Gamma camera/RNI
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
32 Terms
what is nuclear medicine
The use of radiopharmaceuticals to diagnose and treat patients
•Diagnosis:
–Imaging techniques that use and look at physiology
–Non imaging techniques that work by indirect diagnosis
•Treatments:
–Therapies such as I131 for hyperthyroidism
–Y90 microspheres for liver tumour palliative treatment
A radionuclide is attached to a pharmaceutical that will seek out a target organ.
The pharmaceutical is physiologically used in some way by the target organ, it transports the radionuclide to the organ under investigation
Why are alpha emitting radioactive isotopes not used as radiotracers?
alpha emitting radioactive isotopes are composed of a helium nucleus - have poor penetration power and are stopped by a few cm of air and have high ionization potential.
beta is composed of an electron and are stopped by a few mm of aluminium
gamma is composed of electromagnetic wave and is stopped by thick lead
why is technetium-99m suitable as a radiotracer
Tc-99 has a half life of 6 hours which is a long enough time to allow the patient to be injected and imaged in a gamma camera on the same working day. The half life is short enough to ensure the patient is not radioactive for too long. It does not emit alpha particles. Tc-99 emits gamma-rays which can escape the body and be detected by the gamma camera for imaging. One advantage of Tc-99 is that it can be combined with a variety of pharmaceuticals to creates radiopharmaceuticals that the patient is injected with.
what is radiopharmacy
•Responsible for the production of radiopharmaceuticals
•On-site is ideal, but many nuclear medicine departments are supplied by a central radiopharmacy
•Tc99m Generator delivered
–Every morning it is eluted
–Tc99m is bound to the pharmaceuticals required for the days investigations
–Technologists carry out production
–Rigorous checks required before dispatch
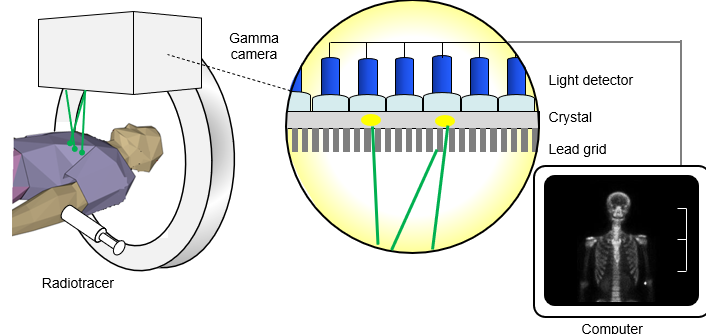
whats the purpose of the gamma camera
•Used to detect gamma emissions produced by radionuclides that have been administered to the patient
•Images are produced of the distribution of the radioactive substance within different organs and systems
•This can be compared with normal distribution to diagnose if a medical condition is present and assess its extent or severity
what are dual head system gamma camera
Increased patient throughput
Reduced risk of patient movement on various scans
Optimal for Single Photon Computerised Tomography (SPECT) examinations:
• Cardiac (Myocardial Perfusion)
• Bone (Lumbar Spine)
• Tumour & Infection (MIBG/In111/NeoSpect)
• Neurology (DAT scans – I123 / Ceretec – Tc99m)
Cost – Can be relatively expensive (£250,000)
what are single headed gamma camera systems
Useful for small enclosures
Useful for paediatric imaging
Mobile systems
Cheap/cost effective for small departments
Drawbacks include increased scan time &risk of movement (ie cardiac imaging)
what are hybrid camera?
•Gamma camera 3D functional imaging in SPECT mode
•CT provides detailed 3D anatomical information
•Combine – show location, size shape of functionally active lesion
•Lots of applications in oncology
whats the light detector,crystal and leas grid
what are the reasons for bone imaging?
•Radiopharmaceutical: Tc99m HDP binds to osteoblast activity
•Activity: 400-800MBq
•Common reasons for scan:
–? Mets
–? Metabolic bone disease e.g. paget’s
–? Stress fracture
•Continuous/static scan (imaged with a delay)
•Can also be dynamic
•Scans last approx 20 – 30mins
•SPECT/CT can be used for localisation
gamma camera basics
•Collimators
•Scintillation Crystal
•Light Pipe/Guide and Optical Coupling
•Photomultiplier Tubes and Dead Time
•Gamma Ray Event Positioning
•Spatial Resolution
•Pixel Size
whats the gamma camera head
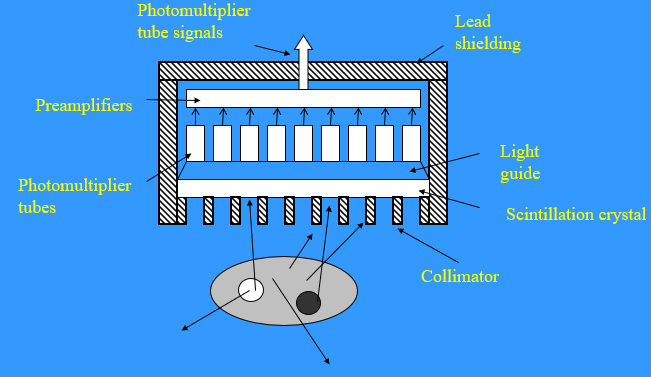
what are gamma camera basics
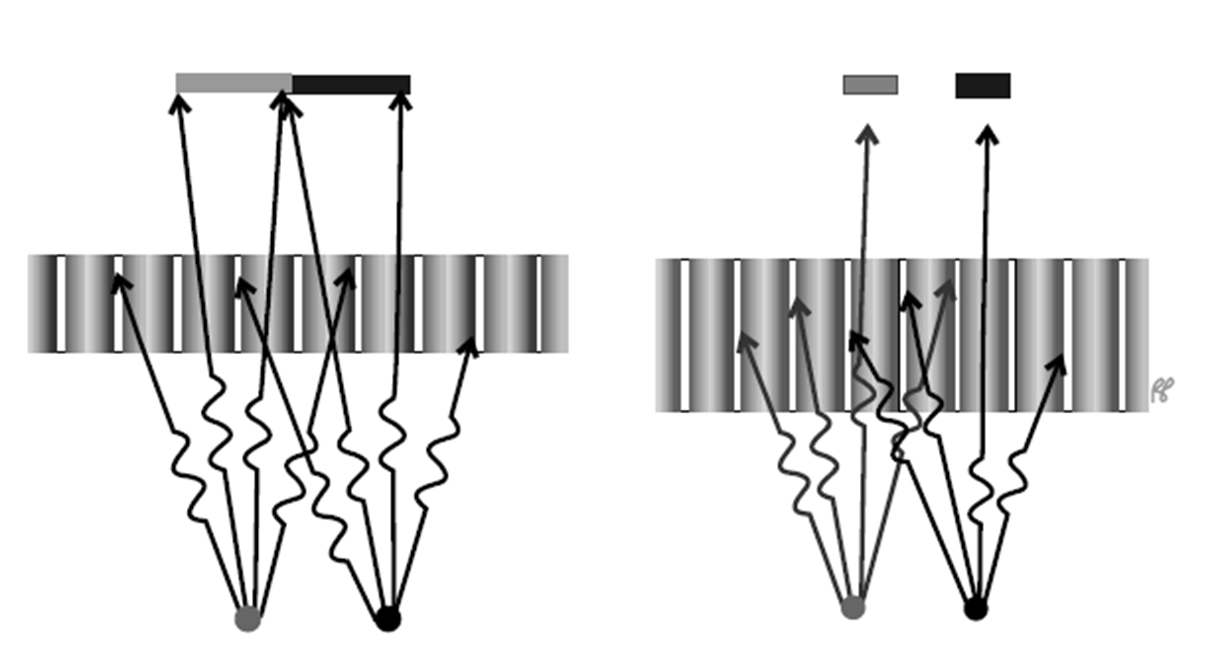
1.Require image of distribution of a gamma ray emitting tracer within patient
2.Only gamma rays travelling parallel to holes in the collimator pass through to crystal
3.Gamma rays interact with sodium iodide scintillation crystal (thalium doped) leading to the scintillation of visible light photons (1000s of ~410nm photons)
4.Light photons pass through Light Pipe / Guide towards Photomultiplier tubes (PMTs)
5.A current is produced in the PM tubes proportional to number of light photons produced by scintillation in crystal. Each PM tube produces output signal
6.Information on position and gamma ray energy are determined by camera by analysing signals from all PMTs
7.Scatter is rejected by only accepting gamma rays with energies inside a preset energy window
8.Image of gamma ray emitting tracer is produced for set matrix size
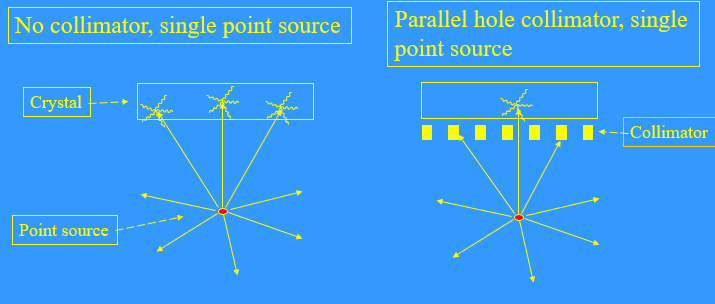
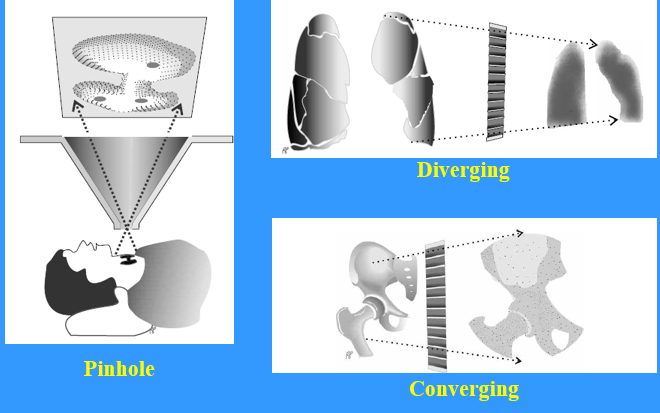
what are the different types of collimator design
•Different types: parallel hole, pinhole, diverging and converging collimators
•Material – usually holes drilled or cast in lead / Shaped lead foils
•Holes - usually hexagonal, occasionally triangular - can closely pack square holes for higher energies
•Septa - lead between the holes,
•Aim for 99% absorption with about 0.25 mm of lead for Tc99m (140 keV)
what are parallel hole collimators
•Parallel Hole collimators are the most commonly used in nuclear medicine.
•In parallel hole collimators the holes are parallel to each other and at 90 degrees to crystal.
•There is a fixed relationship between object size and image size (1 to 1)
•The energy of the radionuclide being imaged is the main determinant of septal thickness
•Sheet of lead with holes in positioned between patient and crystal
•Only gamma rays travelling parallel to the collimator holes pass through to the crystal
•Hence the position of gamma ray absorption in the scintillation crystal is related to position of the gamma source in body and hole geometry
whats the function of the collimator
Function is to map the 3-D radioactive distribution in the patient onto a 2-D representation on the crystal
what are different types of collimator used for
things to consider when choosing the right collimator
•Is a special collimator needed ? ( e.g. for a small superficial organ, use the pinhole)
•What energy will be imaged ? - only consider collimators with a septal thickness that gives <5% septal penetration
•Does the image require optimised count density or resolution ?
–for count density, use high sensitivity (or general purpose)
–for resolution, use high resolution
how is collimator performance described
•Sensitivity – ratio of the number of gamma rays passing through holes to total number emitted by source (incident on collimator) - Unit of counts /sec / MBq
•Resolution – This is the resolution limitation of the detector. Worsens with increasing distance. It can be measured by calculating the size of the FWHM of a line source.
•Different collimators with different septal thicknesses are used for different energy
•There is a trade-off between sensitivity and resolution.
how does hole length affect performance
The longer the bore, the higher the resolution - for the same hole diameter.
what is the properties of the scintillation crystal
Must “scintillate” - i.e. absorb high energy gamma photons and emit the energy as a number of lower energy light photons
•Best if it has a high attenuation coefficient - i.e. high atomic number and also good conversion efficiency
•Must be transparent to light
Most common scintillator in gamma cameras is sodium iodide with traces of thallium impurities - NaI(Tl)
•One property of materials that scintillate is that the number of light photons emitted is proportional to the energy deposited by the gamma ray. This property allows discrimination against gamma photons arising from scatter events
•Thick crystals have higher efficiency but poorer spatial resolution
•Thin crystals have lower efficiency but better spatial resolution
what is NaI(T1) crystal
•NaI (doped with thallium) - high attenuation and conversion efficiency of photons (Max Emission Peak ~415nm)
•Disadvantages: hygroscopic - needs to be sealed in an aluminium can, also cannot withstand rapid changes in temperature or mechanical shock.
•Can degrade or yellow over time - 10 years.
•Thickness - 6 or 13 mm - thicker crystal for higher energies. Also would want it thin to reduce light spread from PMT as this effects the intrinsic resolution. It is easier to calculate the position of a gamma ray scintillation event with a thinner crystal. (Tradeoff)
•Most gamma cameras are designed for optimal detection of γ ray energies of 100-200keV. (Tc99m ~140 keV)
what is the light pipe/guide
•The light Pipe/Guide acts as an optical coupling between the exit window of the NaI(Tl) crystal and the PM tubes
•The light guide increases the light efficiency , by channelling scintillation light away from gaps between PMT tubes and improve uniformity of light collection as function of position
•Made from a transparent plastic such as quartz impregnated Plexiglas
•To obtain the best possible resolution it should be as thin as possible and match the refractive index of the crystal
what is optical coupling?
•An air/solid medium interface would drastically reduce the amount of light reaching the PM tubes due to total internal reflections
•So the crystal is coupled to the light guide, and the light guides to the PM tubes, by an optical coupling material, usually silicone grease or oil.
•There must be no air bubbles between surfaces as these will allow internal reflection.
•Over a period of time the coupling grease may harden altering its refractive index and affecting light transmission. Then the detector must be dismantled and re-greased.
what are photomultiplier tubes (PMT)
•Converts scintillation light into an electrical signal
•Contains a photocathode, array of dynodes and an anode.
•Photocathode - converts light flashes (Max Emission Peak ~415nm) produced in the crystal into electrons
•The dynode array is used for electron multiplication
•The anode collects the electrons.
•Light detection signals are outputted from each PMT
Light entering the PMT displaces a photoelectron which is electrostatically focused to the first-stage dynode. Each dynode has a positive voltage bias relative to the previous one, and so electrons are accelerated from one dynode to the next. The increase in kinetic energy acquired by this process is sufficient to displace a number of electrons at the next dynode, and so on, causing large amplification by the end-stage dynode.
how are electrons accelerated in PMTs
•Light strikes photocathode and ejects an electron
•Electron accelerated by the high voltage on the 1st dynode
•On striking the 1st dynode, the electron knocks off a few more electrons
•Each of these electrons is accelerated towards the second dynode where each knocks off a few more electrons
This process is repeated for ~ 12 or more dynodes, producing a large pulse of electrons at the output
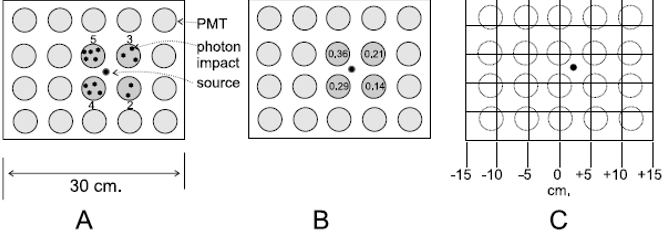
•Uses 30 to 100 vacuumed PMTs , ~ 50 – 60 mm diameter
•Intrinsic resolution higher for higher number of PM tubes
•PM tubes smaller than 50 mm are inefficient. Too many PMTs can introduce unacceptable noise in the light detection process. More dead space.
•Costly to have large numbers and more electronics which could go wrong
•Each PMT outputs X, Y and Z signal for each detected gamma ray interaction. X and Y signals are used to calculate a scintillation position while the Z signal represents the energy of the detected pulse
•Analogue to digital converters are used to convert the analogue X, Y and Z signals into digital form before processing in a modern gamma camera
gamma ray event positioning
•Gamma-ray interacts with crystal at source.
•4 PMTs receive light photons.
•Upper left recieves the greatest number – 36% in total.
•Actual location of interaction is ~2.5 cm from the crystal center in X+ direction.
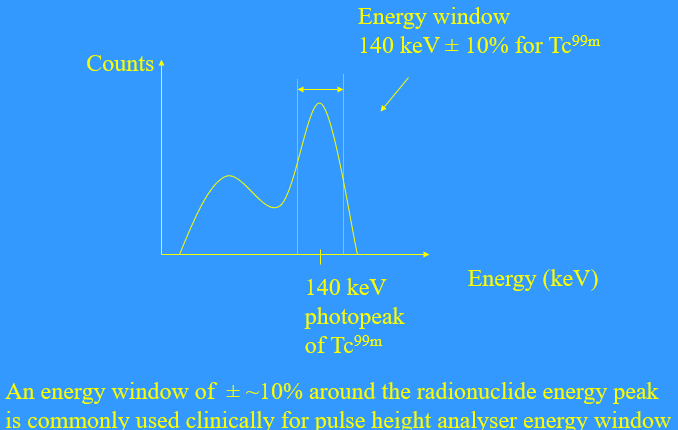
what is the pulse height analyser
•Pulse Height Analyser is used to reject all detected gamma rays outside a set energy window around the radionuclide energy
•Energy window depends on energy resolution
•Gamma camera detects gamma rays scintillation events in crystal with an energy spectrum
•Most of the spectrum is Compton scatter
Only the non scattered detected gamma rays are used in the final image / dataset
Energy spectrum of Tc 99m detected by gamma camera
what is matrix/pixel size
•Use 256 matrix for bones where likely to encounter high spatial frequencies.
•Dynamic images - short frames, low counts use 128 matrix.
Question: Calculate the approximate pixel size of a gamma camera FOV that is 50cm by 50cm for 64 by 64, 128 by 128 and 256 by 256 imaging matrices.
Answer:
64 by 64 matrix = 50 cm / 64 pixels = 7.8 mm / pixel
128 by 128 matrix = 50 cm / 128 pixels = 3.9 mm / pixel
256 by 256 matrix = 50 cm / 256 pixels = 2.0 mm / pixel
512 by 512 matrix = 50 cm / 512 pixels = 1.0 mm / pixel
Thus the pixel size in either the X or Y direction decreases from 7.8 mm in a 64 by 64 matrix to 1.0 mm in a 512 by 512 matrix.
•A matrix cannot resolve points separated by less than 1 pixel.
Maximum resolution of the image is limited by the resolution of the camera and collimator
what are the different imaging modes
•Different imaging modes- static, dynamic, single photon emission computed tomography (SPECT).
•Static – Patient is placed such that region of interest is in the detector’s field of view.
–Can have different views (sometime angled), eg anterior and posterior.
–Data are collected for a specific amount of time or number of counts.
•Dynamic –
–Type of video recording to catch images of fast action.
–Data are acquired in rapid sequential frames allowing change in change in distribution of radiopharmaceutical over time to be observed and quantified-eg passage of tracer through the kidneys.
what are External Factors To the gamma camera affecting image quality
•Low counts - obese patient
•Patient movement
•Acquisition parameters
•Poor injection-extravasation-tracer usually injected into a vein (elbow or hand/foot).
•Extravasation occurs if not all of the tracer enters the vein and ends up in the surrounding tissue.
what are the acquisition parameters
•Type of acquisition – static (how many views) /dynamic/SPECT
•Type of collimator – parallel hole/pinhole etc.
•If parallel hole – high resolution or high sensitivity
•Pixel / Matrix size – Choose pixel size to match the required maximum spatial frequency in patient
•Time of acquisition – long enough to obtain adequate counts – not too long or patient may move.
•Dynamic frame time depends on physiological system being imaged.