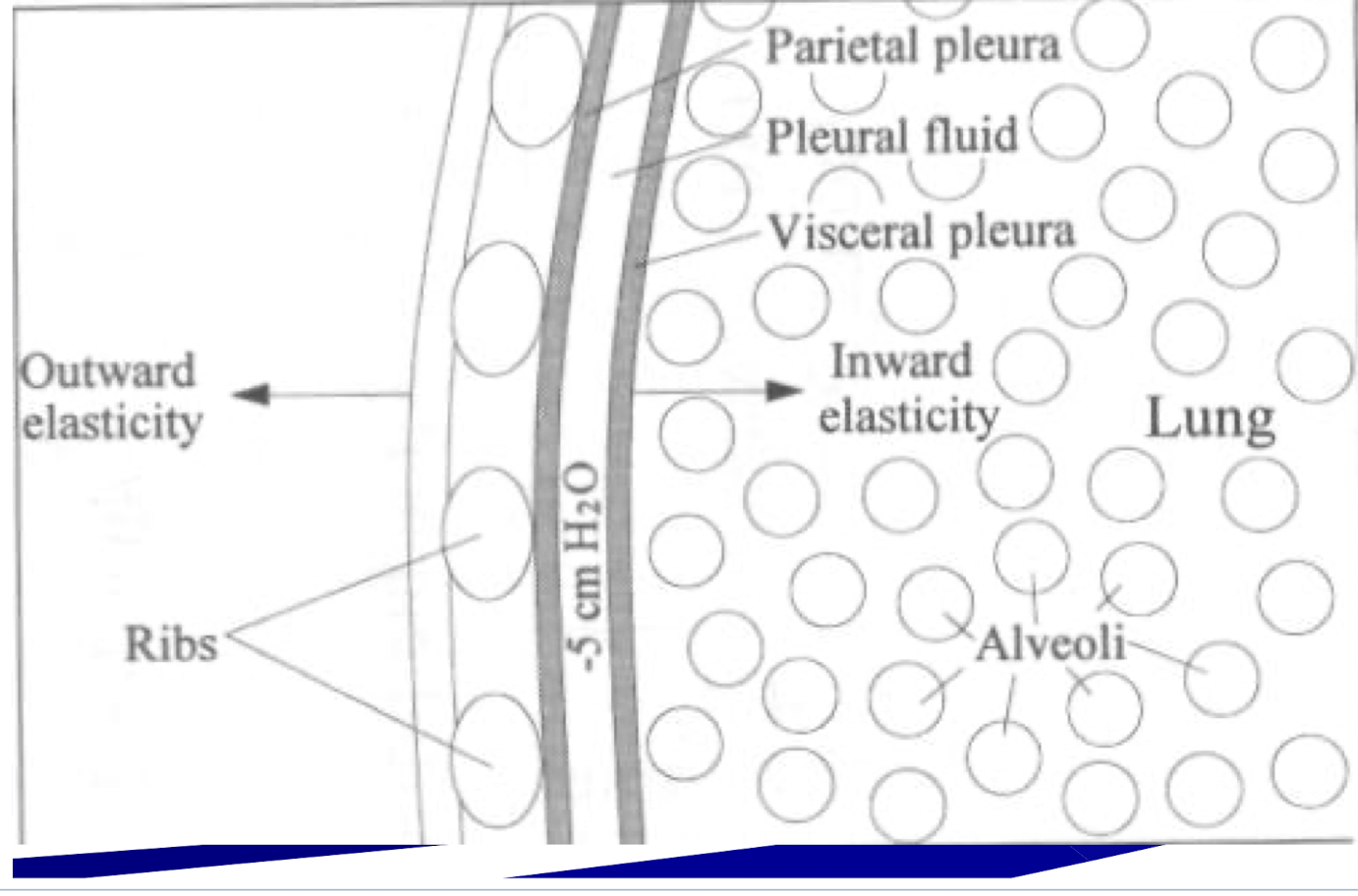
Describe how pressure is related to this image
The inward elasticity of the lung will try to collapse on itself but the outward elasticity prevents that from happening and will create the -5cm H2) pressure within the pleural fluid
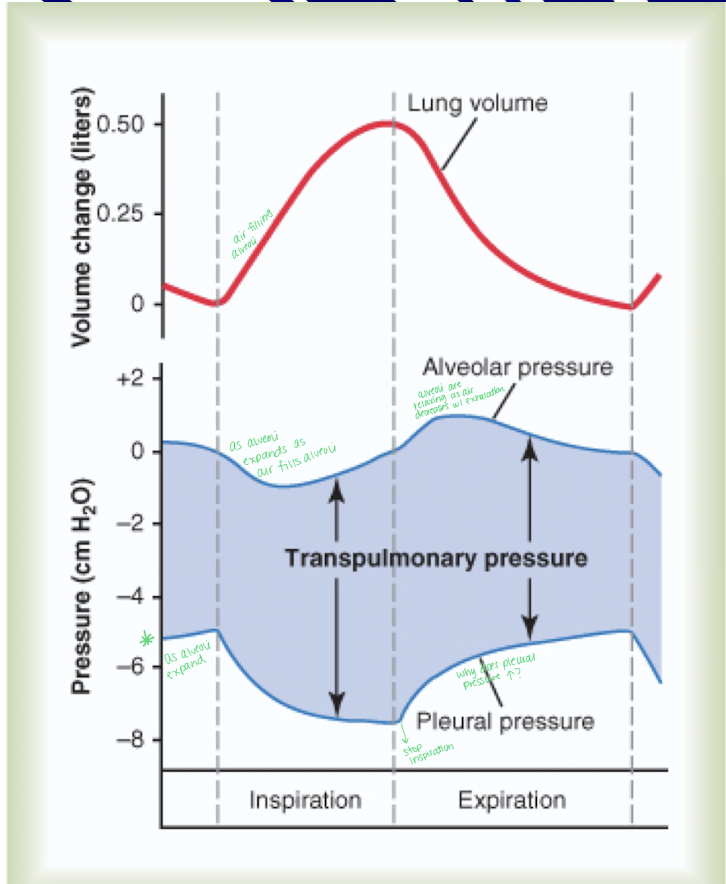
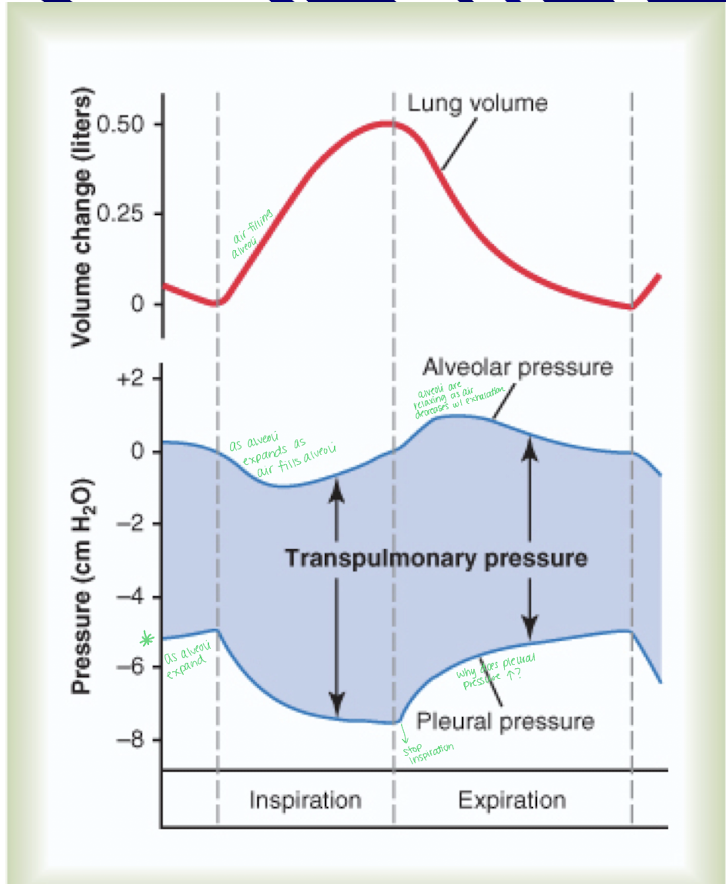
Explain the relationship between lung volume, alveolar pressure, and pleural pressure in relation to inspiration and expiration
Inspiration
Lung volume will increase
Alveolar pressure will decrease because the alveoli will expand as air flows in
Pleural pressure will become more negative, aiding in lung inflation (-5 cm H2O)
Expiration
Lung volume will decrease
Alveolar pressure will increase as the lungs compress causing alveoli to relax
Pleural pressurewill become less negative, helping to expel air from the lungs.
What are two key characteristics of alveoli?
Elastic - when they lose their elasticity, getting air out can be hard (pulmonary diseases)
thin-walled - for diffusion purposes, they allow fast diffusion of ions
T/F: the alveoli have a large blood-gas barrier
false - very small
When is the alveolar pressure equal to atmospheric pressure (0 cm H2O or 760 mm Hg)?
When the glottis is open and there is no air movement.
What must occur to alveolar pressure (increase/decrease) for air to be sucked into the alveoli
Decrease
What is transpulmonary pressure and what does it measure?
When is transpulmonary pressure the highest?
It is the pressure difference between the alveoli and the outer surface of the lung.
Representing elastic forces tending to collapse the lungs with each expiration.
During exercise
Explain the relationship between alveolar pressure and transpulmonary pressure during inspiration and expiration
Inspiration
Alveolar pressure decreases
transpulmonary pressure increases
Expiration
alveolar pressure increases
transpulmonary pressure decreases
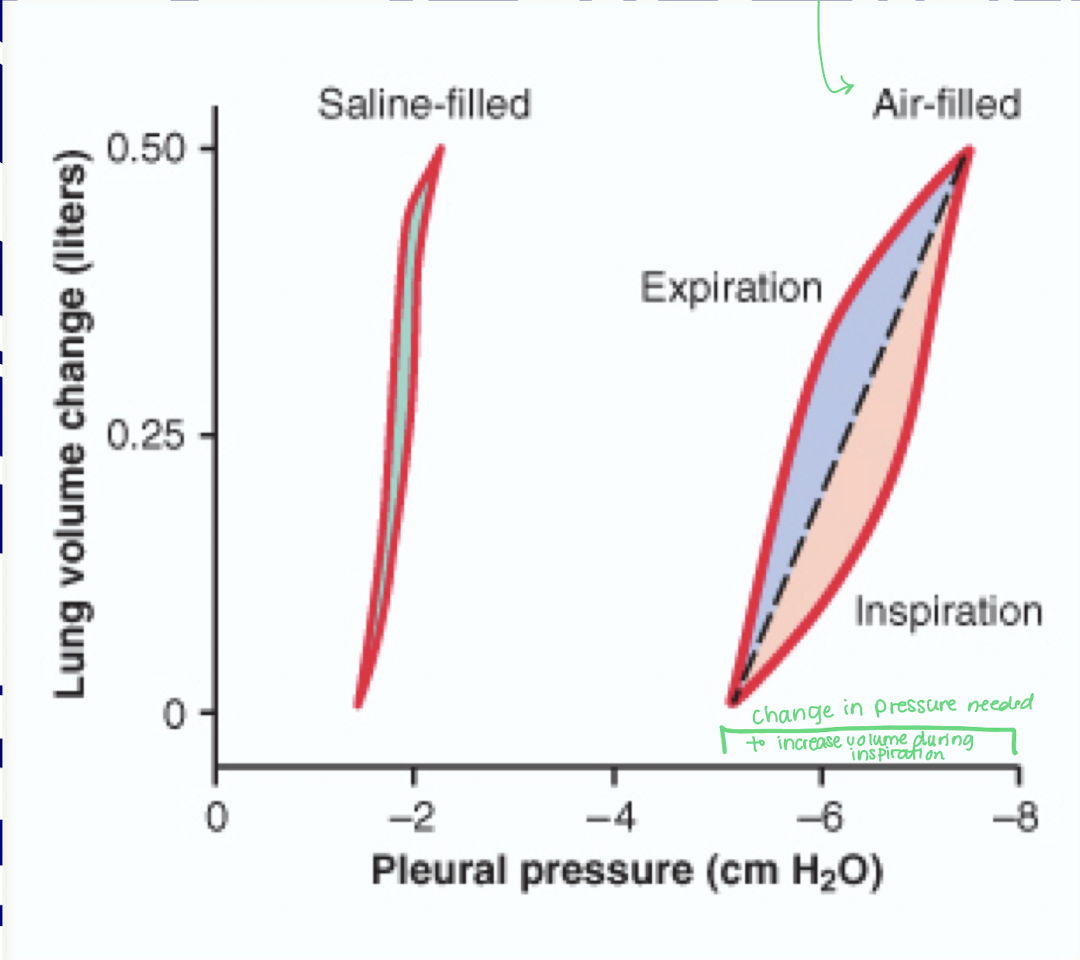
What is lung compliance?
What is the average amount of air per 1 cm of water pressure change
The extent to which the lungs will expand for each unit increase in transpulmonary pressure.
Low compliance makes it difficult to breathe (inspiratory problem) because it takes more effort to expand the lungs.
High compliance is when the elastic recoil from stretched alveoli is lost making it difficult to expire
200 mL
What two factors rely on lung compliance?
how much alveolar volume changes with change in intrapleural pressure
List some causes of low lung compliance.
Low compliance
Alveolar edema
Fibrosis
High surface tension
High Compliance
Aging
Emphysema
What are the two elastic forces of the lung?
Elastic force of lung tissue and elastic force caused by surface tension of the fluid lining the alveoli.
increase in surface area = increase in ability of alveoli to contract on itself
occurs in air filled lungs and it will take a greater amount of pleural pressure to increase volume during inspiration because surface tension makes compliance harder
Saline filled has NO surface tension because it has less compliance, less surface tension to overcome to inflate
What is surface tension elastic force?
elastic contractile force of the entire lung
What is the function of surfactant?
What are type II alveolar cells
It reduces surface tension reducing the effort required by the respiratory muscles to expand the lungs
secrete pulmonary surfactant
What is respiratory distress syndrome?
Occurs in newborns when babies are born premature and can’t breathe on their own due to undeveloped lungs. They will be missing surfactant and treatment is positive pressure ventilator
What are the three fractions of the work of inspiration?
Compliance work - work required to expand the lungs against the lung AND chest elastic forces
tissue resistance work - work required to overcome viscosity of the lung and chest wall structures
airway resistance work - work required to overcome airway resistance to movement of air into lungs
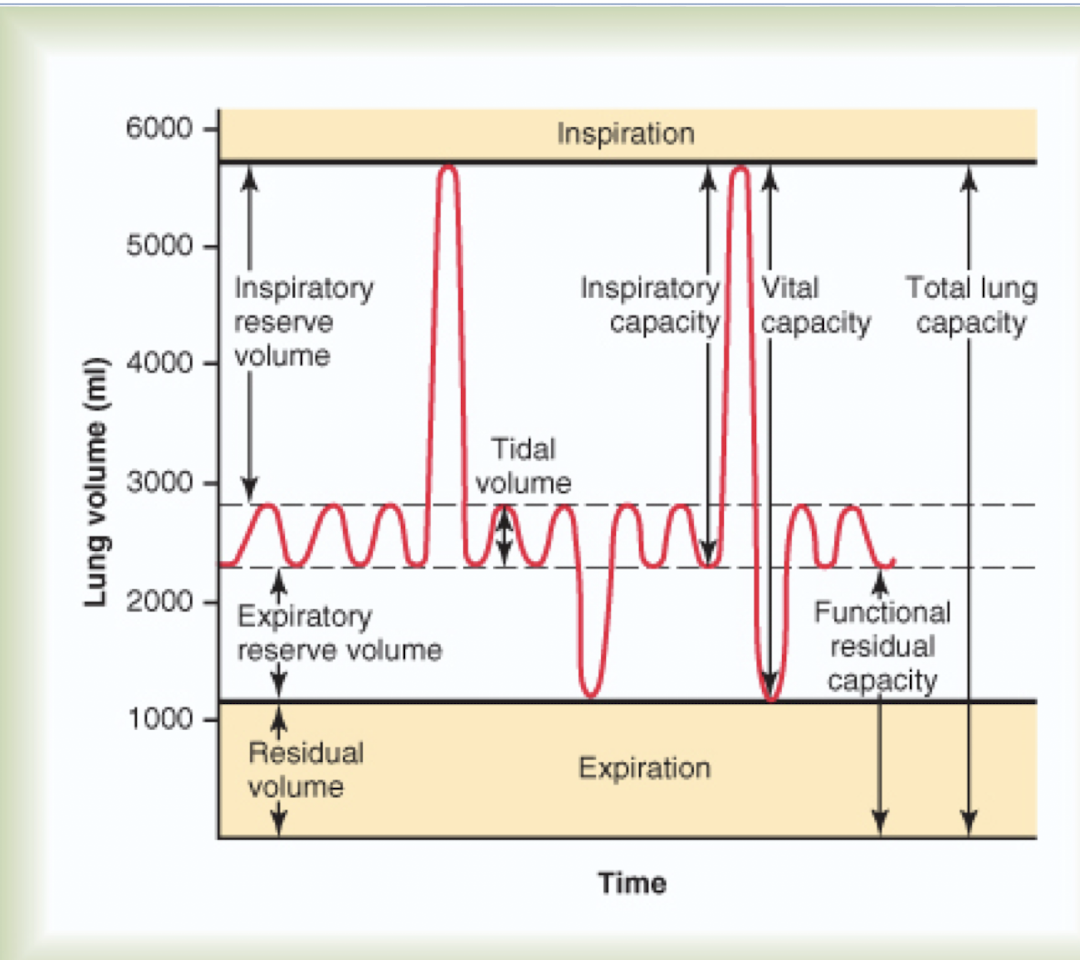
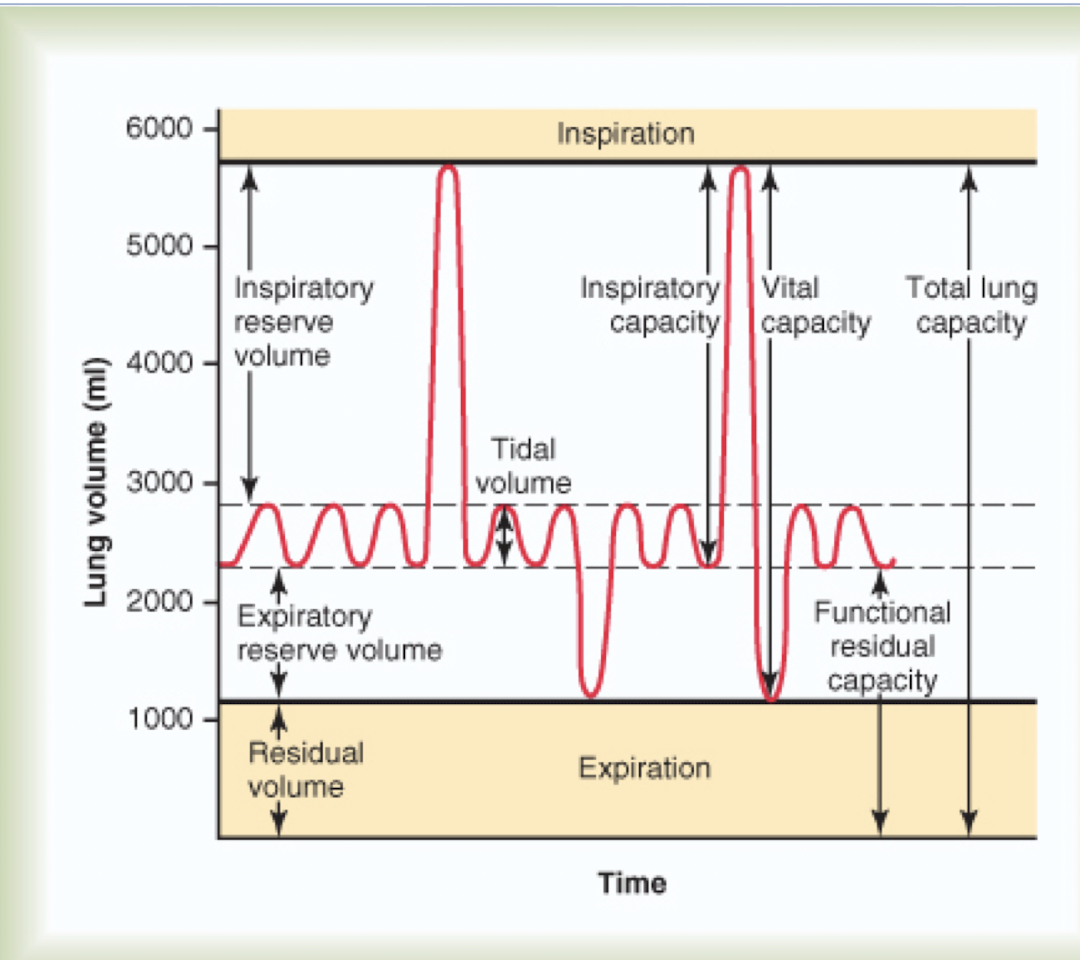
What are the four total lung volumes?
Tidal volume (TV) - amount of air normally inspired or expired (happens constantly)
inspiratory reserve volume (IRV) - maximal volume inspired AFTER normal inspiration
expiratory reserve volume (ERV) - volume expired AFTER normal expiration
residual volume (RV) - volume remaining in the lungs after MAXIMAL EXPIRATION
T/F: residual volume will increases with age along with total lung capacity remaining stable
true - due to loss of elastic recoil in the lungs and increased stiffness of the chest wall.
What is the general lung capacity (in liters) for both men and women?
Men hold 1.2 L of oxygen
Women hold 1.0 L of oxygen
What are the four lung capacities?
Total lung capacity (TLC) - volume within lung after maximal inspiration
inspiratory capacity (IC) - max volume inspired from the end of tidal expiration
functional residual capacity (FRC) - volume in lungs after normal expiration
vital capacity (VC) - max volume expired after max inspiration (air we can actually use)
What is minute ventilation
How is minute ventilation calculated?
Minute ventilation is closely related to _____
volume of new air moved into the respiratory passage in one minute, including dead space
Tidal volume times frequency (12 breaths x 0.5L = 6 L/min)
CO2 production
In minute ventilation oxygen consumption increases which is closely associated with _______
CO2 production
What is alveolar ventilation?
How is alveolar ventilation calculated?
Rate at which gas exchange areas receive new air in the alveoli only
(TV - DS) x frequency
Where does minute ventilation occur compared to alveolar ventilation?
Minute ventilation (6 L/min) occurs in the thorax region versus alveolar ventilation (4.2 L/min) occurs only in the alveoli
What is anatomical dead space?
What is the physiological dead space?
Areas of the conducting zone not designed for diffusion of gases.
areas of lung and pulmonary capillary bed unable to perform gas exchange as designed
Explain sympathetic control of bronchioles.
Bronchial tree is exposed to NE and Epi by medulla and bind to beta receptors to cause dilation of bronchial tree.
Explain parasympathetic control of bronchioles.
ACH causes mild to moderate constriction of bronchioles
Atrophine is given to block ACH and offers some relief
____ is provided to block ACH affected the bronchioles
Atropine
What is pleural pressure at rest?
What is pleural pressure at normal inspiration?
-5 cm H20
-7.5 cm H20