Maxillary Anesthesia Techniques
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
32 Terms
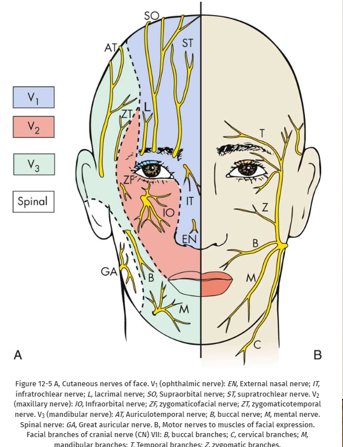
nerve anatomy in head and neck
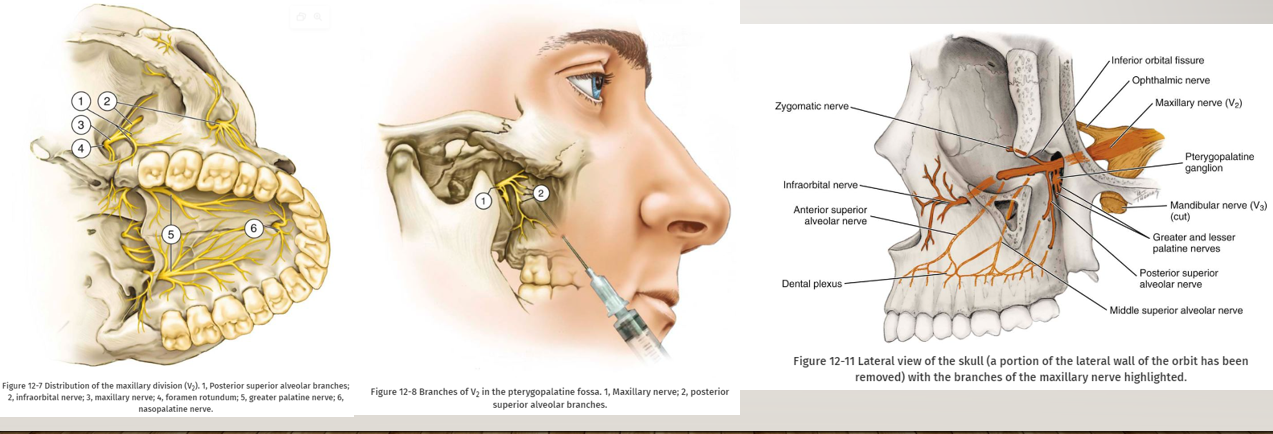
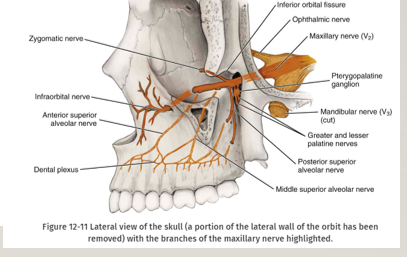
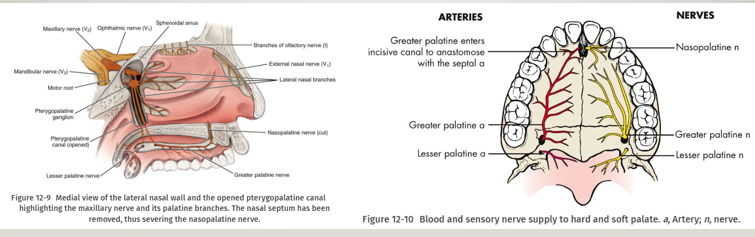
branches of the maxillary division (italicizes = special significance in dental pain control)
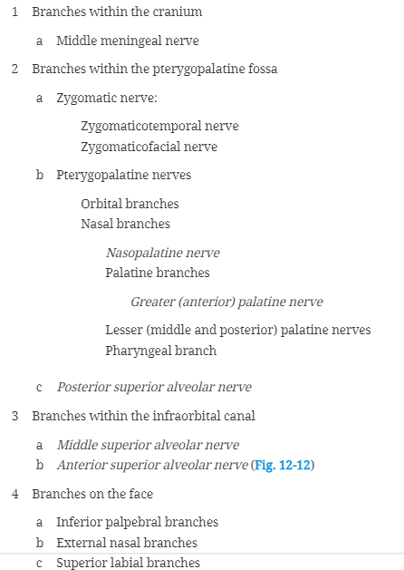
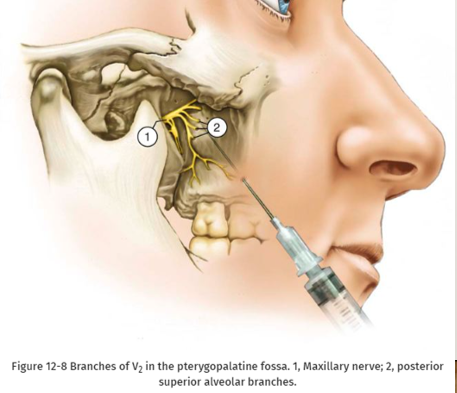
branches of V2 in pterygopalatine fossa
local infiltration
local infiltration- steps/info
-27-gauge needle is recommended
-area of insertion: height of the mucobuccal fold above the apex of the tooth being anesthetized
-target area: apical region of the tooth to be anesthetized
-landmarks: mucobuccal fold, crown of the tooth, root contour of the tooth
-orientation of the bevel: toward bone
-procedure: (see next flashcard)
-slowly withdraw the syringe
-make the needle safe
-wait 3-5 minutes before commencing the dental procedure
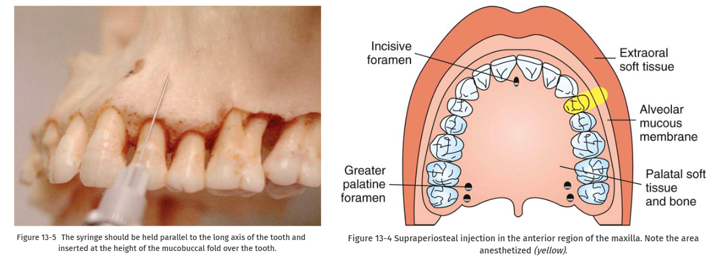
local infiltration procedure
-prepare tissue at injection site: clean with sterile dry gauze, apply topical antiseptic (optional), apply topical anesthetic for min. of 1 minute
-orient needle so bevel faces bone
-lift the lip, pulling the tissue taut
-hold the syringe parallel with the long axis of the tooth
-insert the needle into the height of the mucobuccal fold over the target tooth
-advance the needle until its bevel is at or above the apical region of the tooth; in most instances, depth of penetration is only a few mm; because the needle is in soft tissue (not touching bone), there should be no resistance to its advancement nor should there be any pt discomfort
-aspirate x2
-if aspiration negative, deposit approximately 0.6mL (1/3 of a cartridge) slowly over 20 seconds- do not allow tissues to balloon
posterior superior alveolar block (PSA block)
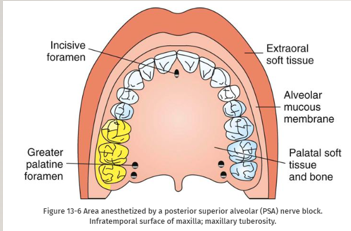
PSA block- areas anesthetized
-pulps of the maxillary third, second, and first molars (entire tooth = 72%, MB root of the maxillary first molar not anesthetized = 28%)
-buccal periodontium and bone overlying these teeth
-***second injection necessary for treatment of the first molar (MB root) in 28% of pts→infiltration as second injection
PSA block- disadvantages
-risk of hematoma, which is usually diffuse, also discomfiting and visually embarrassing to the pt
-technique somewhat arbitrary: no bony landmarks during insertion
-second injection necessary for treatment of the first molar (MB root) in 28% of pts
PSA block technique
-27-gauge short needle recommended
-area of insertion: height of the mucobuccal fold above the maxillary second molar
-target area: PSA nerve- posterior, superior, and medial to the posterior border of the maxilla
-landmarks: mucobuccal fold, maxillary tuberosity, zygomatic process of the maxilla
-orientation of the bevel: toward bone during the injection; if bone is accidentally touched, the sensation is less unpleasant
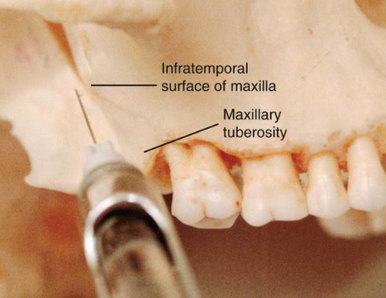
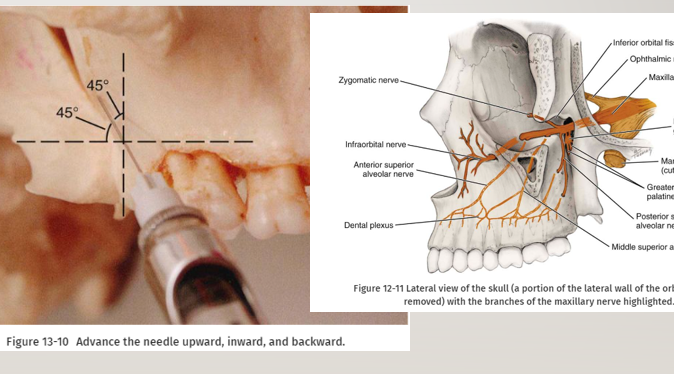
PSA block procedure
-assume correct position: for left PSA nerve block- sit at the 10 o’clock position facing the patient, for right PSA block- sit at 8 o’clock position facing the patient
-prepare the tissues at the height of the mucobuccal fold for penetration: dry with sterile gauze, apply a topical antiseptic (optional), apply topical anesthetic for a minimum of 1 minute
-orient the bevel of the needle toward bone
-partially open the patient’s mouth, pulling the mandible to the side of injection
-retract the pt’s cheek with instrument (for visibility)
-pull the tissues at the injection site taut
-insert the needle into the height of the mucobuccal fold over the second molar
-advance the needle slowly in an upward, inward, and backward direction in one movement
-slowly advance the needle through soft tissue- should be no resistance and no discomfort to pt, if resistance is felt the angle of the needle in toward the midline is too great (withdraw the needle slightly and bring the syringe barrel closer to the occlusal plane, readvance needle)
-advance needle to desired depth: adult- 16mm (1/2 of short needle), 10-14mm for smaller adults and children
-aspirate in 2 planes
-if both aspirations negative: slowly deposit 0.9-1.8mL of anesthetic solution over 30-60 seconds, aspirate several additional times during drug administration
-slowly withdraw syringe
-make the needle safe
-wait minimum of 3-5min before commencing the dental procedure
PSA block complications
-hematoma: commonly produced by inserting the needle too far posteriorly into the pterygoid plexus of veins; maxillary artery may be perforated; use of short needle minimizes the risk of pterygoid plexus puncture
-visible intraoral hematoma develops within several minutes, usually noted in the buccal tissues of the mandibular region- bleeding continues until the pressure of extravascular blood is equal to or greater than that of intravascular blood; there is no easily accessible intraoral area to which pressure can be applied to stop the hemorrhage
-mandibular anesthesia: deposition of LA lateral to the desired location may produce varying degrees of mandibular anesthesia; most often, pts mention that their tongue and lower lip are anesthetized since the mandibular division of V3 is located lateral to the PSA nerve
middle superior alveolar artery block
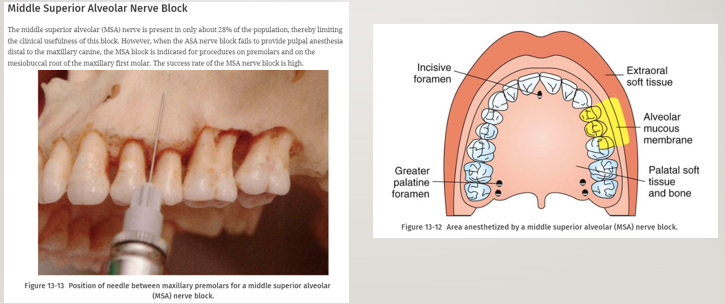
middle superior alveolar artery block steps
-27-gauge short or long needle recommended
-area of insertion: height of the mucobuccal fold above the maxillary second premolar
-target area: maxillary bone above the apex of the maxillary second premolar (a little higher than infiltration point)
-landmark: mucobuccal fold above the maxillary second premolar
-orientation of the bevel: toward bone
middle superior alveolar artery block- procedure
-assume correct position: for right MSA nerve block- 10 o’clock, for left MSA nerve block- 8 or 9 o’clock
-prepare tissue at site of injection
-stretch the pt’s upper lip to make the tissues taut and to gain visibility
-insert the needle into the height of the mucobuccal fold above the second premolar with the bevel directed toward bone
-penetrate the mucous membrane and slowly advance the needle until its tip is located well above the apex of the second premolar
-aspirate
-slowly deposit 0.9-1.2mL (1/2-2/3 cartridge) of solution
-withdraw the syringe
-make the needle safe
-wait 3-5min minimum before commencing dental therapy
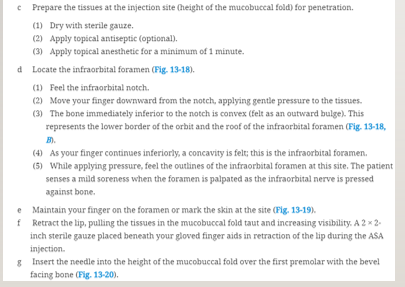
infraorbital nerve block, anterior superior alveolar block- nerves anesthetized
-anterior superior alveolar
-middle superior alveolar
-infraorbital: inferior palpebral, lateral nasal, superior labial
-ASA nerve block not the same as the infraorbital nerve block- infraorbital anesthetizes soft tissues of the anterior portion of the face, not the teeth or intraoral soft and hard tissues
infraorbital nerve block- areas anesthetized
-pulps of the maxillary central incisor through the canine on the injected side
-in about 72% of pts, pulps of the maxillary premolars and mesiobuccal root of the first molar
-buccal (labial) periodontium and bone of those same teeth
-lower eyelid, lateral aspect of nose, upper lip
infraorbital nerve block- indications
-dental procedures involving more than 2 maxillary teeth and their overlying buccal tissues
-inflammation or infection (which contraindicates supraperiosteal injection): if a cellulitis is present, the maxillary nerve block may be indicated in lieu of the ASA nerve block
-when supraperiosteal injections have been ineffective because of dense cortical bone
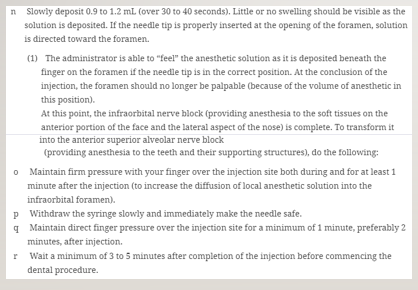
infraorbital nerve block technique
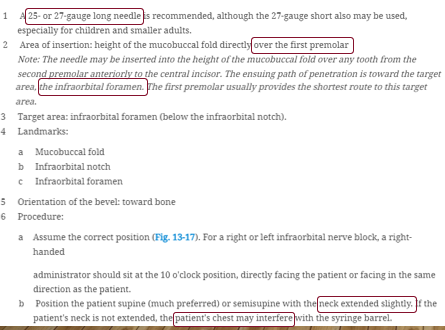
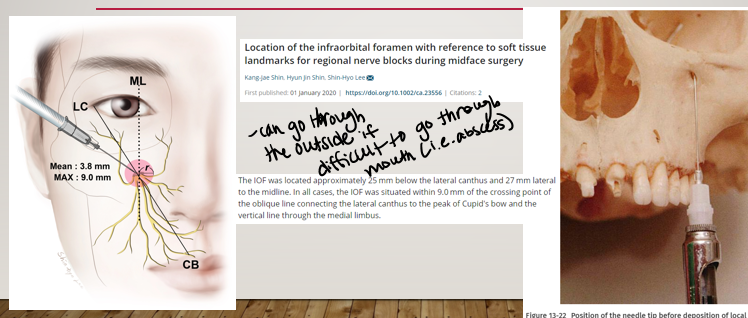
infraorbital block- procedure continued
infraorbital block- continued
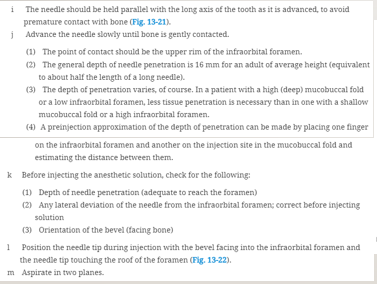
infraorbital block- final steps
infraorbital nerve block- going through the outside
greater palatine, nasopalatine nerve blocks
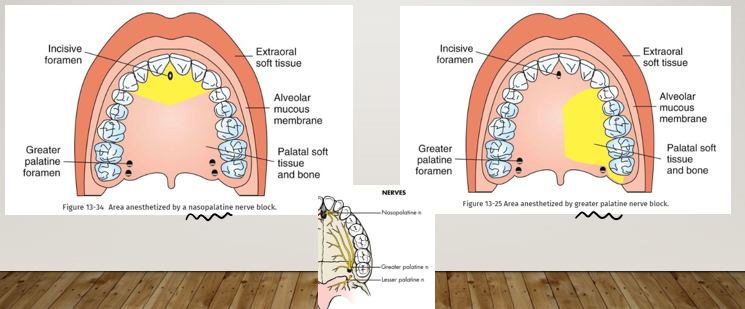
anesthetized areas- greater palatine and nasopalatine nerve blocks
greater palatine nerve block- steps
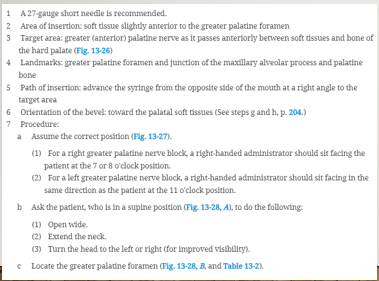
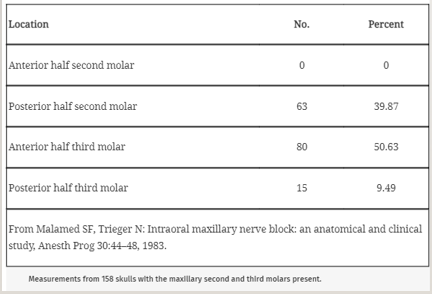
greater palatine nerve block- procedure
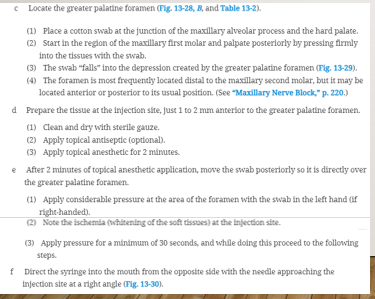
greater palatine nerve block- procedure continued
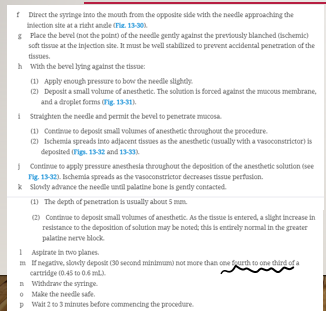
****greater palatine nerve block locations and percentages
nasopalatine nerve block- procedure
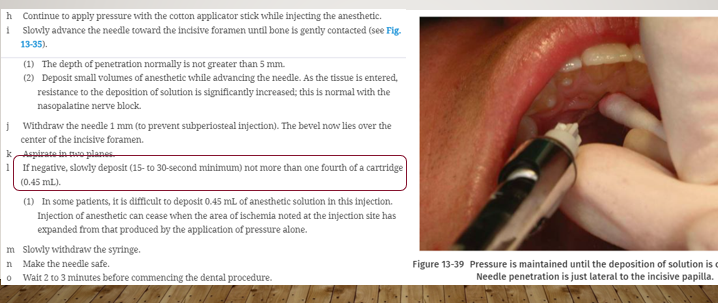
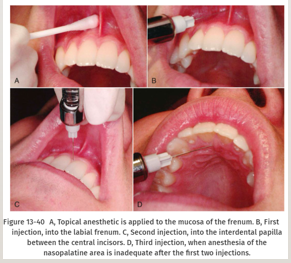
nasopalatine nerve block alternative
-patients appreciate this- less painful, good to do in kids
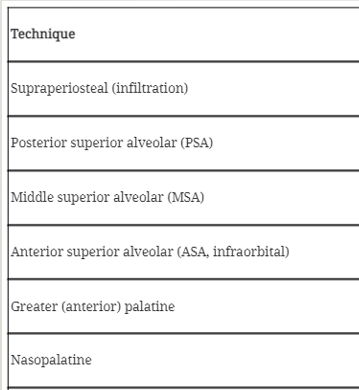
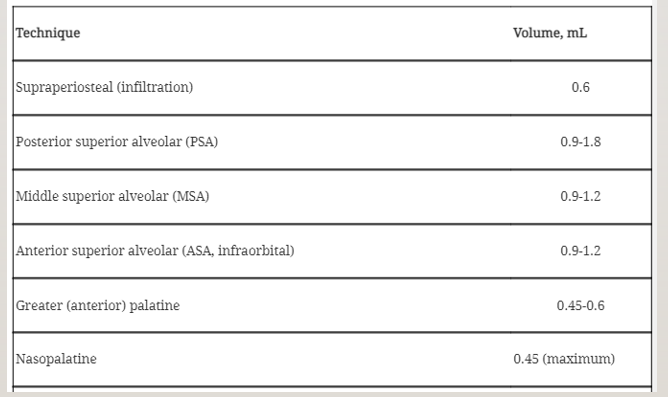
technique, volume