Gas Exchange and Transport: O2 (Week 2, Mod 9)
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
25 Terms
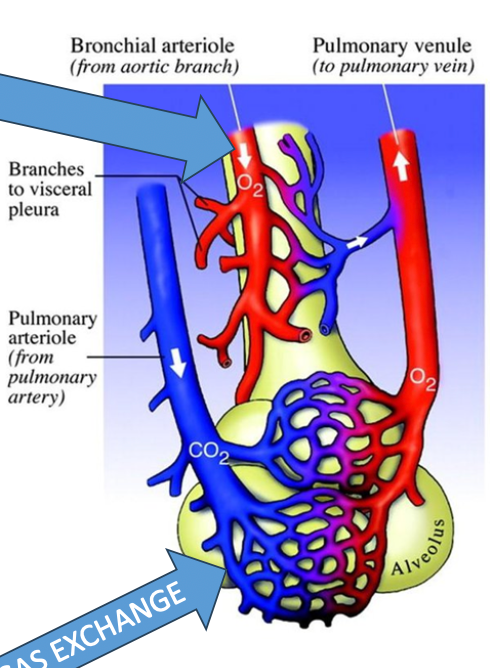
What are the 2 different types of circulatory systems in the lungs? Describe them.
1) Bronchial Circulation
Part of systemic circulation (oxygenates lung parenchyma)
Oxygenated blood is brought to the bronchial parenchyma… when it becomes deoxygenated, the deoxy blood is passed to the pulmonary venule (via anatomic shunt) to join the oxygenated blood there (see image)
Returns to the heart from there to be distributed through the body
2) Pulmonary Circulation
Arteries: Bring DEOXY blood from the heart to the capillaries that surround the alveoli
Brings deoxy blood to the areas of gas exchange
Veins: Brings NEWLY OXYGENATED blood from the lung to the heart, allowing the heart to pump oxygenated blood through the body
What are the “gas gradients” within the pulmonary circuit?
Remember: GAS ALWAYS MOVES FROM HIGH TO LOW PRESSURE
In the pulmonary circuit, O2 partial pressure is MUCH higher in the alveolus than it is in the deoxygenated blood (PO2 = 100 in alveolus, 40 in deoxy blood)
This means that O2 will easily pass into the deoxy blood from the alveoli, making partial pressure of O2 in the blood 100
Essentially, O2 enters the blood, while CO2 leaves
What are the “gas gradients” within the systemic circuit?
In the systemic circuit, partial pressure of O2 will be much higher in the blood than it is in the tissues initially (PO2 = 95 in blood, 40 in tissue)
As it passes by the deoxygenated tissues, O2 will move from the blood to the tissues, reducing its partial pressure in the blood BACK DOWN to 40
Will be returned to the heart / lungs for oxygenation
Essentially, O2 leaves the blood, CO2 enters
KNOW THE NUMBERS FOR YOUR GAS GRADIENTS
What is the PO2 when tissues, blood, or alveoli are oxygenated? What is the PO2 when they are DEoxygenated?
When oxygenated, whether its tissue, blood, or alveoli -> PO2 = 100-95
When deoxygenated -> PO2 = 40
What is the driving force for gas exchange at respiratory surfaces? In what way can these be maximized?
Diffusion is the driving force for gas exchange
To maximize gas exchange, the lipid membrane should be as thin as possible
Has its own issues though; easy to damage when thin
In vertebrates, who has the thickest respiratory membrane for gas exchange?
FISH
Due to environment and lifestyle (endotherm vs. ectotherm)
Goes from fish → amphibians → reptiles → mammals → birds
What is a “respiratory unit”?
Respiratory unit = gas exchanging unit:
A basic physiological unit of the lung consisting of respiratory bronchioles, alveolar ducts and alveoli
WHERE GAS EXCHANGE OCCURS
What is one factor that majorly influences the partial pressure of O2 within the body?
ATMOSPHERIC PRESSURE (Patm)
How do you calculate PO2 in the body, and how do its factors influence it?
Equation:
PO2 = Patm x F
Patm is in mmHg
F = mole fractional concentration of O2 in the air
IS CONSTANT: 0.21
So, if atmospheric pressure changes due to altitude at all, there will be a change in PO2 in the alveoli and blood
What is ANOTHER factor that can effect the PO2 in the body? How does this change the original PO2 equation?
The presence of humidity can REDUCE conc. of O2
PO2 is less in humidified air
PO2 of humidified gas in airways is calculated by:
PO2 = (PATM – PH2O) X FinhaledO2
Basically the same as the equation before, just subtracting the pressure of the humidity in the air from the atmospheric pressure
When inhaling, the partial pressure of the inhaled oxygen is = PIO 150, BUT by the time it gets to the alveoli for gas exchange, its reduced to PO 100. Why is this?
The amount of oxygen inhaled =/= oxygen AVAILABLE for gas exchange
This discrepancy is influenced both by HUMIDITY in the air (as discussed previously) and the amount of CO2 that is being produced / consumed in the body and passed into the pulmonary artery (see image)
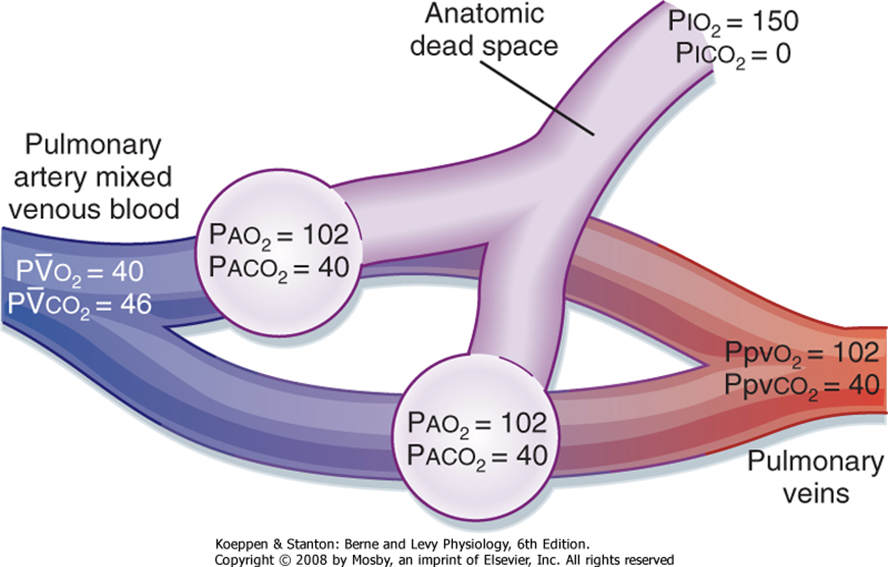
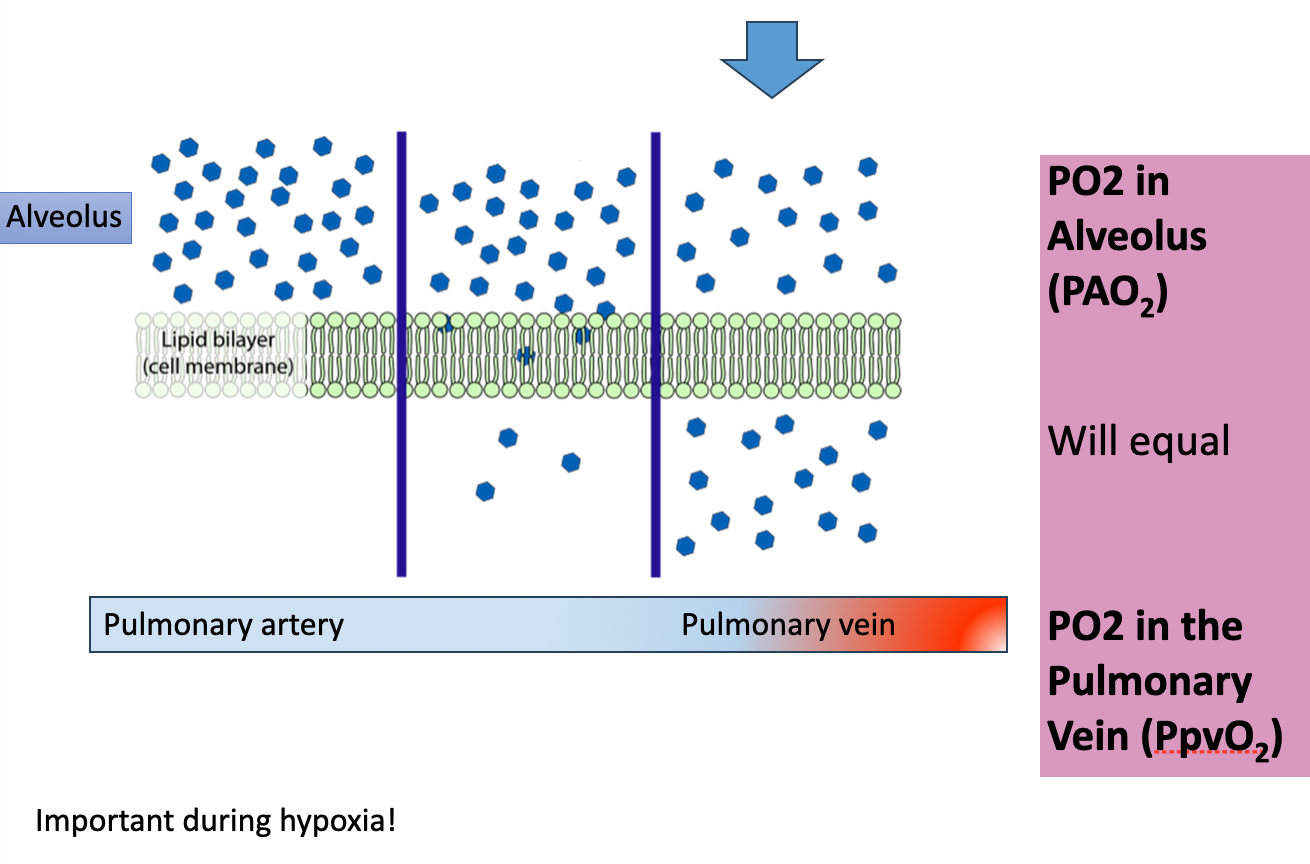
REMINDER!!! Gases will ALWAYS reach equilibrium!!!!
What are the 2 different ways that O2 is transported through the blood?
1) Dissolved in the blood (very small %)
2) Bound to hemoglobin
Composed of 4 heme groups, each of which contains iron in the reduced ferrous form (Fe++)
Is the site of O2 binding
What are 3 ways that the transportation of O2 can be influenced?
1) Concentration of pigment (Hb)
2) Rate of circulation
3) O2 affinity of pigment
Describe how the concentration of pigment (Hb) influences the transport of oxygen…
Concentration of pigments is very variable (birds and mammals 15-20mL/100mL)
The LESS pigment an animal has, the less efficient O2 transport is gonna be
Describe how the rate of circulation influences the transport of oxygen…
The circulatory system of mammals and birds operates at a leisurely pace at rest
During EXERCISE, O2 demand increases, so the circulatory system responds
Increases deoxygenation of venous blood, which then ENHANCES the delivery of O2 and increases its rate of circulation
Describe how the O2 affinity of hemoglobin influences the transport of oxygen…
At areas of HIGH PO2 (ie. lungs), Hb affinity for O2 INCREASES
At areas of LOW PO2 (ie. tissues), Hb affinity for O2 DECREASES
Makes sense that at areas of high PO2 (the lungs), O2 will have an increased affinity for Hb, while areas of low PO2 (tissues) will encourage O2 to leave Hb
When plotting the relationship between % saturation of O2 and PO2 for the dissociation curve, what shape does the graph take? Why is this?
A sigmoidal curve
Hb has 4 sites of binding for O2… the binding of O2 at one site increases the affinity for O2 at the remaining sites, resulting in a sharp increase in O2 saturation before quickly plateauing
Essentially, when one starts, the others quickly follow
Sheep flock analogy:
Trailer is your hemoglobin molecule
Whole flock is waiting for one sheep to get on, is very difficult at first
As soon as one goes, though, the rest follow easily
Same for unloading the trailer
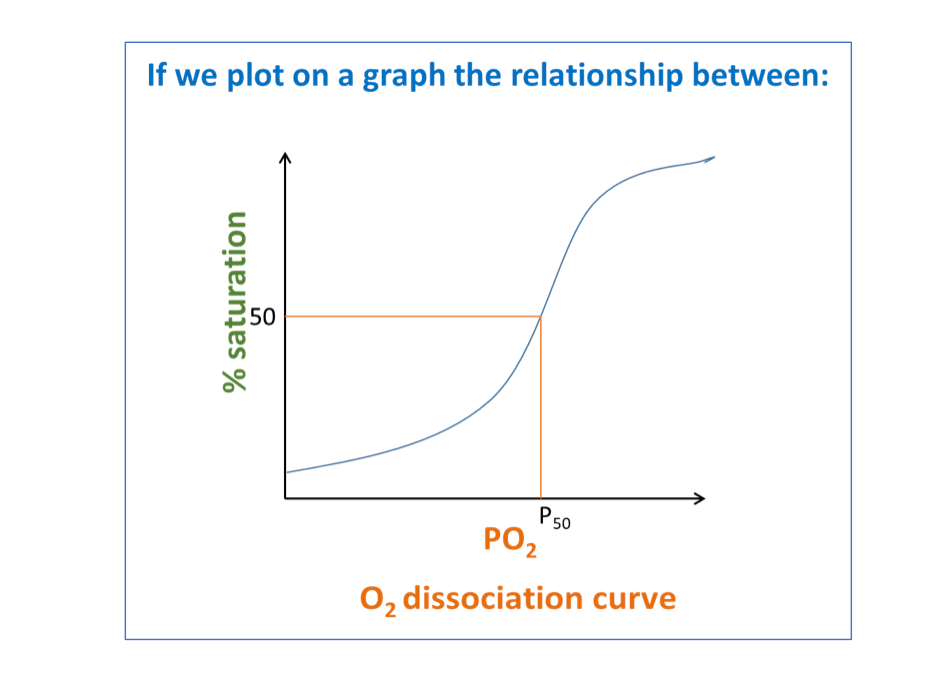
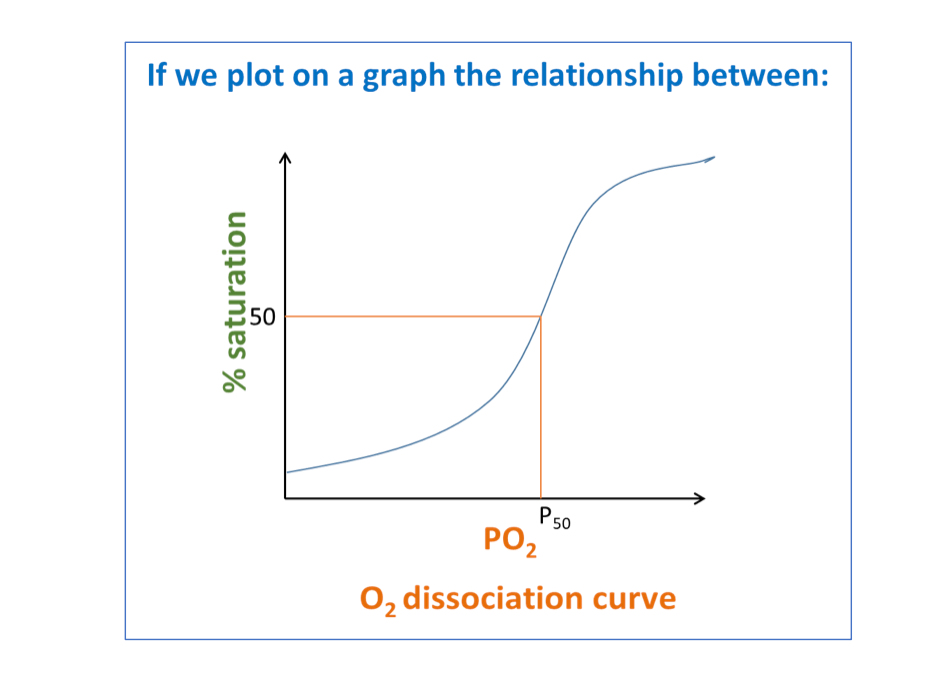
What is the P50 value in the O2 dissociation curve and what does it represent?
P50 = The partial pressure of O2 at which 50% of Hb is bound to O2
What does the O2 dissociation curve look like for myoglobin? Why is this?
Has a hyperbolic curve
Due to the fact that it only has ONE binding site for O2… doesn’t have exponential binding after the initial interaction like hemoglobin
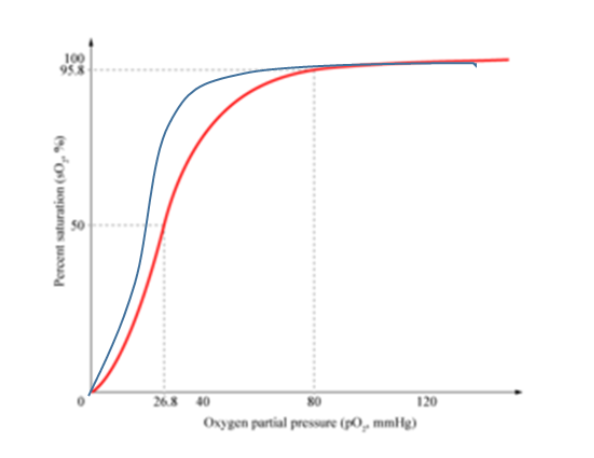
How do respiratory hemoglobins vary in their O2 affinity? How does this present on the O2 dissociation curve graph?
Hemoglobin will have a HIGHER AFFINITY for O2 at LOW PO2
Hemoglobin will have a LOWER AFFINITY for O2 at HIGH PO2
Lowering the Hb’s affinity for O2 shifts the sigmoidal curve TO THE RIGHT
What are the 4 factors that can affect Hb’s affinity for O2?
1) pH and CO2 - The Bohr Effect
2) Temperature
3) Ions
4) Organic compounds
Describe the Bohr shift and how pH and CO2 influence O2 affinity…
Reducing pH (makes things more acidic) or increasing PCO2 (which then ALSO lowers pH) lowers O2 affinity for Hb
Enhances O2 delivery
Dissociation curve then shifts to the RIGHT
Makes sense; during exercise, more metabolic processes are happening, which results in a higher CO2 release and a lowering in pH overall… will need more O2 during exercise, so these factors help to stimulate that
How does temperature influence O2 affinity?
An INCREASE in temperature DECREASES O2 affinity
Enhances O2 delivery to the muscles
Has a similar effect as the Bohr effect
How do ions and organic compounds reduce O2 affinity?
Ions:
Ions in the blood can allosterically modulate O2 affinity of respiratory pigments
Ex: Cl - ions in RBC are a critical allosteric modulator to O2 gas exchange
Organic compounds:
2,3 - diphosphoglycerate (DPG) reduces O2 affinity of Hb molecules it binds to
Can be increased via chronic hypoxia, anemia, and acclimation to high altitudes