Ch. 41 Transport of Oxygen & Carbon Dioxide in Blood & Tissue Fluids
1/20
Earn XP
Description and Tags
Flashcards about the transport of oxygen and carbon dioxide in blood and tissue fluids, based on lecture notes.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
21 Terms
What causes oxygen to diffuse into the pulmonary capillary?
What happens to the blood by the time it leaves the pulmonary capillaries?
Blood stays in the capillary almost _____ times as long as it needs to under resting conditions to become fully oxygenated.
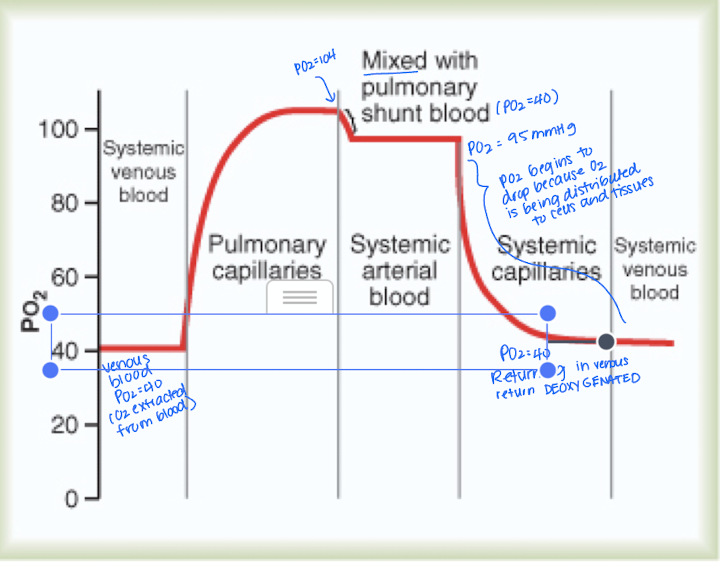
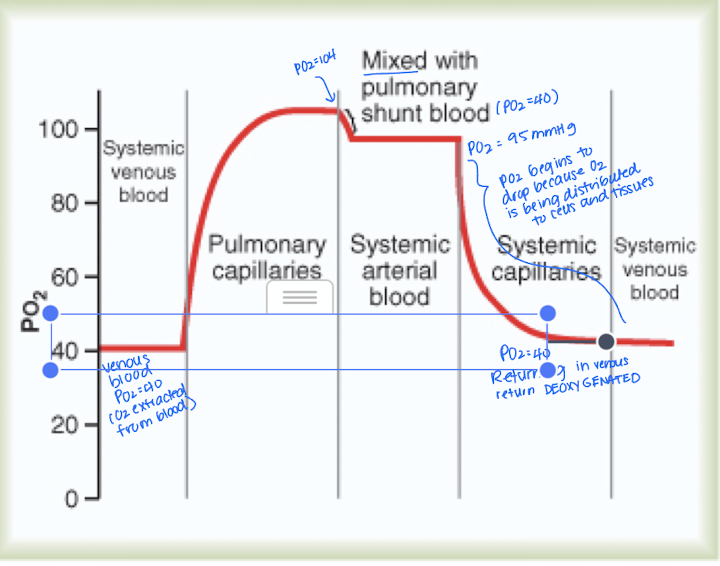
Initial pressure difference between the alveoli (104 mm Hg) and pulmonary capillary
*greater the pressure, faster the diffusion
oxygen will be almost saturated by the time it leaves
3 times
What percentage of blood entering the left atrium from the lungs has been oxygenated, and to what PO2?
What is 'shunt flow' in the context of oxygenated blood?
About 98% of blood that enters the left atrium from the lungs has passed through the alveolar capillaries and has become oxygenated to a
The 2% of blood that bypasses the alveolar capillaries and isn't exposed to oxygen exchange areas - goes from aorta to tissues
What is the composition of shunt blood and what is its PO2?
Systemic venous blood (PO2 = 40 mm Hg) that mixes with oxygenated blood in the pulmonary veins, resulting in a PO2 of 95 mm Hg.
this is the 2% not exposed to alveoli
What happens to carbon dioxide when oxygen is used by cells?
When oxygen is used by cells, carbon dioxide is produced proportionately and diffuses in the opposite direction as oxygen.
How does the diffusion rate of CO2 compare to that of O2?
Carbon dioxide diffuses 20 times faster than oxygen (because CO2 has greater solubility) - therefore pressure difference for CO2 does not have to be nearly as great
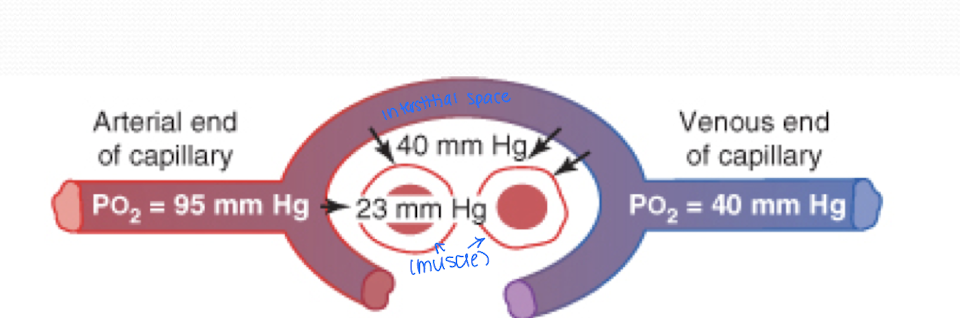
Explain this image
The image shoes the diffusion of oxygen from the peripheral capillaries into the tissue fluid
When arterial blood reaches the peripheral tissues, PO2 in the capillaries is still 95 mmHg
The PO2 in the interstitial fluid surrounding the tissue cells is 40 mmHg.
the large interstitial difference that causes O2 to diffuse rapidly from capillary blood to tissues causing capillary PO2 to almost equal the 40 mm Hg pressure in the interstitial fluid
PO2 of the blood leaving the tissue capillaries and entering the systemic veins is also about 40 mmHg
How is oxygen primarily transported in blood?
97% of oxygen is transported from the lungs to the tissue via hemoglobin, while 3% is dissolved in plasma.
When PO2 is high, how does O2 react to hemoglobin?
What happens when PO2 is low?
High PO2 (in pulmonary caps (lungs)) causes O2 to bind to Hb
Low PO2 (in tissue caps) will cause O2 to be released from Hb because O2 needs to reach the muscles and tissues
At alveolar PO2, ____ mm Hg or 0.3 mL of oxygen dissolves in each dL of blood. This results in about 3 mL of O2 per liter of blood with a total of (2.)____ L of blood volume (15 mL dissolved O2)
104 mmHg
5
T/F: dissolved O2 establishes the PO2 of blood
true
it helps regulate breathing and determine loading of hemoglobin (binding affinity)
Men have ____ grams/dL of hemoglobin
15
What is the oxygen-carrying capacity of hemoglobin?
Each gram of hemoglobin combines with 1.34 mL of O2; with normal Hb levels, each dL of blood contains about 20 mL of O2 (compared to the 15 ml dissolved in 5 L).
If there is an increased affinity of hemoglobin, where can this occur?
Where can we see a decreased affinity?
lungs (high PO2)
in tissues (low PO2)
How much oxygen is utilized at rest?
25% because venous blood carries 15 mL of O2 dL per blood
What is the Bohr effect?
The Bohr effect shifts the oxyhemoglobin dissociation curve to the right, enhancing the release of oxygen from the blood in tissues and oxygenation of blood in the lungs.
Name conditions that can create the Bohr effect.
Increased PCO2 (as we consume more oxygen)
increased temperature
increased 2,3-DPG
decreased pH
What are the three mechanisms for CO2 transport?
Dissolved in plasma, plasma bicarbonate, and bound to hemoglobin.
How much CO2 is transported as dissolved CO2?
About 5% of CO2 is transported as dissolved CO2, which establishes the PCO2 of the blood.
How is CO2 transported as bicarbonate?
The most important transporter of CO2; 70% of CO2 is transported this way.
CO2 is combined with water to form carbonic acid
which is processed to carbonic anhydrase
The carbonic acid ionizes into hydrogen ions and bicarbonate ions
creating the chloride shift - which is went chloride content of venous RBC is greater than arterial RBC
How is CO2 transported as carbamino compounds (second way to transport CO2)?
CO2 reacts directly with Hb to form carbamino compounds.
associated with the Haldane effect: Hb interaction with O2 reduces its ability to bind to CO2. This aids in releasing CO2 in the lungs BUT as O2 is removed from Hb (goes to tissues), Hb will go back to binding with CO2
What is the Haldane Effect?
Hb interaction with O2 reduces its ability to combine with CO2, aiding in releasing CO2 in the lungs.