Eating Disorders
1/67
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
68 Terms
what are eating disorders?
a form of mental disorder characterized by problems with eating
as a group, eating disorders distinguished from normal variations in eating bas4ed on at least 1 of the following
present distress
disability/impairment
eating disorders in the DSM-5
anorexia nervosa (AN)
bulimia nervosa (BN)
binge eating disorder (BED)
other specified feeding or eating disorder (OSFED)
atypical AN
sub threshold BN
sub threshold BED
purging disorder (PD)
night eating syndrome (NES)
anorexia nervosa (AN)
Restriction of energy intake leading to significantly low body weight
DSM-5 lets clinician determine what is low weight for an individual
intense fear of gaining weight or becoming fat, or persistent behavior that interferes with weight gain
disturbance in experience of body weight, undue influence of weight/shape on self-evaluation, or denial of the seriousness of low weight
AN Subtypes (restricting and binge/purge)
both meet same criteria 1-3
bulimia nervosa (BN)
Recurrent episodes (occurring at least 1/wk on average for 3 months) of binge eating characterized by both
eating within a 2-hour period an amount of food that is definitely larger than most people would eat in a similar condition
a sense of loss of control during the episode
Recurrent (occurring at least 1/wk on average for 3 months) inappropriate compensatory behaviors to prevent weight gain
undue influence of weight and shape on self-evaluation
No low weight (e.g., not anorexia nervosa)
Binge Eating Disorder (BED)
Recurrent (occurring at least 1/wk on average for 3 months) episodes of binge eating (same core features as in BN required)
Binge episode accompanied by ≥3 associated symptoms:
eating much more rapidly than normal
eating until feeling uncomfortably full
eating alone because of feeling embarrassed by how much one is eating
feeling disgusted with oneself, depressed, or very guilty afterwards
Distress regarding binge eating is present
not low weight and no compensatory behaviors
i.e., it’s not AN or BN
problems with DSM-5 categories
many people with clinically significant disorders of eating do not meet DSM-5 criteria for AN, BN, or BED, and the boundaries between them are not always clear
OSFED
Disorder of eating that does not meet criteria for AN, BN, or BED or the feeding disorders (pica, rumination, ARFID)
Atypical AN - all criteria for AN except that, despite significant weight loss, the individual’s current weight is in the normal range
All criteria for BN were met except that binge eating and ICB occur at a frequency of less than once/week or duration of less than 3 months
All criteria for BED are met except that binge eating occurs at a frequency of less than once/week or duration of less than 3 months
Purging Disorder (PD) - recurrent purging in the absence of binge eating
vomiting, laxatives, diuretics
Night Eating Syndrome (NES) - recurrent night eating (nocturnal eating or excessive intake after evening meal) of which the person is aware
Diagnostic and Statitical Manual of Mental Disorders (DSM)
produced by the American Psychiatric Association
contents have changed across each of its 5 editions
International Classification of Diseases (ICD)
produced by the World Health Organization
contents have changed across each of its 11 editions
How is the ICD-11 different from the DSM-5?
ICD-11 doesn’t have “specified” disorders in the Other Specified category
Different definition of binge eating:
“A binge eating episode is a distinct period of time during which the individual experiences a subjective loss of control over eating, eating notably more or differently than usual, and feels unable to stop eating or limit the type of amount of food eaten.”
BED does not require “associated characteristics”
DSM-5 categories
many people with clinically significant disorders of eating do not meet DSM-5 criteria for AN, BN, or BED, and the boundaries between them are not always clear
feeding disorders in the DSM-5
pica, rumination disorder, avoidant/restrictive food intake disorder (ARFID)
pica
persistent eating of non-nutritive substances for a period of at least one month
the eating of non-nutritive substances is inappropriate to the developmental level of the individual
the eating behavior is not part of a culturally supported or socially normative practice
if occuring in the presence of another mental disorder (e.g., autism spectrum disorder), or during a medical condition (e.g., pregnancy), it is severe enough to warrant independent clinical attention
Pica Treatment
test for nutritional deficiencies
Calcium and iron deficiencies most common
treat any deficiencies with diet supplements
behavioral interventions
Reinforce (reward) discarding a non-food item
Rumination Disorder
repeated regurgitation of food for a period of at least one month. Regurgitated food may be re-chewed, re-swallowed, or spit out
the repeated regurgitation is not due to a medical condition (e.g., gastroesophageal reflux)
the behavior does not occur exclusively during AN, BN, BED, or ARFID
if occurring in the presence of another mental disorder (e.g., intellectual developmental disorder), it is severe enough to warrant independent clinical attention
rumination disorder treatment
behavioral training
train patients to identify when regurgitation is about to occur
move from subconscious to conscious behavior
engage in diaphragmatic breathing at first sign of regurgitation
relax muscles and prevent food from coming up
Avoidant-Restrictive Food Intake Disorder (ARFID)
An eating or feeding disturbance as manifested by persistent failure to meet appropriate nutritional and/or energy needs associated with one (or more) of the following:
significant loss of weight (or failure to achieve expected weight gain or faltering growth in children)
significant nutritional deficiency
dependence on enteral feeding or oral nutritional supplements
marked interference with psychosocial function
The behavior is not better explained by a lack of available food or by an associated culturally sanctioned practice
The behavior does not occur exclusively during AN or BN, and there is no evidence of a disturbance in the way one’s body weight or shape is experienced
if occuring in the presence of another condition/disorder, it is severe enough to warrant independent clinical attention
(sensory factors, fear of consequences, lack of interest)
ARFID treatment
family-based treatment
also a treatment for AN in children, blurring distinctions between ARFID and AN
cognitive behavioral treatment
Differences between Eating and Feeding Disorders
Eating Disorders are characterized by body image disturbance (AN and BN) or distress (BED) that is absent in Feeding Disorders
Feeding disorders are diagnosed based on the presence of behaviors and the absence of ED-related cognitions because they typically emerge at ages where abstract concepts do not exist
Feeding disorders typically emerge when parents are feeding children rather than children being responsible for feeding themselves (a.k.a., eating)
BMI of obese adults
BMI > 30 kg/m²
>40 kg/m2 is morbid
Waist circumference
>40’” in men or >35” women
obese BMI for ages 2-19 years
>95th percentile for age and gender
Why has obesity increased?
changes in diet (1974→2014)
where we eat
what we eat
when we eat
how we eat
why we eat (marketing)
changes in activity level
Is obesity an eating disorder?
Imbalance between energy needs and energy intake suggests that obesity represents a problem with eating too much
linked to BED
however, an ED characterized by excessive food intake already exists (BED), and not everyone with BED is obese
Most individuals who are obese do not have BED or any loss of control over their eating
According to AMA and WHO, obesity is a disease
Death Risk BMI (Obesity)
BMI 25-30: lowest risk of death from any cause
BMI > 35 increased risk
BMI < 18.5 increased risk
Who is stereotyped to have an eating disorder?
women
Grillot & Keel, 2018 (Treatment Seeking for Eating Disorders)
Background
Most individuals with an eating disorder never seek treatment for their problem, and this is particularly true for men with eating disorders
In addition, most people w/ eating disorders don’t recognize that they have a problem with their eating
Why are men even less likely to seek treatment than women?
Self-recognition of an ED is required to seek treatment
Based on stereotypes that eating disorders are a “female” disorder, men are less likely than women to recognize when they have an eating disorder
Treatment Seeking for Eating Disorders (Grillot & Keel, 2018)
Methods
Secondary analyses of survey data collected in 2012 from 2,514 respondents
Information collected
Gender, DSM-5 criteria for an ED taken from the Eating Disorder Diagnostic Scale
“questions”
Height and weight
checklist of past mental disorders
Discussion
Most people with an ED don’t recognize it and never get treatment
men are less likely to seek treatment
not recognizing an ED is barrier to treatment seeking for both men and women
women and men are equally bad at recognizing that they have an eating disorder
more research is needed to understand other barriers that are unique to men
What protects men from EDs?
AN and BN are defined by body image disturbance related to weight and shape
intense fear of gaining weight or becoming fat
misperception of the body as being too fat
undue influence of weight/shape on self-evaluation
BED not defined by body image disturbance
See less (almost half) gender ratio seen for AN and BN
“Reverse Anorexia,” “Bigorexia,” “Muscle Dysmorphia”
Dietary manipulations to increase muscle mass/decrease body fat
excessive exercise to build muscle mass
misperception of size: perceive body as puny despite a well-muscled physique
abuse of anabolic-androgenic steroids
Anabolic-Androgenic Steroids
Man-made derivatives of testosterone
increase protein synthesis and muscle mass
reasons for abuse: desire for increased strength, improved athletic performance, enhanced appearance
negative effects
damage to musculoskeletal, cardiovascular, endocrine/reproductive, and liver systems
increased mood lability, anger, and physical outbursts
Stereotype vs. reality
Eating disorders are less common in men than in women
in addition, men may be more likely to suffer from conditions that have been labeled “body dysmorphic disorders” than “eating disorders”
however, men comprise a larger portion of those suffering from eating disorders than those included in ED treatment and research
Gordon, Perez, and Joiner (2002)
Does race/ethnicity influence recognition of an ED?
Procedure: Read a 5-day diary depicting a high school girl’s activities and then complete series of questions about girl
IV: Mary’s ethnicity (white vs black/hispanic)
DV: Does Mary have any notable problems? How would she respond to _____ [questions from eating disorder scale]
Results:
identification of eating problem linked to Mary’s ethnicity
responses to EDI drive for thinness items did not differ between conditions
suggests a disconnect between the ability to recognize disordered attitudes/behaviors and label this as an “eating problem” in a person who does not fitthe stereotype
results not influenced by participants’ ethnicity
Ethnicity & Access to Care (Becker et al., 2003)
Does race/ethnicity influence access to care?
Study 1: Compared to White participants, both Latino (.60) and Native American participants (.51) were significantly less liekly to recieve referral for treatment controlling for symptom severity
Study 2: No significant difference among racial/ethnic groups in likelihood to seek treatment. Ethnic minority participants were less likely to be asked about eating by doctors and less likely to receive treatment referral (31%) compared to White participants (60%)
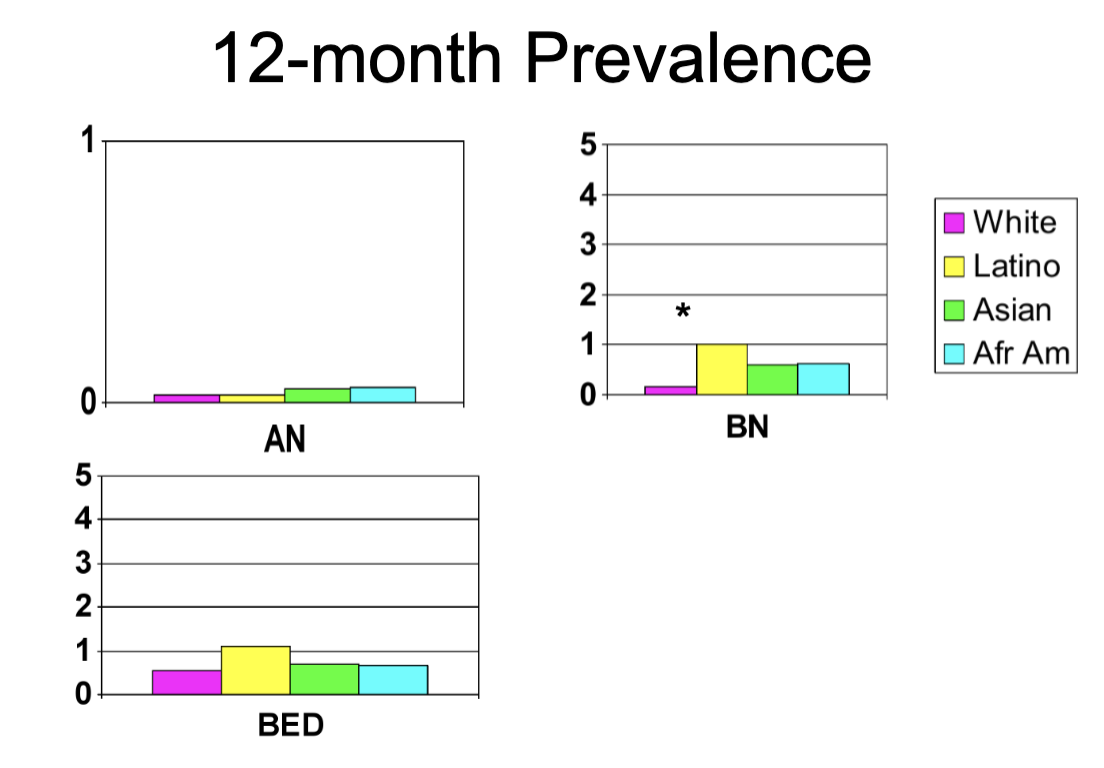
Comparison of ED Prevalence (Marques et al., 2010)
Do racial/ethic groups differ in ED Prevalence?
Pooled Data from the NIMH Collaborative Psychiatric Epidemiological Studies (CPES)
Is acculturation to dominant culture linked to ED risk?
Significant positive association between acculturation and ED prevalence in Latino participants
No significant association between acculturation and ED prevalence in Asian participants
Is the likelihood of mental health care associated with race/ethnicity for those with EDs?
White participants with ED significantly more likely to have received mental health treatment compared to Latino, Asian, and African American participants
ED & culture
eating disorders are more common in industrial, often Western, cultures
eating disorders appear to be a modern problem
increaser in eating disorder incidence associated with increasing idealization of thinness
Non-western cultures (AN and BED prevalent in all 5). Where is BN prevalent in non-Western cultures?
East Asia, Middle Eastern/Arab, Southeast Asia
Introduction of TV to Ethnic Fijians (Becker et al., 2002)
Does exposure to Western media increase disordered eating in non-Western cultures?
Fiji has a low prevalence of eating disorders; values idealize a fuller figure, encourage robust appetites, and view thinness as arising from a lack of family support/caring
83% of girls in 1998 reported that TV influenced their or their friends’ feelings and behaviors about body weight/shape
77% indicated that TV influenced their own body image
40% believed that losing weight/eating less would help them obtain successful careers
associated with significant increase in EAT-26 scores and vomiting behavior
Native Korean vs Korean immigrant vs Korean American ED levels
NK and KI have higher disordered eating levels than KA
suggests that Western culture is not the only source of cultural influences that may contribute to eating disorders
Non-Western cultures contribute to EDS
no association between acculturation to Western ideals and eating pathology for Asian individuals in the US or outside the US
AN is not culturally bound illness
Korean women in Korea have higher EAT-26 scores than Korean women in the US
AN: 13th to 16th Centuries: “Anorexia Miribalis”
Holy Anorexia
Self-starvation as penitence, path to religious piety and purity
Saint Hedwig
Saint Catherine of Siena
Church became concerned
AN: 16th to 18th Centuries: “Miraculous Maids”
Exhibition of starving abilities
Claim to subsist soley on air or water, small amounts of food
Mixture of spiritual and mystic beliefs
Interest by physicians, deaths reported
1689: Sir RIchard Morton (described 2 patients with AN)
AN: 18th to 19th Centuries: Case Studies
1770s: Timothy Dwight
1860: Luis Victor Marce
(Gull, 1888): Miss K. R——
BN: 20th Century
1903: Janet
First to describe a patient with bulimic behaviors: compulsive secretive binges and vomiting
1932: Wulff
described patients with periods of intense cravings and overeating, followed by vomiting
1958: Binswanger
After being teased for weight, patient began using thyroid pills, laxatives, and comiting; consumed dozens of oranges and pounds of tomatoes
Who published the first clinical paper on bulimia nervosa
1979: Gerald Ressel
“An ominous variant of anorexia nervosa”
Individuals with a morbid fear of becoming fat who overeat and purge afterwards
BED: Long Road to Diagnosis
1959: Albert Stunkard
Clinical observation of recurrent episodes of binge eating in some individuals with obesity
Large amounts of food at irregular intervals
1992: “Binge eating disorder” was introduced at the International Conference on Eating Disorders as a provisional diagnosis
2003: Cooper and Fairburn
Noted needed for attention and diagnostic clarity regarding BED
Difficulty distinguishing BED from other forms of overeating (e.g., obesity, non-purging bulimia nervosa)
Have eating disorders become more common with increased idealization of thinness?
Prevalence: proportion (%) of population with illness
Incidence: number of new case per a set number of persons per year (e.g., per 100,000 persons/year)
Prevalence vs. Incidence
Prevalence influenced by new illness onset and illness chronicity
Incidence only reflects new illness onset
Summary of AN over time
Cases found in non-Western cultures in the absence of Western influence
Cases found long before the introduction of AN to psychiatric nomenclature
Only a modest increase in AN incidence during a period of dramatically increasing idealization of thinness
Summary of BN over time
no cases foudn in the absence of Western influence
few cases found before introduction of BN to psychiatric nomenclature, and historical cases differ in demographic and clinical features
dramatic increase in BN incidence accompanying increasing idealization of thinness over second half of 20th century
Summary of Eating Disorders over time
AN has demonstrated modest significant increase over time, but existed long before emergence of the thin ideal
BN demonstrated a dramatic significant increase in latter half of 20th century that appeared to be receding heading into the new millennium
combined with information on culture and ethnicity - more evidence that BN influenced by sociohistorical factors than AN
Too little data on BED, PD, or NES to draw conclusions
Scientific Method
Step 1: Frame a research question
Step 2: Conduct a literature review
Step 3: Form a hypothesis
Step 4: Design a study
Step 5: Conduct the study
Step 6: Analyze the data
Step 7: Report the results
Methods in Eating Disorders Research
Ethnical constraints contribute to various indirect approaches for understanding causes
Cross-sectional/correlation studies
Longitudinal Studies
Retrospective Follow-back
Prospective Follow-up
Experimental Studies
Analogue designs
Treatment/Prevention designs
Designing a Cross-sectional Design
measure all variables at the same time and see how they are associated
pros
requires least resources
time
money
if hypothesis NOT supported in cross-sectional design, saves resources for future hypotheses
Cons
depending on variables, limited inferences regarding cause and effect, “correlation does not prove causation”
variable C could be an underlying third variable
Designing a Longitudinal Study
measure variables over time to see how one variable predicts the other variab;es
pros
for A to casue B, A must precede B in time
allows identification of whether A increase risk for a B (“risk factor”)
Cons
resource-intensive
in prospective follow-up longitudinal designs, Variable A has to be measured before onset of Variable B
for eating disorders, this is a fairly young age
if variable B has low base rate (i.e., low prevalence), one may not observe adequate change in Variable B to reliably determine the association between Variable A and Variable B (i.e., statistical significance)
Additional limitation
cannot draw causal inferences; it’s really just a correlation over time
Retrospective Follow-back design (longitudinal)
compare individuals with an ED tot hose without on factors present BEFORE the age of ED onset
Pro: adequate number of cases
Con: retrospective recall bias
Prospective Follow-up design
start with sample without ED, measure factors, and then follow participants to see which factors predict ED onset
pro - no recall bias
con - few cases, so use broad measures
Designing Experimental Designs
Experimentally manipulate A to see what effect that has on B
Pros
Allows for strongest inferences regarding causation
cons
cannot ethically test hypotheses regarding causes of eating disorders
anologue studies
treatment prevention studies
analogue studies (experimental)
analogue refers to analogy
dieting is like self-starvation
overeating is like binge eating
discrepancy between current and ideal body figure is like body image disturbance
very focused DV
experimental manipulation of very focused independent variable (IV)
does manipulation of IV cause change in DV
Pros and Cons of analogue studies
Pros
many require only slightly more resources than used in cross-sectional designs
strong causal inferences possible
Cons
Causal inferences limited to specific variables examined
Questionable ecological validity
Intervention Studies
Two types
Treatment
Prevention
IV is your assigned condition
Treatment study - SSRI vs. Placebo
Prevention study - Cognitive Dissonance (CD) vs Healthy Weight Control (HWC)
DV is eating disorder/disordered eating
Intervention Studies: Treatment
if outcome is superior in SSRI condition compared to placebo condition, then SSRI caused improvement
Pro - with large samples, adequate power to see change
Con - factors that contribute to remission not necessarily part of cause
Intervention Studies: Prevention
If outcome is superior in CD condition compared to HWC, then CD prevented ED onset
Pro - most powerful design for demonstrating causal factors
Con - resource intensive given low base rate of ED
Analyzing Data
Descriptive statistics
Inferential statistics
Inferential statistics
Tests of Association (e.g., is dieting frequency associated with binge eating frequency?)
Ex., correlation, regression (linear vs. logistic)
Tests of Differences (e.g., do dieters binge more frequently than non-dieters?)
Ex., t-tests, ANOVA
Risk and Maintenance Factors (Dakanalis et al. 2017)
Question: Do appearance-ideal internalization, body dissatisfaction, dieting, negative affect, and self-objectification contribute to?
risk for onset of an eating disorder?
maintenance of an eating disorder?
Analyses: descriptive analyses
who has an ED at each time point
IV = apperance ideal internalization, body dissatisfaction, dieting, negative affect, self objectification
DV = group
Prediction of ED onset using logistic regression
Prediction of ED maintenance using logistic regression
Results:
The 4 groups differed on all 5 factors
Baseline levels of each factor, and change in each factor predicted onset of ED
Baseline levels of each factor, and change in each factor predicted maintenance of ED
Visual comparison of contributions of each factor suggested that self-objectification might have the greatest impact on both onset and maintenance of ED
Discussion:
Overlap in factors contributing to onset and maintenance suggest that prevention and treatment efforts can focus on same set of factors
Self-objectification deserves greater attention in risk and maintenance models
may influence the link between other factors and EDs in onset and maintenance
How thin is too thin (AN)?
General guideline for adults: less than 85% of weight based on age/height
BMI ≤ 18.5