Health and Social Care Unit 2
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
77 Terms
What is the diffrence bwteen a role and a repsponsbility?
Role = what your job is / your position
Example: A physiotherapist’s role is to help people improve movement and reduce pain.
Responsibility = what tasks you must do in that job
Example: A physiotherapist’s responsibilities include creating exercise plans, helping patients with mobility, and keeping records.
In short:
Role = the overall purpose of the job
Responsibility = the specific things you must do
What is a legislation and policy
Whats the diffrence healthcare and socialcare?
Healthcare = medical needs.
Social care = everyday support and wellbeing.
What are the roles, responsibilities of doctors (GPs)?
Doctors provide medical care for patients. They work mainly in surgeries and local communities.
Roles
Provide primary medical care to patients.
Diagnose, treat, monitor, and prevent illnesses
Support patients to maintain and improve their health
Medical Responsibilities
Diagnosing illnesses.
Prescribing treatments to promote healing and recovery.
Providing prescriptions and arranging preventive care (e.g., flu immunisations).
Referring patients to specialists, therapists, and other health professionals.
Non-medical responsibilities
Creating and maintaining relationships of trust with patients.
Observing, listening, and responding when communicating with patients
Maintaining confidentiality
Acting in accordance with legislation
Specialist Doctors
Roles
Provide expert medical care in a specific area (e.g., cardiology, oncology)
Diagnose and manage complex medical conditions
Support patient recovery through specialist treatment plans
Responsibilities
Conducting specialist examinations and tests
Prescribing specialist treatments and medications
Performing medical procedures related to their speciality
Referring or consulting with other healthcare professionals when needed
Non-medical responsibilities
Creating and maintaining relationships of trust with patients.
Observing, listening, and responding when communicating with patients
Maintaining confidentiality
Acting in accordance with legislation
Nurses
Roles
Deliver day-to-day patient care and support
Monitor patients’ health and well-being
Promote comfort, dignity, and recovery
Responsibilities (Medical)
Checking vital signs and monitoring patient conditions
Administering medications and treatments
Supporting patients with personal care needs
Keeping accurate patient records
Non-medical responsibilities
Providing care and counselling
Helping with recovery and rehabilitation
Writing patient care plans
Planning patient discharge from the hospital
Acting as a patient advocate (ensuring their voice is heard, their rights are upheld, and their interests are represented)
Midwifes
Roles
Support women during pregnancy, labour, and after birth
Promote the health of mothers and babies
Provide emotional and physical support to families
Responsibilities
Monitoring the health of the mother and baby
Assisting in childbirth
Providing postnatal care and breastfeeding support
Giving advice on baby care and maternal health
Non-medical responsibilities
Preparing and reviewing patient care plans
Arranging and/or providing parenting and health education
Providing support and advice on the care of newborn babies
Providing support and advice following miscarriage, termination or neonatal death (the death of a baby within the first 28 days of life)
Liaising (acts as a link to assist communication between people or groups).with other agencies to ensure continuity of care.
Healthcare Assistants (HCAs)
Roles
Support patients with daily living needs
Assist nurses and doctors in patient care
Promote comfort and well-being
Medical Responsibilities
Reporting changes in patients’ conditions to nurses
Monitor health by taking temperature, pulse and weight.
Non-medical responsibilities
Washing and dressing patients
Helping with patient mobility, transferring patients safely
Supporting day-to-day routines
Talking to patients
Working under the direction of the nursing staff
Supporting and delivering health education
Making beds and maintaining a clean environment
Occupational therapists
Roles
Help people to live as independently as possible
Support patients to carry out everyday activities
Improve quality of life through practical solutions
Medical Responsibilities
Assessing patients’ ability to perform daily tasks
Creating personalised therapy plans
Teaching patients new ways to complete activities
Recommending equipment or home adaptations
Being aware of acute medical conditions and how to overcome them in contexts such as accident and emergency (A&E) and acute medicine.
Non-medical responsibilities
Advising on specialist equipment to assist with daily activities
Advising on home and workplace alterations, e.g wheelchair access.
Assisting people to return to work
Coaching people with learning difficulties, e.g handling money.
Enabling rehabilitation
Organisations and rehabilitation groups for carers and clients
What are the roles, responsbilites for a care manger?
Roles
Oversee the running of care services.
Ensure high standards of care are provided
Lead and support care staff.
Responsibilities
Creating and reviewing care plans
Managing staff schedules and training
Monitoring quality of care and inspections
Ensuring policies and safeguarding procedures are followed
Key skills, qualities and tasks
Creating and maintaining relationships of trust with residents
Maintaining accurate resident records
Observing, listening and responding to resident concerns
Maintaining confidentiality
What are the roles, responsbilites for a Care assitiant?
What are the roles, responsbilites for a Social Worker?
Roles
Support vulnerable individuals and families
Safeguard children and adults at risk.
Promote independence and well-being.
Responsibilities
Assessing individual needs and risks
Creating support and protection plans
Referring individuals to services and support
Keeping detailed and confidential records
Key skills, qualities and tasks
Preparing and reviewing case files of clients
Taking difficult decisions
Working with a charity serving users of different ages
Ensuring continuity of care
What are the roles, responsbilites for a Youth Worker?
Roles
Support young people’s personal and social development
Provide guidance and positive role modelling.
Promote healthy choices and behaviours.
Support the educational growth of individuals aged 11-25 to help them reach their full potential in society.
Responsibilities
Organising activities and group sessions
Offering advice on education, relationships, and wellbeing
Supporting young people through challenges
Working with schools, families, and agencies
Key skills, qualities and tasks
Working across different sectors, including care and criminal justice and public and private, and voluntary sector organisations.
Developing projects with schools and other organisations, such as debates about elections or capital punishment.
Offering advice on topics such as sexual health using language which is accessible to young people.
What are the roles, responsbilites for a Support Worker?
Roles
Provide practical and emotional support to individuals
Help people live as independently as possible.
Promote inclusion and participation.
Responsibilities
Assisting with daily routines and personal care
Supporting individuals in the community
Recording progress and reporting changes in needs
Encouraging independence and life skills.
Key skills, qualities and tasks
People who provide social or personal care often work with people who have had healthcare or who continue to need it.
Healthcare setting - GP surgires and local health centres (Purpose)
Patients go here first when they need medical
• Doctors diagnose the patient's illness. They
patients to other services.
may issue a prescription for medication or refer
screening, or take blood tests.
• Nurses might carry out treatment or health
Healthcare setting - Clinics
Patients go here to be treated for specific
medical conditions.
• Patients are referred by their GPs to
specialist clinics based in hospitals and in
the community.
• Trained personnel, including doctors and
nurses, work in clinics,
Healthcare Setting - Hospitial
Patients go here for treatment that a GP
Cannot give. It is where operations are
carried out, and Accident and Emergency
(AtE) departments and some walk-in centres
are located
• Patients are refered by their GPs to
∙ specialist medical teams.
Specialist doctors (consultants) may issue
prescription for specialist medication or
refer patients to surgeons for operations,
Healthcare setting - Home
This is where care is provided for housebound
people or those who are recovering from medical
treatment such as an operation.
• Most people prefer to recover at home and some
who are dying prefer to be nursed at home.
◦ Care may be provided at home for births
• Patients are treated at home by community-based
nursing and midwifery staff.
•
Doctors carry out home visits when necessary.
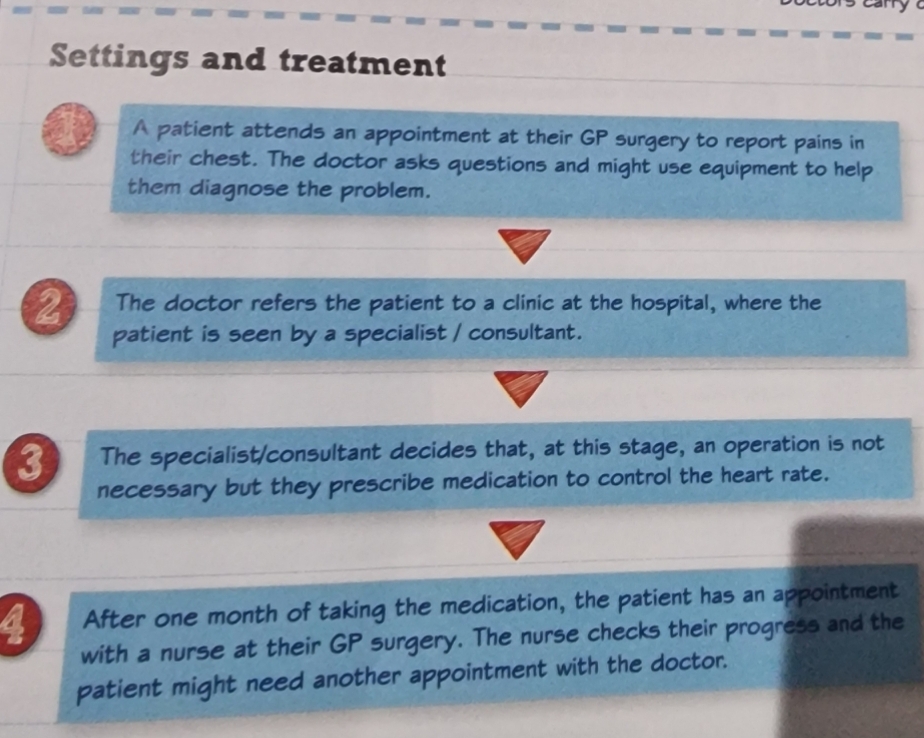
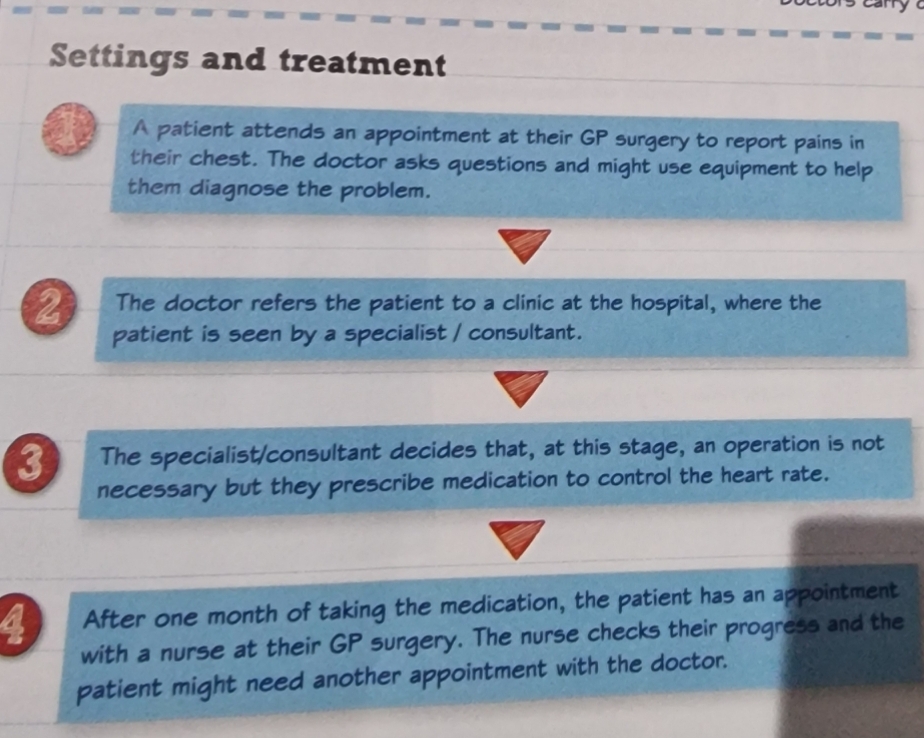
Treatment pathway
Social cafe settings - Resdiential care settings
• These are settings where people who can't be cared for at
thelr own, are looked after.
home, or who feel that they can no longer cope with llving on
They may provide full-time or temporary respite care to give
break to carers, or those who struggle lving on their own.
• Social care workers provide residents with personal care,
such as washing, toileting and dressing.
Benefits for people in residential
Trained staff meet people's needs and Support
them.
Specialist support is available for those with
more complex care needs.
Companionship is provided by other residents
and staff.
A range of stimulating activities iS offered.
Difficulties for people in residential care
Social care workers have to support people to
overcome the difficulties of residential care:
losing some or all of their independence
reluctance to leave their own homes
isolation from friends and relations
cost of care.
Social care setting- Domiciliary Care
• Social care workers provide care for
people in their own home.
◦ Care workers help people lead their daily
lives by supporting their independence.
◦ Social care workers might help people with
shopping, cleaning and transport, such as
taking them to a doctor's appointment
◦ Social care workers can provide carers
with a short break from their duties.
Social care setting - Daycare centres
• These are used by older people
and those with physical and learning
disabilities.
• They provide respite care
• Social care workers might take part in
leisure activities with people attending:
How do workers support people with a physical disability at home?
Ensuring the person has access to all rooms within their home, ensuring facilities are within reach and not at floor level (e.g reaching electric sockets) and if necessary hoist (raising something) in the bedroom and bathroom.
How do workers support people with a physical disability in an Educational Setting?
Ensuring service users can access classrooms and bathrooms, e.g installing minimum door requirements to accommodate wheelchair users.
Disabled children have access to play and exercise facilities.
The curriculum is adapted to meet their needs, e.g languages used in lessons should respect the dignity of people with disabilities.
How do workers support people with a physical disability in work?
Providing awareness training for work colleagues
Providing a support worker to help the person in the workplace.
Providing extra time if necessary to complete work tasks.
How do workers support people with a physical disability in a leisure setting?
Providing accessible changing facilities
Providing sustainable signage (signs collectively, especially commercial or public display signs), e.g., braille for people with visual impairments.
Access to adapted seating and spaces for elevated wheelchair viewing.
Why is following policies and procedures in work settings important?
They ensure the health and safety of service users and health and social care workers, they support the day-to-day routines of service users, enable the needs and preferences of service users to be met and promote independence among service users.
What is discrimnation?
This is when a person is treated unfailry because of who they are, or is treated unequally because of who they are, or experiences prejudice that has been put into practice.unfairly
What are the two types of discrimantion?
Direct discrimnation- treating someone worse, differently or less favourably because of their characteristics, e.g harassment, receiving abusive comments and victimisation, which is when someone is treated badly because they complained.
Indirect discrimination - when an organisation’s practices, polices, or rules have a worse effect on some people than others. An example is pregnancy and maternity discrimination if pregnant women or new mothers are treated unfairly or disadvantaged.discrimination
What are some examples of anti-discriminatory practice in health and social care?
Acessbile signage
Leaflets in many languages
Access to buildings
Longer appointments for people with earning disabilities
Policies such as anti-bullying in schools.
What is positive action?
This is when people who have protected characteristics are at a disadvantage, have particular needs, are under-represented in a type of work or activity, and it is possible to do something voluntarily to help them.
All types of discrimination are illegal, although positive action is allowed in certain clearly defined circumstances.
Describe how the Equality Act 2010 protects people from discrimination?
Protects against discrimination from employers, health and care providers, schools/educational centres, transport services, public bodies such as government departments and local authorities. discrimination
What are the characteritcs which are protected by the Equality Act 2010?
Gender and gender reassigment
Age
Sexutal orienatation
Race
Disability
Marital or civil partnership status
Religion and beliefs
Pregnancy and maternity Sexual orientation
What are some anti-discriminatory practices for travellers?
Enables access to GP services at new locations
Ensure that hostile language is not used
What are some anti-discriminatory practices for transgender people?
Use gender terminology which is acceptable to the service user
Recognise any associated mental health issues
What are some anti-discriminatory practices for a person with a hearing impairment?
Provide hearing loops in GP surgeries
Use British Sign Language to communicate
What are some anti-discriminatory practices for asylum seekers?
Provide translation services if needed
Recognise cultural preferences
What are some anti-discriminatory practices for children with emotional behavioural difficulties?
Provide peer mediation and mentoring in schools
Provide nurture groups in primary schools as an example of early intervention strategy.
What are some anti-discriminatory practices for people with physical disabilities?
Provide accessible rooms in clinics
Support participation in sport and exercise in schools
Doctors should consult patient notes to check the patient’s preferred language and preferred methods of treatment
Nurses should ask whether the patient prefers a male or female nurse
Social workers should advice on actions the service user can take to address any discrimination they experience
Occupational therapists should help people to live independently by ensuring appropriate kitchen equipment for different cultures.
What is empowerment?
This means giving individuals information and support so they can make informed decisions and choices about their lives, in order to live as independently as possible.
How can health professionals empower service user?
Giving individualised care
Promo[ting users dingity
Putting users at the heart of service provision
Balancing the rights of individuals with those of other service users and staff
Promoting independence
Dealing with conflict in an appropriate way
What are rights?
Rights are entitlements that everyone should receive. People's rights are protected by the laws of the UK, such as the Human Rights Act 1998 and the Equality Act 2010.
How is the right of dignity upheld in practice?
Providing privacy for a patient who is using the bathroom in a hospital
How is the right of expressing needs and preferences upheld in practice?
Providing active support to enable the preferences and needs of the individual are met aligned with their beliefs, cultures and preferences.
How is the right of safety and security upheld in practice?
Can support the right by changing legislation (changing smoking in public places), dealing with conflict by applying clear polices and training, protecting from risk or harm by implementing procedures and training behaviour change, balancing individual rights with those of other service users and staff (providing clear training and polices)
What are some possible risks in care?
Abuse by other service users and/or staff
Indequate supervision of support staff, for example, when moving patients.
Lack of illness prevention measures, such as clean toilets =.
Infection due to lack of clean facilities and equipment
Inadequate control of harmful substances
Lack of properly maintained first-aid facilities Inadequate
How do u manage risks in care?
Using risk assessments to identify possible sources of harm, assess the likelihood of them causing harm and minimise the chance of harm.
Staff training to manage risks
Clear codes of practice which are familiar to all staff, including safeguarding and control of harmful substances.
Appropiralty qualfied staff
Ensuring all staff have a DBS (Disclosure and Barring Service) clearance.
Regular and evidence-based checks of facilities and provision of safe drinking water
Availability of protective equipment and knowledge of infection control procedures.
Knowledge of procedures for reporting and recording accidents, incidents and complaints
Provision of maintained first-aid facilities.facilities
What are the stages or reporting incidents and accidents?
Detect an incident or an accident
Record incident or accident
Report the incident or accident to the relevant person
Classify an incident or accident according to type and severity.
Prioritise issues for appropriate actions
Propose preventive measures
Implement changes to working practices
Monitor the effectiveness of changes in preventing future incidents.
What are some barriers to incident reporting?
The incident or accident is seen as not important at the time.
The incident is too long or requires too much detail.
Care staff have other, more pressing duties or procedures.
It may be difficult to access the person who needs to receive the incident/accident report.
There may be pressure from managers not to report incidents and accidents.
What are some problems with evidence?
Inconsistent witness statements
Lack of detail in statements
Poor recall of events
Written evidence that conflicts with other types of evidence, e.g CCTV or voice recording.
Low standard of written English
What are the key points about complaint procedures?
All care settings must have them in place
All care settings must enable service users to access and use them
They are checked when care providers are inspected
They can lead to service improvements
What is the right to complain?
Serivce users have the right for complaints to have complaints dealt with within an appropriate time frame, to have complaints taken seriously, full and thorough investigations of concerns raised, and information about the outcomes of investigations into their complaints.
What is the Data Protection Act 1998?
The Data Protection Act 1998 controls how personal information is used by organisations, businesses or the government. Data must be:
Used fairly and lawfully
Used for limited, specifically stated purposes
Used in a way that is adequate, relevant and not excessive
Accruate
Kept for no longer than is necessary
Handled according to people’s data protection rights
Kept safe and secure
It is strong legal protection for information about your:
Ethnic background
Political opinions
Religious beliefs
Health
Sexual health and preferences
Criminal record (if you have one)
What is some data that an employer in health and social care can keep about their employees?
Name
Address
Date of Birth
Gender
Emergency contact details
Details of any disability
National Insurance number and tax code
Employment history and work experience
Education and qualifications
Gender
Define what is meant by confidentiality?
Confidentiality in health and social care settings means restricting access to information about a service user to individuals who are involved in their care unless permission to disclose the information is given by the service user. NEED TO KNOW BASIS
Where is different data stored?
Computers, tablets and mobile phones
Social Media
Written paper records
Photographs
CCTV cameras in health and social care are used to protect those who are working in health and social are settings and people who use these services. Photographs and images collected by CCTV can only be used in particular circumstances, and for specific purposes; this is one way in which confidentiality is protected by cameras
What is a regulation?
A regulation is a law which sets the standard of professional conduct required of people who work in health and social care settings. Regulations are mandatory.
Why must workers be regulated and what are the consequences of workers who do not follow regulations?
Proffessional bodies must regulate services in their sector. "Regulating employees" means establishing and enforcing rules, policies, and procedures to guide worker behaviour, ensure compliance with laws, and meet organisational goals. Workers must follow codes, be familiar with and able to apply current codes of practise, ensure that check procedures are done before working, for example DBS check, following procedures for raising concerns.
Consequences - Workers can be disciplined by their employer or professional organisation, and this can result in them losing responsbilites, Professional status and suspension without pay.
What do safeguarding regulations do?
Safeguarding regulations protect service users from harm, abuse and neglect and promote their health and wellbeing. Safeguarding and prevention of harm takes place in the context of person-centred care and personalised care, with individuals empowered to make choices and supported to manage risks
Examples
In the Hosptial making sure that all equipment is sterile.
Ensure all staff have a DBS declaration
Ensure effective procedures for reporting accidents and incidents.
What does the Local Safeguarding Children Board (LSCB) require that every local authority to have?
The Job of the LSCB is to :
Make sure everyone understands how important it is to keep children safe.
Make sure that all the agencies that are a part of the LSCB are doing the best job.
Report to the Department of Health
Look into cases where children are badly hurt or have died
Keep a check on information about child deaths
Advise agencies
Listen to childrens veiws and ideas
Hold discussions to find out what people think about children’s issues
What does the Care Act 2014 say about safeguarding adults?
The Care Act 2014 provided this duites for local authorities where they provide care for adults.
Making enquiries where there is a safeguarding concern
Hosting safeguarding adults boards (multi-agency partnerships in the UK, established under the Care Act 2014, to protect adults with care and support needs from abuse and neglect by coordinating local safeguarding efforts).
Carrying out safeguarding adults reviews
Arranging for provision of independent advocates
Leading a multi - agency local adult safeguarding system
Why is partnership important within healthcare?
Improves the lives of vulnerable adults and children
Improves the efficiency of the care system as a whole systemas a whole because patients don’t have to give the same info to different health and social workers.
helps the service user feel the way are being treated as a whole person (Hosltic care.
What are the difficulties of partnerships?
Failure to communicate information between services, for example, between social workers and the police in cases where children are in danger.
Lack of coordination of health and social care services so people do not receive the care they need or experience duplication.
Cuts in funding that prevent effective partnership working, computers or not enough equipment, not enough employees.
What is a holistic approach?
A holistic approach takes account of people’s wider needs (physical, intellectual, emotional, social, cultural and spiritual) and seeks to meet these needs to promote health and wellbeing.
What are some examples of actions included in some holistic approaches?
Most people only want their particular illness or symptom treated.
Generally, doctors do not look for other issues during diagnosis
Health and social care workers are not employed or skilled to manage all aspects of an individual’s needs.
Advocacy
Service users, their carers and other advocates should be involved in decision-making and planning support with service providers, working in partnership. Advocacy allows people to :
Express their views and concerns, so that they are taken seriously.
Access info and services
Defend and promote their rights and responsibilities
Explore choices and options
Why is monitoring care internally important and what are the internal monitor roles?
Lead nurses or senior nurses are in charge of a group of wards and can deal with a problem if the ward staff are unable to do so.
Doctors are medical consultants who oversee diagnosis, investigations and treatment.
Matrons are in charge of a group of wards and take responsibility for ensuring excellent patient experience and safety.
What’s whistleblowing within healthcare and why is it done?
Whistleblowing can take place in both social care and health settings. In a health setting, for example, a staff member may raise concerns about patient care, such as when the health and safety are put at risk. These concerns are reported to the relevant staff in the hospital, such as a senior nurse, a docter or one of the hospital managers.
When they are not followed:
Bad practice could continue, harming individuals
There will be more complaints from service users about their representatives.
Staff may leave or perform less well
The service provider may receive more negative reports.
Whistleblowers are protected by law and should not be treated unfairly or lose their jobs.