Parasites End of year
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
50 Terms
Trichostrongylus
Black Scour
SI, Abomasum
Ruminants, horses, pig

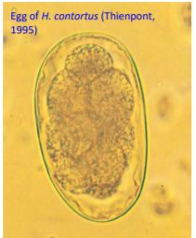
Haemonchus Contortus AKA Barber’s Pole
Abomasum cattle
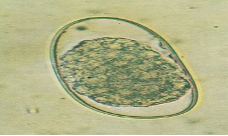
Eggs: Long egg w/parallel sides
Path: Fatal anaemia, sudden death in heavy infections
bottle jaw, anaemia, ascites, red-brown abomasum, Dx (Cattle)
Dx: FAMACHA, Haemostix/Dipstix

Ostertagia/Teladorsagia AKA brown stomach worm
Abomasum - cattle sheep goat

Cooperia Punctata & Pectinata AKA Cooper’s Worm
SI Cattle »sheep»goat

Nematodirus Threadneck worm
SI Sheep
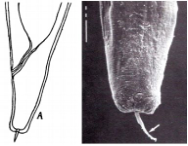
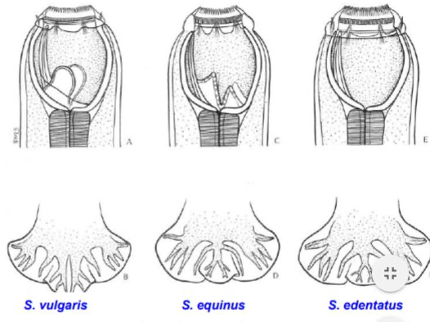
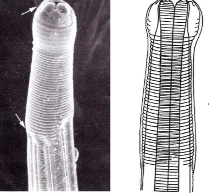
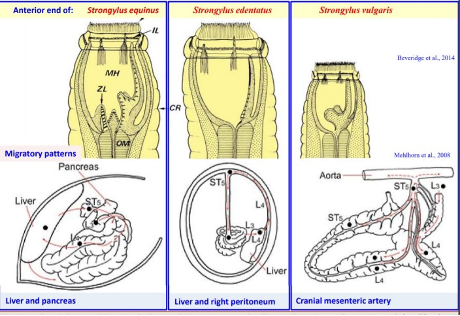
Strongylus Vulgaris
Verminous arteritis
Horse, donkey, mule

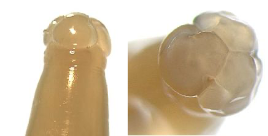
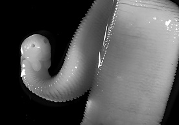
Cyathostominae AKA Small Strongyles, Redworms
Horse, bird
Caecom, colon glands
Strongyloids
oesophagostomum
LI
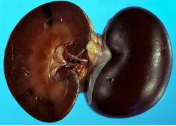
Stephanurus Dentatus AKA Kidney Worm

Bunostomum
Lungs —> Intestine
Dairy calves
Hookworm
Ancylostoma Caninum
SI
Tracheal, oral, somatic
Dog, wolf
Bloody diarrhoea + Anaemia in puppies
- Dx eggs – faecal smear, faecal flotation
- Low numbers of eggs considering dz severity:
o Many worms likely immature – very pathogenic, don’t lay eggs
- Txm to puppies
o Via milk most likely
o Hypobiotic larvae in tissue of female, reactivation during preg last trimester
o Insensitive to Tx during hypobiosis, may have been reactivated also from Tx
(decline in adult population in female)
o But many routes of Txm from L3
Percutaneous
ingestion (milk, PH, env)
- c/signs
o feed on mucosa and blood, change feeding sites 4-6x per day
o leave behind bleeding wounds, large amounts of blood lost through GIT
- how to Tx
o eliminate parasites immediately – pyrantel, BZ, ML
o supportive Tx – blood transfusion, Fe, fluids, enteral nutrition ASAP
- prevention
o Tx puppies at 2wo & every 2w until 3m
o Tx female at same time as puppies
o Then treat animals either monthly (NG spectra)
- Significance for human health
o CLM, dvp in SI of humans


Heterakis Gallinarum
SI —> Caecum
Birds


Ascarid
Toxocara Canis
SI - can migrate to stomach, bile ducts
Dogs
Diarrhoea, vomiting, anaemia, rough coat. Worm can be seen in vomit
- Infection
o Placenta, milk most likely
o Other Txm routes – ingest: PH, embryonated egg, immature worms
(how female got infected)
- Tx/prevention
o Tx puppies with milbemax from 2wo every 2w until 3mo
o Then monthly or 3monthly wormer (NG spectra, or Bravecto plus, or drontal)
o Eggs very resistant in env (can survive many years, not killed by typical disinfectants)
- Significance for humans
o OLM, VLM – common in children
- Prevention in humans
o Worm puppies and dogs regularly – emphasis on nursing bitches/puppies
o Reduce stray animals, educate owners on zoonoses
o Clean faeces from soil/pavements
o Prevent dogs in playgrounds


Toxocara Cati
Liver —> Somatic
Cats

Ascaris Summ
SI, stomach, liver, lungs
Pigs

Parascaris Equorum
SI, liver, lungs
Fenbenzadole

Habronema Muscae
Gastritis/ulcers
Horse
Draschia Megastoma causes similar disease


Dirofilaria Immitis AKA Heartworm
Most animals
Adults – peripheral pulmonary a., right ventricle +- RA, CdVC, Microfilaria – Blood
-Microfilaria detection: Absent if prepatent, single sex, geriatric, drug-mediated elimination
Methods: Blood smear, modified knotts test, filter test
Ag detection: Produced by the uterus of females →persists 3-5m post death
Issues: Ag suppressed by ML’s, may lag behind mature female appearance by weeks
Melarosmine, Mls, Doxycycline (Wolbachia)

Oxyuris Equi
Horse
LI
yellow grey curst on anus

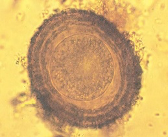
Trichuris AKA Whipworms
LI and in mucosa anteriorly
Pis, dogs, ovine, cattle
- Detection
o ZnSO4 floatation (high gravity, don’t float easily)
o Sedimentation (direct method)
- Young animals high burden?
o Long PPT (3yo dog)
o Worms not eliciting sig protective immune response
- Why intermittent shedding
o F = intermittent egg producer, produce low # eggs/day
o Sample faeces over a few days
o Do not float in all floatation solutions
- Drug failure (pyrantel)
o Drug insensitive parasite
o Distant taxonomy to most nematodes (different subclass)
- Tx recommendation
o BZ – fenbendazole 3d consecutively
o Drontal – ML + febantel combined
o Repeat treatment monthly for 3months (resistant), reinfection likely
o Hygiene – remove faeces
- Significance for humans
o Very rarely infects humans

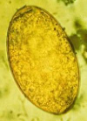
Fasciola Hepatica AKA Liver Fluke
Tx: Triclabendazole (Both stages), Closantel for adult
Sheep, cattle.


Paraphistomum Ichikawa AKA Stomach Flukes
Adults – Rumen & reticulum, Immature – Duodenum & abomasum
Cattle, sheep
Tx: OLY oxycloxanide or niclosamidme (immature)

Tapeworm
Taenia
SI
Canine, feline
Echniccocus identical to taenia
Tx: Praziquantel
- Infection
o Ingest RABBIT with cysticercus pisiformis larval stage
o No c/signs in DH
- Tx – Prazi, Epsiprantel, BZ
- Prevention – don’t feed offal to dog, work prazi every 6w (PPT longer than 6w)
- Tx puppies? No need, no txm via milk/placenta
- Sig for humans – none.

Anoplocephala Perfiolata
Ileo-caecal junction
Horse
Praziquantel

Moniezia Expansa – Triangular shape, Benedeni – Square shape
SI
Dipylidium Caninum
SI
Dogs, cat
Diarrhoea, constipation, anorexia, scooting
- Infection:
o Ingestion of flea IH – Ctenocephalides spp. (esp C. felis)
- Why infected if wormed?
o FenBZ Effective against nematodes, cestodes from Taenia spp
o Not against D. caninum
- Fleas feed on blood, how do they become infected?
o Flea larvae in env feed on proglottids, ingest eggs
o Eggs dvp into larve as fleas matures
o DH ingests fleas, pass proglottids
- Tx
o Praziquantel works well, or Epsiprantel
o Control fleas
- Prevention
o Flea control
- Human significance?
o Can mature in SI of humans, esp children


Spirometra Erinacei AKA Zipper Worm
SI
Cat, dog
Praziquantel
- Infection
o Ingest secondary IH - small vertebrates/amphibians
o or PH (snakes)
- c/signs
o weight loss, D+, V+, most no clinical signs
- Tx & prevention
o praziquantel 4x normal dose (but increasing dose increases BZ dose also)
o prazi chemo resistance does not seem to occur, but from a different order of cestodes
o PPT ~1month (treat monthly)
o prevent praying
- humans significance
o Can become infected with larval stages – causes Sparganosis (larvae in viscera)
o Inf for humans – water with copepods, raw/undercooked meat (frog, snake esp)
o Cutaneously – flesh of infected frog to ulcer/wound/sore eye
o HUMANS = PH


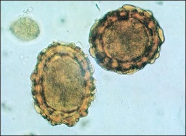
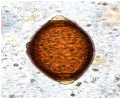
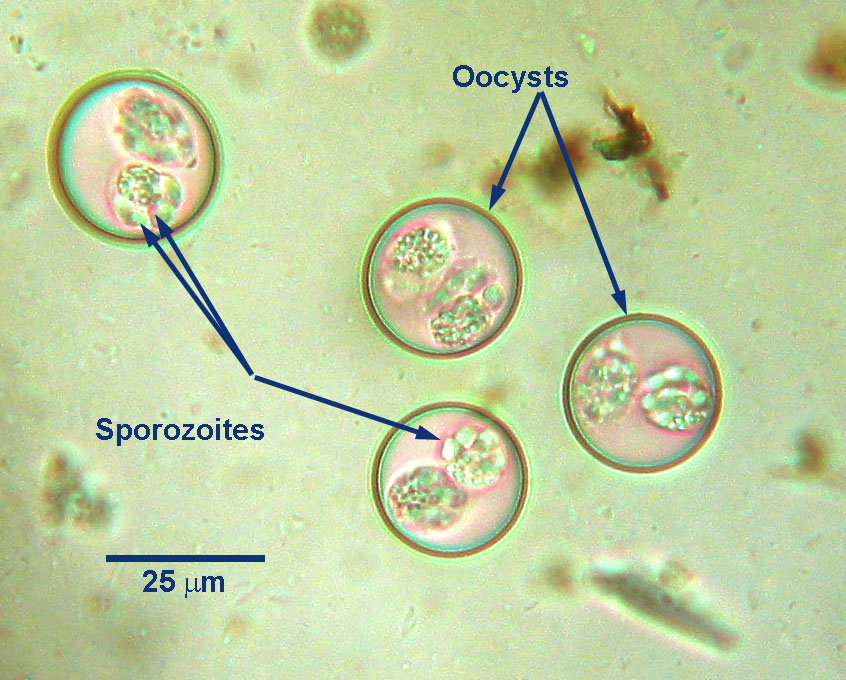
Eimeria AKA Coccidiosis
Cattle, sheep, chicken
Lower ileum, caecum, colon
Toltrazuril
- Why no clinical signs
o Usually seen in young animals or < immunity adults
- Infection
o Ingestion of sporulated oocysts or PH from env
- Tx?
o Treat, adults source of infection for puppies up to one year
o In puppies —> severe bloody D+, anaemia, V+, < weight, anorexia
o Oocysts an survive many months in env
- Tx
o Toltrazuril – isospora
- Prevent infection in puppies
o Oocysts resistant to most disinfectants in env
o Hygiene, remove faeces (before oocysts sporulate 12h, < overcrowding
o Steam sterilisation
o Treat with all wormer from 2wo, every 2w for 3m
Isospora AKA Cystoisospora
Pigs, dogs, cats
SI

Cryptosporidium Parvum
Dairy calves
Halofuginone

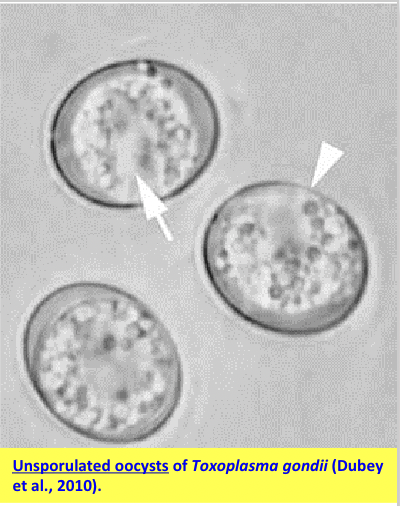
Toxoplasma Gondii
SI or any nucleated cell, can be IH for any animal
Definitive Hosts: Cats - intestinal + extreintestinal. Cats <1 year will produce greater no. of oocysts. Intestinal immunity in these cats.
Abortion, immunocompromised,
Liver: yellow/white foci of necrosis
Lungs: Oedema
CNS: nodular aggregates of macrophage, lymphocyte, neutrophil
Infx: sporulated oocysts, undercooked tissue cysts
Trachyzoite: Transplacental/Transfusion
Dx: Detection of oocysts in faeces of cats, Serology by ELISA, cytology
Tx: Toltrazuril, Clindamycin

Trichomonas Foetus

Paralysis Tick
Ixodes Holocyclus
- Lifecycle
o Three host tick
o Engorged F feeds 1-3w, drops off, lays eggs in env ~1m
o larvae attach to host, drop to ground, moult to nymph
- c/signs in animal
o due to engorged F tick – 1 tick can kill dog/cat.
o salivary neurotoxin (holocyclotoxin) during feeding flaccid paralysis
o inhibits Ach release
o toxin secreted after 3-5d of attachment
o clinical signs 3-5d after tick attachment – asc paralysis
o dyspnoea, cardiac failure, laryngeal mm paralysis (voice change)
- where to look
o all over body – head & shoulders most common (ant half of body)
- tick season
o August —> Feb (Spring – summer) – like temp 27C+
- What factors will influence distribution of this parasite?
o Humidity – eggs/ larvae sensitive to desiccation
o Stable bandicoot population
- Tx
o Remove ticks, tick clip, check 4-hourly (may be pinpoint sized)
o Administer tick anti-toxin if showing c/signs – graded on ambulation, resp
- Neutralises unbound toxin – most effective EARLY in disease
- Slow injection 1ml/kg IV
- Risk of TAS reaction – adrenaline, anti-histamines, corticosteroids
o Supportive therapy
- Oxygen – flow by, ventilator if progresses and owner willing
- Pleural effusion – frusemide
- Anxiolytics/ sedation – butorphanol
- IV fluids judiciously (pleural effusion)
- Prevention
o Tick prevention
- Advantage – just fleas, lice
- Bravecto 4-6m for ticks oral
- NG monthly
o Avoid animal in the bush, tick check after being in bush lands
o Summer peak tick season – TICK CHECK DAILY!!!!
- Look for engorged tick, or tick crater
- Human significance
o Can kill humans – 20 deaths in AUS!


Rhipicephalus Australis AKA Boophilus (Subgenus) AKA Cattle Tick
Transmits B. Bovis, B. bigemina, Anaplasma marginale


Sarcoptes Scabiei
- Infection
o Direct contact from infected animal – shelter common place
o Very contagious
o Indirect infection also possible
- How is it infected if on monthly ML + spinosad?
o Ivermectin only works on sarcoptes at high dose (risky)
o Spinosad – effective against fleas, not mites
o Contraindicated to admin – spinosad with high doses of ivermectin.
- Where to do skin scrape?
o Ear margins, elbows, hocks – hard to find
o Skin lesions – caused by hypersensitivity reaction, often scrape negative
- Faeces + enzymes secreted by parasites stimulate hypersensitivity reaction, responsible for skin lesions – intense pruritus, papules, erythema
- Dx methods
o Skin scrape – find mites and/or eggs
o Detect Ab by ELISA
o Response to Tx
o Pinnal-pedal reflex (poor specificity)
- Tx –
o ML (revolution, Advocate)
o afoxalaner (NG), or fluralaner (Bravecto)
- Sig for humans?
o Contagious to humans, but won’t complete life cycle


Notodres Cati
- Infection
o Direct contact with infected cat, indirect txm can occur
o Notoedric mange = very contagious
- Treatment
- Selamectin (revolution) – 2x monthly, successful but not registered for N. cati Treat all in contact cats


All species
Chorioptes Bovis


Otodectes Cynotis AKA Ear Mite
Cats, dogs
- Infection
o Direct contact – esp during nursin
o Indirect – can surivive in env 2w
- c/signs
Caused by hypersensitivity to saliva —> ITCHY
Eggs —> Embryonated egg —> Larvae
Tx: Selamectin, 1-2 monthly treatmentsRarely infests humans


Demodex Canis
Dogs, cats, cattle
- Where do parasites locate?
o In hair follicles and sebaceous glands
- Condition
o Juvenile onset generalised demodicosis
- Infection
o Direct prolonged contact with mother as neonate
o hereditary T cell defect in immune system involved in pathogenesis
- Pathogenesis
o Normal skin commensal
o Demodicosis = excessive multiplication of mites in skin due to immunodeficiency
o Can be juvenile or adult onset, localised or generalised (5+ body regions, 2+ limbs)
o Adult onset – immunocompromised, typically from underlying condition (hyperA, hypoT, DM, neoplasm, chronic stress, GC therapy)
- Tx – treat for 1 month beyond resolution of c/signs & 2 negative skin scrapes
o acaricides (amitraz) weekly
o Doramectin inj (weekly, off label)
o Nextgard - 2 week intervals (afoxalaner)
o + AB/antifungal – Tx 2ndary microbial component (broken skin barrier, likely)

Cheyletiella AKA Walking Dandruff
Cats, dogs


Haemtopinus Lice

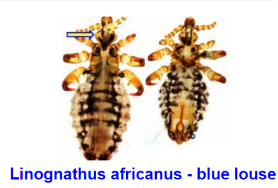
Linognathus

Bovicola Ovis

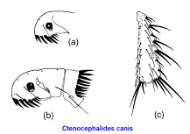
Ctenocephalides

Gastrophilus
Bot fly

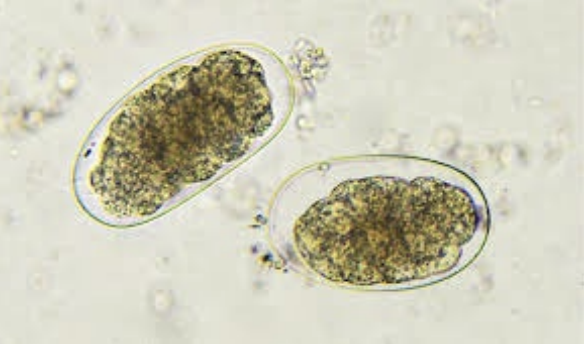
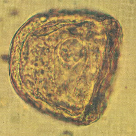
Giardia duodenalis
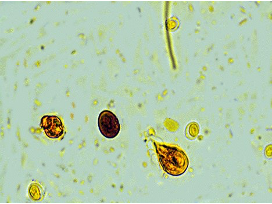
- Image
o Giardia trophozoite
o Oocysts
- Difficulties of Dx
o faecal floatation – solution destroys trophozoites, might see cysts
o shed intermittently – collect over 3d
o cysts – small numbers, small
o c/signs can precede cyst shedding by 1-2 days
o animals without c/signs can shed giardia in faeces
- Best Dx methods
o ZnSO4 centrifugal floatation
o Immunochromatography/lateral flow test (Snap test IDEXX)
o IFA (illuminates giardia)
- Infection
o Ingestion of cysts with water/food (trophozoites don’t survive long in env)
- Tx
o FenBZ, febantel – drontal wormer (febantel, pyrantel, prazi)
o Pyrantel not effective
- Sig for humans
o Dogs/cats play minor role in source of inf for humans
o carry some genotype that infects humans
Echinococcus Granulosus
- Infection of dog
o ingestion of offal (liver/lungs) from IH containing fertile cysts
o sheep, or wildlife most likely – many mammals are IH, including humans
- Control on farm
o Drontal (prazi, febantel, pyrantel)
o Treat dogs 5-6weekly, don’t feed offal (even cooked) or dead carcases
o Reduce stray population
o Don’t allow dogs into farm/ abattoir
o Educate farmer/dog owner
- Sig for humans
o Taenia spp in Aus – no significance
o Echinococcus – humans IH & DH
- Ingest eggs from infected dogs - Even manipulating coat (eggs adhere)
- Ingest food/water with egg
- Difference in infection E. granulosus v Taenia spp. for humans
o Eggs of echinococcus directly infective when shed in env for humans
o Eggs adhere to fur coat, can infect humans from patting
o Vs taenia – takes 2w for eggs to become infective, and by then broken down in env


Echidnophaga gallinacea
- Common host
o Birds – but can infest/feed on many species including dogs
o Fleas not host specific, LICE are.
- How does dog get infected
o Immature stagess – develop in env (like sandy soil)
o Dog – likely infected from env
- Tx
o ML, alfoxalaner, Imidacloprid, fipronil…
- Control infestation on farm – hygiene env, Tx poultry
o Free range poultry likely source of infestation – focus control on them
o Confine poultry, impervious floor
o Remove droppings regularly clean sheds
o Tx poultry (prethroids) regularly – whole flock together
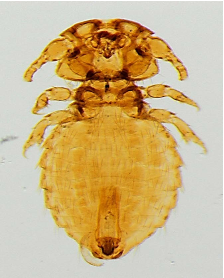
Trichodectes canis (biting lice)
- Infection in dogs
o Direct contact, can get indirectly from grooming equipment
- Tx (some options)
Selamectin
Fipronil
No sig for humans - lice are host specific

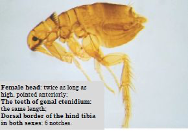
Ctenocephalides felis
Flea Allergy Dermatitis
- Dx made based on
o History – age of animal when clinical signs began, inconsistent flea Tx
o Clinical sins – scractching, chewing and licking
o Lesion distribution – dorsum
o Finding fleas & flea faeces on the body (fine toothed comb, many dogs/cats like them off)
o Finding D. caninum in faeces of host - IH for D. Caninum
o Response to flea treatment & intradermal testing
o Detection of specific Ab by ELISA
- Infection: From the environemnt
- Lesions – hypersenstivity reaction to Ag in saliva of fleas
- Design control program
o Treat dogs for fleas first – adulticides:
Selamectin (revolution), Simparica (sarolaner)
Bravecto (fluralaner), NG (Alfoxalaner)
Comfortis (spinosad)
Frontline (fipronil), Advantage (imidacloprid) – kills fleas & their larvae
Advocate (imidacloprid + moxidectin)
o Protocol for killing fleas
Kills adult fleas on dogs/ cats (rapid acting adulticide)
Eliminate immature stages from env (IGRs) – Lufenuron, methoprene
· Clean env
o educate pet owner – get fleas from the env
Treat all in contact animals – be consistent
Avoid untreated animals from entering home
Mechanical control – cleaning bedding, vacuum carpets etc
o Tx dogs for tapeworm
Epsiprantel, Praziquantel
o GC if dogs show intense pruritus
Contraindicated if concurrent bacterial infection