Lacrimal System
1/83
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
84 Terms
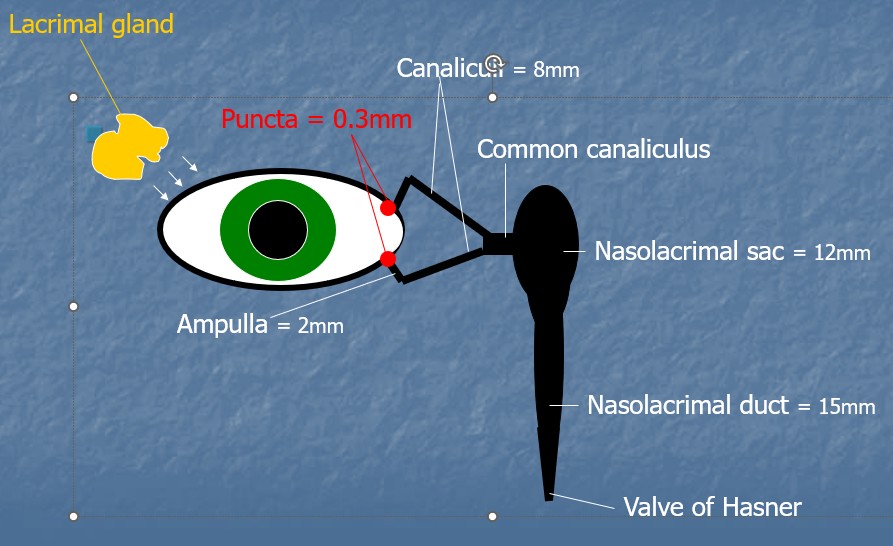
Schematic Diagram of the Lacrimal system
Function of the lacrimal system?
Main aqueous producer for the tear film - aided by accessory glands Krause and Wolfring
Contain 6-12 ducts - originating in orbital lobe and ending in the superior conjunctival fornix
What is the lacrimal system innervated by?
Ophthalmic division of the trigeminal nerve
Emotional response - tearing - lacrimal system receives afferent fibres from hypothalamus
Facial nerve also has some control over lacrimal gland in Bell’s Palsy = dry eye
What is Bell’s Palsy?
7th nerve palsy
Inability to close the eye - DRY EYE
Inability to smile
Inability to puff cheeks
What is dacryoadenitis?
Rare inflammatory condition of lacrimal gland - sx of swelling and blurred vision, dry eyes + watery eye
Acute form can be bacterial (staphylococcus/gonococcus) or viral (mumps/herpes simplex)
Chronic - due to non-infectious inflammatory disorders e.g sarcoid, thyroid eye disease

What is a lacrimal gland tumour?
From epithelial cells that line the lacrimal gland
50% Benign, 50% Malignant
Commonly present in 3rd decade or teenage years
Very rare
Sx of lacrimal gland tumour?
Proptosis - eyes bulge from natural position
Dipl + distorted vision
Pain

Function of the TF?
Lubricates the globe
Provides smooth pre-corneal refracting surface
Removes Debris from ocular surface
Provides Microbial Defence
Helps regulate temperature of globe
Size and function of Mucin layer
Innermost layer - 0.5 micrometres in thickness
Wets the microvilli of of corneal epithelium
Helps prevent pathogen adhesion to epithelium
Contributes to regulation of epithelial growth
Size and function of Lipid layer
Outermost layer
0.2 to 0.9 micrometres in thickness
Inhibits aqueous evaporation
Hydrophobic barrier - prevents overspill of tears
Size and function of Aqueous layer
Middle layer - 6.5 to 7.5 micrometres in thickness
Provides nourishment of avascular cornea
Microbial defence and washes away foreign bodies/debris
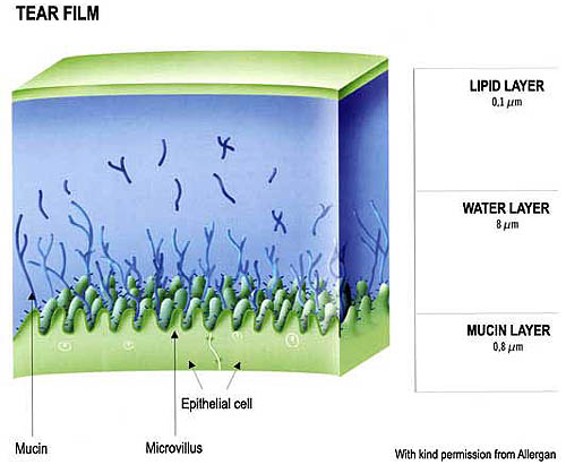
IMG of the TF layers
Modern day thoughts about the aqueous and mucin layers?
Now considered a single layer of mucoaqueous gel
Decreasing mucin concentration towards the lipid layer
What is the Mucin layer produced by?
Conjunctival goblet cells
Crypts of Henle
Glands of Manz
What is the Aqueous layer produced by?
Lacrimal gland
Accessory glands of Krause and Wolfring - serve as backup
What is the lipid layer produced by
Meibomian glands,
Glands of Zeiss and Moll
Where are the accessory glands of Krause and Wolfring located?
Krause - superior fornix
Wolfring - Tarsal conjunctiva - above the top edge of the tarsal plate
What does the Aqueous layer contain to provide microbial defence?
Lysozyme - enzyme which destroys gram +ve bacterial cell wall e.g Staphylococcus, Streptococcus
Immunoglobulins - IgA is the main immunoglobulin - Act as an antibody by binding onto pathogens and neutralising
Lactoferrin - mops up iron which leads to bacterial death
Beta-Lysin - protein that destroys whole bacterial cell
What happens to microbial defence in ADDE?
Defence proteins are decreased = eye more vulnerable to infection
Where are the meibomian glands located and how do they secrete lipids?
Located within tarsal plate
25 upper lid, 20 lower eyelid
Secrete lipid via duct and orifice
What are Glands of Zeiss and Moll?
Backup to meibomian glands in lipid secretion
ZEISS - Discharge into each eyelash follicle
Moll - discharge via duct to surface of eyelid
What is the tear volume?
7-10 microliters
Majority is the in the upper and lower marginal tear strips e.g tear meniscus height (5-6 microliters)
What does Tear Meniscus height show?
Reliable predictor of tear volume insufficiency
Normal height around 0.45mm
Dry eye around 0.24mm
Definition of Dry eye
Loss of homeostasis of the TF leading to;
TF instability
Hyperosmolarity
Ocular surface inflammation
Damage
What is hyperosmolarity and what is the threshold between normal and Dry eyes?
Osmolarity is an objective measurement of salt concentration in Px’s tears
Hyperosmolarity is indicative of reduced aqueous levels
308mOsm/L is the threshold
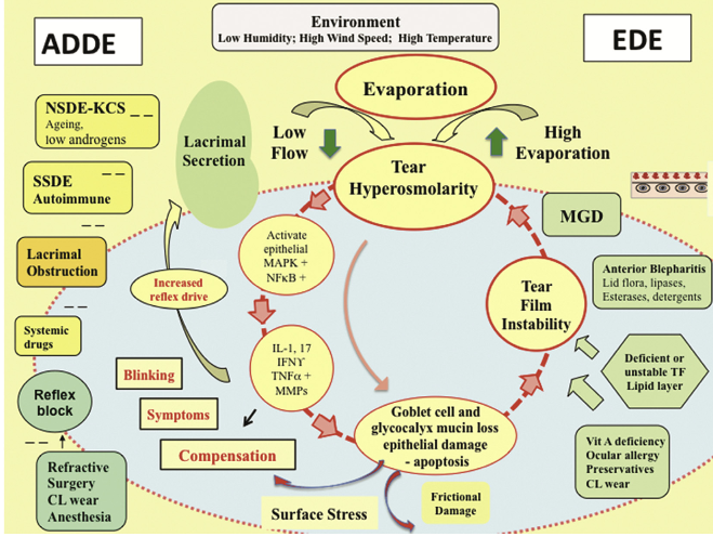
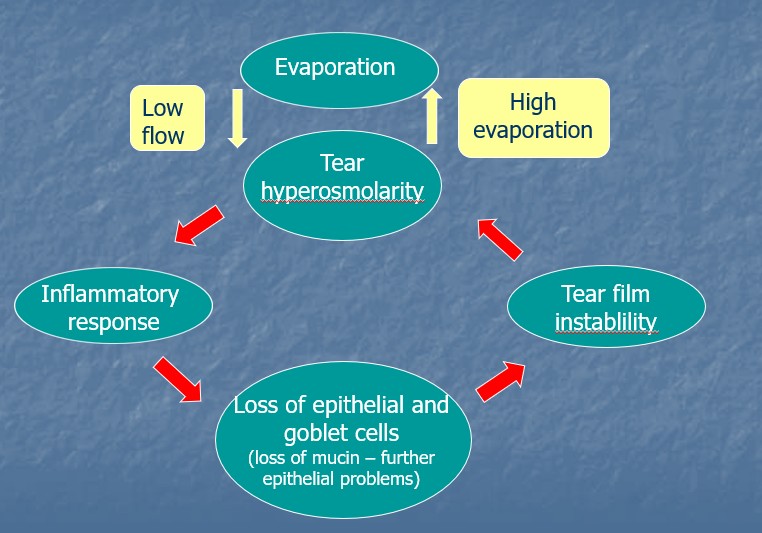
Diagram linked ADDE and EDE
ADDE
Insufficient secretion rate from lacrimal gland - tear drainage exceeds production
Leads to keratoconjunctivitis sicca
Can be caused by;
Atrophy of lacrimal glands (Age related or pathology)
Reduced neural input to gland (Rx surgery)
Poor tear retention due to eyelid abnormality
EDE
Deficient Lipid layer - MGD
Deficient Mucin layer
Contamination of the tear film by environmental factors; airborne pollution, irritants/chemicals
Why does MGD lead to EDE?
Reduced rate of lipid secretion due to an increase in viscosity (orifices)
Without lipids in TF, evaporation is not prevented
70% of chronic DE due to MGD
Why might MGD occur?
Hormonal changes - change in oestrogen levels lead to thickening of the oils
Change in oestrogen levels also increase the amount of staphylococcal bacteria resulting in MG inflammation
Blepharitis
What has recent research shown regarding MGD?
Hormone Androgen involvement - control MG secretion - precursor to Oestrogen
Deficient androgens = loss of lipid layer due to thicker, more viscous secretions
Px taking antiandrogenic therapy e.g has prostate disease results in DED
What happens if MG is lost?
Irreversible changes once atrophied
What causes MG dropout?
Radiation therapy / Chemotherapy
Cases of ADDE?
Taking systemic drugs
Refractive surgery
Ageing
CL Wear
Cases of EDE?
Vitamin A deficiency
Ocular Allergy
Preservatives
CL Wear
What are the similarities and differences between ADDE and EDE?
ADDE and EDE exist continuously and are part of a cycle
ADDE - lacrimal function issues - not enough production of tears
EDE - lid related (MGD, blink rate) and ocular surface (mucin production and CL wear)
Cause of Dry eye?
Deficient tear volume (ADDE)
Deficient tear quality (EDE)
Abnormal eyelid function - (ADDE)
Systemic disease / Medication
Environmental factors e.g humidity
Refractive surgery
Treatment for MGD
Hot compress - Eye bag / rice bag
Massage lids after heating
Treat any blepharitis - lid wipes/cotton buds
Flaxseed oil
What is an Internal Hordeolum?
Tender inflamed swelling within the tarsal plate
Bacterial infection (usually staphylococcal) of Meibomian gland
More painful than stye
May point anteriorly through the skin
What is a Chalazion (Meibomian Cyst)?
Cessation of lipid secretion due to total blockage of MG ducts leading to a stagnation of meibomian gland contents
Focal, hard, painless nodule
Non-infectious, granulomatous inflammation of meibomian gland
May develop from retention of gland secretions
Why might a Deficient Mucin layer occur?
20 mucin synthesizing genes - defect in these genes may be a factor in DE
Loss of Goblet cells
Vitamin A deficiency
What can cause Loss of Goblet Cells?
Steven-Johnson syndrome
Pemphigoid
Burns
Trachoma
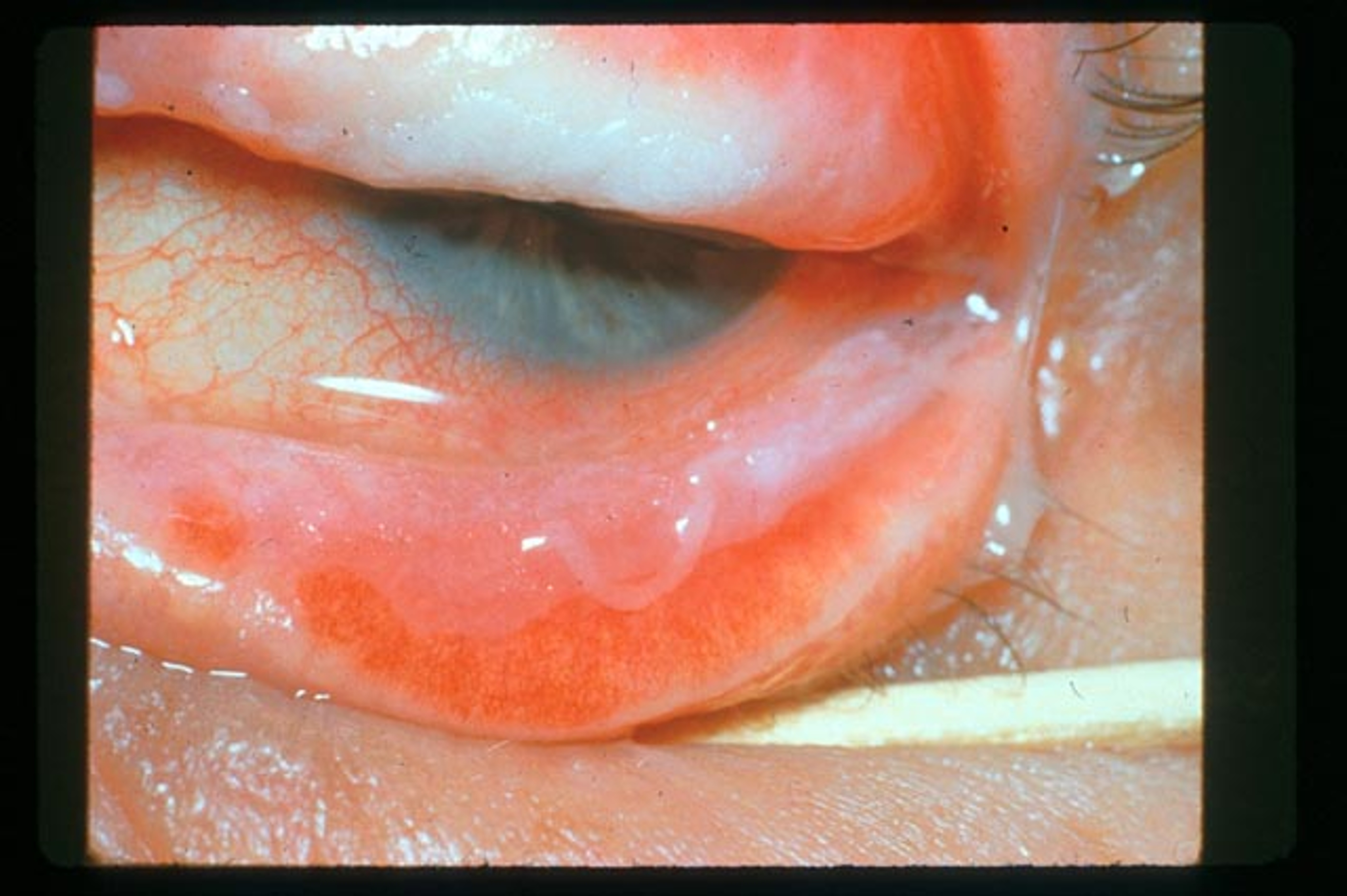
What is Steven-Johnson syndrome and RF?
Disorder of the immune system caused by an adverse reaction to drugs and viruses e.g herpes simplex
Hypersensitivity of mucous membranes and skin - MUCIN DEFICIENCY
Males more susceptible (2:1)
Signs of;
Papillary conjunctivitis
Dry eye
Epiphora following lacrimal drainage obstruction
What is Pemphigoid and its RF?
Systemic autoimmune inflammatory disease - ‘blister’
Usually bilateral
Females - mainly in the 7th decade - females more prone to autoimmune conditions - rule!!
What is Trachoma?
Caused by the bacterium Chlamydia trachomatis
Spread by direct contact with eye, nose and throat secretions from affected individuals or items they have used
Also spread by flies

Vitamin A deficiency
Leads to build up of Keratin Debris - common in children in developing world
Bitot’s Spots
Interpalpebral conjunctival foamy looking patches
Can eventually lead to corneal ulceration

What does Abnormal eyelid function lead to?
Poor post-blink redistribution of TF
Poor tear pump mechanism
Large palpebral aperture e.g in ectropion / thyroid eye disease - elevated tear evaporation due to greater exposed ocular surface - resulting in DED and epiphora
Elevated tear secretion rate e.g entropion = corneal irritation leading to reflex lacrimation - resulting in epiphora
What systemic diseases cause Aqueous deficiency?
Sjogren’s Syndrome
Systemic lupus erythematosus
What is Sjogren’s syndrome?
Autoimmune disorder affecting primarily salivary and lacrimal glands - DRY EYE; AQUEOUS DEFICIENCY
Joints and muscles affected by mild arthritis
Females 90% of cases, onset most commonly in 40s

What is Systemic Lupus Erythematosus?
Autoimmune disorder can affect multiple organ systems such as heart, skin, joints and nervous system
May have butterfly rash on forehead and cheeks
DRY EYE; AQUEOUS DEFICIENCY
Can only treat sx, no cure
Females 90%
What is Rheumatoid Arthritis and its Ocular issues?
When the body's immune system targets affected joints which leads to pain and swelling - AUTOIMMUNE
Females 3x more affected
Ocular manifestations occur in 25% of cases
Keratoconjunctivitis sicca in 15-25% cases
Episcleritis 0.17%
Scleritis 0.67%
No correlation between DED and RA

Management of Px with DED and RA?
Ocular lubricants - if not responsive to treatment - mild topical steroid 2-4x daily
What is hyperthyroidism?
Overactive thyroid gland
Swelling of EOM
Proptosis - eye bulges out
Inadequate globe coverage by eyelids = incomplete blink

What environmental factors lead to DED?
VDU use
Air Conditioned offices and cars - reduced humidity
Pollution - increase tear debris + reflex lacrimation = epiphora
Wind
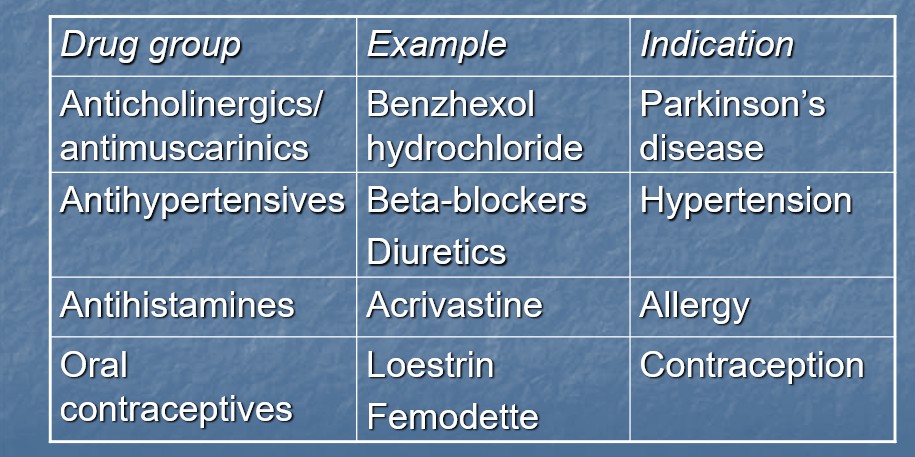
Medicines causing dry eyes?
What is the link between Rx surgery and dry eyes?
Reduction in rate of tear secretion - anterior corneal nerve plexus damaged during surgery = reflex lacrimation rate reduced
Damage to corneal epithelium = mucin layer disrupted = localised reduction in corneal wetting
Sx of Wet eye?
Excessive tearing
Itching
Soreness of skin below eye
Wet eye Sx can be worsened by?
Wind
Cold conditions
What tests can you use to evaluate the tear volume?
Schirmer test
Color Bar test
Phenol red thread test
Tear meniscus
Ocular surface assessment (staining agents)
Schirmer test 1 without anaesthesia:
Measure of basal and reflex tear secretion
Fold schirmer strip at notch and hook over temporal part of lower eyelid
Leave in place for 5 mins - encourage normal blinking
Greater than 10mm of wetting = normal
5-10mm of wetting = borderline dry eye
5mm or less = dry eye
Schrimer test 1 with Anesthesia:
Measure basal lacrimation only
Instil one drop of 0.5% proxymetacaine HCL
Expect lower level of secretion compared to without anaesthesia
5mm or less in 5 mins = borderline dry eye
Schrimer test 2:
Direct measure of reflex lacrimation
Instil 1 drop of 0.5% proxymetacaine
Stimulate nasal mucosa with cotton bud for 15-20 seconds
Measure tear secretion after 2 mins
Normal if greater than 15mm of tear secretion in 2 mins
What is the Phenol Red Thread test?
70mm thread impregnated with phenol red
Yellow when dry, red once wetted by tears
Hook over lower eyelid such as Schrimer test for 15 seconds
Less than 9mm of wetting = dry eye
Less than 5 seconds TBUT is indicative of?
KCS
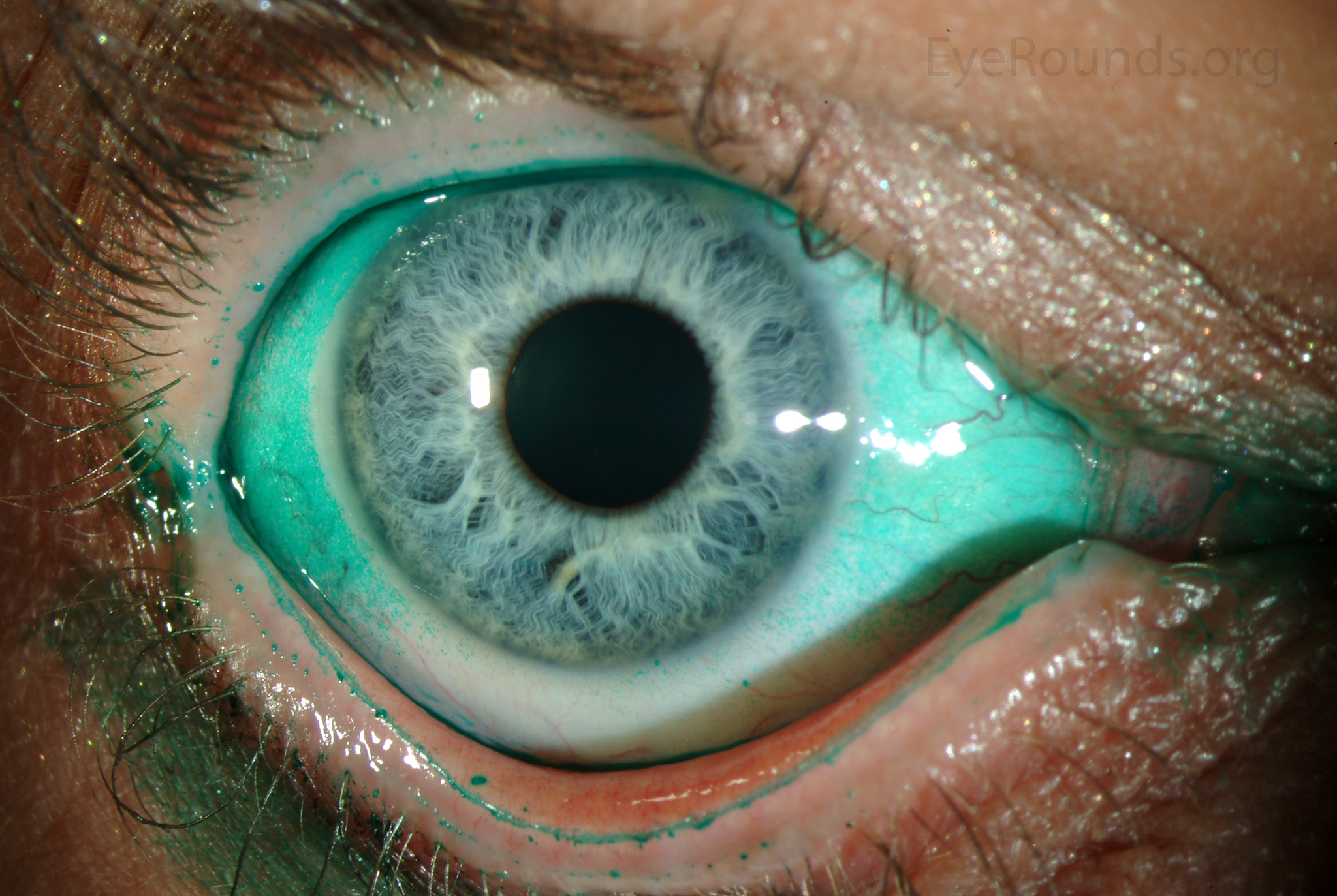
How do the different staining agents work?
Fluorescein - stains damaged cells
Rose Bengal - stains dead cells, mucus and mucin-deficient tissues - shows devitalized epithelial and conjunctival cells - incomplete blinking - stings but gold standard for detection of ocular damage due to dry eye
Lissamine Green - stains damaged cells, dead cells and mucus - much more comfortable than RB and also gold standard
How should you use lissamine green?
Staining fades quickly so assess one eye at a time
Assess 1-4 mins after instillation
Use a Wratten 25 filter
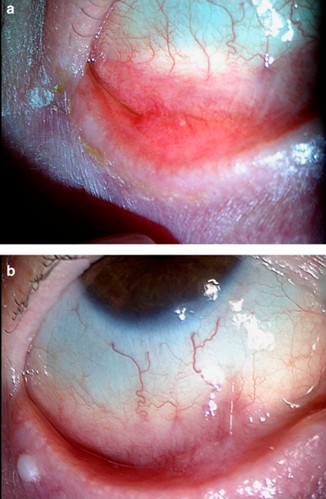
Signs of Keratoconjunctivitis Sicca;
Bulbar conjunctiva stains first
Temporal and inferior cornea stain as disease progresses
Signs of Bacterial Keratoconjunctivitis sicca?
Diffuse punctate staining
Management of tear dysfunction?
Increasing tear volume and ocular lubrication - Artificial tears, Dietary changes
Reducing rate of tear fluid loss from conjunctival sac - Punctual occlusion, alter environment/eye shield
Improvement of tear quality /consistency - Lipid layer deficiency - use hot compress, lid massage
Improvement of lacrimal drainage in cases of epiphora
Formulation of artificial tear substitutes?
pH 7.4
Tonicity 0.9% sodium chloride
Viscolizing agent - substitute for mucin
Preservatives - prevent bacterial colonisation once opened
Examples of artificial tears
Systane Polyquad - preservatives (can cause irritation) - contain Polyethylene Glycol - can get on the NHS
Hycosan - sodium hyaluronate 0.1%
Hyabak - sodium hyaluronate 0.15%
Artelac - Hypromellose 0.32%
What Dietary changes can we advise?
Omega-3 fatty acids - soften secretions from MG
Increase water intake
Flaxseed oil
Fish oil
Oily fish - tuna, salmon, sardines
What are the 2 types of silicone punctal plugs?
Freeman type
Herick type
Reducing rate of tear evaporation; Changing temperature/surgery/optical
Use of room humidifiers
Reduce room temp
Computer breaks!
Reduce palpebral aperture area - lateral tarsorrhaphy
Everest-Harris specs - side shields reduce evaporative effect of wind
Where do tears drain from?
70% drain via inferior canaliculus - gravity
How to investigate the drainage system?
Dilation and irrigation
lacrimal syringing
lacrimal lavage
can also have therapeutic value - dislodge mucus
Jones Dye test - 1 and 2
Interpretation of Dilation and Irrigation?
Px feels saline in throat - drainage system is fine - D&I has cleared obstruction
if fluid regurgitates through upper punctum - blockage exists in/beyond the common canaliculus
IF fluid regurgitates through Lower Punctum - blockage exists between inferior punctum and common canaliculus
Jones Dye Tests
Used in cases of suspected obstruction of lacrimal drainage system
Carried out after dilation and irrigation procedure
Results Jones Dye Test 1
Dye detected initially after 5 mins = normal drainage
Dye detected after massage and nose blow = partial obstruction of nasolacrimal duct
If no dye present carry out Jones Dye Test 2
Results of Jones Dye Test 2
Dye present in collected fluid = functional blockage of nasolacrimal duct - fluid flow only under high pressure
Fluid present but no dye = functional blockage of nasolacrimal duct = site of blockage is close to punctum
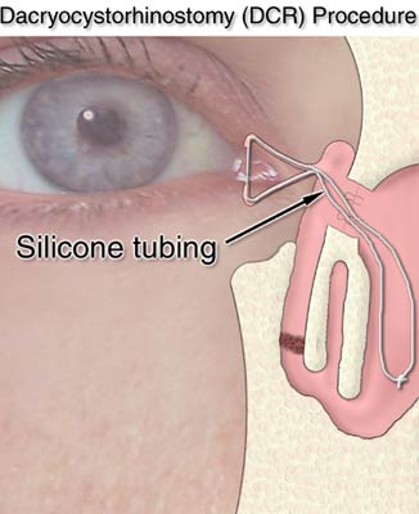
What happens if Dilation + Irrigation doesn’t work?
Dacryocystorhinostomy
Hole drilled into nasal cavity - silicone tube inserted to maintain drainage
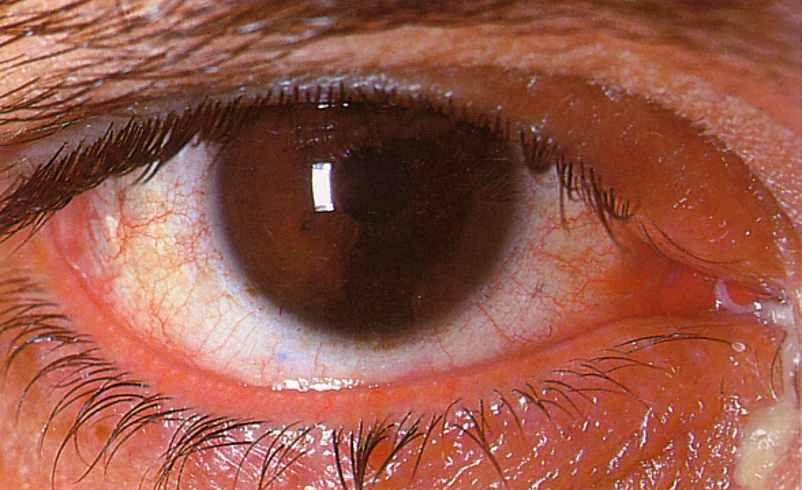
What is canaliculitis?
Inflammation of the canaliculi - relatively rare
Px over 50s
Signs include - chronic unilateral red eye with epiphora - mucopurulent discharge, more likely to be inferiorly
Can get dacryoliths building up - form pockets and block drainage
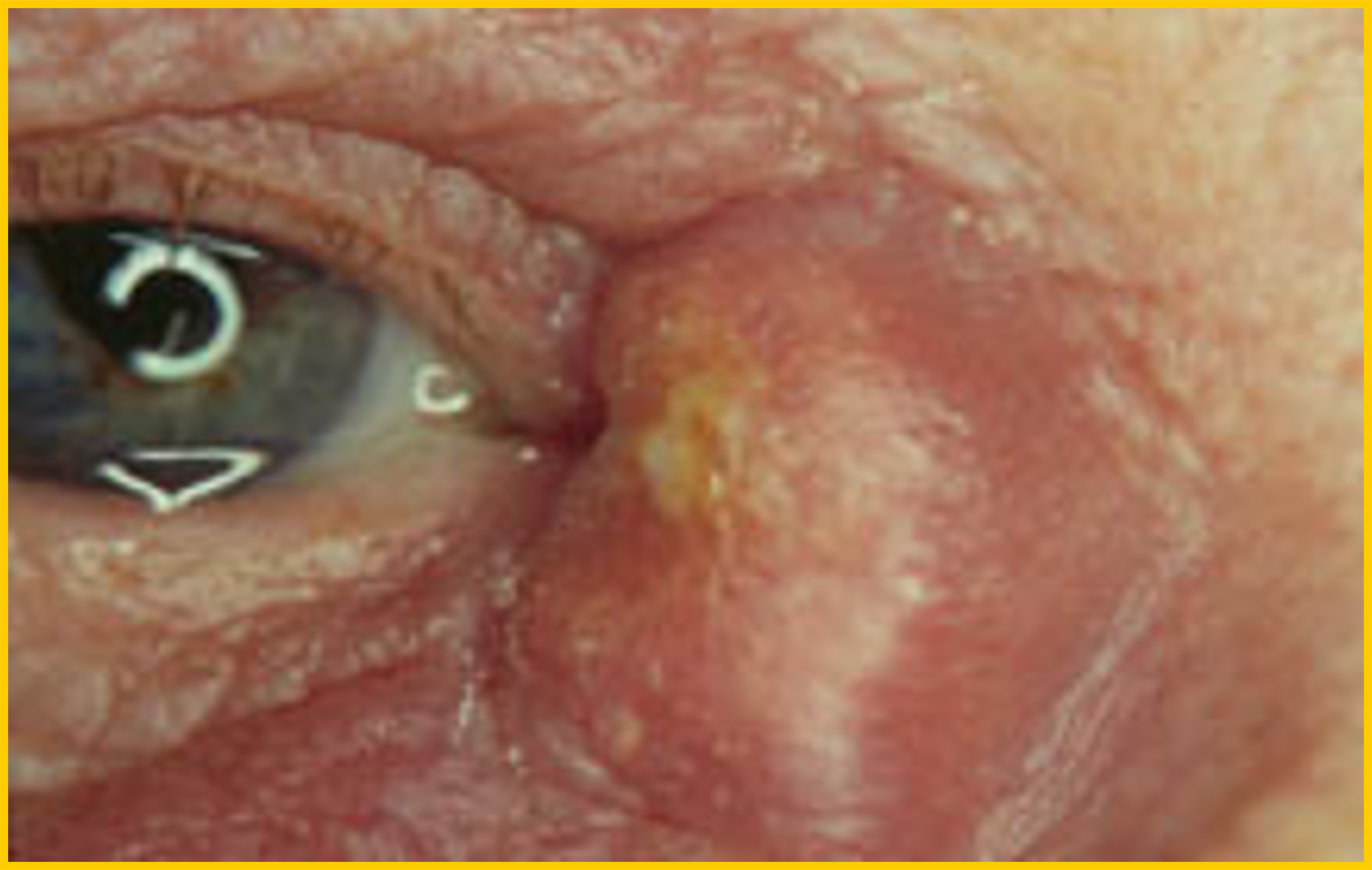
What is Dacryocystitis?
Bacterial infection within the nasolacrimal sac
Rare - occurs when nasolacrimal duct is blocked
Acute - painful swelling at medial canthus, sac full of pus - treated with antibiotics, warm compress and dacryocystorhinostomy
Chronic - conjunctivitis with epiphora, sac filled with mucoid material - treated with dacryocystorhinostomy
What is a Nasolacrimal Sac tumour?
Interferes with tear drainage - epiphora
Rare
Needs complete excision followed by radiation
Congenital occlusion common - often spontaneously resolves - 70% by 3/12, 90% 12/12