Dental Specialties Proc & Exp Funct- Ch 55- COMPLETE
1/50
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
51 Terms
What can the dental assistant assist with during periodontal procedures?
periodontal charting
periodontal surgeries
provide home care instructions to the patient
The Periodontal Practice
Patients are referred by the general dentist or dental hygienist for treatment of a periodontal condition
*After the periodontal treatment, the patient will return to the general dentist for routine dental care
*Frequently, periodontal patients will alternate periodontal maintenance (cleaning) appointments between the periodontist’s office and the general dentist’s office
The Periodontal Examination
A periodontal examination includes:
Medical and dental history
Radiographic evaluations
Examination of the teeth
Examination of the oral tissues
Supporting structures
Periodontal charting
Periodontal charting includes pocket readings, furcation's,*tooth mobility, exudate (pus), and gingival recession
Medical and Dental History
Systemic diseases such as acquired immunodeficiency syndrome, human immunodeficiency virus infection, and diabetes can decrease resistance of the tissue to infection
Dental history used to gather information about conditions that could indicate periodontal disease
For example, patients with periodontal disease often complain
* of bleeding gums
* loose teeth
* bad taste in the mouth
Dental Examination
Mobility
It is normal for teeth to have a slight amount of mobility (tooth movement) because of the cushioning effect of the periodontal membranes
Excessive mobility important sign of periodontal disease
Oral Tissues and Supporting Structures
The periodontal examination includes:
Assessment of the amounts of plaque and calculus
Changes in gingival health and bleeding
Assessment of the level of bone
Detection of periodontal pockets
Supporting Structures
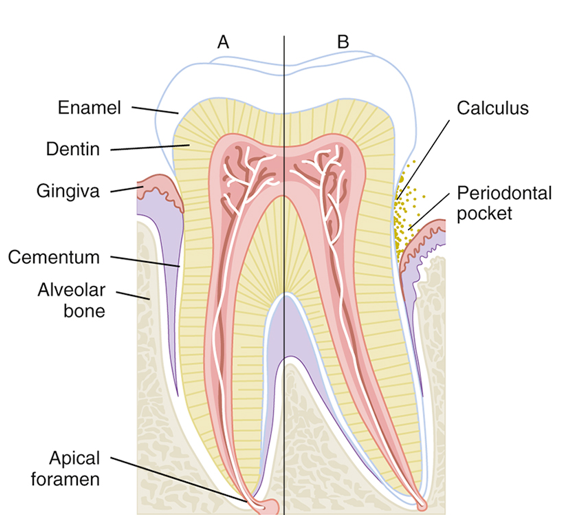
Periodontal Probing
A periodontal pocket results when the gingival sulcus becomes deeper than normal (<3 mm)
Periodontal probing measures how much epithelial attachment has been lost to disease
The greater the depth of the periodontal pocket results in
* the greater the loss of epithelial attachment
*the greater loss of bone
*more serious the periodontal disease
Periodontal pockets are very difficult, and sometimes impossible, for the patient to clean
Early Signs of Periodontal Disease
Changes in the gingiva (color, size, shape, texture)
Gingival inflammation
Gingival bleeding
Evidence of exudates
Development of periodontal pockets
Bleeding Index
The severity of gingival inflammation can be measured by the bleeding index
Several different systems of recording bleeding scores are used
Occlusal Adjustment
Patient’s bite is evaluated for areas of unequal pressure
Occlusal trauma can result if excessive biting pressure is noted in a specific area
Occlusal adjustment: Procedure that adjusts patient’s bite so that occlusal forces are equally distributed over all the teeth
Radiographic Analysis
Radiographs are a valuable aid for evaluating periodontal disease
Bitewing radiograph: Can accurately depict bone height along the root surface
Vertical bitewing radiographs are excellent for determining the extent of crestal bone loss
Periodontal Instruments
Periodontal therapy requires the use of specialized instruments
*to remove calculus,
*smooth root surfaces
* measure periodontal pockets,
*perform periodontal surgery
In general, the dentist or registered dental hygienist who uses these instruments takes responsibility for maintaining their sharpness
Periodontal Probes
Used to locate and measure the depth of periodontal pockets
On some types of probes, the tip is color-coded to make the measurements easier to read
Periodontal probe
* tapered to fit into the gingival sulcus
* shape is blunt or rounded tip
Six measurements are taken and recorded for each tooth
Scalers and Files
Sickle scalers are used primarily to remove large deposits of supragingival calculus
Chisel scalers are used to remove supragingival calculus in the contact area of anterior teeth
The blade on the chisel scaler is curved slightly to adapt to the tooth surfaces
Hoe Scalers are used to remove heavy supragingival calculus
Hoe Scalers are most effective when used on buccal and lingual surfaces of the posterior teeth
Curettes
Curettes are used to remove
*subgingival calculus,
*smooth rough root surfaces (root planning),
*remove the diseased soft tissue lining of the periodontal pocket (soft tissue curettage)
A curette has a rounded end, unlike a scaler, which has a pointed end
Two basic designs of curettes
Universal
Gracey
Types of Curettes
Universal curettes are designed so that one instrument can be used on all tooth surfaces
Gracey curettes have only one cutting edge and are area-specific
They are designed for use on specific tooth surfaces (mesial or distal)
Treatment of the entire dentition requires the use of several curettes
Pocket Markers
These perforations, which are referred to as bleeding points, are used to outline the area for an incision on the gingivae
Ultrasonic Scaler
Allows for rapid calculus removal and reduces hand fatigue for the operator
Works by converting very-high-frequency sound waves into mechanical energy in the form of very rapid vibrations
A spray of water at the tip prevents the buildup of heat and provides a continuous flushing of debris and bacteria from the base of the pocket
Because of the spray of water at the tip, there is a large amount of potentially contaminated aerosol spray
Highly desirable for the operator of an ultrasonic scaler to have the dental assistant help with using the high-volume evacuator to minimize aerosol contamination.
Indications for Use of the Ultrasonic Scaler
Removal of supragingival calculus and difficult stains
Removal of subgingival calculus, attached plaque, and endotoxins from the root surface
Cleaning of furcation areas
Removal of deposits before periodontal surgery
Removal of orthodontic cements; debonding
Removal of overhanging margins of restorations
Contraindications to Use of the Ultrasonic Scaler
Communicable disease: transmitted by aerosols, such as tuberculosis, poses a risk to the operator
Immunocompromised: A compromised patient is open to infection
Respiratory problems: Materials can be aspirated into the lungs of a patient with respiratory problems
Swallowing difficulty: Problems with swallowing or a severe gag reflex
Cardiac pacemaker: Consultation with the patient’s cardiologist is necessary
Precautions for Children
Young tissues are very sensitive to ultrasonic vibrations
These vibrations and heat may damage the pulp tissue of primary and newly erupted permanent teeth
Nonsurgical Periodontal Treatment
Dental prophylaxis
Prophylaxis is the complete removal of
*calculus
* soft deposits
* plaque
*stains from all supragingival
* unattached subgingival tooth surfaces
Dentist and dental hygienist are licensed to perform this procedure
Scaling, Root Planing, and Gingival Curettage
Scaling and root planing are done as part of a periodontal debridement
In some cases, gingival curettage, a nonsurgical technique, may also be indicated
A local anesthetic is usually administered before these procedures
Scaling
Scalers
*supragingival calculus from the tooth surface
Curettes
*remove supragingival and subgingival calculus
Root Planing
Root planing is performed after scaling procedures to remove any remaining particles of calculus and necrotic cementum embedded in the root surface
After root planing, the surfaces of the root are smooth and glasslike
Anesthetic is usually required for this procedure
Gingival Curettage
Curettage means scraping or cleaning with a curette
Some patients also require gingival curettage in addition to scaling and root planing
Gingival curettage, also known as subgingival curettage, is the scraping of the gingival lining of a periodontal pocket
This is performed to remove necrotic (dead) tissue from the pocket wall
Antimicrobial and Antibiotic Agents
Tetracycline is an antibiotic that is particularly useful for the treatment of periodontitis
Penicillin
Fluoride mouth rinses
A twice-daily chlorhexidine rinse (Peridex) is the most effective means available for reducing plaque and gingivitis
Locally Delivered Antibiotics
New methods can be used to apply antibiotics directly into the periodontal pockets
In one technique, a fiber that contains tetracycline is packed into periodontal pockets
Other methods include using a syringe to insert dissolvable materials such as a gel into the pocket
A dissolvable chip that releases chlorhexidine is inserted into deep pockets
Surgical Periodontal Treatment
When nonsurgical treatment is ineffective in stopping the disease process, periodontal surgery is indicated to control the progress of periodontal destruction and loss of attachment.
Advantages of Periodontal Surgery
*Allows access to the root surface for scaling and root planing
*Makes it easier for the patient to clean difficult areas
*Results in better access to furcations and other areas that are very difficult to reach during traditional scaling and root planing
Disadvantages of Periodontal Surgery
The health status of the patient, age of the patient as well as limitations of the procedures
From the patient’s point of view: Time, cost, esthetics, and discomfort
Excisional Periodontal Surgery
This surgery is used to remove the excess tissue
It is the most rapid means of reducing periodontal pockets
Common Types of Excisional Surgeries:
*Gingivectomy
*Gingivoplasty
Gingivectomy
Gingivectomy is the surgical removal of diseased gingival tissues
Performed when it is necessary to reduce the depth of the periodontal pocket and when fibrous gingival tissue must be removed
Recently, the use of dental laser equipment in gingivectomy has become popular
Gingivoplasty
*surgical reshaping
*contouring of the gingival tissues
Incisional Surgery
Incisional surgery known as periodontal flap surgery or simply flap surgery
Performed when an excisional surgery is not recommended
Osseous (Bone) Surgery
Periodontal surgery that involves modification of the supporting bone
This surgery is performed to eliminate pockets, remove defects, and to restore normal contours in the bone
Two types of bone surgeries are:
Osteoplasty
Ostectomy
Osteoplasty
In osteoplasty, or additive surgery,
*bone is contoured and reshaped
In addition, bone may be added, either through bone grafting (taking bone from one area and placing it in another) or placement of bone substance.
Ostectomy
In ostectomy, or subtractive surgery, bone is removed
This procedure is necessary when the patient has large exostoses (bony growths)
For example, ostectomy is performed if a patient needs a denture and the bony growth would interfere with the comfort and fit of the denture
Crown Lengthening
A surgical procedure that is designed
* to expose more tooth structure for the placement of a restoration such as a crown
Crown lengthening is becoming a very common procedure for esthetic anterior restorations
Soft Tissue Grafts
Pedicle graft
The pedicle graft is “freed” on three sides but remains attached on one side and retains its blood supply
Free gingival soft tissue graft
Has a donor site that is located away from the grafted site
Postsurgical Patient Instructions
After surgery, the periodontist will most likely prescribe an analgesic and possibly an antibiotic
Many periodontists recommend the use of an antibacterial rinse twice a day to help with plaque control
A chlorhexidine mouthwash may also be used during the first week to freshen the mouth and inhibit plaque formation during the early stages of healing
Postoperative instructions should be given to the patient to ease discomfort and promote healing
Periodontal Surgical Dressings
Periodontal dressings, also known as periopacks, are used to:
Hold the flaps in place
Protect the newly forming tissues
Minimize postoperative pain, infection, and hemorrhage
Protect the surgical site from trauma during eating and drinking
Support mobile teeth during the healing process
Types of Periodontal Surgical Dressings
The most commonly used materials are:
Zinc oxide–eugenol (ZOE) dressing
Noneugenol dressing
ZOE Dressing
Patient may experience redness and burning pain in the area of the dressing
ZOE dressings are supplied as a powder and a liquid that are mixed before use
Material may be mixed ahead of time, wrapped in waxed paper, and frozen for future use
ZOE has a slow set time, which allows for a longer working time
Sets to a firm, heavy consistency and provides good protection for tissues and flaps
Some patients are allergic to the eugenol
Noneugenol Dressing
Most widely used type of periodontal dressing
Supplied in two tubes: One of base material and the other of the accelerator
Easy to mix and place and has a smooth surface for patient comfort
Has a rapid setting time if exposed to warm temperatures
Cannot be mixed in advance and stored
Lasers in Periodontics
The term laser is an acronym for light amplification by simulated emission of radiation
A laser beam is a highly concentrated beam of light
Power of this beam can be adjusted to enable it to cut, vaporize, or cauterize tissue
The use of lasers is a promising new technology in dentistry
Use of Lasers on Soft Tissue
*Removal of tumors and lesions
*Vaporization of excess tissues, as in gingivoplasty, gingivectomy, and frenectomy
*Removal of or reduction in hyperplastic tissues
*Control of the bleeding of vascular lesions
*Aid in the removal of cold sores on the lip
Advantages of Laser Surgery over Conventional Surgery
Laser incisions heal faster than incisions made with electrosurgery
*Hemostasis (control of bleeding) is rapid
*The surgical field is relatively dry
*The opportunity for bloodborne contamination is reduced
*There are fewer traumas to adjacent tissues
*There is less postsurgical swelling, scarring, and pain
*Some procedures can be performed more quickly
*Patients who are afraid of “surgery” may accept this method
Laser Safety
Precautions must be taken to protect both the patient and dental staff during laser procedures
Any person who operates a laser or assists during a laser operation must be thoroughly trained in the use of this powerful instrument
Guidelines for Laser Safety
*Shielded eyeglasses: Protect the eyes; dental staff and patient must wear special shielded eyeglasses
*Matte-finished instruments: Reflective surfaces such as instruments, mirrors, and even polished restorations can reflect laser energy
*Protection of nontarget tissues: Nontarget oral tissue (tissues not being treated with the laser) should be shielded with the use of wet gauze packs
*High-volume evacuation: High-volume evacuation should be used to draw off the plume (cloud) created when tissue vaporizes
This plume should be considered infectious