KNES 323 - Blood Pressure
1/36
Earn XP
Description and Tags
lectures 20 + 21
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
37 Terms
Blood pressure is an important ___________ pressure measure in the body that is defined as:
hydrostatic, the force exerted by blood upon the walls of the blood vessels and on the chambers of the heart
Arterial blood pressure in the larger vessels consists of several distinct components. What are they? (4)
systolic BP (top number)
diastolic BP (bottom number)
pulse pressure (difference between systolic + diastolic BP)
mean arterial pressure
Systolic pressure reflects the ____________ resulting from a ________________.
Diastolic pressure reflects the ____________ during _______________.
peak arterial pressure, ventricular contraction
arterial pressure, ventricular relaxation
Pulse pressure should be at least ______ of the systolic pressure.
25%
What does a low pulse pressure indicate? What does a high pulse pressure indicate?
low (narrow): may indicate a low stroke volume as seen in congestive heart failure, stenosis of the aortic valve, etc.
high (wide): common in healthy people during + following strenuous exercise
How is mean arterial pressure calculated? Why?
1) adding 1/3 of the pulse pressure to the diastolic pressure or
2) adding 1/3 of the systole pressure to 2/3 of the diastole pressure
the cardiac cycle is roughly spent as 1/3 in systole and 2/3 in diastole
What are the 5 main variables that affect blood flow and blood pressure?
cardiac output
compliance
volume of the blood
viscosity of the blood
blood vessel length + diameter
Any factor increasing cardiac output will _____________ blood pressure. What are some of those factors?
Any factor decreasing cardiac output will ____________ blood pressure. What are some of those factors?
increase
sympathetic stimulation, epinephrine, norepinephrine, thyroid hormones, increased Ca2+
decrease
parasympathetic stimulation, altered K+ levels, decreased Ca2+
What is compliance? Are veins or arteries more compliant? When is compliance reduced and what are the effects on blood flow?
ability of a blood vessel to expand to accommodate increased content → a compliant vessel is able to expand with surges in blood flow without increased resistance or blood pressure
veins are more compliant than arteries + therefore can hold more blood
compliance is reduced when arteries are stiffened (hypertension) and resistance to blood flow is increased
When does blood volume decrease? When does it increase?
decrease: dehydration, vomiting, severe burns, diarrhea, bleeding
increase: retention of water + Na+
What are the 2 main determinants of blood viscosity? The viscosity of blood is directly proportional to _____________ and inversely proportional to _____________.
formed elements + plasma proteins, resistance, flow
Vessel length is ______________ to its resistance. Why?
directly proportional
longer vessels have greater resistance causing lower flow
shorter vessels have lower resistance causing greater flow
How does blood vessel diameter affect resistance and blood pressure?
smaller diameter increases the amount of blood contacting the vessel walls, increasing both friction and resistance → increasing BP
What is Poiseuille’s Law?
resistance is inversely proportional to the radius of the vessel raised to the fourth power (R = 1/r4)
How does the skeletal muscle pump work?
increases pressure in the veins through contraction of surrounding skeletal muscles
leg muscles contract, they exert pressure on nearby veins which causes blood to flow upwards
upward blood flow opens valves superior to the contracting muscles so blood flows through
simultaneously, valves inferior to contracting muscles close, preventing blood flow back to the feet
How does the respiratory pump aid blood flow through the veins of the thorax and abdomen?
during inhalation, volume of the thorax increases + compresses the abdominal cavity, which decreases air pressure in the thorax
thorax vein blood pressure decreases to below abdominal vein pressure
blood flows along its pressure gradient from abdominal veins to thoracic veins, then to the atria
during exhalation, air pressure increases within the thoracic cavity, thoracic vein BP also increases, which increases blood flow velocity into the heart
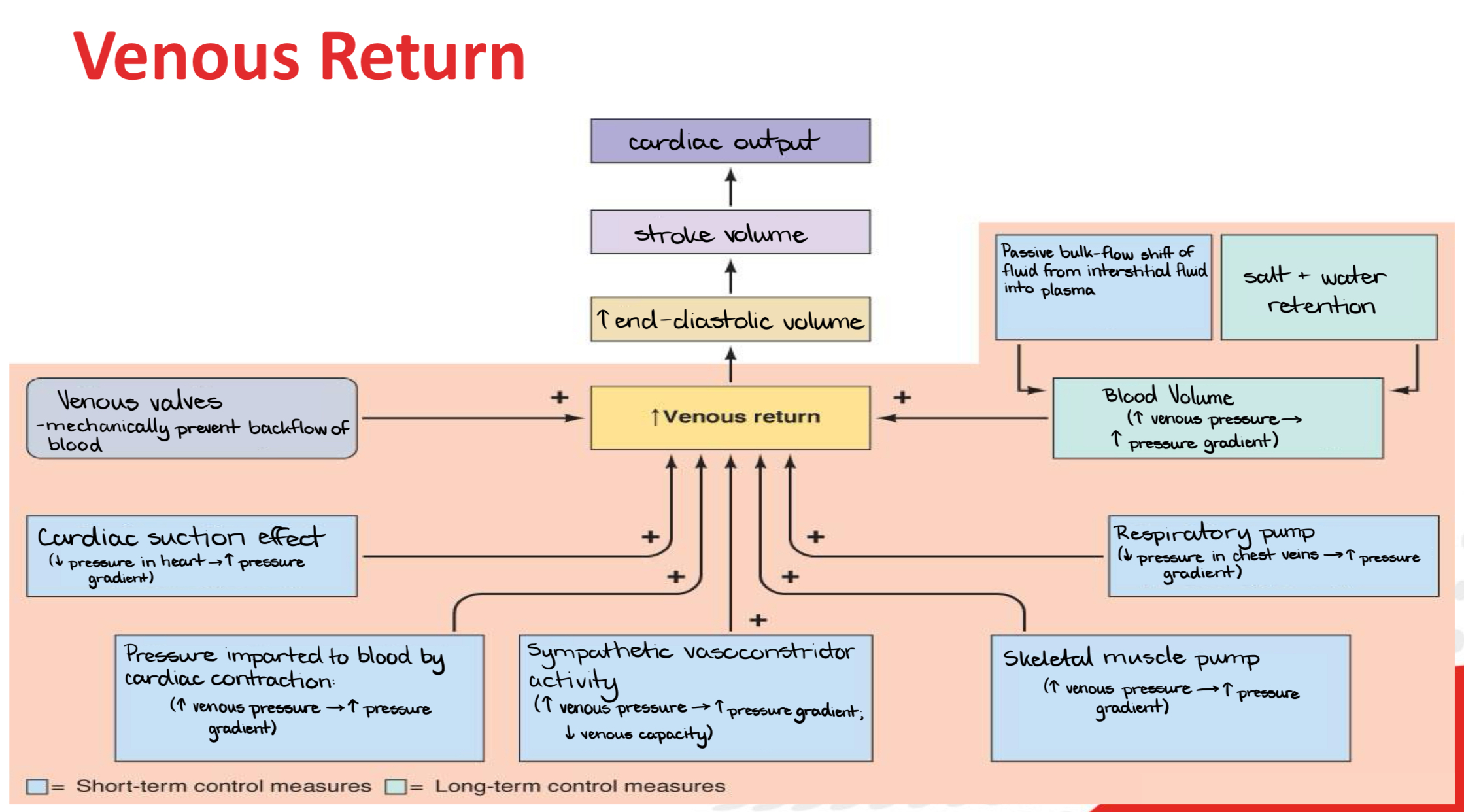
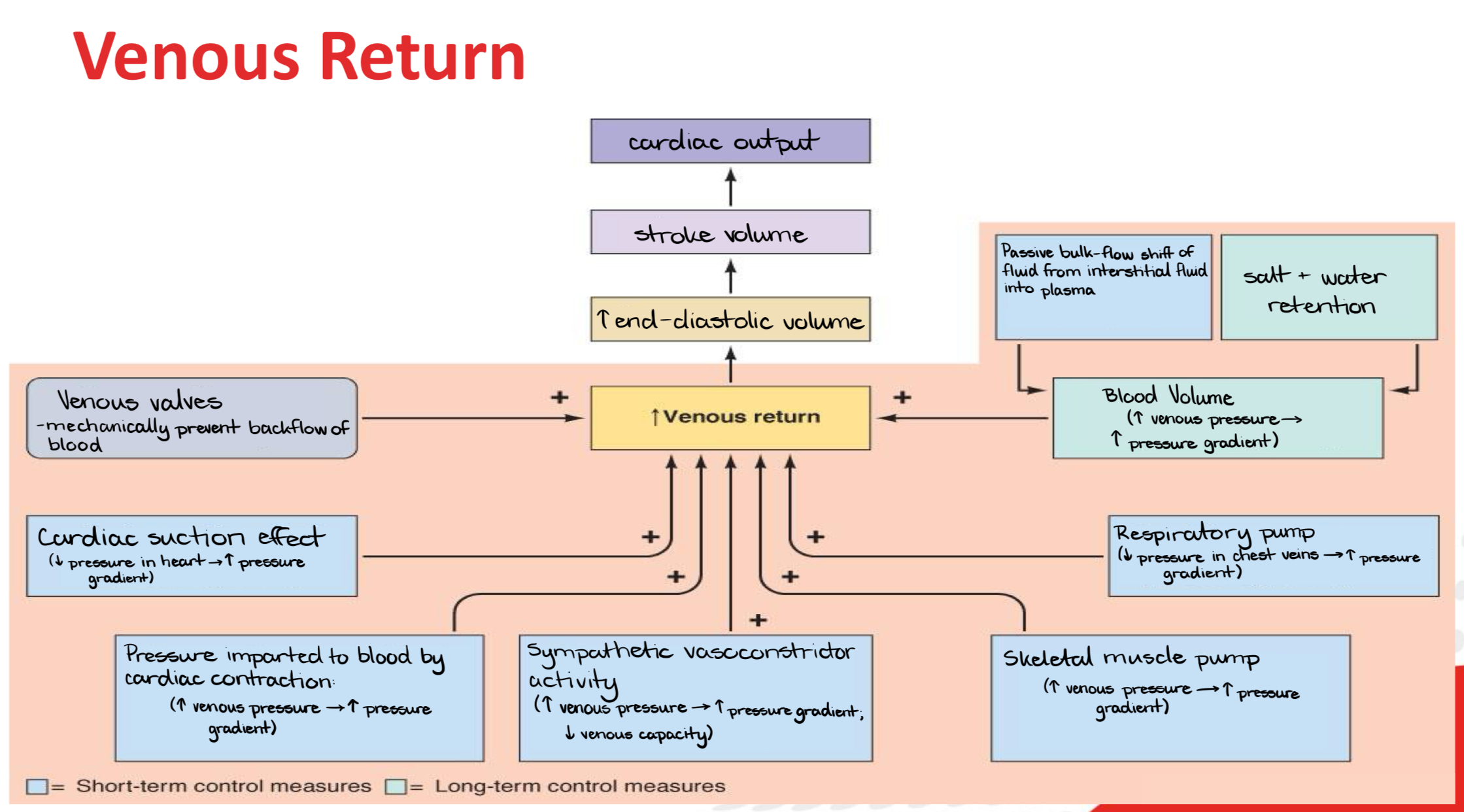
Go through this flowchart.
______________ are specialized stretch receptors located primarily in the aorta and carotid sinuses that send impulses to the _________________ in the medulla oblongata to regulate blood pressure.
baroreceptors, cardiovascular center
If blood pressure falls, stretch receptors __________ their firing rates which initiates the ____________ to accelerate HR, ___________ force of contraction and promote vasoconstriction.
decrease, sympathetic reflexes, increase
If blood pressure rises, stretch receptors __________ their firing rates which initiates the _______________ to decelerate HR, ___________ force of contraction, promote vasodilation.
increase, parasympathetic reflexes, decrease
The chemoreceptors respond to increasing CO2 and H+ (more acidic) levels by _____________ and ______________ peripheral vessels, which ______________ blood return to lungs so that CO2 can be exhaled.
increasing ventilation, constricting, increases
The chemoreceptors respond to decreasing CO2 and H+ levels by _____________ and ______________ peripheral vessels, which ______________ return to lungs.
decreasing ventilation, dilating, decreases
ADH (vasopressin) is produced in the ___________ and released from the ________________.
hypothalamus, posterior pituitary
What does ADH do?
signals the kidneys to reabsorb more water → decreases urine output
results in an increase in overall fluid levels + restores blood volume + pressure
What is the function of the renin-angiotensin system?
to raise blood pressure when it is too low by constricting blood vessels and increasing Na+/water retention
Explain the steps of the renin-angiotensin system.
low BP (low blood flow) → kidneys secrete renin → renin activates angiotensinogen (produced in liver) into → angiotensin I → converted to angiotensin II in the lungs (stimulates thirst in the hypothalamus) → angiotensin II causes vasoconstriction + increases aldosterone + ADH → increases water reabsorption → BP increases
Atrial natriuretic hormone (ANH) is secreted by cells in the _________ when blood volume is high enough to cause stretching of the _______ cells. What does ANH do?
atria, cardiac
promotes loss of Na+ and water from kidneys
suppresses renin, aldosterone + ADH production + release
decreases BP
What are autoregulation mechanisms?
self-regulatory mechanisms that don’t require specialized nervous system stimulation or endocrine control, allow each region of tissue to adjust its own blood flow + perfusion through chemical + physical alterations
What chemical signals control blood vessel dilation/constriction? How does the dilation/constriction occur?
dilation:
decreased O2
increased CO2
histamine release
these conditions stimulate endothelial cells to release NO which dilates blood vessels
constriction:
increased O2
decreased CO2
antihistamine release
these conditions stimulate endothelial cells to release endothelins which constrict blood vessels
What is ambrisentan?
a strong vasoconstrictor
What is the Bayliss effect?
myogenic response by which blood vessels regulate their own diameter in response to stretching of their walls (activation of Na+ and Ca2+ channels in the smooth layer)
high pressure → more stretch → vessels constrict to prevent flooding
low pressure → less stretch → vessels dilate to maintain flow
____________ and _____________ are the short-term controls for BP, ____________ is the long-term control for BP.
Baroreceptors, cardiovascular system, renal/blood volumes
The Valsalva maneuver is _____________ against a closed glottis. Performing it causes an __________ in intrathoracic pressure, leading to a reduction in ___________ to the heart.
forced expiration, increase, preload
What is phase I of the Valsalva maneuver?
onset of strain, rise in BP because of the emptying of some blood from the large veins + pulmonary circulation (not breathing)
What is phase II of the Valsalva maneuver?
positive intrathoracic pressure leads to a reduced venous return to the heart → reduced stroke volume → fall in BP → baroreceptors activated → sympathetic system triggered → tachycardia → increased CO2 → vasoconstriction → recovery of BP to normal values (not breathing)
What is phase III of the Valsalva maneuver?
release of strain which leads to a sudden dip in BP → release of positive pressure leads to expansion of pulmonary vascular bed + reduces left ventricular CSA → fall in BP
What is phase IV of the Valsalva maneuver?
overshoot of BP above the baseline because of resumed normal venous return to the heart stimulated by sympathetic nervous system in phase II — overshoot of BP leads to baroreflex stimulation → bradycardia → return to baseline BP