PHSL 3051 cardiovascular
1/125
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
126 Terms
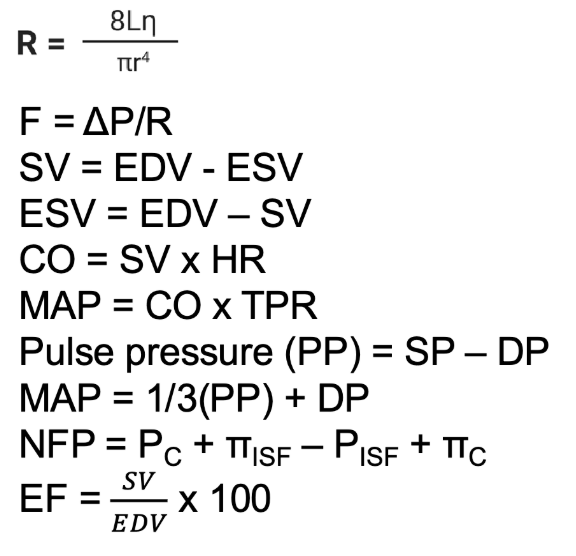
cardiovascular equations
the cardiovascular system - roles in homeostasis
main transport system for delivering nutrients, removing wastes, distributing hormones and other signaling molecules
temperature regulation
*to be biologically viable most cells in the body are within 10um of a capillary
components of the cardiovascular system
heart: the biological pump; generates force to move the blood
2 events for each beat: electrical (action potential) followed by mechanical (contraction)
blood: the medium thigh through which O2 and nutrients are transported
vasculature: the vessels through which the blood flows; they are not
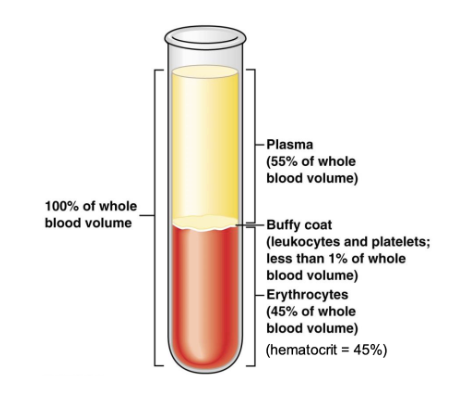
blood
total volume of blood, on average, is 5.5 liters
plasma averages 55-58% of total blood volume, and is part of the ECF
buffy coat: contains leukocytes (immune cells) and platelets (clotting
erythrocyte (red blood cells) volume averages 42-45% called the hematocrit (mainly for gas transport)
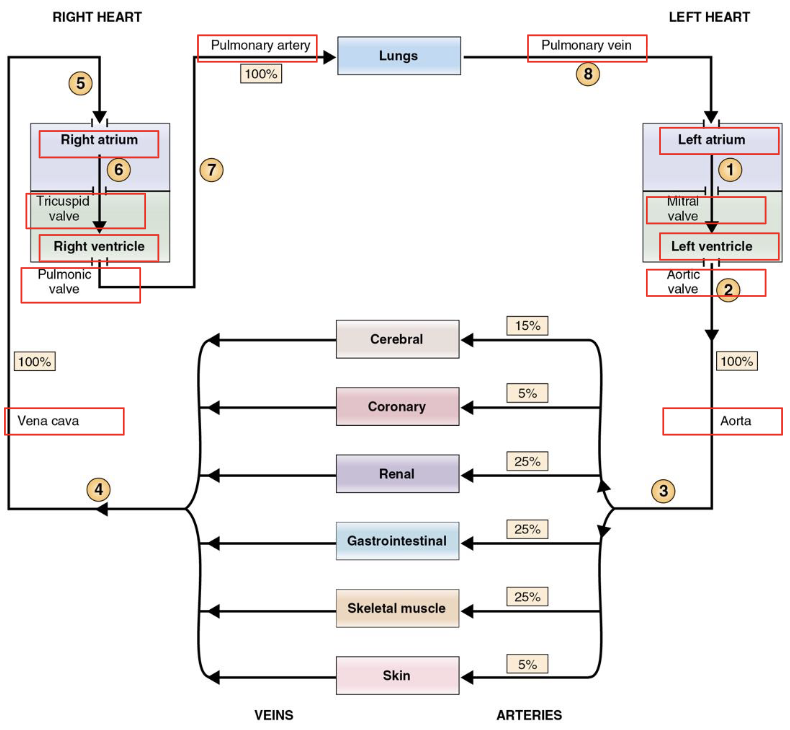
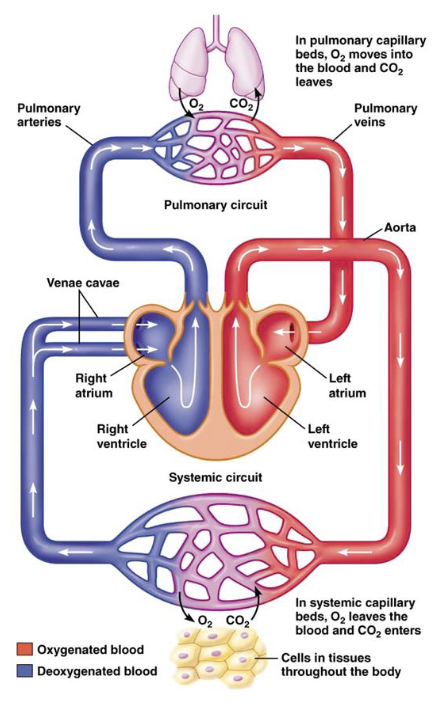
overview of heart and vasculature
2 pumps (right ventricle RV and left ventricle LV) and 2 circulatory systems (pulmonary and systematic)
parallel vascular beds vs vascular beds in series
pressure differences between pulmonary and systemic circuits
perfusion
ischemia
perfusion
passage of blood flow through a vascular bed
ischemia
lack of oxygen/blood flow - typically due to an occlusion
size difference of the heart and vasculature
wall of the LV (the myocardium - the muscle) is much thicker than the right. this allows the LV to generate greater pressure
the pressure in the systematic circulation is much higher than the pressure in the pulmonary circulation. the ventricles must generate enough pressure to create a gradient so that blood can flow (from high to low pressure)
parallel vs series arrangement of vascular beds
the pulmonary circuit is arranged in series, systemic is in parallel
same quality of blood to all tissues
allows for better regulation of blood flow
takes less pressure than if arranged in series
*total resistance across a system arranged in parallel is less than if the same system was arranged in series
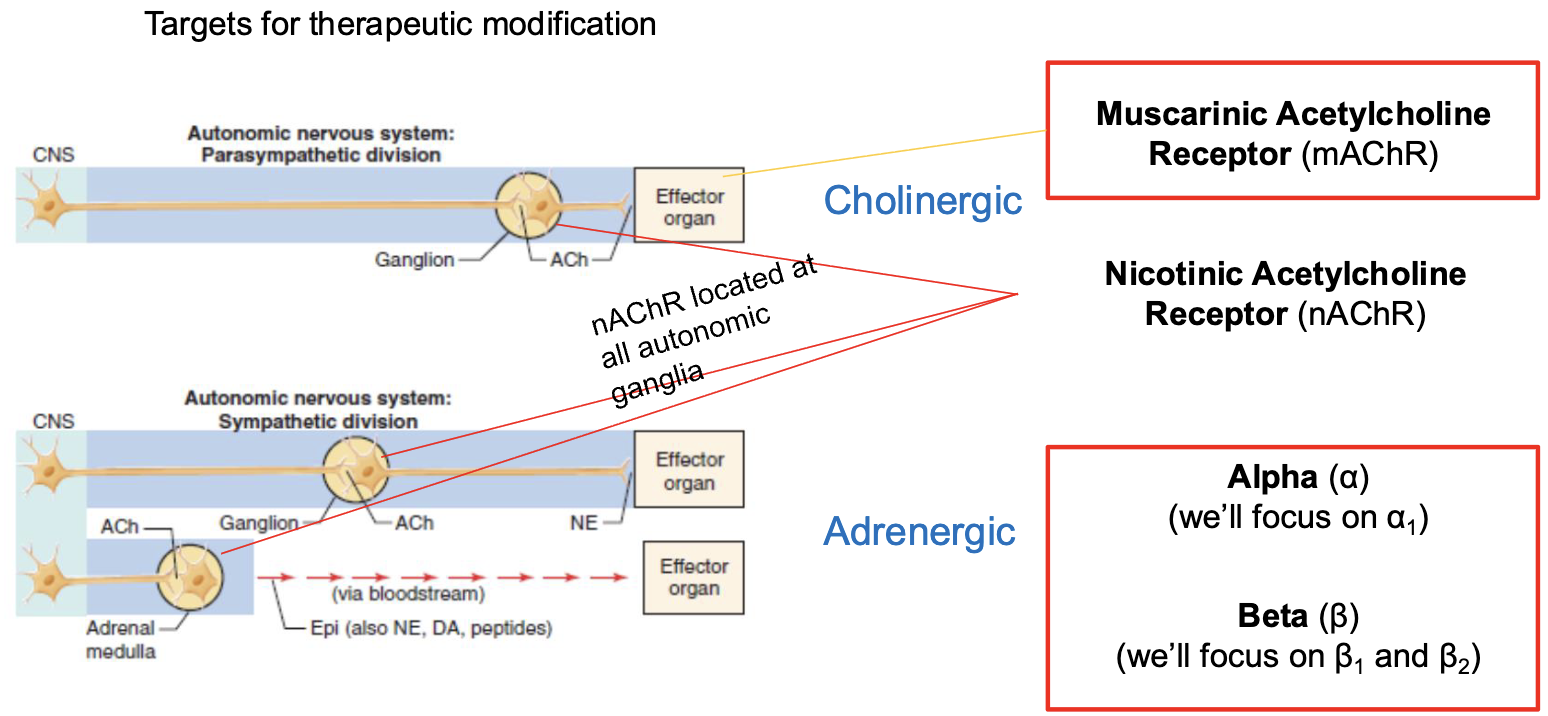
receptors of the CV system
muscarinic acetylcholine receptor (mAChR)
nicotinic acetylcholine receptor (nAChR)
alpha (a)
beta (B)
pressure, flow, resistance
F (or Q) = flow (L/min)
ΔP = pressure difference between two points (mmHg) - its the gradient that matters, not the absolute pressures
R = resistance to flow (mmHg*min/L)
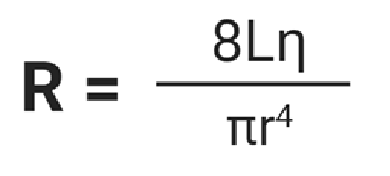
resistance
as resistance goes up, flow goes down
L = vessel length
n = viscosity of the blood
r = radius of vessel (to the 4th power)
purpose of heart valves
to promote one way direction of blood flow
2 types of heart valves (4 total)
atrioventricular valves (AV)
semilunar valves (SL)
*pressure gradients induce opening and closing of valves - a passive process
atrioventricular valves and function
right AV (tricuspid)
left AV (bicuspid; mitral)
prevent backflow from the ventricles into atria
semilunar valves
pulmonary semilunar valve
aortic semilunar valve
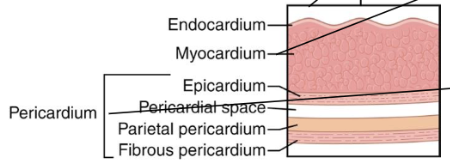
walls of the heart (inner to outermost)
endocardium
myocardium
pericardium
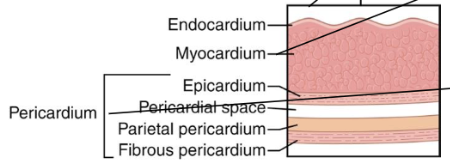
endocardium
innermost layer of the heart
separates chambers from the heart muscle (myocardium)
myocardium
thick layer of cardiac muscle
pericardium
fluid filled sac that surrounds the heart, protecting it and providing lubrication
epicardium separates the myocardium from the pericardial fluid
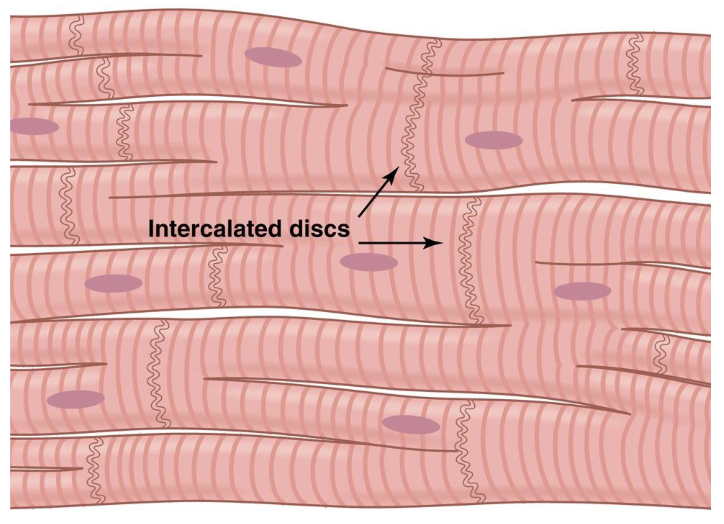
electrical connections between cardiac muscle cells (coordination of the heart beat)
connected via gap junctions → provides rapid communication
desosome
gap junctions
electrical synapse
desmosome
adhesive that holds neighboring cells together
functional syncytium
heart muscle cells are synchronized in health
cardiac myocytes
striated
mostly mononucleated
branched ends
cardiac vs. skeletal vs. smooth muscle similarities
sliding filaments and cross bridges
ATP powers the force generation
elevated Ca2+ triggers contraction
cardiac vs. skeletal muscle similarities
has sarcomeres
striated
has troponin
T-tubules
cardiac vs. smooth muscle similarities
pacemaker cells
gap junctions (syncytium)
Ca2+ entry from ECF
autonomic/hormones modulate activity
involuntary
sequence of blood vessels in the systemic circulation
arteries → arterioles → capillaries → venules → veins
conduction pathway
SA node (true pacemaker of the heart - these cells are the first to generate an action potential, beginning the electrical events of the cardiac cycle)
atrial contractile cells (atrial kick)
AV node (propagation is slow)
bundle of His (conducting cells)
bundle branches (conducting cells)
purkinje fibers (conducting cells)
ventricular contractile cells
timing of activation of the myocardium
rapid conduction through the atria allows the atria to contract at essentially the same time
AV Node delay gives the atria time to contract before ventricular excitation occurs
rapid conduction through the interventricular septum
depolarization of the ventricular contractile cells is almost simultaneous
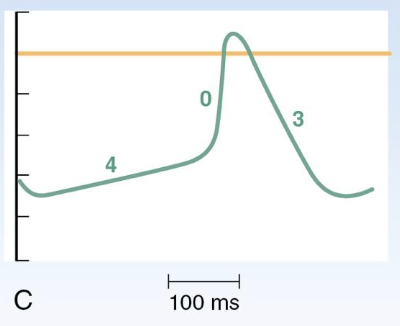
action potential of a cardiac ventricular contractile cell
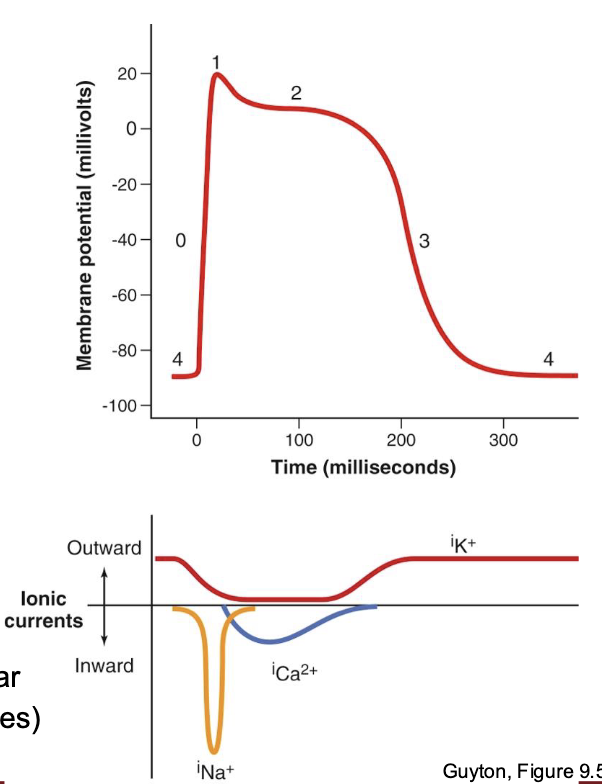
phase 0
depolarization
fast Na+ channels open
phase 1
initial repolarization
fast Na+ channels close
transient (fast) K+ channels open
phase 2
plateau
L type Ca2+ channels open (L for long) (same as DHP channels)
transient K+ channels close
phase 3
rapid repolarization
L type Ca2+ channels close
slow K+ channels open
phase 4
resting membrane potential
-80 to -90 mV in ventricular contractile cells
this phase is the pacemaker potential in some cell types
cardiac action potentials
ventricle
atrium
sinoatrial node
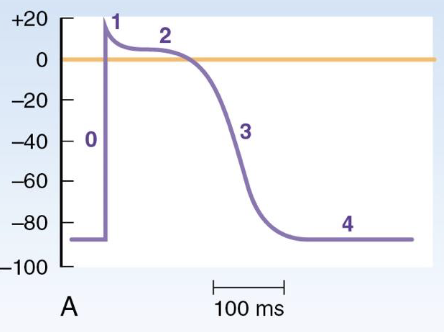
ventricle AP
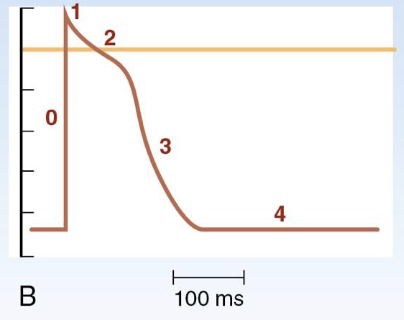
atrium AP
SA Node AP
cardiac ion channels
the - indicates minimal/insignificant
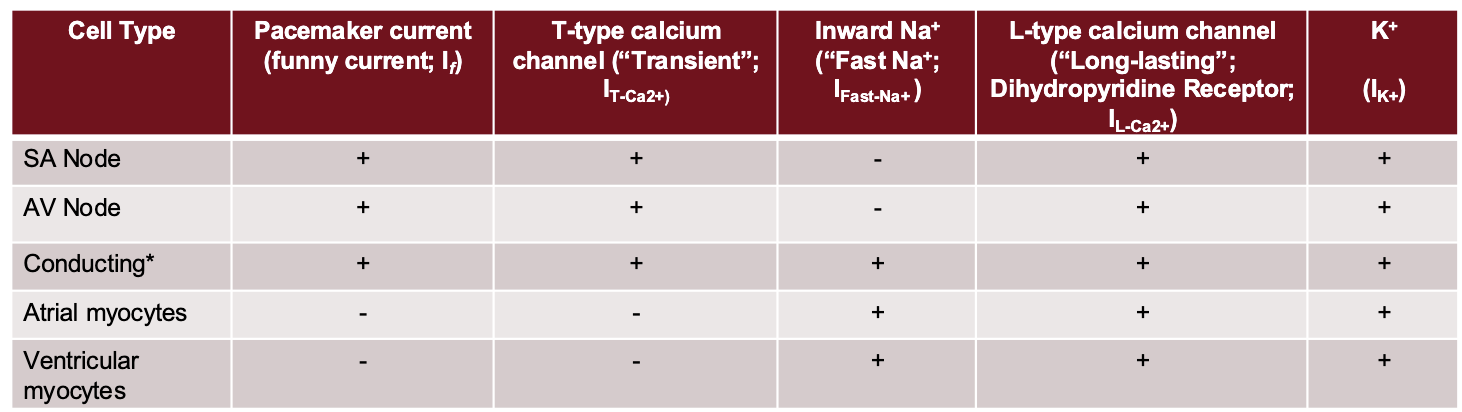
describing excitation in the heart
automaticity
sinus rhythm
latent pacemaker
ectopic pacemaker
automaticity
capable of generating spontaneous action potentials (pacemaker potential)
Sa node, AV node, conducting cells
sinus rhythm
normal cardiac excitation sequence beginning at the SA node
latent pacemaker
not actively driving
includes AV node and conducting cells (cells that have pacemaker potential)
ectopic pacemaker
abnormal
any site/group of cells driving heart rhythm that is not the SA node
intrinsic firing rate
action potentials per minute
intrinsic firing rate - SA node
100-110
intrinsic firing rate - AV node
60-80
intrinsic firing rate - conducting cells
bundle of His - 40
Purkinje fibers - 15-20
cardiac muscle excitation-contraction coupling
calcium induced calcium release (CICR)
similar to smooth muscle
Ca2+ from the ECF entering the cell and causing additional Ca2+ release from the SR
cardiac muscle excitation-contraction coupling STEP 1
the membrane is depolarized by Na+ entry as an action potential begins
cardiac muscle excitation-contraction coupling STEP 2
depolarization opens L-type Ca2+ channels in the T-tubules
cardiac muscle excitation-contraction coupling STEP 3
a small amount of “trigger” Ca2+ enters the cytosol, contributing to cell depolarization
this trigger Ca2+ binds to and opens ryanodine receptors (RyR) located in the SR membrane (calcium-induced calcium release)
cardiac muscle excitation-contraction coupling STEP 4
Ca2+ flows out of the SR into the cytosol, raising the Ca2+ concentration
(for every 1 Ca2+ that enters cell through L-type channel, 10 Ca2+ are released from SR through RyR)
cardiac muscle excitation-contraction coupling STEP 5
binding of Ca2+ to troponin exposes cross bridge binding sites on thin filaments (actin)
cardiac muscle excitation-contraction coupling STEP 6
cross bridge cycling causes force generation and sliding of thick and thin filaments
cardiac muscle excitation-contraction coupling STEP 7
Ca2+ ATPase pumps return Ca2+ to the SR
cardiac muscle excitation-contraction coupling STEP 8
Ca2+ ATPase pumps (and also Na+/Ca2+ exchangers) remove Ca2+ from the cell into the ECF
cardiac muscle excitation-contraction coupling STEP 9
membrane is repolarized when K+ exits to end the action potential
refractory periods of cardiac muscle
absolute refractory period (ARP)
relative refractory period (RRP)
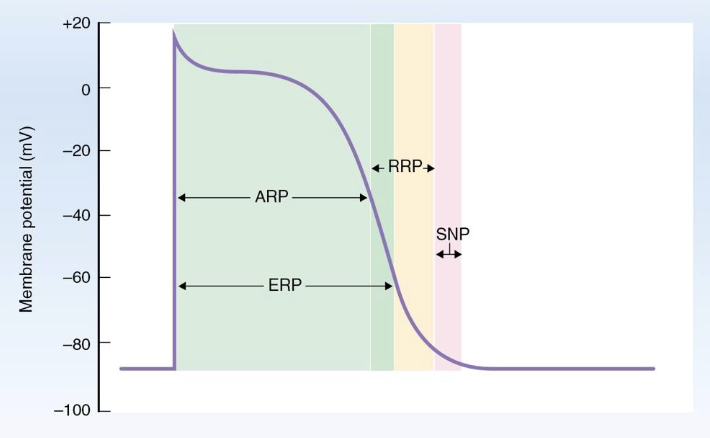
absolute refractory period
the ventricular cell is completely refractory to fire another action potential, regardless of stimulus size
fast Na+ channels are inactive and unavailable to carry inward, positive current
relative refractory period
begins at the end of ARP and continues until the cell membrane has almost fully repolarized
some amount of fast Na+ channels have recovered and are available to open (and carry inward current) again
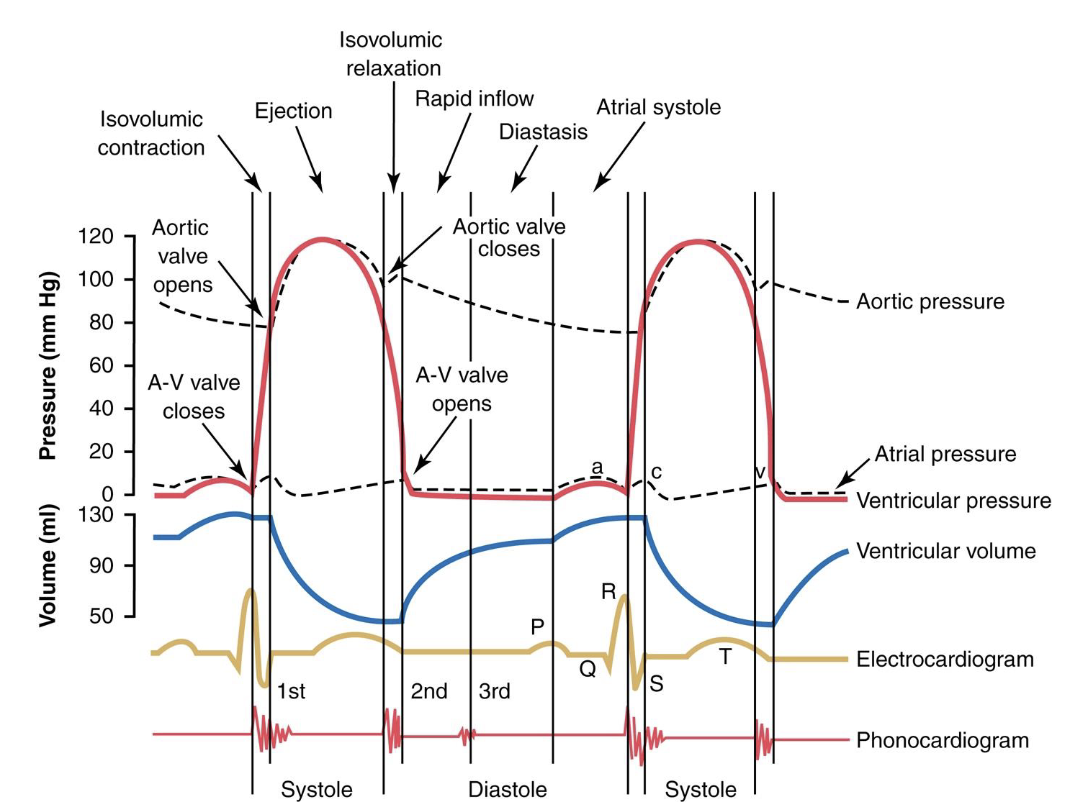
the cardiac cycle - diastole
relaxation of the ventricles
longer; 2/3 of time
the cardiac cycle - systole
contraction of the ventricles
shorter; 1/3 of time
4 phases of the cardiac cycle (in reference to the LV by default)
one cardiac cycle
ventricular filling → diastole
isovolumetric contraction → systole
ejection → systole
isovolumetric relaxation → diastole
end product of each cardiac cycle
stroke volume (SV) - the volume of blood ejected from each ventricle per beat (mLs/beat)
SV = End-Diastolic Volume - End-Systolic Volume
SV = EDV - ESV
ventricular filling (diastole)
AV valves - open
aortic and pulmonary valves - closed
ventricles fill with blood during diastole
the initial period of ventricular filling is passive; blood passively moving from atria to ventricles
followed by “atrial kick” (atrial contract). this contributes to an additional 10-20% of blood to the ventricles
the end of this phase is EDV
EDV = final volume of blood in the ventricle after filling (~135mLs at rest)
isovolumetric contraction (systole)
AV valves - closed
aortic and pulmonary valves - closed
ventricles contract (corresponds to ECG event - QRS complex)
1st heart sound at the start of this phase (S1): “lub” caused by AV valves closing
volume constant at EDV
pressure in ventricles < pressure in aorta and pulmonary artery
pressure in ventricles > pressure in atria
ejection (systole)
AV valves - closed
aortic and pulmonary valves - open
pressure in ventricles > pressure in aorta and pulmonary artery
stroke volume: volume of blood ejected from each ventricle per beat (~70 mLs at rest)
reach ESV
ESV = volume of blood remaining in the ventricle after ejection
ESV = EDV - SV
isovolumetric relaxation (diastole)
AV valves - closed
aortic and pulmonary valves - closed
2nd heart sound at the start of this phase (S2): “dup” caused by semilunar valves closing
volume constant at ESV
pressure in ventricles < pressure in aorta and pulmonary artery
pressure in ventricles > pressure in atria
ejection fraction and heart failure
measure of the efficiency of the heart. typically measured in the LV
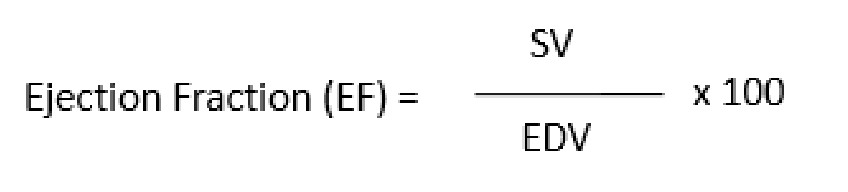
normal EF values
55-70% - values below can be indicative of heart failure
heart failure with reduced ejection fraction (HFrEF)
traditional marker of heart failure
could be indicative of systolic dysfunction
heart failure with preserved ejection fraction (HFpEF)
the ventricle is stiff and has difficulty relaxing
could be indicative of diastolic dysfunction
wiggers diagram
chart includes
pressures
volumes
ECG
phases of cardiac cycle
when pressure lines cross, important events occur (and valves open/close)
LUB (AV valves close) and DUB (semilunar valves close) heart sounds are due to valves closing
diagram *memorize
cardiac output
cardiac output (CO) is the volume of blood ejected from each ventricle per unit time
it is the product of heart rate (HR) and stroke volume (SV), and is typically expressed as liters/min
CO is flow! - volume of blood per unit time

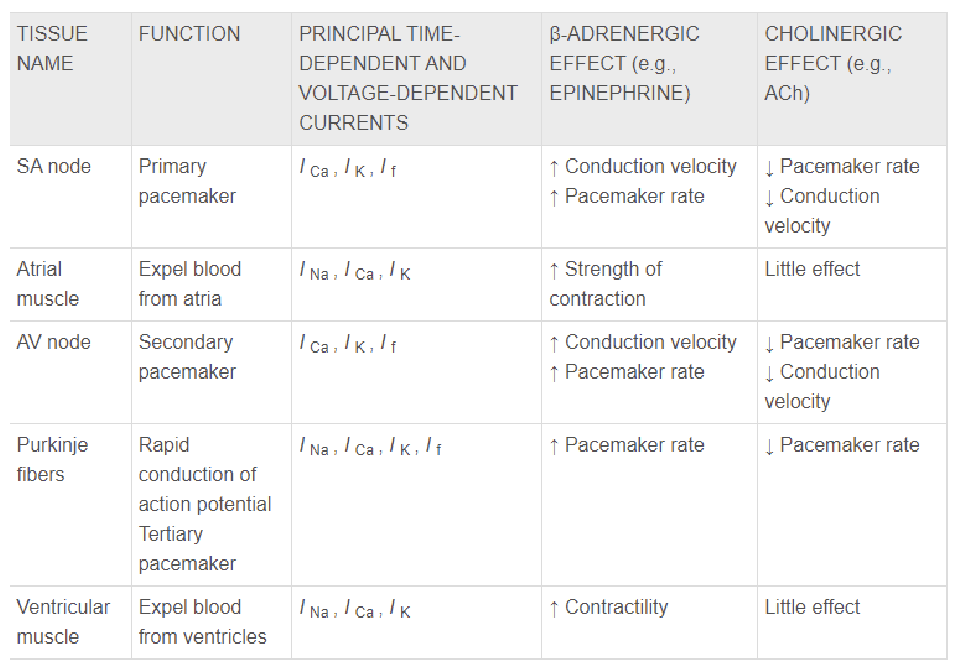
autonomic innervation of the heart
majority (75-80%) of beta-adrenergic receptors in the heart are B1
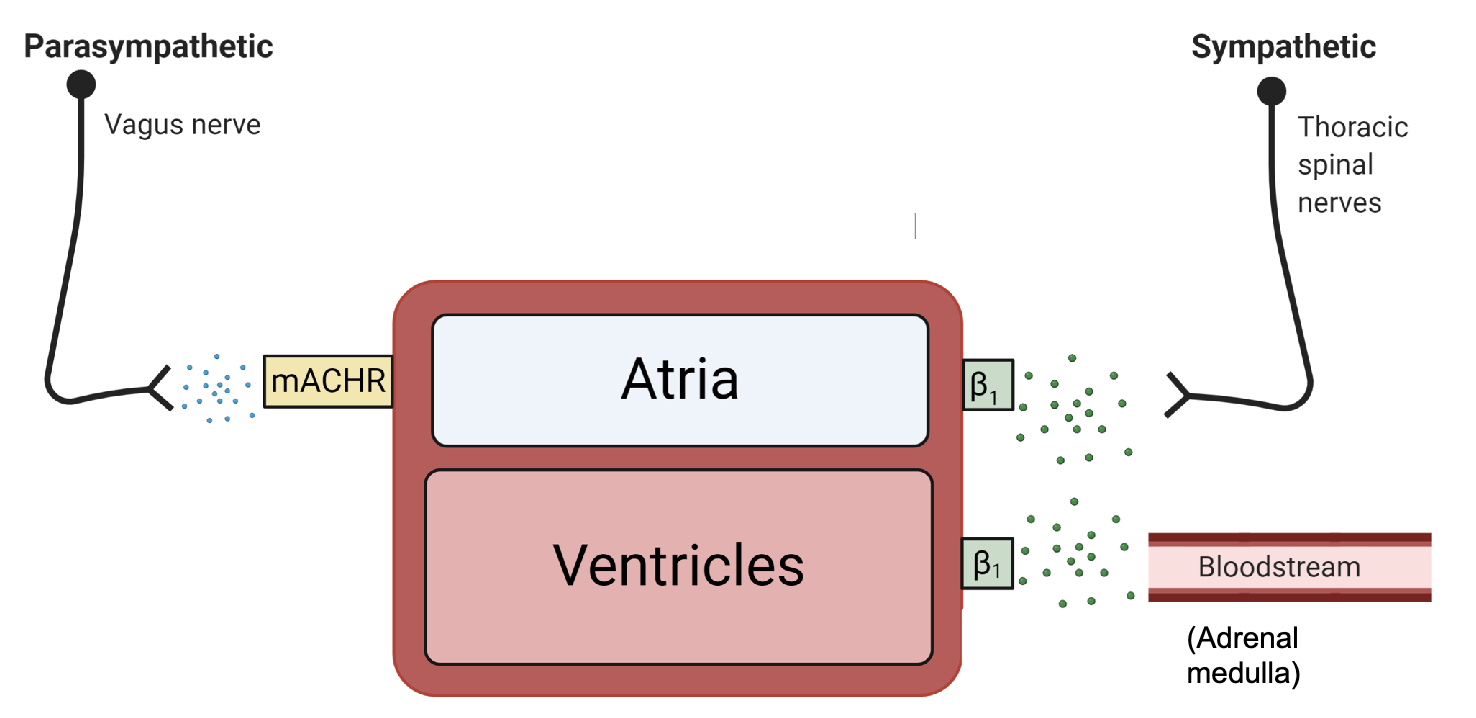
effects of parasympathetic
slower HR
weaker atrial kick
slower AV conduction
effects of sympathetic
faster HR
stronger contraction = increased CO
timing
NE is immediate
Epi supports NE effects and helps direct blood flow
control of heart rate
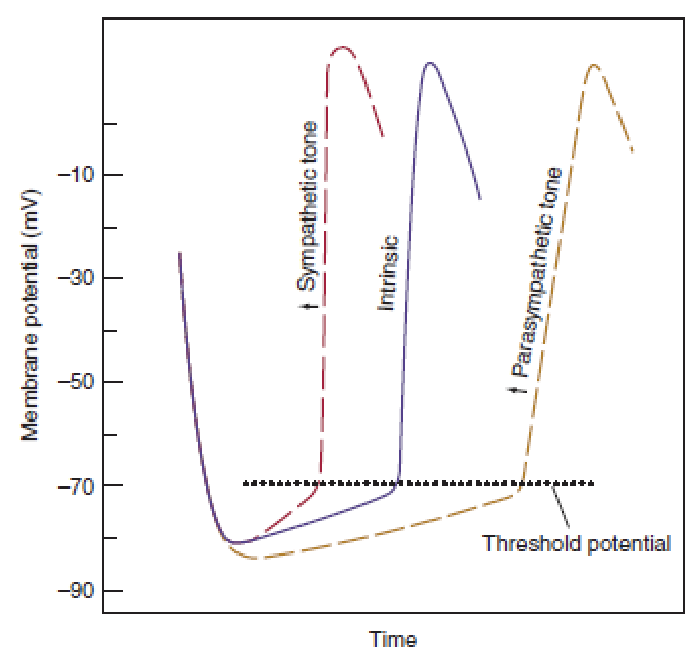
control of heart rate - resting individual
parasympathetic input = on
sympathetic = mostly off
control of heart rate - increased physical activity
decreased parasympathetic input
increased sympathetic input
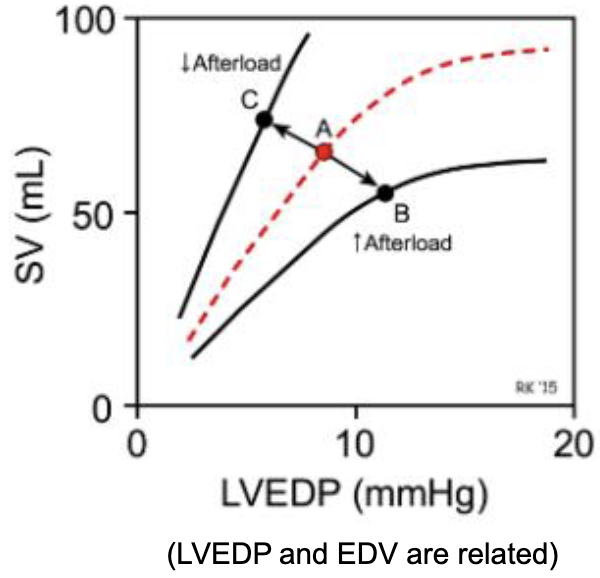
control of stroke volume
a. due to changes in EDV (aka load)
b. due to sympathetic stimulation (increased contractility)
c. due to MAP (afterload)
control of stroke volume
a. due to changes in EDV (aka load)
length tension relationship
increase in EDV
causes stroke volume to increase
HOW?
change filament overlap and spacing
increase Ca2+ release from SR
increase sensitivity of troponin to Ca2+
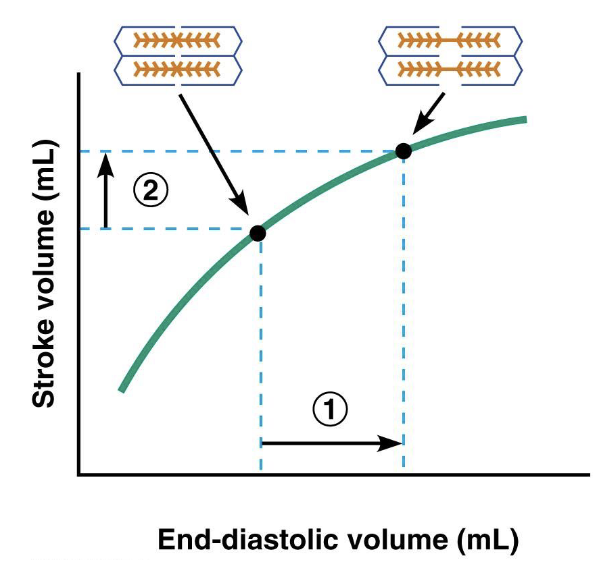
frank starling relationship
hearts stroke volume increases in response to a greater volume of blood entering the ventricles before contraction
increased EDV leads to a stronger contraction
implications of the frank starling relationship
control of ESV
prevents ESV from increasing (thus preventing clots)
matching of CO from LV and RV
outflow from right and left sides of the heart remain equal
prevention of rise in venous pressure (venous return determines EDV)
prevents blood from backing up into veins/capillaries
helps regulate the size of the heart
importance of matching output between RV and LV
any mismatch can lead to circulatory failure
control of stroke volume
b. due to sympathetic stimulation (increased contractility)
sympathetic stimulation results in increased SV without a change in EDV
*parasympathetic input does not directly impact the contractility of the ventricles (no/few m-ACh receptors on the ventricles)
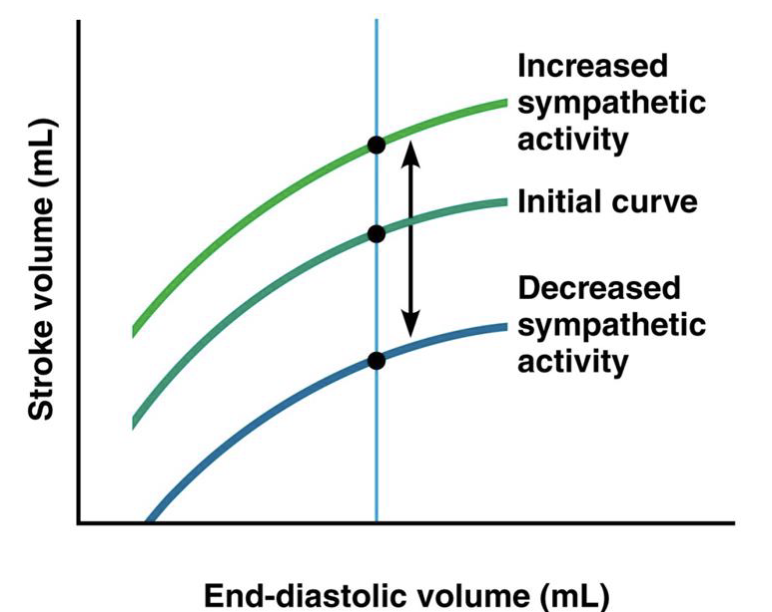
increased sympathetic stimulation results in
increased L-Ca2+ current (bigger trigger)
more Ca2+ into cytosol
more troponin saturation
faster Ca2+ removal (via SR pump)
END result of increased sympathetic stimulation
a stronger, faster (briefer) contraction
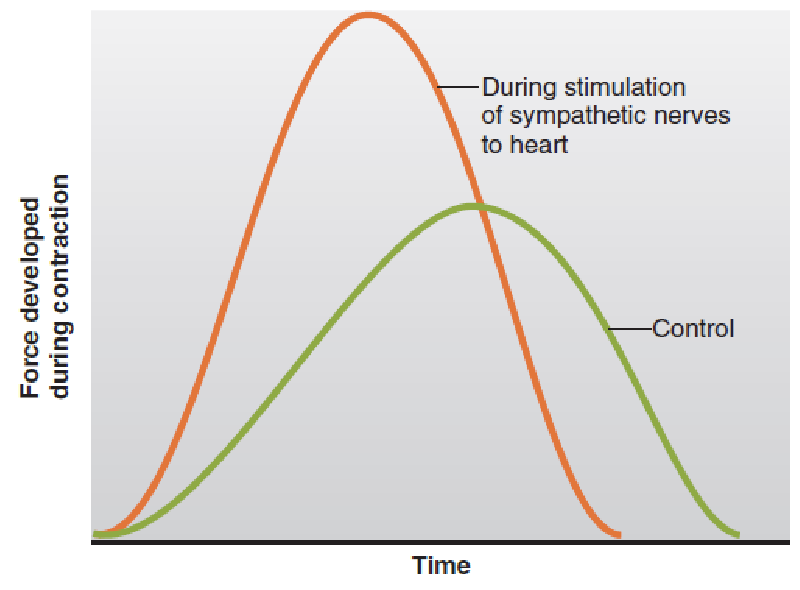
autonomic nervous system - impact on the function of the heart
control of stroke volume
c. due to MAP (afterload)
high mean arterial blood pressure (MABP) decreases stroke volume (assuming equal contractility and EDV)
INCREASED AFTERLOAD = DECREASES SV
increased pressure in arteries decreases the ability of ventricles to shorten
similar concept to placing a heavier load on skeletal muscle
for a healthy heart, afterload plays a minor role compared to other factors affecting CO
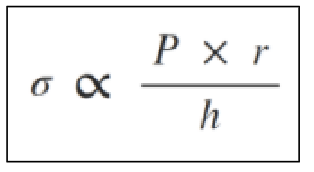
dilated cadiomyopathy
dilated cadiomyopathy
thinner wall results in increased afterload
wall stress (afterload)
control of stroke volume review
EDV (preload) - increases SV
contractility (sympathetic stimulation) - increases SV
afterload (~MAP) - decreases SV