Communication Assessment and Intervention
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
66 Terms
Normal Voice and Speech Production Systems
respiratory system
phonatory system
resonance
articulatory system
Respiratory system
lungs and diaphragm
phonatory system
larynx
resonance
pharynx, nasal cavity, oral cavity
articulatory system
Palate, tongue, teeth, cheeks, lips
Impact of Upper Airway Diversion: trach
Alteration to taste and smell
Reduced Secretion Management (sensation)
Unproductive cough (inflated cuff)
Reduced Subglottic Pressure
Reduced Sensation in Larynx
Redirection of airflow
Impact of Upper Airway Diversion..
and the resulting effects
reasons:
laryngeal tissue changes
tracheal injury
reduced laryngeal elevation
effects
loss of voice production
reduced subglottic air pressure
difficulty coordinating voicing and breathing
laryngeal tissue changes
Granulomas, vocal fold lesions, edema
Impact on glottic closure
tracheal injury comes from…
Damage from cuff inflation (necrosis)
reduced laryngeal elevation
Tube size: Larger diameter leaves minimal space for movement
Weight of tube: Increased weight = decreased elevation
Cuff inflation: Laryngeal tethering
loss of voice production
aphonia
dysphonia
reduced subglottic air pressure
Air exchange at neck reduces air pressure generation
difficulty coordinating voicing and breathing, particularly on…
the vent
respiratory specific considerations
COPD, tracheomalacia, sleep apnea, infections, obstructions
cardiovascular considerations
CVA, tumor, cardiac conditions
trauma diagnosis considerations
MVA (motor vehicle accident), GSW (gun shot wound), SCI (spinal cord injury)
degenerative disease considerations
ALS, MS, muscular dystrophy, Guillain-Barre
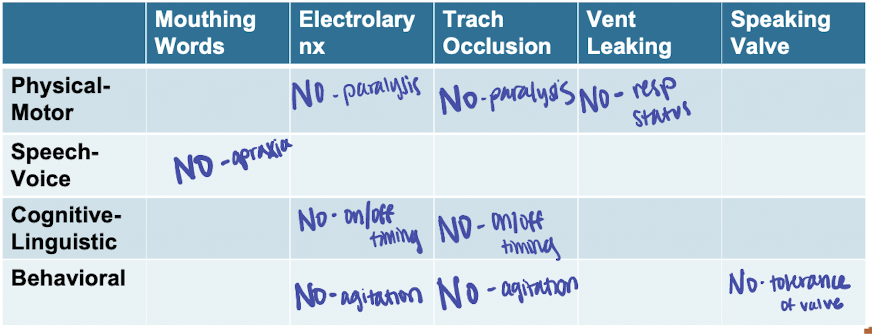
physical motor impairment considerations
AAC access considerations
Stoma occlusion
specific speech/voice impairment considerations (artic/resonance ability impacted)
Glottic cancer, Tongue cancer
Dysarthria/anarthria, apraxia, dysphonia/aphonia
cognitive-linguistic considerations
Complexity of communication option
Expressive/receptive language, memory, attention
behavioral considerations
Willingness to use the communication option
Anxiety, agitation, level of alertness
Upper Airway and Voice Assessment
At Minimum: ______________________
Ideal Scenario: _____________________
At Minimum: finger occlusion (first step in eval)
Ideal Scenario: laryngoscopy (FEES)
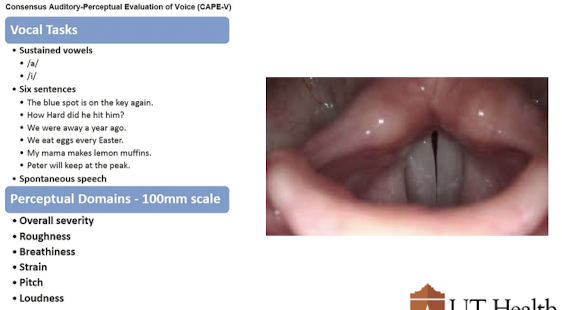
Perceptual Voice Assessment
At Minimum: ______________________
Ideal Scenario: _____________________
At Minimum: CAPE-V, GRABAS
Ideal Scenario: stroboscopy (need to look at vibratory characteristics)
What are the 4 main impairment areas you want to consider that will guide your voice/speech assessment and intervention planning?
physical motor impairment
specific speech/voice impairment
cognitive-linguistic
behavioral
Resulting effects of damage to the laryngeal tissue (from prior intubation or trach) include aphonia and dysphonia. Consider what specifically may contribute to development of Dysphonia
atrophy of VFs, incomplete closure bc they are so weak, laryngeal webbing
Resulting effects of damage to the laryngeal tissue (from prior intubation or trach) include aphonia and dysphonia. Consider what specifically may contribute to development of aphonia
nerve damage (can’t approximate VFs), stenosis
oral communication options with a trach
Mouthing Words
Electrolarynx
Trach Occlusion
Vent-Leaking
Speaking Valves (PMV)
Mouthing Words- how are they helpful?
Easy for some, quick in the moment, functional in many environments
Mouthing Words- directions for pts
over articulation (emphasize)
slow down
Mouthing Words challenges
Communication breakdowns are common
Dentures facilitate better articulation, but may not be present
electrolarynx is not just for…
HNC
electrolarynx pt needs
Good oral motor control
Physical ability to use
Ability to use mouthing words strategies
electrolarynx challenges
Finding the sweet spot (soft tissue spot)
Continuous skin contact
Volume and noise
Training time
cuff must be _______ for trach occlusion
deflated
trach occlusion procedure
Take a breath
Trach occluded
Patient phonates
Remove finger for breathing
trach occlusion challenges
Coordination of breath
Requires physical use of arm/finger to occlude
Infection control
vent-leaking
Suctioning of the oral cavity
Suctioning of the trach
Cuff deflation to allow leak
RT controls vent settings
Patient speaks on air leak around trach
vent-leaking challenges
Not all patients can tolerate a leak from the machine
Must have enough space between the tube and the trachea for the air to move up and out
speaking valves:
cuff:
may…
check what 2 things?
Cuff must be deflated
May require trach change to a smaller sized trach
Check finger occlusion first
Check back pressure
May be used on or off the vent
back pressure
hear a whoosh of air after taking off PMV, not enough room for air to escape, need adequate space for air to move around the tube
what do you monitor closely for speaking valves?
Heart rate
Respiratory rate
O2 saturations
clinical benefits of PMV
improves speech production
Improves swallowing and may reduce aspiration
restores natural positive airway pressure
facilitates secreation management
improves oxygenation
expedites ventilator weaning and decannulation
facilitates infection control
improves smell, taste, and sensation
facilitates pediatric speech/language development
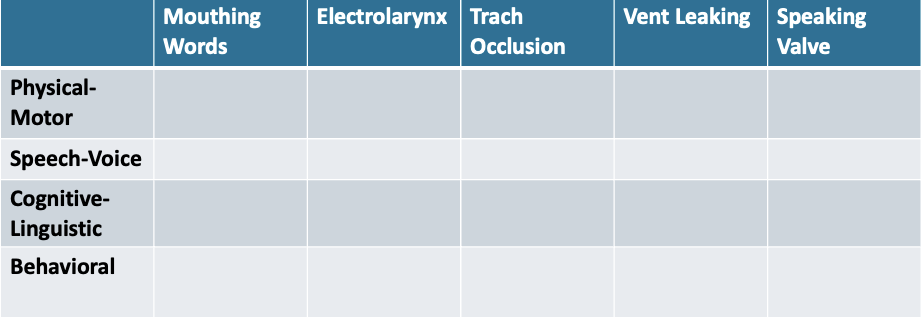
Consider the 4 main impairment considerations (slide 7). For each, state which oral communication methods would NOT be appropriate to consider for each in the table below:
In-Line PMV Assessment on the Vent Steps
Cuff deflation (RT)
RT present to manage vent
PMV placed in-line with vent tube
Pt voices after inhale triggered from vent
Monitor for tolerance
Remove PMV (after trial is over)
Replace vent tubing
RT restores vent settings
Relay the findings to pt and team (are they a good candidate?)
what happens after In-Line PMV Assessment on the Vent?
trach collar (ideal scenario bc no support from vent)
PMV on trach collar steps
Cuff deflation
Patient education (explain what will happen)
Finger occlusion
PMV placement
Check back pressure after approx. 15-30 secs (difficulty with airflow movement)
Replace if tolerated, continued speaking
Monitor for about 30 min if tolerated (can wear for a meal)

why do we do finger occlusion first?
to see if they can generate voice and mobilize air
PMV Stop Criteria (On or Off the Vent)
Back pressure at trach site
HR > 20bpm from baseline
RR > 35
O2 < 90
we don’t want to see spikes in these areas
Troubleshooting: Maximizing Airflow Around the Trach
Trach modification (most common)
Switch to fenestrated trach
Trach modification
size & cuff
Pts often started with 8-0 CUFFED for vent use
Downsize to 6-0 CUFFLESS often required for smaller stature patients
Switch to fenestrated trach
Must have fenestrated inner cannula
Risk of granulation tissue growing into trach
Contraindications for Speaking Valves
Tracheal or laryngeal stenosis
Airway obstruction
Inability to tolerate cuff deflation
End-stage pulmonary disease
Unstable medical/pulmonary status
Laryngectomy (physically separate from upper airway)
Severe anxiety
My patient can’t wear the PMV because…
“… they had a severe brain injury”
“… they have too many secretions”
Secretions increase in response to …
trach tube in airway
Excess secretions are result of…
poor laryngeal/pharyngeal sensation, reduced subglottic pressure, poor cough strength
_______% reduction in secretion accumulation with PMV
40%
“…they had a severe brain injury”
Early placement increases sensation to upper airway
May promote vocalizations
Requires closer SLP/RT monitoring
Training Speech with a PMV Steps
Patient must first acclimate to the valve wear
Cue the patient to inhale
Open vowel on exhale (ah)
Inhale- voice- inhale
Work up the speech hierarchy (vowel, syllable, word,…)
articulation intervention
Facial ROM and strengthening exercises
Open vowels, Syllables, Words, Phrases, Sentences, Reading, Spontaneous speech
resonance intervention
Improving oral/nasal resonance with voice techniques
SOVT (lip-trills, hum), resonant voice exercises
phonation intervention
Direct voice treatments
glottal adduction exercises (Phorte, LSVT), vocal function exercises (pitch range),
respiration intervention
Improve inspirtory and expiratory strength (IMST/EMST)
Target respiratory-phonatory coordination
Non-Oral Communication Supports
Call Light/Buzzer
Writing
Yes/No Response system
Low-Tech Communication Boards
Text to Speech App
High-Tech AAC SGDs
List 2 contraindications for PMV wear
laryngectomy
severe anxiety
In your own words, what does back pressure mean?
inability to efficiently move air like we need to
Describe aloud what the process is for PMV placement with a patient
this valve is going to go over your trach tube
make sure that your balloon is deflated becuase we need the air to come up to the VFs in order for your to voice.