HLTHPS001 - TAKE CLINICAL MEASUREMENTS
0.0(0)
Card Sorting
1/208
Last updated 9:19 AM on 10/30/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
209 Terms
1
New cards
Duty of care takes into account several different aspects:
» Legal: What does the law suggest you do?
» Professional/ethical: What do other your colleagues expect you to do?
» Organisational: What does your organisation and/or its funding body expect from you?
» Community: What do the parents of your patients (if they are minors) expect you to do?
» Personal: What do your own beliefs and values suggest you do?
» Professional/ethical: What do other your colleagues expect you to do?
» Organisational: What does your organisation and/or its funding body expect from you?
» Community: What do the parents of your patients (if they are minors) expect you to do?
» Personal: What do your own beliefs and values suggest you do?
2
New cards
Informed Consent
consent by a patient to undergo a medical or surgical treatment or to participate in an experiment after the patient understands the risks involved
3
New cards
in the case of dealing with teenagers, confidentiality may be broken
» they believe a child is seriously at risk of harming or killing himself
» they believe a child is being harmed, or at risk of being harmed
» they believe a child is harming someone else or at risk of harming someone else.
» they believe a child is being harmed, or at risk of being harmed
» they believe a child is harming someone else or at risk of harming someone else.
4
New cards
Children in the Workplace
Managing the health of a child, the responsibility falls to a parent or legal guardian. It is their role to manage the child’s best interests, both by interacting with healthcare professionals and making sound decisions on their behalf.
5
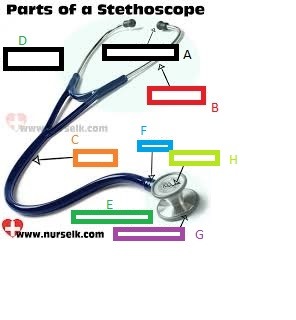
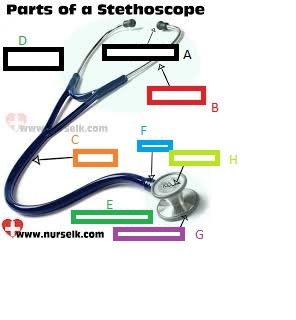
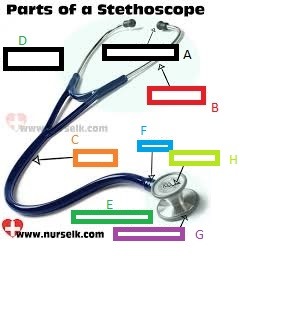
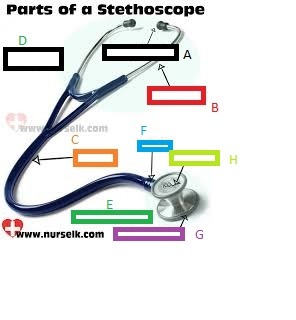
New cards
Duty of Care
you have a responsibility to your patients to foresee any harm or injury they may experience, and it’s up to you to reduce or limit appropriately. What adds a layer of difficulty to this, however, is your responsibility to one party (let’s say your employer, for example) might conflict with the responsibilities you have to your patients.
6
New cards
Mandatory Reporting
used to describe the legislative requirement for selected groups of people to report suspected cases of child abuse and neglect to government authorities
7
New cards
Records Management
8
New cards
Confidentiality
Confidentiality relates to the rules that limit access to any information discussed between a person and their healthcare practitioner.
9
New cards
Disclosure
means to reveal or expose information that has previously been kept a secret
10
New cards
Industry Standards
In Australia, we follow the National Safety and Quality Health Service (NSQHS) standards, which provide a nationally consistent statement of the level of care consumers can expect from health service organisations.
11
New cards
three guiding principles applied in the Australian healthcare system.
1. Everyone has the right to be able to access health care, and this right is essential for the charter to be meaningful.
2. The Australian government is committed to international agreements about human rights which recognise everyone’s right to have the highest possible standard of physical and mental health.
3. Australia is a society made up of people with different cultures and ways of life, and the Charter acknowledges and respects these differences.
2. The Australian government is committed to international agreements about human rights which recognise everyone’s right to have the highest possible standard of physical and mental health.
3. Australia is a society made up of people with different cultures and ways of life, and the Charter acknowledges and respects these differences.
12
New cards
seven fundamental rights
Safety - A right to receive safe and high-quality healthcare.
Privacy- A right to privacy and confidentiality of your personal e.
Access - A right to access health care.
Respect - A right to be shown respect, and to be treated with dignity and consideration.
Communication - A right to be informed about services, treatment, options and costs in a clear and open way.
Participation - A right to be included in decisions and to make choices about your health care.
Comment - A right to comment on your health care, and to have your concerns addressed.
13
New cards
Workplace boundaries
allows organisations to be able to work more efficiently because redundant tasks can be eliminated, and people can be held accountable for their duties.
14
New cards
Standard Procedures for Infection Control
» hand washing
» use of personal protective
equipment (PPE)
» avoiding contact with bodily fluids
» sharps injury considerations
» waste disposal
» use of personal protective
equipment (PPE)
» avoiding contact with bodily fluids
» sharps injury considerations
» waste disposal
15
New cards
Hand Washing
» before touching a patient
» before clean/aseptic procedures
» after body fluid exposure/risk
» after touching a patient
» after touching patient surroundings.
» before clean/aseptic procedures
» after body fluid exposure/risk
» after touching a patient
» after touching patient surroundings.
16
New cards
Use of Personal Protective Equipment (PPE)
In healthcare settings is to control cross infection, by acting as a barrier between infectious materials and your skin, nose, mouth or eyes, thus blocking the transmission of contaminants from blood, bodily fluids or respiratory secretions.
17
New cards
PPE inclues
Gloves: protect your hands from germs, helping to reduce their spread
Masks: help cover your mouth and nose, protecting you from germs and preventing your germs from spreading.
Eye protection: like shields and goggles which protect your eyes from bodily fluids like blood.
Clothing: To stop the liquids or other hazardous materials touching your skin
Masks: help cover your mouth and nose, protecting you from germs and preventing your germs from spreading.
Eye protection: like shields and goggles which protect your eyes from bodily fluids like blood.
Clothing: To stop the liquids or other hazardous materials touching your skin
18
New cards
where in the eyes germs get in
mucous membranes
19
New cards
if you come in contact with either bodily fluids or blood:
» Flush the area with running water
» Wash the area with plenty of warm water and soap
» Report the incident to the appropriate staff member
» Record the incident via the Disease/Injury/ Near Miss/Accident (DINMA) reporting procedure
» Seek medical advice.
» Wash the area with plenty of warm water and soap
» Report the incident to the appropriate staff member
» Record the incident via the Disease/Injury/ Near Miss/Accident (DINMA) reporting procedure
» Seek medical advice.
20
New cards
Waste can be divided into three key groups
» general = Place in the general waste bin for removal
» clinical = has the potential to cause injury, infection or offence
» pharmaceutical = leftover pharmaceuticals, you should return to pharmacy for correct disposal
» clinical = has the potential to cause injury, infection or offence
» pharmaceutical = leftover pharmaceuticals, you should return to pharmacy for correct disposal
21
New cards
needlestick injury
- Wash the area of the wound with soap and water or alcohol-based hand
- Notify your manager or WHS officer by filling out an accident report
- Seek medical treatment immediately in order to have testing done to check for infectious diseases
- Notify your manager or WHS officer by filling out an accident report
- Seek medical treatment immediately in order to have testing done to check for infectious diseases
22
New cards
Equipment used to take clinical measurements might include:
» Sphygmomanometer
» Stethoscope
» Timing device
» Peak flow meter and disposable mouthpieces
» Penlight
» Stethoscope
» Timing device
» Peak flow meter and disposable mouthpieces
» Penlight
23
New cards
sphygmomanometer
It is a device that is used to measure a person’s blood pressure. A combination of Greek words; ‘sphygmos’ which means the pulse or beating of the heart, and ‘manometer’ which is a tension or pressure-measuring device.
24
New cards
A sphygmomanometer consists of three main parts:
» An inflatable cuff that is designed to wrap around the upper arm
» An inflation mechanism which is either a manually or electronically operated bulb or pump
» A measuring unit which displays the systolic and diastolic pressure reading during arterial blood flow.
» An inflation mechanism which is either a manually or electronically operated bulb or pump
» A measuring unit which displays the systolic and diastolic pressure reading during arterial blood flow.
25
New cards
Aneroid sphygmomanometers
an air pressure gauge that registers the blood pressure by a pointer on a dial.
26
New cards
Digital sphygmomanometers
use electronically inflated cuffs to measure systolic and diastolic blood pressure. easy to operate and practical in noisy environments. (less reliable)
27
New cards
Using a blood pressure cuff that is too small:
using a cuff that is too small can cause a patient's systolic blood pressure measurement to increase 10 to 40 mmHg.
c Full bladder: Make sure the bladder has been recently emptied before reading as blood pressure increases as the bladder fills. Studies have shown that the systolic blood pressure measurements could increase 10 to 15mmHg when you have a full bladder.2
c Full bladder: Make sure the bladder has been recently emptied before reading as blood pressure increases as the bladder fills. Studies have shown that the systolic blood pressure measurements could increase 10 to 15mmHg when you have a full bladder.2
28
New cards
Using a blood pressure cuff used over clothing:
Try to place the cuff on a bare arm as studies have shown clothing can impact a systolic blood pressure from 10 to 50 mmHg.
29
New cards
Patient not resting for 3-5 minutes before reading:
Any activities including exercise or eating can affect systolic blood pressure measurement 10 to 20 mmHg.
30
New cards
Arm/Back/Feet Unsupported:
Patients should always be seated in a comfortable chair, with legs uncrossed, and their back and arm supported. Crossing legs has shown to raise systolic blood pressure by 2 to 8 mmHg. The positioning of the upper arm below heart level will also result in higher measurements, whereas positioning the upper arm above heart level will give lower measurements. These differences can increase/decrease systolic blood pressure 2mmHg for every inch above/below heart level.
31
New cards
The effect of emotional state on readings:
A poor emotional state can cause significant increases in blood pressure. To avoid this, the patient should try to think about calming things
32
New cards
Talking
Encourage patients to be quiet during readings as studies have shown that systolic blood pressure measurement may increase 10 to 15mmHg if talking
33
New cards
Smoking, alcohol and caffeine:
These all cause spikes in blood pressure and so should be avoided for at least 30 minutes before a reading is taken.
34
New cards
Full bladder
Make sure the bladder has been recently emptied before reading as blood pressure increases as the bladder fills. Systolic blood pressure measurements could increase 10 to 15mmHg when you have a full bladder.2
35
New cards
stethoscope
a medical instrument for listening to the sounds generated inside the body
36
New cards
heart makes typically what sound
“lub-dub, lub-dub
37
New cards
when heart makes whooshing sound
this may indicate a heart murmur or other irregularities in blood flow.
38
New cards
When listening to the lungs
Wheezes may indicate that the airways are restricted, and crackles might mean there is fluid in the lungs.
39
New cards
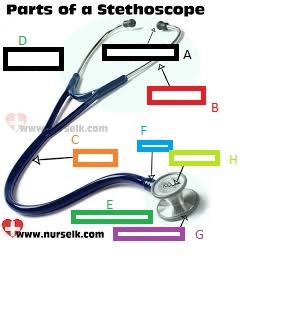
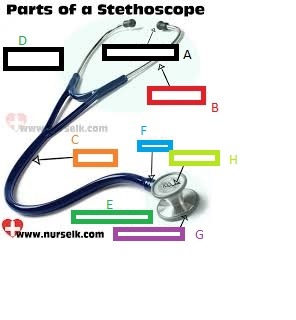
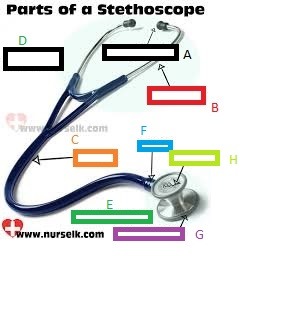
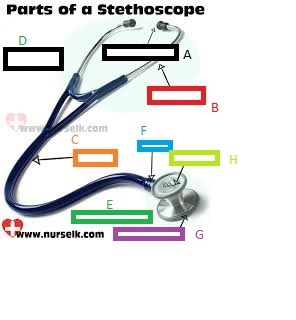
What part of the Stethoscope is A?
Eartip
40
New cards
What part of the Stethoscope is B?
Eartube
41
New cards
What part of the Stethoscope is C?
Chestpiece
42
New cards
What part of the Stethoscope is D?
Headset
43
New cards
What part of the Stethoscope is E?
Tubing
44
New cards
What part of the Stethoscope is F?
Stem
45
New cards
What part of the Stethoscope is G?
Diaphragm
46
New cards
What part of the Stethoscope is H?
Bell
47
New cards
Choosing a diaphragm or bell
diaphragm is generally better for hearing medium or high-pitched sounds like heart. The bell will be superior for hearing low-pitched sounds like lungs.
48
New cards
stethoscope
a medical instrument for listening to the sounds generated inside the body, eg heart beat, lung sounds, brachial pulse for blood pressure
49
New cards
Position your patient
If you want to listen to your patient’s heart or abdomen, you will need to position them in a supine position; in layman’s terms, this means lying down. To listen to the lungs, it’s best to have them sitting up.
50
New cards
Caring For Your Stethoscope
You should also avoid bending the tubes too tightly
51
New cards
Digital thermometers
allow a person’s temperature to be taken with minimal contact between the instrument and the person, meaning the disinfection process for the thermometers, between patients, is minimal or altogether unnecessary.
52
New cards
Non-contact thermometers
can be used to record temperatures from the mouth, armpit or rectum, and are best to be used with a probe cover where available.
53
New cards
armpit temperature
Armpit temperatures are the least accurate in all age groups, where, by comparison, rectal temperatures provide the most accurate readings for children aged 3 months to 3 years.
54
New cards
mouth temperature
In older children or adults, take an oral reading by having them place the digital thermometer under the tip of their tongue, towards the back of their mouth. They should then close their lips around the thermometer, until it beeps to indicate it has taken its reading.
55
New cards
A peak flow mete
is a small hand-held tool that is used to measure a person’s peak expiratory flow rate, often shortened to their PEFR. This is the amount of air a person can quickly force out of their lungs in one breath.
56
New cards
primary use of PEFR measurements
a guide for managing asthma symptoms, or occasionally other respiratory conditions including chronic obstructive pulmonary disease (COPD). These measurements can also be used to monitor whether there is an increase or decrease in symptoms.
57
New cards
effectively use of a peak flow meter
the user must blow forcefully into the device where the meter will measure the forced air in litres per minute. And should be taken while standing up
58
New cards
Asthma Management Plan
peak flow measurements is a large part of many asthmatic to help treat their condition. The recognition of symptoms at this early stage allows prevention mechanisms to be put into place to at least decrease them, if not stop them altogether.
59
New cards
How to Use a Peak Flow Meter
1. Ensure the indicator or pointer is set at zero.
2. Take a deep breath.
3. Place the meter in the mouth, making sure that the tongue is both down and away from the mouthpiece.
4. Close lips around the mouthpiece.
5. Blow out hard and fast until the indicator moves in response to the exhalation.
6. Look at the number on the scale where the pointer or indicator is; this indicates the peak expiratory flow.
7. Move indicator back to zero and repeat the process two more times.
8. Take the best number of the three attempts and record it.
2. Take a deep breath.
3. Place the meter in the mouth, making sure that the tongue is both down and away from the mouthpiece.
4. Close lips around the mouthpiece.
5. Blow out hard and fast until the indicator moves in response to the exhalation.
6. Look at the number on the scale where the pointer or indicator is; this indicates the peak expiratory flow.
7. Move indicator back to zero and repeat the process two more times.
8. Take the best number of the three attempts and record it.
60
New cards
A decline in peak flow results could indicate:
- the need to get medical care promptly
- a flare-up of symptoms and an imminent asthma attack
- a need to revise daily medication plans.
- a flare-up of symptoms and an imminent asthma attack
- a need to revise daily medication plans.
61
New cards
Improvements or steadying of peak flow results could indicate:
- current medication and course of action is working
- asthma symptoms are well controlled.
- asthma symptoms are well controlled.
62
New cards
penlight
a thin flashlight that is shaped just like a pen. Penlights are designed to illuminate one particular area with a bright light, rather than a wide area.
63
New cards
Penlights are usually used as ..
as a diagnostic tool and are especially handy when used to assess symptoms in the mouth and throat or relatively small areas where it would be difficult to use a traditional flashlight.
64
New cards
Penlights are commonly used to assess:
Penlights are commonly used to assess:
» Pupil response: Abnormal pupil response can be symptomatic of many conditions, including concussions, alcohol intoxication, drug use and injury to or disease of the eyes and their nerves.
» Wounds of the mouth/throat: Overhead light isn’t always strong enough to illuminate wounds and injuries in this area for a full assessment. Luckily a penlight is a perfect size and shape to examine those areas quickly and without being invasive for the patient.
» Illuminating a patient’s room: In a hospital environment, healthcare professionals often use a penlight at night if they’re checking in on
a patient. This saves the need to turn on the overhead lights and reduces the risk of waking them unnecessarily.
» Pupil response: Abnormal pupil response can be symptomatic of many conditions, including concussions, alcohol intoxication, drug use and injury to or disease of the eyes and their nerves.
» Wounds of the mouth/throat: Overhead light isn’t always strong enough to illuminate wounds and injuries in this area for a full assessment. Luckily a penlight is a perfect size and shape to examine those areas quickly and without being invasive for the patient.
» Illuminating a patient’s room: In a hospital environment, healthcare professionals often use a penlight at night if they’re checking in on
a patient. This saves the need to turn on the overhead lights and reduces the risk of waking them unnecessarily.
65
New cards
Pupil response:
Abnormal pupil response can be symptomatic of many conditions, including concussions, alcohol intoxication, drug use and injury to or disease of the eyes and their nerves.
66
New cards
Wounds of the mouth/throat:
Overhead light isn’t always strong enough to illuminate wounds and injuries in this area for a full assessment. Luckily a penlight is a perfect size and shape to examine those areas quickly and without being invasive for the patient.
67
New cards
Illuminating a patient’s room:
In a hospital environment, healthcare professionals often use a penlight at night if they’re checking in on a patient. This saves the need to turn on the overhead lights and reduces the risk of waking them unnecessarily.
68
New cards
Percussion (Reflex) Hammer
is an instrument used to test deep tendon reflexes. Testing these reflexes is a crucial part of the physical, neurological examination and used to detect abnormalities in either the central or peripheral nervous system.
69
New cards
The strength of a reflex can be ..
used to gauge central and peripheral nervous system disorders
70
New cards
accepted convention for recording deep tendon reflexes
0 (No response) = abnormal
+1 (A slight but definitely present response) = may or may not be normal
+2 (A brisk response) = normal
+3 (A very brisk response) = may or may not be normal
+4 (The tap elicits a repeating reflex) = abnormal
+1 (A slight but definitely present response) = may or may not be normal
+2 (A brisk response) = normal
+3 (A very brisk response) = may or may not be normal
+4 (The tap elicits a repeating reflex) = abnormal
71
New cards
A measuring tape or tape measure
is a portable device that is used to quantify the size of a particular object or the distance between objects.
72
New cards
measure over tight filling clothing or on bare skin. Key areas for circumference measurements include:
- Bust:
- Chest:
- Waist:
- Hips:
- Thighs and calves:
- Upper arm:
- Chest:
- Waist:
- Hips:
- Thighs and calves:
- Upper arm:
73
New cards
Bust: (measurement)
Measure around the chest in line with the nipples. Ensure you don't pull the tape too tight.
74
New cards
Chest: (measurement)
This measurement is taken just under the bustline.
75
New cards
Waist: (measurement)
Measure just above the belly button or at the smallest part of the patient’s waist.
76
New cards
Hips: (measurement)
The measurement should be taken around the widest part of the hips.
77
New cards
Thighs and calves: (measurement)
Measure around the widest part of each thigh or calf.
78
New cards
Upper arm: (measurement)
Measure above the elbow around the largest part of each arm.
79
New cards
Equipment for measuring height and weight
In children, this might be to track their growth rate, while in adults it might be to ensure they are maintaining a healthy weight to avoid the onset of conditions such as heart disease, high blood pressure, type 2 diabetes and a range of other problems that can be triggered by obesity.
80
New cards
A stadiometer
is a piece of equipment that’s used for measuring human height. It is usually constructed out of a ruler/measuring tape, and a sliding horizontal headpiece which when adjusted downwards should rest gently on the top of a patient’s head to ascertain a correct reading.
81
New cards
Measuring Weight
Done by using scales. Babies will be weighed naked to get an accurate indication of their progress, whereas children and older patients will generally be weighed in underwear or light clothing.
82
New cards
what to avoid for weight -ins
Shoes and heavy clothing, including jackets, should be removed, and similar clothing should be worn for consecutive weigh-ins.
83
New cards
Four primary vital signs:
- body temperature (BT)
- pulse or heart rate (HR)
- blood pressure (BP)
- breathing rate or respiratory rate (RR).
- pulse or heart rate (HR)
- blood pressure (BP)
- breathing rate or respiratory rate (RR).
84
New cards
vital signs
a group of the most critical medical signs to indicate the status of the body’s life-sustaining functions; the reason they’re referred to as vital!
85
New cards
Vital signs are recorded using
an internationally accepted standard coding system called the LOINC
86
New cards
To obtain accurate readings
ensure the person not smoke, drink coffee, or exercise vigorously for 30 minutes before measuring their vital signs,
87
New cards
body temperature
The body’s core temperature is controlled by a process called thermoregulation
88
New cards
An average temperature reading
is considered to be 37°C (degrees Celsius), equivalent to 98.6°F (degrees Fahrenheit). However, anything between 36.4°C and 37.5°C (97.6°F to 99.6°F) is generally considered acceptable.
89
New cards
A temperature over 38°C (100.4°F) indicates :
indicates a fever that’s caused by illness or injury. On the other end of the spectrum is hypothermia which occurs when the body temperature dips below 35°C (95°F).
90
New cards
Blood Pressure
indicates how effectively oxygenating blood is moving through the circulatory systems of blood vessels.
91
New cards
Blood pressure is expressed in two parts:
firstly, systolic pressure which is the pressure created when blood pumps from the heart into the arteries and secondly; diastolic pressure which is the pressure inside the artery as the heart rests between beats.
92
New cards
The blood pressure measurement:
is recorded with two numbers, in units expressed as mm Hg (millimetres of mercury). The reading shows as systolic/diastolic, which might, for example, be displayed as 82/125.
93
New cards
n adults, systolic pressure should show
a reading of less than 130, and diastolic pressure should show a reading of less than 85.
94
New cards
Blood pressure that is too low and too high is called:
Blood pressure that is too low is called hypotension, and blood pressure that is too high is called hypertension
95
New cards
Heart Rate (Pulse)
The number of times a heart beats per minute (bpm) is referred to as the pulse or heart rate. The pulse should range between 60 to 100 beats per minute. Many highly trained athletes have an average resting heart rate closer to 40 beats per minute
96
New cards
Patients whose readings fall outside the range of 60 to 100 beats per minute:
Will likely be sent for additional testing, if the patient displayed symptoms such as dizziness or shortness of breath. The further lines of investigation would likely start with an electrocardiogram, or an ‘ECG’.
97
New cards
Respiration rate
is how many breaths a person takes per minute. There are a variety of factors such as fever, illness, agitation, age, and sleep that can affect breathing and as such, the respiratory rate.
98
New cards
To take the respiration rate:
1. Wash your hands thoroughly.
2. Place your fingers on either side of the individual’s wrist.
3. Count their breaths (inhale + exhale = 1 respiration) for one minute.
4. Document their respiration rate, making sure also to note any other observations,
2. Place your fingers on either side of the individual’s wrist.
3. Count their breaths (inhale + exhale = 1 respiration) for one minute.
4. Document their respiration rate, making sure also to note any other observations,
99
New cards
To take heart rate:
1. Wash your hands thoroughly.
2. Ensure that individual is at rest and relaxed before you begin.
3. Find the pulse.
4. Use your first and second fingertips and press firmly, but gently on the wrist.
5. Use a time measuring device and begin counting the beats of the pulse over a 60 second period. You can also count for 15 seconds and multiply by 4 to calculate your result but for the best result, count for the full 60 seconds.
2. Ensure that individual is at rest and relaxed before you begin.
3. Find the pulse.
4. Use your first and second fingertips and press firmly, but gently on the wrist.
5. Use a time measuring device and begin counting the beats of the pulse over a 60 second period. You can also count for 15 seconds and multiply by 4 to calculate your result but for the best result, count for the full 60 seconds.
100
New cards
Never use your thumb when measuring
a patient’s pulse as our own pulse can be felt through this digit and can be mistaken for the patient’s pulse.