Salivary Gland Disorders
1/113
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
114 Terms
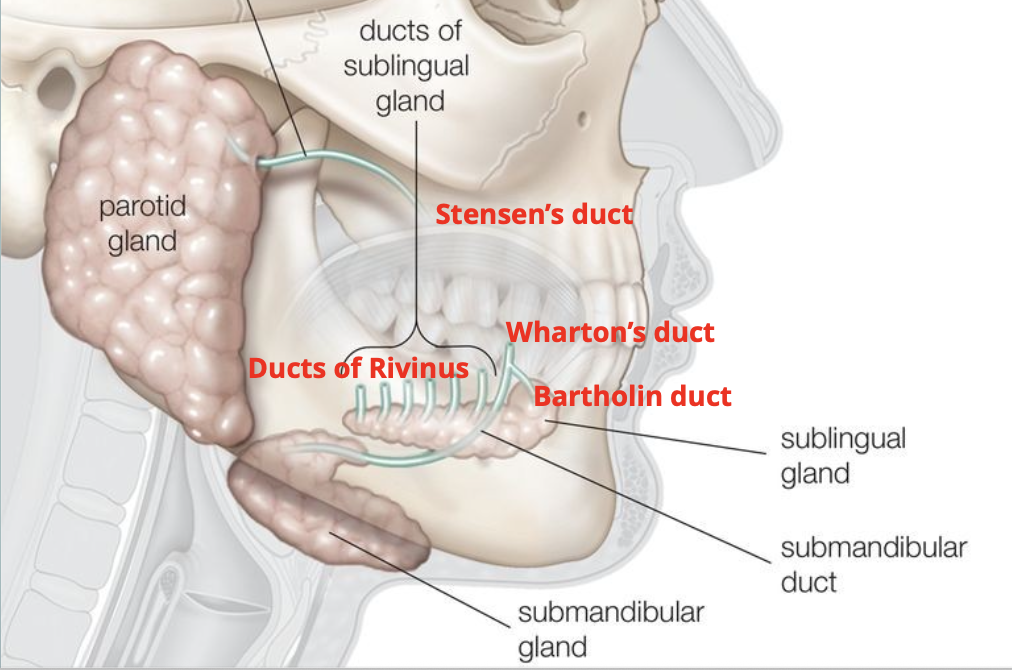
Name the major salivary glands
Parotid
Submandibular
Sublingual
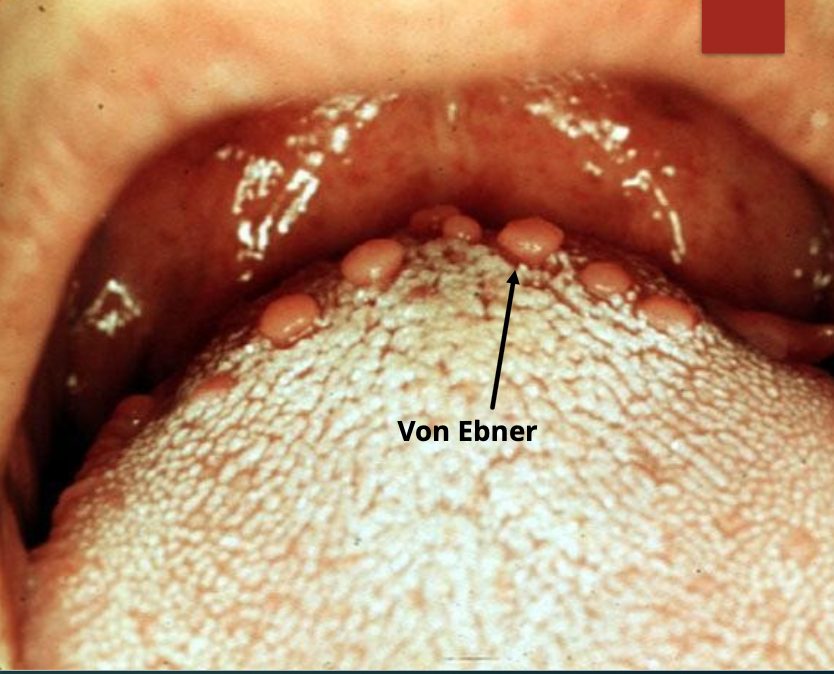
Name the minor salivary glands
Labial
Palatal
Buccal
Lip
Tongue (von Ebner)

What is a mucocele?
A common cause of oral mucosal swelling caused by rupture of salivary gland duct —> spillage of mucin

In what demographic would you find a mucocele?
All ages but especially children, young adults

What is the cause of a mucocele? What does it look like?
Due to trauma, appears as a dome-shaped mucosal swelling and has a bluish, translucent hue, it is fluctuant

Where might you find a mucocele? What are the clinical symptoms?
Occur anywhere, but mostly lower lip (80%), many patients report history of swelling, rupture, and recurrent swelling

If you have a mucocele on the floor of the mouth, what is it called?
Ranula

If you have a mucocele on the ventral tongue, what is it called?
Blandin-Nuhn

What is the treatment for a mucocele?
Surgical excision of lesion + minor salivary glands
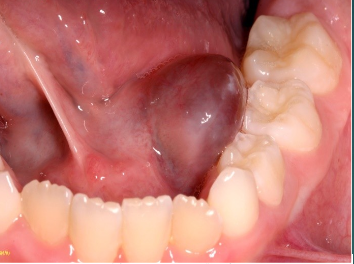
What is a ranula?
A mucus-filled cyst that occurs in the floor of the mouth, originating from the sublingual gland

Where is a ranula typically located?
In the floor of the mouth, lateral to the midline

What salivary gland is associated with a ranula?
Sublingual gland

What triggers the size increase of a ranula?
It increases just before and during meals

What is a plunging ranula?
Mucin dissects through the mylohyoid muscle, causing neck swelling
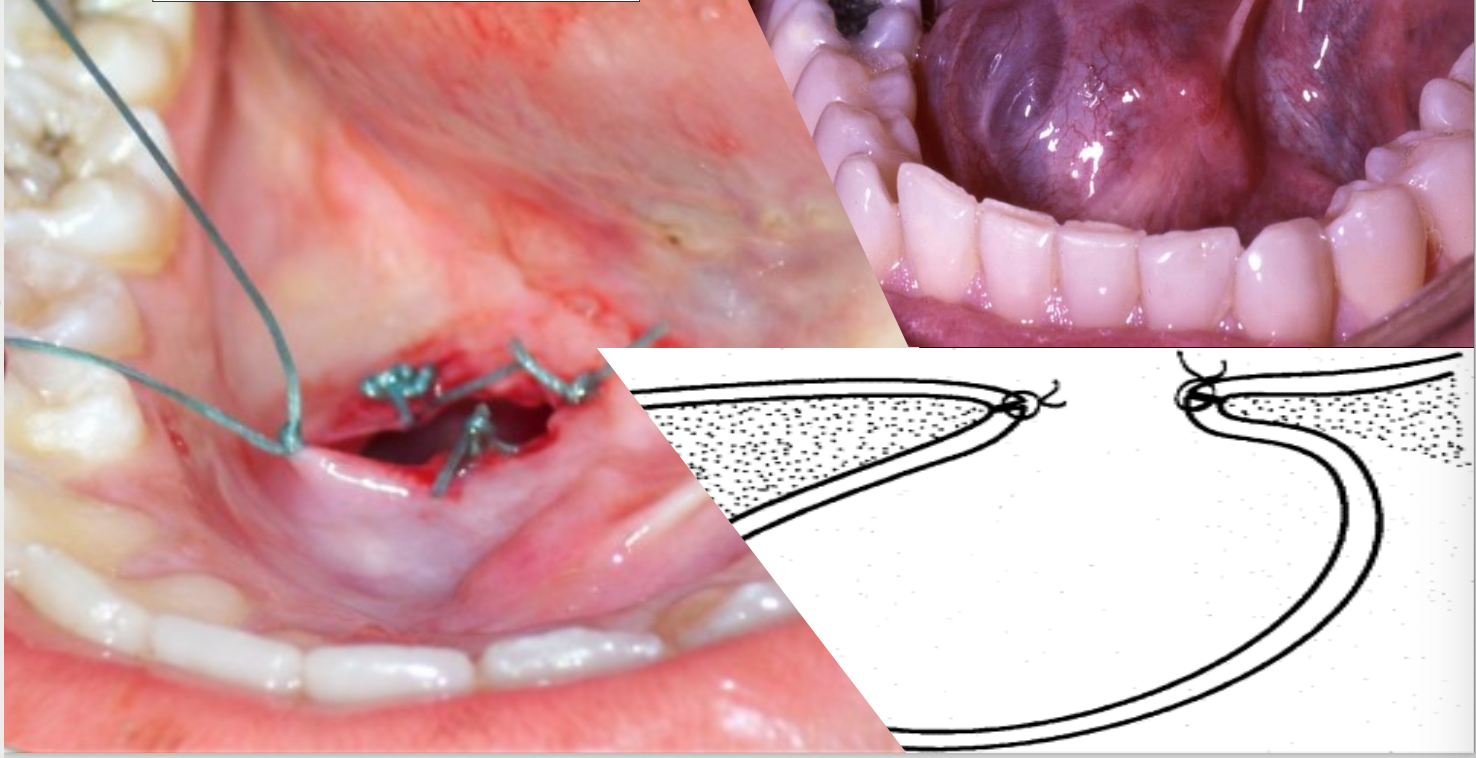
What is the treatment for a ranula?
Removal of the sublingual gland through surgery or marsupialization
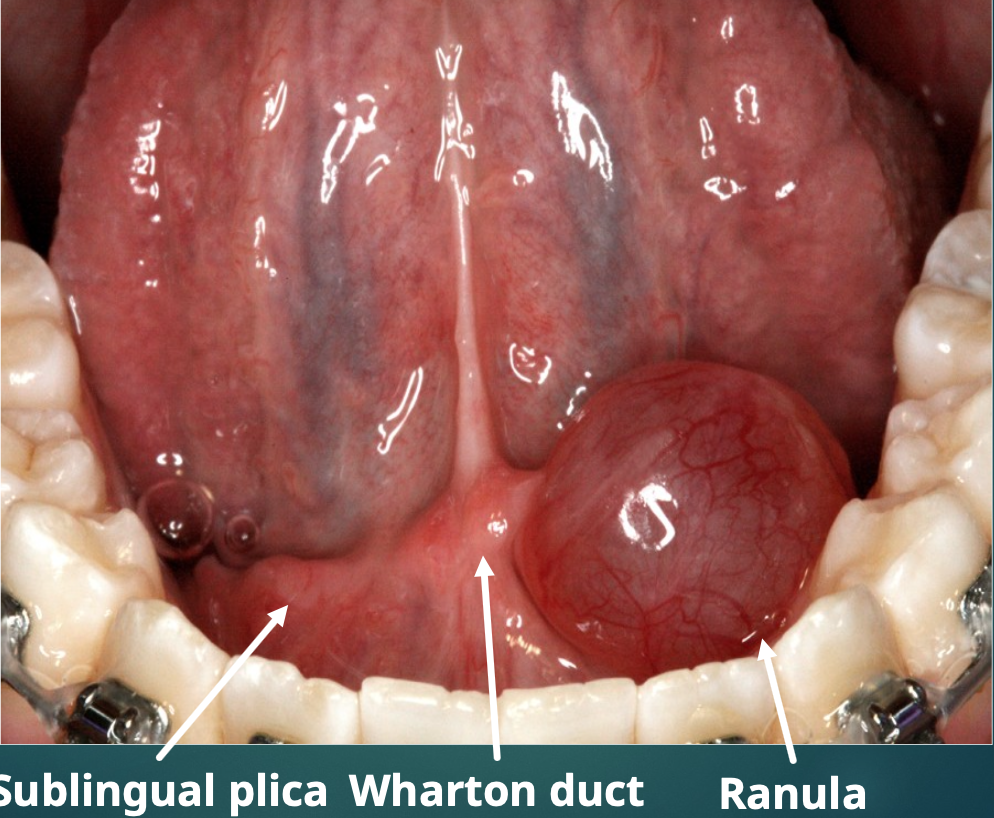
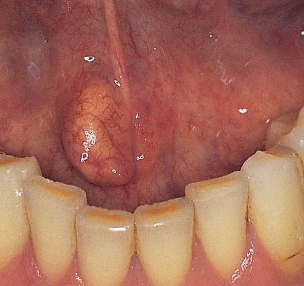
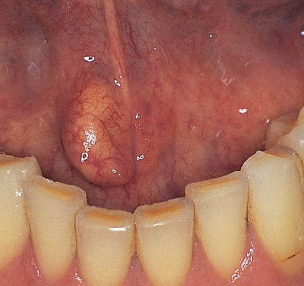
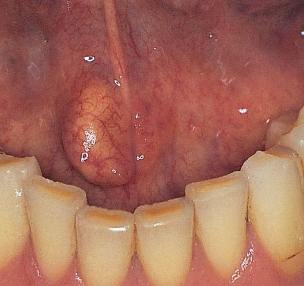
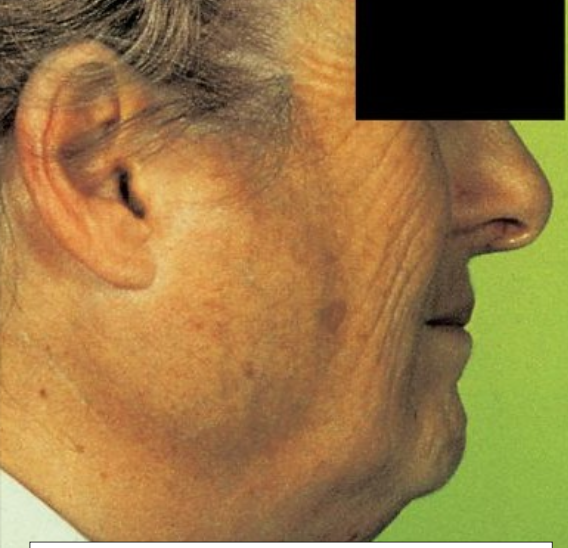
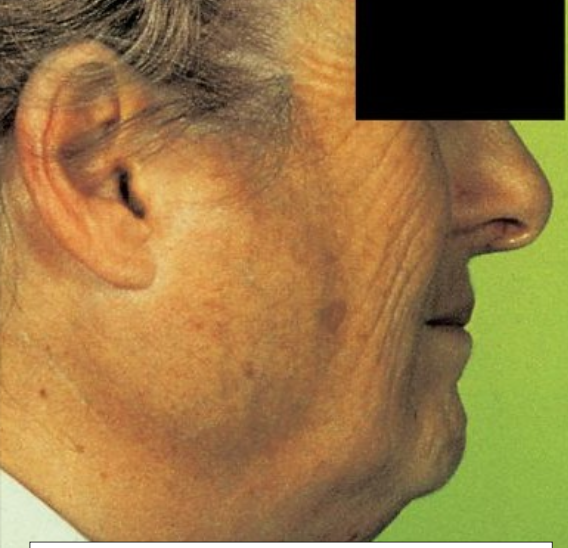
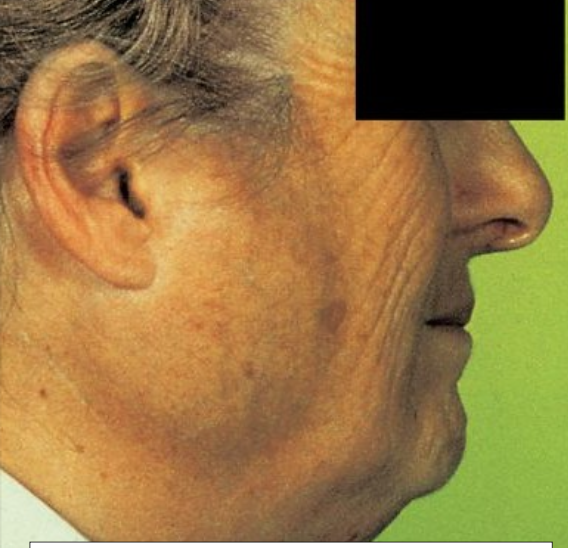
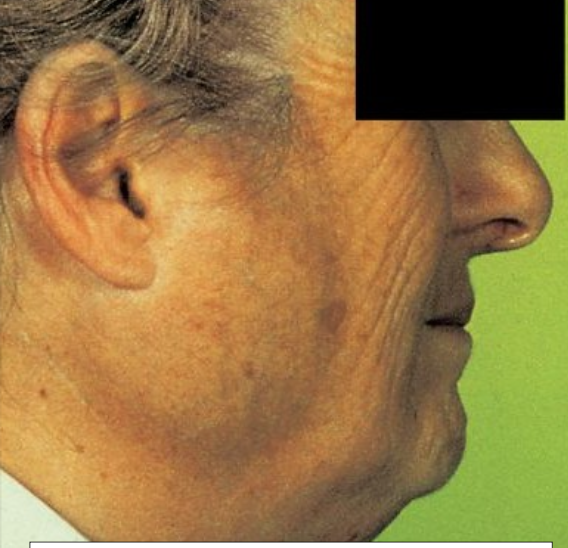
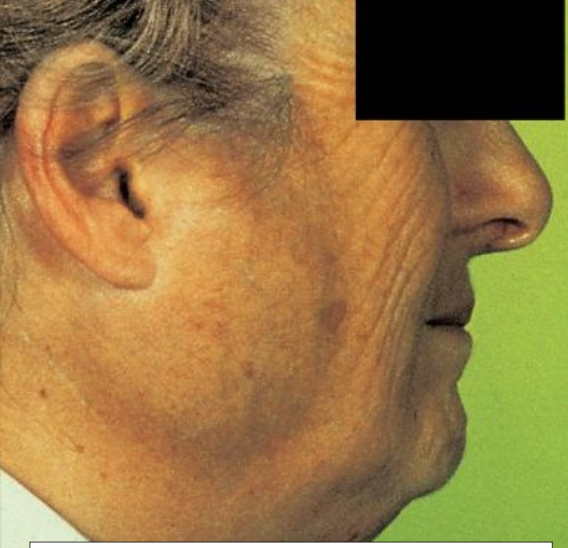
What is this?
Ranula

What is another name for salivary duct cyst?
Mucus retention cyst
What is a salivary duct cyst?
An epithelium-lined cavity that arises from the salivary gland tissue (TRUE CYST) vs. mucocele

In which population is a salivary duct cyst more common in?
Adults
Where might you find a salivary duct cyst?
It can occur in minor or major gland (more common on upper lip vs. mucocele)
What is the treatment for a mucus retention cyst?
Conservative excision
What is a major difference between a mucocele and a salivary duct cyst?
A mucocele lacks an epithelial lining

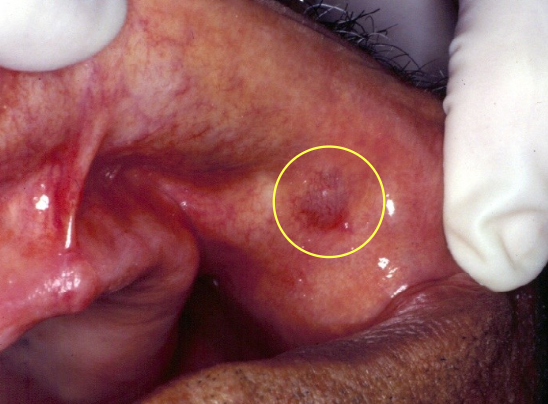
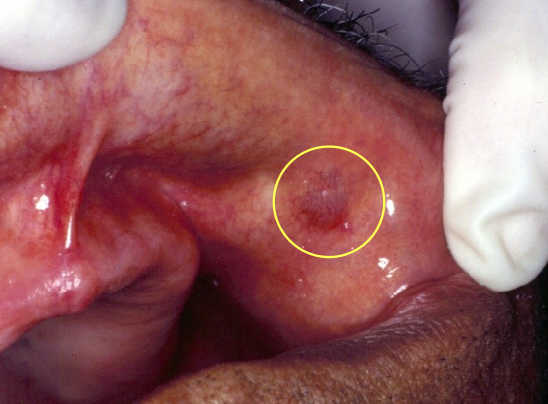
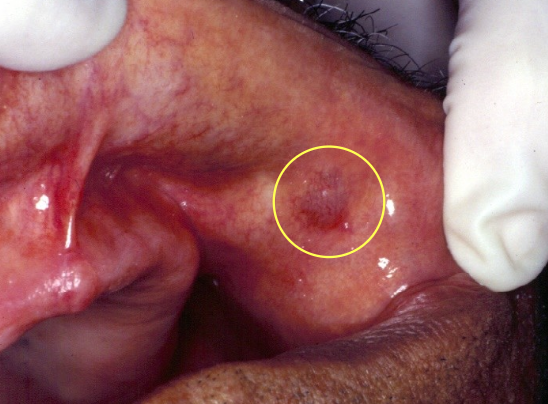
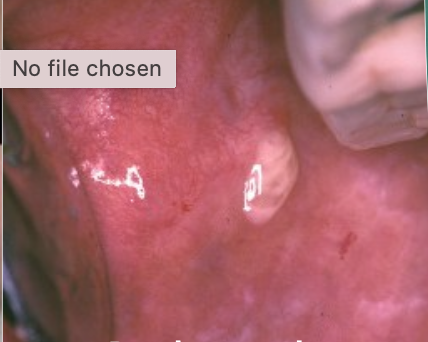
What is this?
A mucocele- most common location is lower lip, due to trauma, usually in kids

What is this?
Ranula- Floor of mouth from sublingual gland

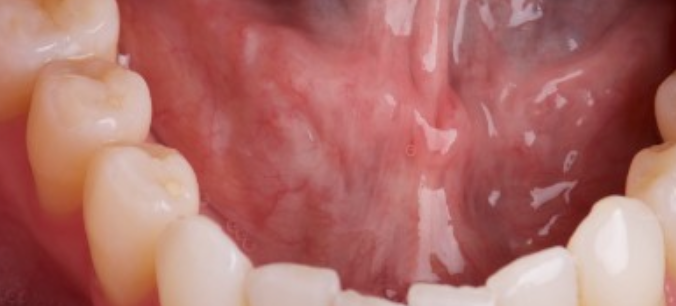
What is this?
Salivary duct cyst- usually in adults, more common in upper lip

What is cheilitis glandularis?
A rare inflammatory condition of the minor glands

What is the cause of cheilitis glandularis? Where might you find it?
Unknown; lower lip

What are the clinical features of cheilitis glandularis?
Openings of the ducts are inflamed and dilated; it is commonly associated with actinic cheilosis

What is the treatment for cheilitis glandularis?
Vermilionectomy (lip shave)

What is necrotizing sialometaplasia?
An uncommon, locally destructive inflammatory condition of the salivary gland

What causes necrotizing sialometaplasia?
Ischemia that leads to infarction (death) of salivary glands

Where does necrotizing sialometaplasia most commonly occur?
Hard palate

What are the clinical stages of necrotizing sialometaplasia?
Begins as painful, non-ulcerated swelling
After 2–3 weeks, tissue sloughs out and becomes a painless ulcer

Why is biopsy typically performed in suspected necrotizing sialometaplasia?
Because it mimics malignancy

How long does necrotizing sialometaplasia take to resolve?
Resolves within 6-10 weeks

What is the cause of nicotine stomatitis?
From repeated contact with pipe and cigar

Is nicotine stomatitis considered a precancerous lesion?
No, it is not a precancer

What does nicotine stomatitis look like clinically?
Inflamed salivary glands: Elevated “volcano-like” papules with red central dots

How long does nicotine stomatitis take to develop?
It takes years to develop
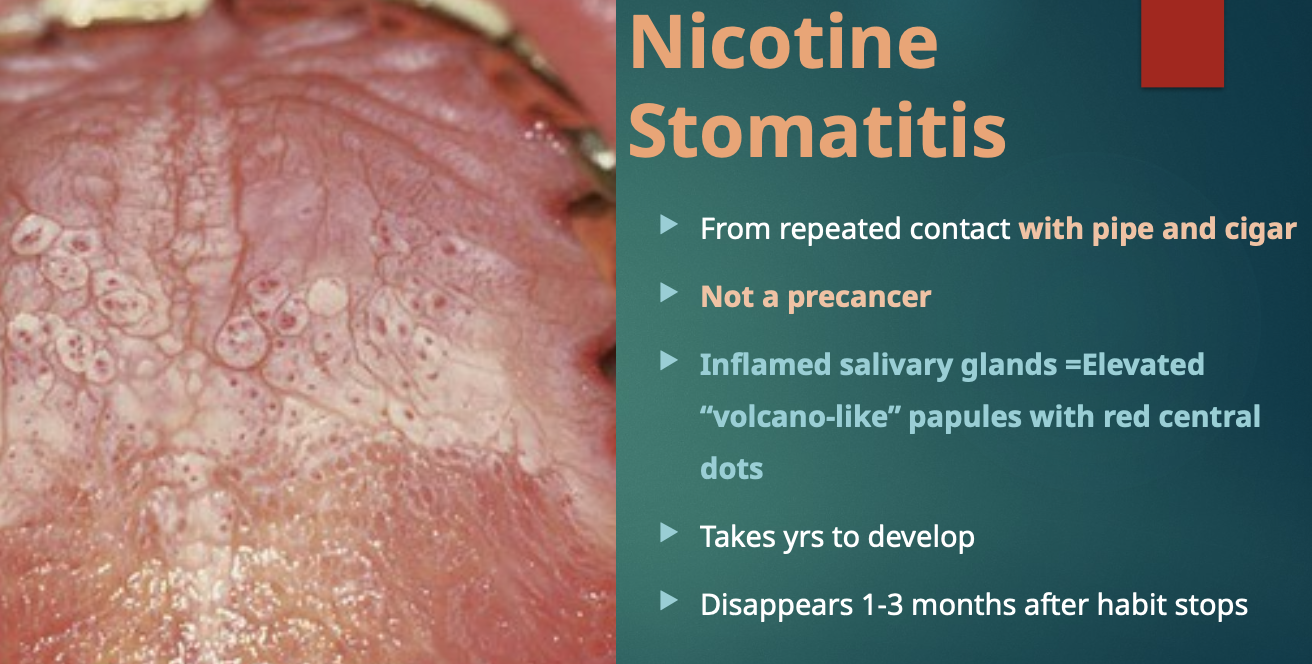
What happens to nicotine stomatitis after the smoking habit stops?
It disappears within 1–3 months

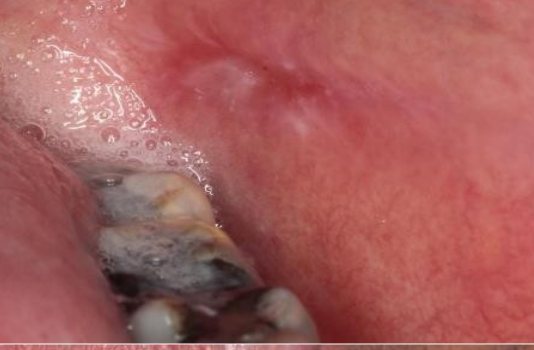
What are sialolithiasis?
Calcified structures that develop within the salivary ductal system; appear as radiopaque
What is the most common major gland involved in sialolithiasis?
Submandibular gland
What is the clinical presentation of sialolithiasis?
Swelling or episodic pain during chewing

What is the best way for one to see sialolithiasis?
Submandibular is best seen with an occlusal x-ray
What is the treatment of sialolithiasis?
Remove surgically, gentle massage to “milk” saliva toward orifice, moist heat, increase fluid intake to “flush”, sialogogues (medications which stimulate saliva, sour sugarless candies
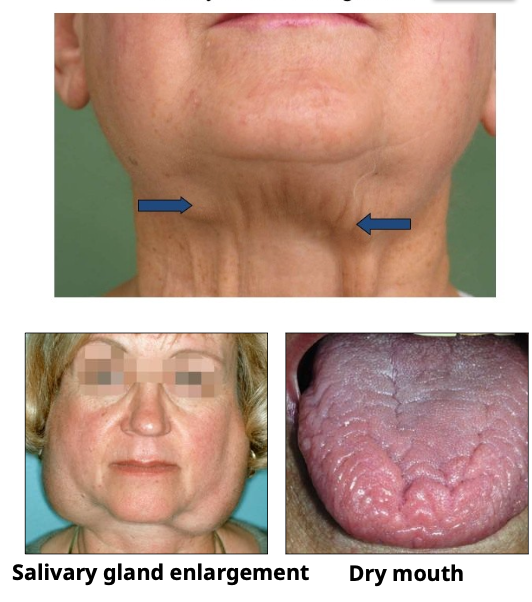
What is sialadenosis?
Enlargement of salivary gland due to a non-infectious cause
Which salivary gland is most commonly affected by sialadenosis?
The bilateral parotid glands
What are possible causes of sialadenosis?
Sialolith (stone)
Systemic conditions:
Diabetes
Malnutrition
Alcoholism
Bulimia
Sjögren syndrome
Recent surgery (aka surgical mumps)
What are "surgical mumps"?
May arise because the patient has been kept without food or drinks (NPO) and has received atropine during surgery
How effective is treatment for sialadenosis?
Unsatisfactory, fair to poor

What is sialadenitis?
Acute or chronic inflammation of the salivary glands
What do you see in acute sialadenitis?
Purulent discharge

What salivary gland is affected by sialadenitis?
Mainly submandibular gland

What is the cause of sialadenitis?
Infection such as bacterial or mumps

What is the treatment for sialadenitis?
ABx if infection, or rehydration, surgery, massage, or heat

What is lymphoepithelial sialadenitis (LESA)?
An autoimmune condition with mainly parotid and lacrimal gland involvement

Which glands are primarily affected in LESA?
Parotid and lacrimal gland

What syndrome is LESA often associated with?
Sjögren syndrome (can be isolated or associated with it)

What are the clinical features of LESA?
Female predilection
Middle-aged or older
Unilateral or bilateral firm, non-tender parotid swelling

Why might the course of LESA not be benign?
Because the infiltrate may be monoclonal, possibly representing low-grade lymphoma in situ

What are possible treatment options for LESA?
Do nothing
Low-dose radiation

What is sialorrhea?
Excessive saliva production

Is sialorrhea a common condition?
No, it is uncommon

What are some causes of sialorrhea?
Local irritations (e.g., aphthous ulcers, ill-fitting dentures)
Rabies or heavy-metal poisoning
Medications (like clozapine)
Poor neuromuscular control

What is the treatment for sialorrhea?
Surgical
Botulinum toxin A (botox)
Anticholinergics (atropine ophthalmic drops)

What drug is a cholinergic agonist that stimulates saliva and is used for xerostomia?
Pilocarpine

What is xerostomia?
Extreme dry mouth that affects 25% of older adults

What are some causes of xerostomia?
Salivary gland hypofunction (Sjögren syndrome)
Medication
Radiation
Sjögren syndrome
What are some clinical features of xerostomia?
Ropey, thick, or foamy saliva
Dorsal tongue is often fissured with atrophy of the filiform papilla

What are some medications that cause xerostomia?
Antihistamine
Anticholinergic
Antidepressants
Sedatives and anxiolytic agents
Antihypertensive agents
List some side effects of xerostomia
Frothy saliva
Infection such as candidiasis
Ulcers
Rampant cervical caries
Halitosis or malodor
Normal saliva
Frothy saliva
Loss of papilla seen in xerostomia

Erythematous candida seen in xerostomia


Ulcer from no saliva
Pseudomembranous candida

Rampant cervical caries

What are some treatments for xerostomia?
Good hydration/frequent sips of water
Artificial saliva
Sialogogues, sugar-free lemon drops
Salagen (pilocarpine) or evoxac (cevimeline)
1% neutral sodium fluoride gel or toothpaste nightly
Antifungal therapy as needed
More frequent dental recall
What is Sjogren syndrome?
Autoimmune condition causing a decrease in saliva and tears; cause is unknown
What is exophthalmia?
Decreased lacrimal flow results in dry eyes
What is keratoconjunctivitis sicca?
Damage to the eyes
What is primary sjogren?
Salivary and lacrimal gland involvement without the presence of another autoimmune disease (xerostomia + keratoconjunctivitis sicca)
What is secondary sjogren?
Another autoimmune disease accompanies salivary and lacrimal gland involvement (50%)
What is the gender predilection and age range for Sjogren Syndrome?
Females > males (9:1), usually middle-aged to older adults
Which glands are primarily affected in Sjogren Syndrome?
Salivary and lacrimal glands
What are the clinical features of Sjogren Syndrome?
Bilateral parotid gland swelling (in ~50%)
Xerostomia (dry mouth)
Exophthalmia (dry eyes)
Burning tongue
Risk of dental caries, candidiasis, and periodontal disease
What serious malignancy is associated with Sjogren Syndrome?
Non-Hodgkin B-cell lymphoma (MALT lymphoma)
What tests help diagnose Sjogren Syndrome?
Biopsy of salivary gland
Positive RF (Rheumatoid Factor) in ~60%
Anti-nuclear autoantibodies (ANAs) in ~80%
Sialogram (imaging of salivary ducts)
What eye test was historically used for Sjogren Syndrome but is now outdated?
Schirmer test

What is another name for frey syndrome?
Auriculotemporal Syndrome
Gustatory sweating and flushing

What is frey syndrome?
Facial flushing and sweating along the distribution of the auriculotemporal nerve during mastication

What is the cause of frey syndrome?
Damage to the nerve by
Parotid surgery
Forceps delivery
Diabetes with neuropathy

What are mumps (epidemic parotitis)?
A viral infection; paramyxovirus of the salivary glands

In which demographic do you see mumps in?
Mostly children

What is the treatment and recovery for mumps?
No treatment; recovery is about 3-10 days
Which of the following is FALSE?
Ranula affects the submandibular gland
Cheilitis glandularis is most commonly located on the
Lower lip
Which of the following is TRUE?
Sialolithisos are salivary gland stones
Which of the following is FALSE?
Nicotine stomatitis is premalignant