Endocrine Drugs #2: Insulin et al
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
74 Terms
What are the two types of Diabetes? What is the difference between the two?
Diabetes mellitus (Insulin Based)
Issues with insulin (either to produce it (type I) or if the body has become resistant to it (type II))
Diabetes Insipidus (ADH hormone based)
A rare hormonal disorder causing excessive thirst (polydipsia) and urination (polyuria) due to issues with antidiuretic hormone (ADH), leading to watery urine
What is the difference between type I and type II Diabetes mellitus?
Type I
aka “Insulin Dependent“
Permanent/absolute deficiency due to destruction of pancreatic Beta Cells
Mostly seen in dogs
Type II
aka “Non-insulin Dependent”
Insulin resistance and Beta-Cell dysfunction
The cells don’t respond to insulin like they should
What function does Insulin serve?
It targets the liver, muscle, and fat cells.
It decreases gluconeogenesis and promotes glucose storage as glycogen
During an absolute or relative insulin deficiency, there is increased hepatic ___________ and __________, leading to hyperglycemia
Gluconeogenesis
Glycogenolysis
When there is not enough insulin the liver will start producing more glucose (gluconeogenesis) and breaking down stored glycogen (glycogenolysis), resulting in an elevated glucose level in the blood (hyperglycemia)
______ is a major factor for Diabetes Mellitus in cats, it can decrease insulin sensitivity by >50%
Obesity

_____ is co-secreted with insulin from the pancreas, if insulin secretion increases so does _____, why is this bad for the pancrease?
Amylin
This is bad for the pancreas because Amylin deposits in the Islets of Langerhans (Beta-cells) as Amyloid. Amyloid is toxic to the Islets and results in the apoptosis of Beta-cells
65-90% of cats with DM also have amyloid deposition
Patients may. have a preclinical diabetic period, what occurs during this period?
The patient is clinically normal
They have increased glucose despite increased insulin release
How can chronic Hyperglycemia result in DM?
Hyperglycemia and pancreatic amyloid are closely linked in Type 2 Diabetes, where chronic hyperglycemia increases the production of islet amylin, which eventually becomes Amyloid
Amyloid is toxic to the Islets of Langerhans (Beta cells) in the Pancreas resulting in their death
The damage to the Beta cells reduces insulin production → worsens the hyperglycemia → body tries to produce more insulin, and it also produces more Amyloid
A viscous cycle is created
What are the main goals of Insulin Therapy?
Resolve C.S
Normalize serum glucose concentration
Prevent secondary complications
Remission in cats
T/F: Oral Hypoglycemics are usually an effective method of managing DM
False, they are usually not efficacious
How do Oral Hypoglycemics work?
They stimulate insulin release from Beta Cells
Why aren’t Hypoglycemics generakky effective for dogs and cats?
Because diabetic dogs don’t have any beta cells, and cats don’t have many beta cells
There is nothing for the Oral Hypoglycemics to stimulate
Insulin is described by what 4 pieces of information?
Source
Species of origin
Onset and duration of action
Rapid vs intermediate/long acting
Formulation
Never oral, SC/IM
Potency
Usually 40 units per mL (easier to give in small amounts)
Which source of insulin is best used in cats?
Beef and Pork
Describe the difference between Basal Glucose and Postprandial Glucose
Basal glucose refers to the stable, fasting blood sugar level between meals
Postprandial refers to the elevated blood glucose level after eating
Prandial = referring/relating to a meal
In order to achieve normalglycemia 24/7, the patient needs a _____ and a _______ release of insuline
Basal
Postprandial
When should products used to treat DM be given IV?
For emergencies (this are usually rapid acting/short during insulin products)
When should products used to treat DM be given PO?
Nevah
Insulin exists as monomers, dimers, and hexamers, why is this important to know/understand?
Insulin Monomers and Dimers are considered to be the active form
Hexamers are the inactive forms
They are important as they keep insulin monomers (which are highly reactive) protected but available
In order to get the monomers the hexamers just need to be broken down
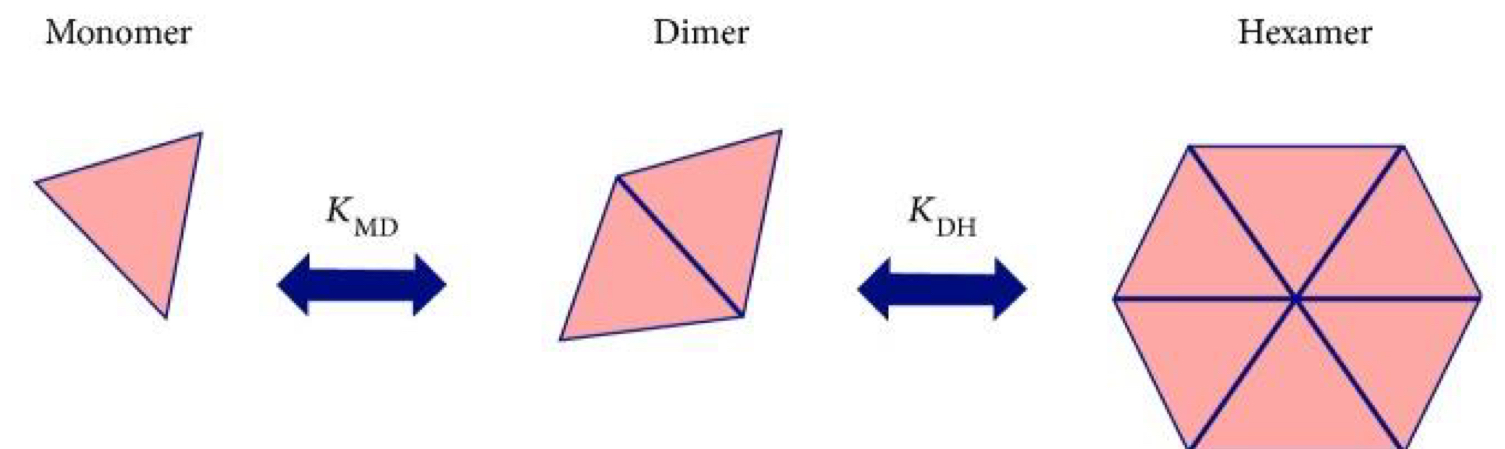
Insulin is often combined with __ to increase insulin hexamers and slow absorption
Zn
After injection into the SC, insulin monomers and dimers are readily absorbed by blood capillaries, what happens to the hexamers?
They are too large and cannot be absorbed by the capillaries
Instead they are absorbed into the lymphatics
Insulin hexamers that are absorbed by the lymphatics generally undergo a slow transport process before eventually entering the systemic circulation
Zinc and protamin ____ the dissociation rate of insulin
Slow
Niacinamide and citrate ______ the absorption rate of insulin
Increase
Short-acting _______ insulin used for the acute in-hospital management of diabetic ketoacidosis (what is diabetic ketoacidosis?)
Human (Humulin R, Novolin R)
Dangerous buildup of acidic ketones (as the result of fat breakdown for energy), leading to severe dehydration, electrolyte imbalances, and potential organ damage
Why is Regular Insulin (Humulin R, Novolin R) not used for long term treatment of DM?
It is short-acting (duration of effect 5-8 hrs)
Because of this, it would have to be given multiple times a day
What are the 2 intermediate acting insulins that we discuss?
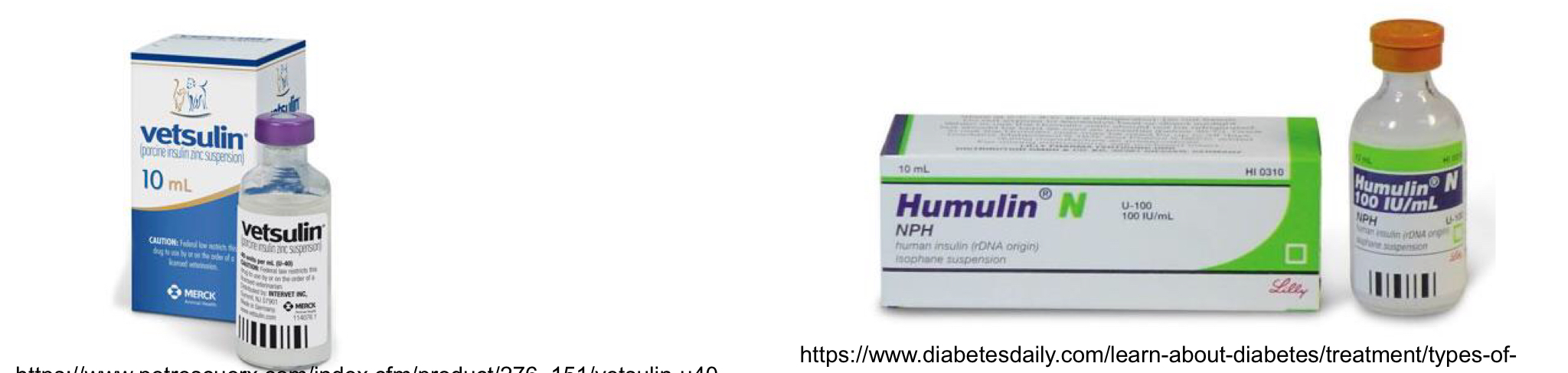
NPH (Humulin N, Novolin N less $$)
Porcine lente (Vetsulin)
NPH U-100 insulin is a crystalline ____ insulin combined with ______
Zinc
Protamine
Both are agents that slow the absorption of insulin, they cause insulin crystals at the injection site that need to dissolve before the hexamers can be broken down
NPH insulin is a good first line treatment for ____, but it can also be used in ___, just to variable duration of action
Dogs
Cats
For cats with insulin resistance and recurrent ketosis, what type of onset/potency would be most likely to be successful?
Shorter-acting insulins with greater potency (Intermediate)
________ is the only remaining animal source insulin that is still in use
Vetsulin (porcine)
Vetsulin (Porcine lente zinc insulin) is a lente product, what does lente mean?
Lente refers to intermediate-acting insulin for DM management
Lente means slow
Lente Insulins (such as Vetsulin) are biphasic, what does this mean? and why is it essential to how they function?
Biphasic means they have two phases
1st Phase
Shorter acting lente amorphous insulin (30%)
2nd Phase
Longer acting crystalline (70%)
These 2 phases allow Lente insulins (such as Vetsulin) to have both short and longer effects, making them intermediate insulins
T/F: Lente Insulins (such as Vetsulin) contain protamine and zinc but in higher concentrations
False, they just have zinc and acetate buffer
T/F: Intermediate acting insulins are given SID
False, they are usually given BID (sometimes can be SID)
The goal of DM treatment in cats is ________
Remission
What are the advantages of Vetsulin (Porcine lente zinc insulin)?
Accurate dosing
More predictable onset and peak than PZI (Protamine zinc insulin)
Some dogs can be treated SID, but <75% require BID
Which insulin utilizes Zinc and Acetate buffer to prolong its absorption?
Vetsulin (Porcine lente zinc insulin)
Can Vetsulin (Procine lente zinc insulin) be used for cats?
Yes, but
Shorter duration of action than when used in dogs
Poorer control of clinical signs then when used in dogs
Around a 20% remission rate
Long acting insulin analogues are _______ released from the injection site
Slowly
T/F: For the best control of diabetes mellitus Long acting Insulin is the way to go since it is in effect for the longest period of time
False! Intermediate is the the preferred method for better control of DM
What is the most commonly used long acting Insulin?
Glargine (Lantus)
PZI (Prozinc) is a _____-acting (U-40) ______ recombinant insulin
Long-acting
Human recombinant
T/F: PZI is a first choice for treatment of DM
False, it is more so a 2nd choice
The duration go PZI is usually __ hours, but it is given every __ to maintain therapeutic index
36
12
T/F: PZI can be given SID in cats to get them into remission
False, it should be given BID for that, if goal is not remission than it can be given SID to cats
What are the advantages and disadvantages of using PZI?
Advantages
Accurate dosing (40 U)
Longer duration of action than lente insulin
Disadvantages
More variable glucose lowering efects than shorter-acting insulins
Lower remission rates than other longer acting insulins (Glargine and detemir)
What onset of action do we reach for to treat diabetes mellitus in dogs?
Intermediate (NPH and Vetsulin)
What onset of action do we reach for to treat diabetes mellitus in cats?
Long acting (Glargine)
Glargine has been modified by replacing one asparagine amino acid with a glycine and adding two arginine amino acids to the c-terminal end of the molecule. This changes the __ and makes it ____________ at the SC injection site.
pH
Microprecipitate
The slow absorption at the injection site (caused by the microprecipitation) give Glargine its long duration of action
Glargine takes __ hours for the full effect to occur, why is this important to know?
72 hours
It means that daily increases of the dose, if the patient is not in its target glucose range, are inappropriate because the full effect of the initial dose of Glargine hasn’t taken effect yet
Which insulins can be used to treat diabetic ketoacidosis in cats?
Regular Insulin
Glargine
Vetsulin
What are the advantages and disadvantages of Glargine?
Advantages
Reduced frequency/severity of clinical hypoglycemia
Higher remission rates than Lente (vetsulin) and PZI
Disadvantage
100 U/mL concentration (which is not standard for vet med)
What is the difference between to 100 U and 40 U?
U-100 (100 units/mL) and U-40 (40 units/mL) represent different insulin concentrations;
U-100 is 2.5 times more concentrated than U-40.
U-100 is standard for humans, while U-40 is common for veterinary use.
In cats, ______ has similar efficacy to glargine
Detrimir
How is Detrimir (Levemir) different than Glargine?
It is newer
It is a long acting human insulin analogue (100 U) with an added fatty acid side chain to cause it to bind reversibly to albumin
What benefit does binding to albumin serve ______?
Detrimir
Binding provides a consistent absorption and prolonged duration of action due to slow release from the albumin into the plasma and slower excretion
Can Detrimir be used in dogs?
Yes
It is currently a 2nd choice for DM treatment, but that is currently because it is new and lacks the data
In some dogs it can result in imporved glycemic control
T/F: Detrimir is a good longterm insulin choice for small dogs, but not large ones
False
Since detrimir is a human analogue insulin it is dosed 100 U
This makes it difficult to get an accurate dose in small dogs
This is not an issue for larger dogs
_______ is often used in dogs with difficult to control DM
Detrimir
All insulins can accidentally cause _________
Hypoglycemia
What are some of the C.S of a patient with Hypoglycemia?
Tachycardia
Hunger
CNS (seizures/Coma)

How is Bexagliflozin (Bexacat) different from insulin based DM treatments?
It is a SGLT-2 (Na/Glucose cotransporter) Inhibitor
It ignores insulin and tries to control the amount of glucose in the body
How does Bexagliflozin work?
It inhibits SGLT-2 (Na/Glucose cotransporter) → Blocks the resorption of Na and glucose → Na and Glucose are expelled in the urine
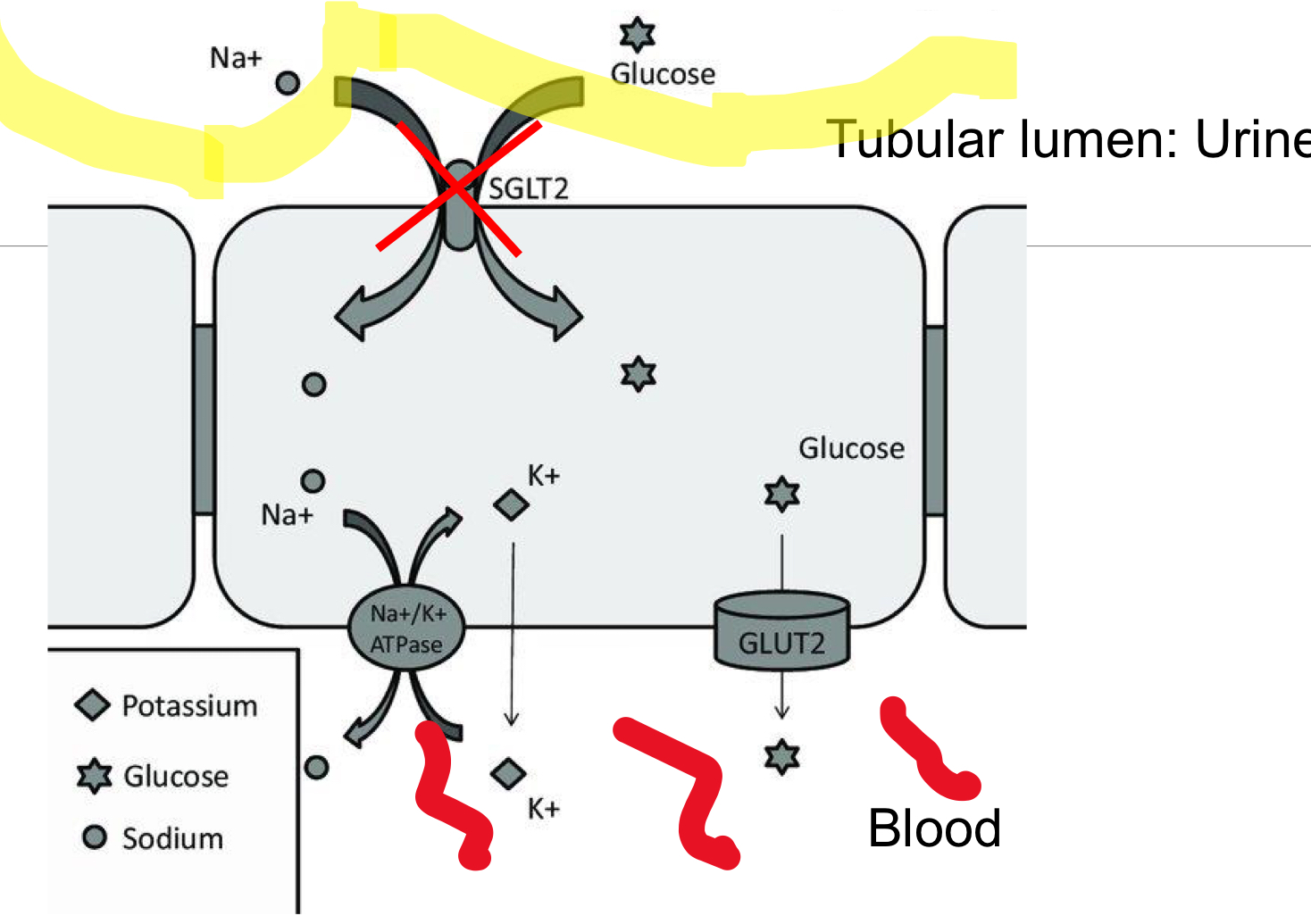
Bexagliflozin works specifically to treat type _ diabetes
Type II diabetes
Candidates for Bexagliflozin should be otherwise healthy and not have received _____ treatment, why?
Insulin
Sick cats and cats that have gotten insulin that receive Bexagliflozin are at an increased risk of diabetic ketoacidosis
If the body doesn’t have enough glucose for energy it will turn to fat stores → can cause diabetic ketoacidosis
What are Incretins?
Incretins are metabolic gut hormones, primarily GLP-1 and GIP, released after meals to increase insulin secretion from pancreatic beta cells in a glucose-dependent manner
What is the purpose of incretins?
They warn the liver and pancreas of incoming nutrients
How does Incretins work to treat DM?
GLP-1 is trophic for pancreatic Beta cells (islets of Langerhans)
It inhibits hepatic gluconeogenesis (production of glucose) and stimulates pancreatic insulin release
A popular human Incretin is ______
Ozempic
In the a future, Incretins/Incretin analogues may directly restore pancreatic function with minimal/no risk of _________
Hypoglycemia
______ is a GLP-1 receptor agonist (Incretin) that is safe to use in cats
Exenatide
Synthetic GLP-1 analogues (incretin analogues) are licensed for use in people with Type _ DM
2
Dogs with diabetes ______ require insulin therapy
Always
Which is the first choice for insulin treatment of DM in dogs? Intermediate/Long acting? Name at least one example of each
Intermediate is the correct choice
Vetsulin or NPH
Long acting
Glargine or PZI