Mechanical Ventilation Papers
1/106
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
107 Terms
Ambrosio and Fantoni, 2024
Editorial: Mechanical ventilation in anesthesia and critical care animal patients, volume II
Horses undergoing general anesthesia often present complications related to the position in which they are lying on the operating table
Complications are related to difficulties in gas exchange due to a decrease in the ventilation/perfusion ratio, pulmonary atelectasis, and a drop in blood pressure
In dorsal recumbency, the lungs receive compression from the diaphragm produced by compression of the abdominal viscera
In lateral recumbency the upper lung compresses the mediastinum and consequently the lower lung
Monitoring during alveolar recruitment maneuvers (ARMs) can only be done through electrical impedance tomography, respiratory mechanics, or arterial oxygenation through blood gas analysis in horses
Sacks et al
Comparing the ventilation distribution measured by electrical impedance tomography (EIT) in foals under diazepam sedation, postural changes, and continuous positive airway pressure (CPAP)
In healthy foals, diazepam administration did not alter the distribution of ventilation or minute ventilation and the lateral recumbency results in the collapse of dependent lung areas
CPAP use in dorsal recumbency foals increases pulmonary pressures and improves ventilation in dependent regions, suggesting improvement of ventilation-perfusion mismatch
Brandly et al
Studied flow-controlled expiration technique (FLEX) during anesthesia to reduce PEEP requirement in dorsally recumbent horses
FLEX ventilation was associated with a lower PEEP requirement due to a more homogenous lung ventilation distribution during expiration
Lower PEEP requirement led to more stable and improved cardiovascular conditions in horses ventilated with FLEX
Conclusion: Performing recruitment maneuvers and subsequent administration of PEEP to keep the alveoli open is an essential technique for reversing hypoxemia in horses and dogs during anesthesia or ICU. Also demonstrated the importance of monitoring these to avoid lung injuries and hemodynamic dysfunctions
Open Lung Approach
Ventilatory strategy complementary to the protective ventilation notion that aims to reduce atelectrauma and shear stress by performing recruitment maneuvers and subsequently using higher PEEP, thereby maintaining the lung open
Refractory Hypoxemia
The presence of inadequate oxygenation despite normal levels of inspired oxygen
PaO2 < 60 mmHg or a PaO2/FiO2 ratio below 100 mmHg on a FiO2 or 0.8-1.0 with a positive end expiratory (PEEP) of at least 10-30 cmH2O
Physiologic Mechanisms of Decreasing Atelectasis
In a spontaneously breathing patient, more pronounced diaphragmatic contractions in the dorsal region as well as sigh breaths optimize alveolar recruitment, maintain pulmonary compliance, and decrease formation of atelectasis
Induction of general anesthesia abolishes these physiological mechanisms
Appears to be one of the main mechanisms of acute lung injury, is a major cause of postoperative hypoxemia, and is associated with a prolonged ICU and hospital stay in people
Intraoperative Effects of Atelectasis
Increased alveolar-arterial oxygen gradient, increased pulmonary shunting, and decreased oxygen saturation
Three Distinct Lung Regions Identified During Positive Pressure Ventilation
During positive pressure ventilation, three distinct lung regions can be distinguished because the pressure required to open the alveoli, called the threshold opening pressure, varies along the gravity axis
Lower portion of the lungs = dependent portion - the weight of mediastinal structures increases pleural pressure (making it less negative) and thus reduces alveolar volume
Smaller alveolar volumes mean that the alveoli have more potential for distension, but are less compliant, and therefore able to exchange less oxygen
Upper, non-dependent part of the lungs - includes regions that remain inflated throughout tidal ventilation and can be overinflated by tidal volumes >6 ml/kg and plateau pressures exceeding 30-32 cmH2O
Higher PO2 and ventilates more efficiently due to higher compliance, smaller volumes are exchanged in case of overdistension
Positive Pressure Insufflation in an Acutely Injured Lung
Creates a risk of overdistension of healthy alveoli and shear stresses at the junction between the ventilated and non-ventilated areas, and causes inflammation and epithelial damage in the small airways and alveoli repeatedly mobilized
What are the two main components of VILI?
Atelectrauma
Overdistension
Protective Mechanical Ventilation
Recommends the use of low tidal volumes (4-8 ml/kg of predicted body weight) and low plateau pressures (up to 30-32 cmH2O) to reduce alveolar stretch injury associated with repetitive opening and closing of atelectatic alveoli and tidal overdistension
Lung Recruitment Maneuver
Dynamic and transient increase in transpulmonary pressure that aims to reverse lung collapse, improve lung compliance, increase end-expiratory lung volume, and improve gas exchange
Anatomic Recruitment vs Functional Recruitment
Anatomic recruitment often does not coincide with functional recruitment
In some cases, increasing the inspiratory pressure could worsen the intrapulmonary shunting by increasing perfusion of collapsed lung areas without improving ventilation
The recruitment maneuver may prove ineffective when the applied pressure is insufficient or because the sufficient pressure is excessive
Anatomic and functional lung recruitment can only coincide if restoration of ventilation of the lung units occurs without alteration of perfusion of those same units
Anatomic Recruitment
The restoration of aeration as assessed by computed tomograpy
Functional Recruitment
THe improvement of gas exchange
Recruitability
Mainly explained by the distribution of lung lesions, their nature, as well as the timing of onset
Lung morphology (focal or non-focal) rather than the origin of lung disease (pulmonary or extra-pulmonary) may explain the considerable variability in and among patients with ARDS
In focal ARDS, recruitment maneuvers might expose the patient to overdistension of already open lung regions, but may be beneficial in non-focal ARDS with more collapsed tissue and a potential higher oxygenation benefit
The predominant lesion type could also play a role in the response to recruitment maneuvers
Patients with a better oxygenation response to recruitment maneuvers have been shown to have predominantly interstitial edema and compressive and congestive atelectasis
Subjects with minimal oxygenation response had complete alveolar filling with purulent or hemorrhagic material and consolidation which are more prominent in direct lung injuries such as pneumonia
The timing of the recruitment maneuver relative to the onset of ARDS influences recruitability
A change from an exudative to a fibroproliferative process in late ARDS may later the response to recruitment maneuvers
Unlikely that these maneuvers will be beneficial in patients with ARDS of more than 3-5 days who do not have altered chest wall mechanics
Sighs
First reported recruitment maneuver
Consists of the application of a high tidal volume to mimic physiologic breathing as it occurs in healthy subjects
Efficacy is limited over time and could increase the level of inflammatory markers in the lungs depending on the frequency and volumes applied
Sustained Inflation
Most studied method
Involves use of continuous positive airway pressure of 30-60 cmH2O for up to 60s in sedated and paralyzed patients, while monitoring them for possible adverse effects
Due to uncertainty of benefits and related hemodynamic complications, the routine use of sustained inflations as recruitment maneuvers is no longer recommended
When does the majority of recruitment occur?
Within the first 10s of the recruitment maneuver
Hemodynamic impairment becomes significant after 10 s of initiation
Maximum Recruitment Strategy
Consists of 2 min stepwise increases in PEEP of 5-10 cmH2O with a constant driving pressure (10-15 cmH2O) until a combined value of oxygen and carbon dioxide partial pressures (PaO2 + PaCO2) above 400 mmHg is achieved
PEEP Before and After Recruitment Maneuvers
PEEP higher than that used before the recruitment maneuver (6-7 cmH2O above baseline) is necessary in order to keep the alveoli open and preserve the beneficial effects on oxygenation over time
CT to Assess the Effects of Recruitment Maneuvers
CT is the gold standard for assessing pulmonary reaeration
Recruitment is quantified as the amount of un-aerted tissue at a given pressure that re-inflates at higher pressures and is usually expressed as a percentage of total lung volume
Recruitable areas in patients with moderate to severe ARDS have been estimated at 13% of total lung weight with a strong correlation to the severity of lung injury
A non-focal morphology of ARDS evaluated by CT-scan has been shown predictive of high pulmonary reaeration after recruitment maneuvers
Only measures the anatomical recruitment of tissues
Main Disadvantages Associated with CT for Assessing the Effects of Recruitment Maneuvers
Time consuming, exposes the patient repeatedly to radiation, and cannot be performed at the bedside
Pressure-Volume Curve for Assessing the Effects of Recruitment Maneuvers
A verticalization of the pressure-volume curve after implementation of a higher PEEP implies gas recruitment, thus allowing confirmation (or rejection) of the effectiveness of recruitment maneuvers
Compliance might be more related to the improvement or deterioration of already ventilated lung units than the actual recruitment of atelectatic lung units
Electrical Impedance Tomography for Assessment of Effects of Recruitment Maneuvers
Electrical impedance tomography is a real-time radiation free, non-invasive bedside technique that provides cross-sectional images of the distribution of electrical conductivity within the body
Can estimate the percentage of recruitable collapsed alveoli by measuring relative changes in pixel compliance (total impedance change for that pixel divided by the airway pressure)
Decreasing pixel compliance with reduced PEEP indicates alveolar collapse, whereas declining pixel compliance with increasing PEEP indicates local overdistension
Predominant ventilation in non-dependent areas could predict greater lung re-aeration after a recruitment maneuver
This technique does not provide information about aerated lung tissue like CT-scan but it does provide data about changes in lung volumes associated with a change in ventilator parameters
Disadvantages of Electrical Impedance Tomography for Assessment of Effects of Recruitment Maneuvers
Images created have low spatial resolution compared with CT-scan and magnetic resonance imaging, which limits the ability to provide morphologic information
Electrical impedance tomography is useful for monitoring lung function over time in a single patient, it may not be suitable for interindividual comparisons
Need for optimal and stable skin-to-electrode contact over time to avoid artifacts during data collection is a challenge, particularly in thick-coated patients
Pleural effusion and adjacent cardiac structures can cause paradoxical ‘out of phase’ impedance changes in the surrounding lung tissues due to an overshoot phenomenon introduced by the reconstruction algorithm
Lung Ultrasound for Monitoring the Effects of Recruitment Maneuvers
Observation of anteriorly localized consolidation and crater-like subpleural consolidation predicts a positive response to recruitment maneuvers (i.e. lung recruitability) in patients with ARDS and a highly significant correlation has been found between PEEP-induced lung recruitment, as measured by pressure-volume curves, and the ultrasound aeration score
Four-step algorithm proposed in humans using lung ultrasound to guide recruitment maneuvers in practice
Presence of alveolar collapse is assessed by the identification of simultaneous coalescing B-lines and lung consolidation as well as a high aeration score
If present, a recruitment maneuver is indicated
Hemodynamic status is assessed by various methods using ultrasound
Can include the caudal vena cava collapsibility index, the transmitral E-wave velocity, the end-diastolic left ventricular internal diameter normalized to body weight, or the presence of the papillary muscle kissing sign as demonstrated in dogs
Preload dependence, hypovolemia, vasoplegia, and impaired myocardial contractility are considered contraindication to the maneuver
Detection of the lung opening pressure during the pressure increase of the recruitment maneuver and of the closing pressure during subsequent PEEP titration is performed
Ultrasound probe is positioned in the most dependent region of the atelectatic lung to monitor loss of consolidation pattern
Subsequent evaluation of the contralateral lung is then performed to validate the resolution of consolidation, and the airway pressure at that time is identified as the opening pressure
Reverse logic applies during decremental PEEP titration, allowing identification of the closing pressure, and thus the ideal PEEP
Adjustment of hemodynamic therapies is performed to optimize the improvement of cardiopulmonary function
Disadvantages of Lung Ultrasound for Monitoring the Effects of Recruitment Maneuvers
May be difficult to perform reliably in obses patients or when subcutaneous emphysema is present
The role of lung ultrasound in assessing alveolar overdistension remains undetermined
Stress Index for Monitoring the Effects of Recruitment Maneuvers
Analyzes the shape of the dynamic pressure-time curve during volume-controlled ventilation with a constant inspiratory flow
A linear increase in pressure corresponds to a stress index equal to 1, suggesting tidal inflation of normally aerated alveoli without overdistension
Tidal recruitment is implied with a stress index <1 (downward concavity of the curve, i.e. compliance decreases during tidal inflation)
Mainly used to determine the optimal level of PEEP for a given patient
Limitations of Stress Index to Monitor the Effects of Recruitment Maneuvers
The lungs and chest wall are coupled in series so changes in the extrapulmonary environment can confound its interpretation, especially with ARDS because of the extreme variability in chest wall compliance associated with this condition and the frequent coexistence of pleural effusion
Recruitment-To-Inflation Ratio for Monitor the Effects of Recruitment Maneuvers
Recruitment-to-inflation ratio (R/I ratio) is a novel single breath maneuver that can be performed with any mechanical ventilator, developed to assess lung recruitment in patients with ARDS
Represents the proportion of volume distributed to the recruited lung to that into the baby lung when PEEP is changed
Can provide useful information for identifying both the risk of atelectrauma by setting a low PEEP in patients with a high R/I ratio and hyperinflation by setting a high PEEP in patients with a low R/I ratio
Reference cut-off must be individualized to the different models of ventilators
The R/I ratio provides a promising beside tool to characterize lung recruitability over a given range of PEEP, which can be used to customize this parameter
Hemodynamic Tolerance when Deciding to Perform a Recruitment Maneuver
Increased intrathoracic pressure during recruitment maneuvers transiently compromises hemodynamic function by decreasing right and left ventricular preload and increasing pulmonary vascular resistance and right ventricular afterload, resulting in decreased cardiac output and arterial blood pressure, and increased heart rate
Effect of Recruitment Maneuvers on Survival in Patients with ARDS
A significant reduction in 28 day mortality was found in association with the use of recruitment maneuvers
Recommendations for the Use of Recruitment Maneuvers in ARDS
Best to consider an individualized rather than systemic use of recruitment maneuvers in patients with ARDS
Alveolar recruitment is desirable first if it can be performed safely, which requires prior assessment of lung recruitability
As a general rule, and only in the setting of severe ARDS, performing recruitment maneuvers as rescue therapy should be reserved for a minority of patients with refractory hypoxemia demonstrating good lung recruitability
Appears to be specific situations in which recruitment maneuvers may be appropriate, such as in morbidly obese patients or cases of intraabdominal hypertension
Stepwise approach might be preferred to sustained inflation
If the recruitment maneuver is effective, sufficient PEEP is required to maintain recruitment
Finding the optimal PEEP after a recruitment maneuver is challenging and may depend on the regional distribution of lung lesions, characteristics of the atelectasis (congestive or consolidation) as well as the method used to recruit the lungs
To reduce derecruitment in the acute phase of ARDS, a minimum PEEP of 10-12 cmH2O should be implemented with conventional mechanical ventilation strategies, with values >20 cmH2O necessary in severe cases
When are recruitment maneuvers contraindicated?
In hemodynamically unstable patients (especially with right-sided heart failure), those with intracranial hypertension, pneumothorax or a predisposition to barotrauma
More generally in patients with focal lung pathology
Prone Positioning as a Rescue Therapy
In the supine position, the weight of the ventral lungs, mediastinal structures, and abdominal viscera increases the pleural pressure in the dorsal lungs, promoting alveolar collapse
Prone positioning changes the gravitational forces which promotes re-aeration of the now non-dependent dorsal lungs
Regional diaphragmatic movements homogenize global pulmonary ventilation, improve ventilation perfusion matching via anterior displacement of mediastinal structures, reduce the ventral-dorsal transpulmonary pressure difference, enhance mobilization of secretion, and thus reduce the likelihood of VILI compared with supine positioning
The newly opened dorsal lung regions, despite their non-dependent orientation, remain well perfused, decreasing pulmonary shunting
Some have suggested minimum 12-16 hour daily prone sessions with the head of the bed elevated 30-45* to limit head edema and gastroesophageal reflux
Other important aspects proposed for successful implementation of prone positioning include appropriate prior titration of PEEP, careful use of neuromuscular blocking agents and sedative drugs to avoid diaphragmatic paralysis, and discontinuation of prone positioning when sustained improvement of oxygenation is observed
Long term superiority to prone positioning remains unknown
Complications of Prone Positioning
Most complications related to prone positioning arise when the patient’s position is changed, including accidental removal of the endotracheal tube, drains, or catheters
Contraindications to Prone Positioning
Should not be implemented in patients in shock, or with unmonitored intracranial hypertension, severe traumatic injuries, or spinal instability
Neuromuscular Blockade as a Rescue Therapy
Used in hypoxemic patients with poor ventilator synchrony despite deep sedation
Improved synchrony may result in more uniform lung recruitment and improved compliance and gas exchange
Positive effects of neuromuscular blocking agents could also be related to a decrease in biotrauma
Disadvantages of Neuromuscular Blockade
Neuromuscular blockade-related progressive atelectasis due to loss of diaphragmatic tone with resulting hypoxemia and ICU-aquired weakness
Inhaled Pulmonary Vasodilators as a Rescue Therapy
Use of inhaled pulmonary vasodilators has two purposes
Aim to reverse the pulmonary hypoxic vasoconstriction that occurs naturally in healthy alveoli
Because increased pulmonary vascular resistance due to pulmonary vasoconstriction and atelectasis can lead to right-sided heart failure, inhaled pulmonary vasodilators indirectly support the right ventricular function
Inhaled pulmonary vasodilators theoretically act in well-ventilated lung units, helping to redirect blood flow away from poorly ventilated lung areas and improve V/Q mismatch
Advantages of the inhaled route include its selective delivery to well-ventilated lungs and ease of administration
Two classes of molecules have been used, inhaled nitric oxide and prostaglandins (mainly epoprostenol), both with short half-lives
Besides improving oxygenation, they reduce pulmonary vascular pressure and may be useful in patients with preexisiting pulmonary hypertension
Should be used with the understanding that severe rebound hypertension may happen if the medication is stopped too quickly
Routine use is not recommended
Adverse Effects of Inhaled Pulmonary Vasodilators
Nitric oxide has been associated with methemoglobinemia, kidney failure, inhibition of platelet activity, and hypotension
Also requires a specialized delivery system
Largely replaced by prostaglandins which are less expensive and easily administered via a nebulizer connected to the mechanical ventilation circuit and has fewer adverse effects
Extracorporeal Membrane Oxygenation as a Rescue Therapy
In individuals with profound hypoxemia or severe uncompensated hypercapnia with acidemia resistant to conventional low-volume, low-pressure ventilation, prone positioning and inhaled pulmonary vasodilators, venovenous extracorporeal membrane oxygenation allows for low-tidal volume protective ventilation combined with a lower FiO2, thereby limiting the main injury mechanisms associated with VILI
Tidal volume is also significantly reduced leading to a substantial reduction in plateau pressure without worsening derecruitment as PEEP is kept constant
Disadvantages of Extracorporeal Membrane Therapy
Requires an experienced team, especially with regard to complications related to the intense anticoagulation required to avoid clotting in the circuit and the associated risks of bleeding
Generally used as a last resort in people with severe ARDS and should not be implemented in patients ventilated for more than 7 days, or patients with multiple organ failure that are not candidates for lung transplant, or have absolute contraindications to anticoagulation
Airway Pressure Release Ventilation as a Rescue Therapy
Airway pressure release ventilation (APRV) is a time-cycled, pressure-controlled, inverse ratio ventilatory mode based on the concept of open lung ventilation, which relies on the application of high continuous positive airway pressure to promote and maintain alveolar recruitment, with a short phase of intermittent release to lower pressure allowing ventilation
Allows unrestricted spontaneous breathing throughout respiration
Theoretical benefits
Lung protective recruitment by decreasing the frequency of repetitive inflation/deflation of the lungs, improving ventilation in non-dependent areas through longer inspiratory duration, creating a stabilized open lung using lower pressure compared with conventional modes, and limiting atelectrauma through partial and short emptying of the lungs during the release phase
Improved patient-ventilator synchrony
Improved V/Q mismatch, decreased pulmonary vascular resistance, improved respiratory compliance, cardiac index and oxygen delivery due to unrestricted spontaneous breathing
Reduced need for sedation and neuromuscular blockade, thus theoretically leading to lower intensive care unit related delirium or neuromuscular blocking agent related myopathy
Protection against ventilator-associated pneumonia, which has been primarily observed in humans with trauma suffering from pulmonary contusions
PHigh over a prolonged period allows slow alveolar recruitment, TLow prevents alveolar collapse
The short release period terminates the expiratory flow early, permitting only partial unloading of lung capacity, causing auto-PEEP and preventing alveolar instability
To wean a patient off, the FiO2 must first be reduced, before gradually decreasing PHigh while simultaneously increasing THigh progressively at each step once PHigh reaches 20 cmH2O
The patient can then be weaned to a continuous positive airway pressure mode or switched to a conventional pressure-assisted mode and weaned conventionally
Four Basic Settings to Control in APRV Other than FiO2
High-level pressure (PHigh) - Analogous to continuous positive airway pressure, inspiratory pressure similar to plateau pressure, typically set initially as the patient’s plateau pressure on a conventional mode prior to initiation of APRV
High-pressure time (THigh) - Duration of inspiratory time; combined with PHigh, is referred to as the CPAP phase, which influences oxygenation. Commonly set to occupy 90% of the total cycle time
Low-level pressure (PLow) - Expiratory pressure similar to PEEP, typically set at 0 cmH2O to achieve the greatest pressure differential between PHigh and PLow
Low-pressure time (TLow) - Duration of expiratory time, prevents derecruitment; combined with Plow, is referred to as the release phase, which influences carbon dioxide removal
Two Strategies when Setting APRV
Fixed setting technique
Personal setting approach or time-controlled adaptive ventilation (TCAV)
Most widely used
Time spent at plateau pressure covers about 90% of the respiratory cycle
TLow is set so that the end-expiratory flow/peak-expiratory flow ratio equals ~75%, preventing alveolar collapse
Time rather than pressure controls the end-expiratory lung volume
If hypoxemia is present, an increase of PHigh, then of THigh are warranted
Only as a last resort, FiO2 should be increased
Hypercapnia can be tolerated if pH remains above 7.25 and there are not adverse effects of acidosis
Otherwise a decrease of THigh is indicated while ensuring that the respiratory circuit is free of secretions or excessive moisture
An increase in PHigh can also be considered in order to maximize recruitment and minimize dead space
If hypocapnia is present and with adequate cardiac output, an increase in THigh should be done
Main Benefits Seen with APRV
Mostly short-term endpoints, such as improvement in oxygenation, respiratory mechanics, possible decrease in hospital length of stay and ventilation requirements
High Frequency Oscillatory Ventilation as a Rescue Therapy
Delivers a low amplitude and high frequency tidal volume in combination with maintaining a high end-expiratory pulmonary pressure to decrease alveolar collapse
Should not be a routine practice in adults or pediatrics with hypoxemic respiratory failure
Brandly et al, 2023
Flow-controlled expiration reduces positive end-expiratory pressure requirement in dorsally recumbent, anesthetized horses
Objective: To further evaluate FLEX ventilation in anesthetized horses positioned in dorsal recumbency, hypothesizing that after alveolar recruitment, horses ventilated using FLEX would require lower PEEP to prevent alveolar closure than horses conventionally ventilated
Results:
Following the equilibration period and prior to the PEEP-titration alveolar recruitment maneuver, the mean PaO2 and Cdyn of the horses were 137 mmHg and 248 ml/cmH2O, respectively
After the alveolar recruitment, the PaO2 and Cdyn improved, ranging between 323-566 mmHg and 343-627 ml/cmH2O
After the decremental PEEP titration maneuver, the PaO2 and Cdyn remained stable and were not significantly different between groups
The alveolar closure pressure was significantly lower and significantly less PEEP was required to prevent alveolar closure for horses ventilated using FLEX compared with volume-controlled ventilation (VCV)
The CO was significantly higher in the horses ventilated with FLEX
Conclusion: Concluded that FLEX ventilation was associated with a lower PEEP requirement due to a more homogenous distribution of ventilation in the lungs during expiration. This lower PEEP requirement led to more stable and improve cardiovascular conditions in horses ventilated with FLEX
Guieu et al, 2024
Editorial: Reviews in invasive and non-invasive ventilation in veterinary medicine
High flow nasal oxygen therapy (HFNOT)
In dogs with hypoxemic respiratory failure, the use of HFNOT has been well-tolerated and for dogs failing conventional oxygen therapy, transition to HFNOT has consistently demonstrated improved oxygen parameters in three studies
Successful weaning from HFNOT and discharge was reported in 36-66% of cases while 27-54% died or were euthanized due to declining condition, with an additional 27% requiring escalation to MV
Main reported complications in people associated with HFNOT include various degrees of hypercapnia and rare pneumothorax
PEEP optimization
Incremental/decremental PEEP trials based on serial assessment of arterial oxygenation and/or evaluation of static lung compliance, setting PEEP based on pressure-volume loops, use of published PEEP tables, and evaluation of driving pressure are the most common tools used at bedside
Bundle
An evidence based set of treatment goals that when used together promote optimal outcomes
Most Common Interventions Found in Human Ventilator Associated Pneumonia Bundles
Elevation of the head and thorax approximately 30*
Daily “sedation vacation” to assess readiness to wean
Peptic or stress ulcer disease prophylaxis
Deep vein thrombosis prophylaxis
Oral care with or without chlorhexidine; with or without toothbrushing
Hand hygiene prior to touching any ventilator tubing or patient mouth
Hand Hygiene for Ventilated Patients
Overall compliance for washing hands between patients has been reported to be 18.2-41.7%
Reasons for not washing hands frequently included being “too busy” (72.5%) or an “unpleasant feeling on hands” (24.7%)
Use of examination gloves with any ventilated patient is recommended; however, glove use should not be used in lieu of appropriate hand hygiene
Kirby’s Rule of 20
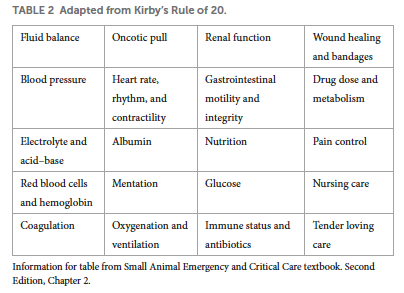
What is the minimum monitoring for any mechanically ventilated patient?
ECG, capnography (ETCO2), and pulse oximeter (SpO2)
What drop in systolic blood pressure during inspiration compared to expiration is indicative of fluid responsiveness?
A drop greater than 10 mmHg
How can intravascular volume status and hydration be monitored in ventilated patients?
Through serial body weights, physical exams, percent dehydration assessments, thoracic point-of-care ultrasound (T-POCUS) including a left atrium (LA) to aortic root (Ao) ratio and a mushroom view to evaluate cardiac contractility and left ventricle volume status
Stroke volume variation, pulse pressure variation, and plethysmographic variability index may be useful in assessing fluid responsiveness in mechanically ventilated patients
Oxyhemoglobin Dissociation Curve When Patients are Receiving Supplemental Oxygen
Sigmoidal nature of the oxyhemoglobin dissociation curve decreases accuracy in predicting PaO2 over 100, as the SpO2 can read at 100% with PaO2 anywhere between 100 and 500
What is the target SpO2 once past stabilization on the ventilator?
Typically a target of 95% SpO2 should be the goal during mechanical ventilation to mitigate the risks between hypoxia and hyperoxia
What are the two main types of probes for pulse oximetry?
Reflectance
Transmittance
Reflectance Pulse Oximetry Probes
Reflectance probes can be secured around the distal limb or tail base, and a spot reading can be performed in the femoral area
Transmittance Pulse Oximetry Probe
Can be clipped to any mucous membrane such as the tongue or lip
EtCO2/PaCO2 Discrepancy
In healthy lungs, EtCO2 is often 2-5 mmHg lower than PaCO2 due to mixing of the exhaled alveolar gas with dead space gas
Larger discrepancies between PaCO2 and EtCO2 can be due to increased dead space from too long of an endotracheal tube or circuit tubing, HME, pulmonary hypoperfusion associated with hypovolemia, or increased physiologic dead space from diseased lungs
What are ventilator settings that can change the PaCO2?
Respiratory rate, inspiratory to expiratory (I:E) ratio, tidal volume, and peak pressure
Methods to Assess Oxygenation in the Ventilated Patient
Assess the PaO2:FiO2 (P:F) ratio if the patient is receiving supplemental oxygen
Assess the A-a (Alveolar-arterial) gradient if the patient is not receiving supplemental oxygen
Goal PaO2 in Mechanically Ventilated Patients
Aiming for a PaO2 of 80 mmHg may decrease the risk of oxygen toxicity
If PaO2 is above 150 mmHg, the FiO2 should be decreased at the clinician’s discretion
Goal FiO2 in Mechanically Ventilated Patients
While many patients may require initial FiO2 of 100%, oxygen should be decreased as tolerated to an FiO2 of <60% within the first 24 hours to further reduce the risk of oxygen toxicity, with continued weaning to FiO2 of 30-40% or less prior to liberation from the ventilator
What is a normal P:F ratio?
>400
Troubleshooting Techniques for Low Tidal Volume or Low-Pressure Alarms
Checking the endotracheal tube cuff for leaks or checking to make sure the airway is still patent and that there are no blockages or leaks
If using a tracheostomy tube, making sure it is still in place
Suctioning the tracheal tube while looking for a mucus plug or increased secretions and/or changing out the tracheal tube for a new sterile one
Increasing the FiO2 to 100% prior to changing out the tracheal tube should be standard practice
What can occlusion of the endotracheal tube be seen as?
A loss or increase of EtCO2, a sudden decrease in tidal volume, an increase in peak inspiratory pressure, and/or a decrease in oxygen saturation
What will a pneumothorax be seen as?
A sudden decrease in tidal volume, an increase in airway pressure, rapidly increasing EtCO2, and rapid desaturation
The patient will typically have decreased lung sounds on one side, pulsus paradoxus, or sudden tachycardia and hypotension
What can lead to the patient “bucking the ventilator”?
Incorrect MV settings, patient discomfort or level of sedation
What are the main complications seen with mechanical ventilation?
Hemodynamic instability due to positive pressure ventilation, infections (ventilator associated and/or hospital-acquired), pneumothorax, ventilator-induced lung injury, medication side-effects, and the inability to discontinue ventilatory support
Other complications may include skin disturbances from prolonged recumbency or edema, increased gastric residual volume, and venous or arterial catheter complications
Main Complications Seen with Long Term Mechanical Ventilation in Dogs
Pneumothorax, oral and corneal ulceration, gastric distension, occlusion of the tracheal tube, urinary tract infection, edema, and non-pneumonia related hyperthermia
Maintenance of Endotracheal Tube Cuff Pressure
Inadequate cuff pressure can increase the risk of VAP, but overinflation of the endotracheal tube can lead to tissue necrosis
If a high-volume, low-pressure (HVLP) endotracheal tube is used (typically with smaller endotracheal tubes), the cuff pressure can be measured every 4 hours and does not need to be deflated and repositioned
If a low-volume, high-pressure (LVHP) endotracheal tube is used, cuff pressure is not a reliable indication of adequate seal of the airway and overinflation can lead to tracheal necrosis
For LVHP, the cuff should be deflated and repositioned every 4 hours after oral suctioning
Endotracheal Tube Replacement
Daily endotracheal tube replacement is no longer recommended
Endotracheal tube replacement should be considered only when increased resistance is observed on the ventilator waveforms and secretion build-up cannot be resolved by suctioning
Endotracheal Tube Tie Maintenance
Repositioning the ties that secure the tube should be done every 4h to reduce the risk of tissue damage of the lips. Ties should be replaced every 24h or when a new tracheal tube is placed
Elevation of the Head and Thorax in Mechanically Ventilated Patients
A body position of >30 degree incline can help reduce the work of breathing
Elevation of the head and thorax also helps avoid aspiration of refluxed gastric contents and oropharyngeal secretions
Oral Care for the Mechanically Ventilated Patient
Should include proper oropharyngeal suction technique and mechanical cleaning of all surfaces within the mouth, usually on 4-8h intervals
Use of sterile saline alone vs chemical antiseptics such as chlorhexidine, povidone iodine, and triclosan has shown to have similar reduction of risk of VAP
Suctioning should be accomplished with a vented suction tube such as a Yankauer rigid suction vented tip or similar implement for good control while suctioning
Eye Care in Mechanically Ventilated Patients
Every 24h, a fluorescein stain evaluation should be performed to monitor for development of ulceration
Gastric Residual Volume (GRV)
It is common practice to routinely aspirate and measure GRV; however there may be little evidence to support this as being beneficial to the patient
Reduction of GRV may decrease incidence of vomiting and regurgitation, however, lower GRV is not necessarily associated with a lower instance of VAP
A negative side effect of regular GRV measurement is decreased total caloric intake for the patient and changes in the electrolyte status
Sacks et al, 2023
Impact of sedation, body position change, and continuous positive airway pressure on distribution of ventilation in healthy foals
Objective: To compare the distribution of ventilation measured by electrical impedance tomography (EIT), in foals under varying clinical conditions or sedation, postural changes, and continuous positive airway pressure (CPAP). To support the interpretation of EIT variables, specific spirometry data and F-shunt calculation were also assessed.
Results:
Respiratory rate was lowered after sedation
While respiratory rate decreased, tidal volume increased maintaining minute ventilation relatively constant
In right lateral recumbency (compared to standing), the ventral to dorsal center of ventilation (COVVD), right to left center of ventilation (COVRL), left centro-dorsal and dorsal regional ventilation were high while the right ventral and dorsal regional ventilation, and right to left lung ventilation ratio (R:L) were lower
Indicates a shift of ventilation toward the dorsal and left areas
The short time elapsed until notably reduced ventilation and lung collapse of the dependent lung indicates a potential deleterious effect of positioning sedated foals in lateral recumbency
F-shunt increased by 6% from standing unsedated to sedated foals in right lateral recumbency
Data of two foals for CPAP10 was excluded from statistical analysis due to prolonged apnea
Apnea may be due to activation of the Hering-Breuer reflex in response to direct activation of airway stretch receptors due to tissue over-distension or increased mean airway pressure
Stepwise increase of CPAP lead to increases of COVVD and VT
A reduction of respiratory rate was detected with increasing CPAP levels
Conclusion: In healthy foals, diazepam administration did not alter distribution of ventilation or minute ventilation, lateral recumbency results in collapse of dependent areas of the lung, and the use of CPAP in dorsal recumbency at increasing pressures improves ventilation in dependent regions, suggesting improvement of ventilation-perfusion mismatch
Raidal et al, 2023
Effects of 2 modes of positive pressure ventilation on respiratory mechanics and gas exchange in foals
Objective: Assess the effect of different airway pressures during CPAP and PSV have on respiratory function in healthy foals with pharmacologically induced respiratory insufficiency. Hypothesized that increased airway pressures would improve respiratory mechanics and increased PEEP would be associated with hypercapnia
Results:
Sedation and dorsal recumbency were associated with significant reductions in arterial oxygen pressure (PaO2), respiratory rate, and tidal volume
Continuous positive airway pressure was associated with improved PaO2, without concurrent hypercapnia
Effect was most strongly correlated with mean airway pressure during ventilation
PIPs up to 20 cmH2O can be used in healthy foals without negative impact on dead space ventilation
Volumetric capnography identified improved V/Q matching and increased carbon dioxide elimination during ventilation, and spirometry identified decreased respiratory rate and increased tidal volume
Peak inspiratory pressure was moderately associated with PaO2 and lung volume
During PSV and CPAP, periods of apnea were common, especially during CPAP of 10 cmH2O where the ventilator switched to PSV
Might be attributed to activation of the Hering-Breuer reflex in response to increased end expiratory pressures
Improved pulmonary aeration was evident in CT images and lung volume was increased, particularly during CPAP
Conclusion: Both CPAP and PSV improved lung mechanics and gas exchange in healthy foals with induced respiratory insufficiency
What does reduced FRC result in?
Less alveolar tension pulling the airways open, and subsequently airway narrowing or collapse and increased airway resistance
What are the two mechanisms that PEEP contributes to decreased cardiac output through?
Increases intrathoracic pressure which contributes to increasing right atrial pressure and decreased venous return
By increased pulmonary vascular resistance, which results in increased right ventricular afterload
What can overdistension from PEEP lead to?
Alveolar inflammation, injury, and increased lung stress
If alveolar pressure is greater than pulmonary capillary pressure, capillaries may be occluded and lead to increased alveolar dead space
Methods to Assess Response to a Recruitment Maneuver
Using POCUS to visualize the most dependent zone of atelectasis with POCUS and monitoring for resolution of consolidation and re-aeration
Measurement of the recruitment-to-inflation ratio (R/I ratio)
Oxygenation is not a perfect marker of alveolar recruitment but it is one of the most commonly used in clincial settings
Techniques for Setting the Optimal PEEP
Arterial oxygenation targets remain the most widely used technique for setting PEEP in practice
Setting PEEP based on the lower infection point on the PV loop
Use of PEEP tables
Compliance
DP
SI
Transpulmonary pressures
Imaging
Electrical impedance tomography
Recommendation for Recruitment Maneuvers
Not sufficient evidence to recommend the routine use of RMs
If a RM is used, a stepwise RM is recommended over a sustained inflation RM
Once the RM is complete, PEEP should be adjusted to maintain the recruitment and prevent de-recruitment
Using ARDS Network PEEP/FiO2 Tables
Involves adjusting PEEP and FiO2 such that PEEP targets must be met before FiO2 is increased further
Adjustments are made based on the table until oxygenation goals of SpO2 88-95% and/or PaO2 55-88 mmHg are met
How does the pressure volume loop change when there is a decrease in lung compliance?
Rotates closer to the x-axis, lying more horizontally
How does the pressure volume loop change when there is an increase in lung compliance?
PV loop rotates toward the y-axis, lying more vertically
Inflection Points on Pressure Volume Loops
Lower inflection point (LIP) - represents the point at which compliance increases significantly, likely due to the recruitment and opening of alveoli
Upper infection point (UIP) on inspiratory limb - point at which compliance decreases due to the overdistension of alveoli
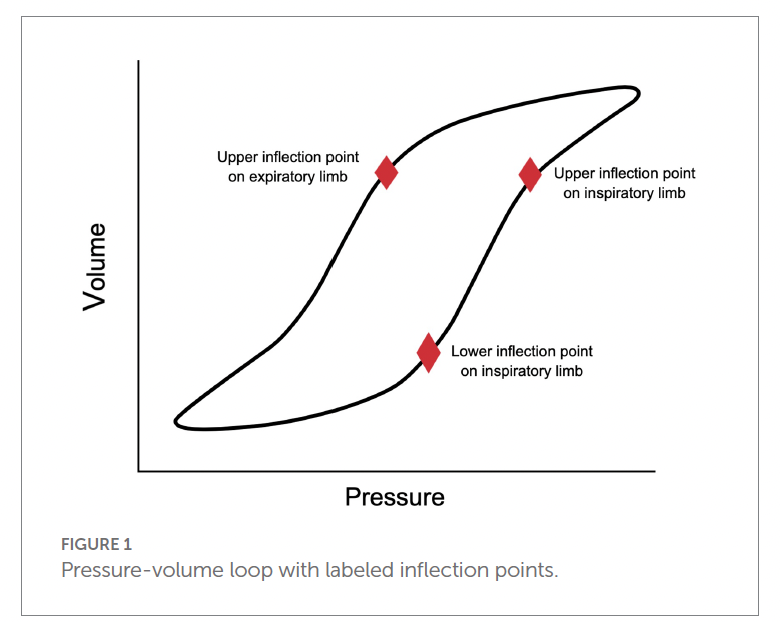
Techniques Currently Recommended for Using the PV Loop to set PEEP
Setting PEEP at 2 cmH2O higher than the inspiratory limb LIP
Setting PEEP at the UIP of the expiratory limb of the UIP
Based on the fact that de-recruitment is an expiratory phenomenon so setting PEEP above the expiratory limb UIP would minimize de-recruitment
Open lung ventilation strategy suggesting setting PEEP above the inspiratory limb LIP and setting tidal volume (TV) so the plateau pressure (Pplat) is below the UIP
Downsides to Using PV Loops to Determine PEEP
Ability to acquire a reliable PV loop without artifact
Neuromuscular blockade and breath holds for static assessments are required to obtain adequate PV loops
Technically challenging
Static Compliance
The pulmonary compliance during no-airflow conditions
Measured during an inspiratory hold
Dynamic Compliance
Pulmonary compliance measured during breathing
Influenced by both compliance and resistance
Static and Dynamic Compliance Formulas
Measurement of plateau pressure is required to calculate Cs and is obtained using an inspiratory hold technique
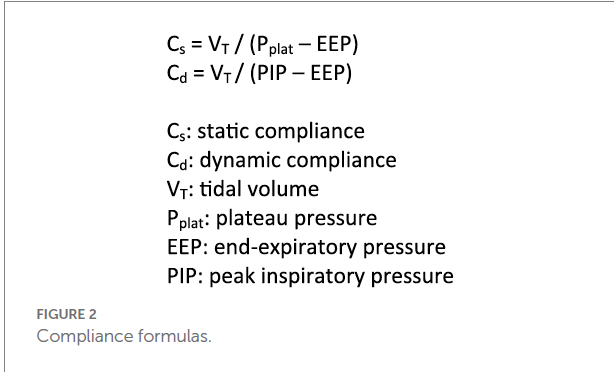
Using Compliance to Set PEEP
Study found that maximum oxygen delivery was achieved at the PEEP associated with the highest Cs
Conerns with using Cs to set optimal PEEP as Cs does not always increase after administration of PEEP, even when there is significant lung recruitment documented with CT
Compliance measurements are global estimates and do not take into account regional variations, when we know that alveolar recruitment and overdistension are heterogenously distributed
To implement this technique, an RM should be performed and PEEP should be increased
Then PEEP should be decreased in a stepwise fashion and Cs measured at each change
The PEEP that produces the highest Cs is the appropriate PEEP setting for that patient
A second RM can be performed, followed by setting PEEP at the appropriate setting based on the previous Cs measurements
Driving Pressure
Driving Pressure (DP) is calculated as the difference between inspiratory plateau pressure and PEEP, or the ratio of TV to compliance (DP = Pplat - PEEP or DP = TV/compliance)
In the absence of respiratory effort by the patient, DP represent the pressure above PEEP which is applied to the respiratory system to achieve ventilation
Reflects the size of TV relative to aerated lung volume and therefore correlates with overall lung strain and pulmonary compliance
Driving Pressure as a Predictor of Outcome
DP has been shown to be a strong predictor of lung stress and outcome
ARDS patients with a DP >7 cmH2O have been shown to have an increased risk for mortality and in a more recent study, a DP of >14 cmH2O on day 1 had a worse outcome
DP also associated with lung stress such that higher DPs have significantly higher lung stress
Decreases in DP have been shown to be more strongly associated with lower mortality compared to increases in the PaO2/FiO2 ratio, confirming DP was the key variable associated with outcome