Serology BOC
1/531
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
532 Terms
1. Antinuclear antibody tests are performed to help diagnose?
A) acute leukemia
B) lupus erythematosus
C) hemolytic anemia
D) Crohn disease
B) lupus erythematosus
2. in the anti-double stranded DNA procedure, the antigen most commonly utilized is
a. rat stomach tissue
b. mouse kidney tissue
c. Crithidia luciliae
d. Toxoplasma gondii
c. Crithidia luciliae
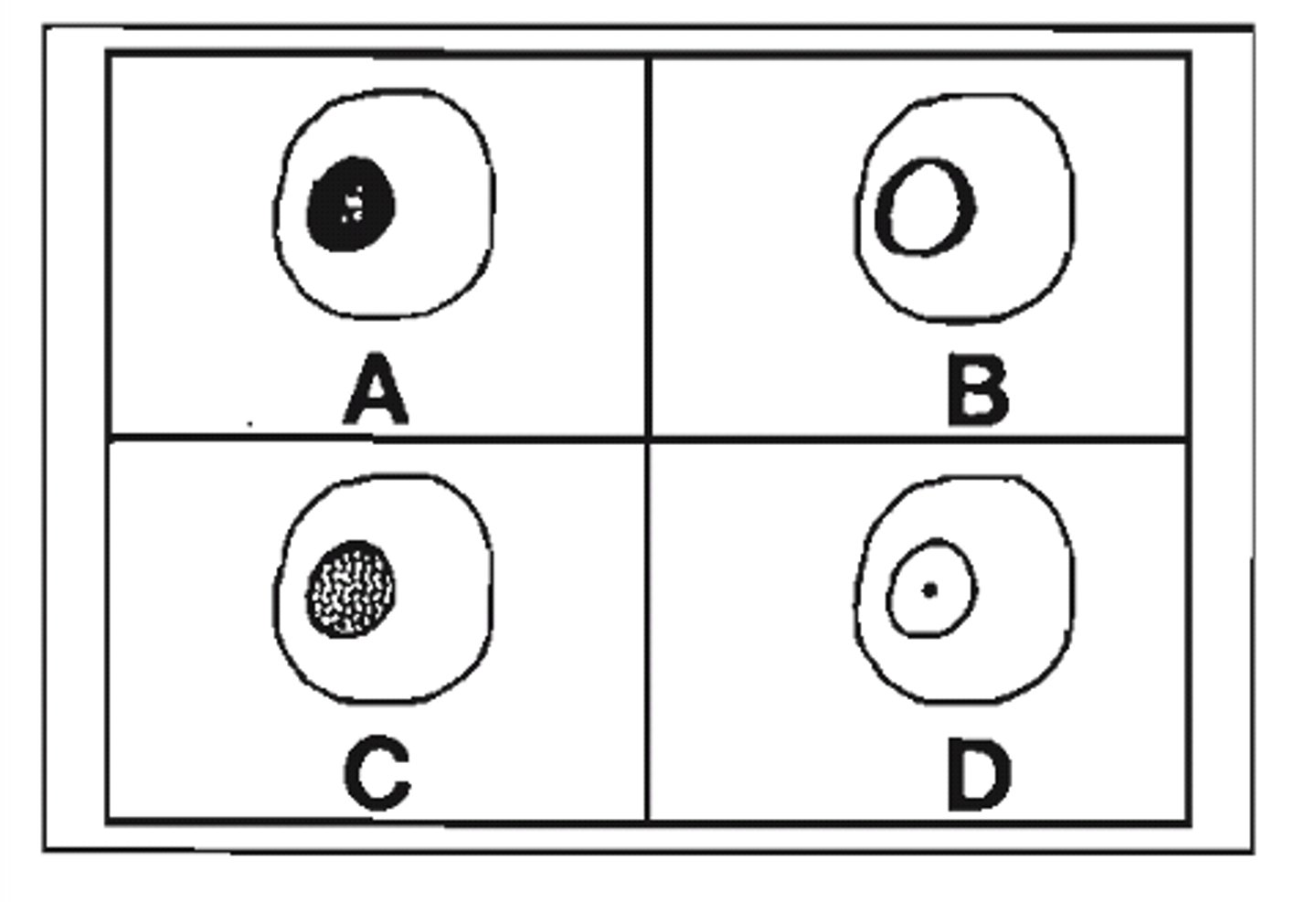
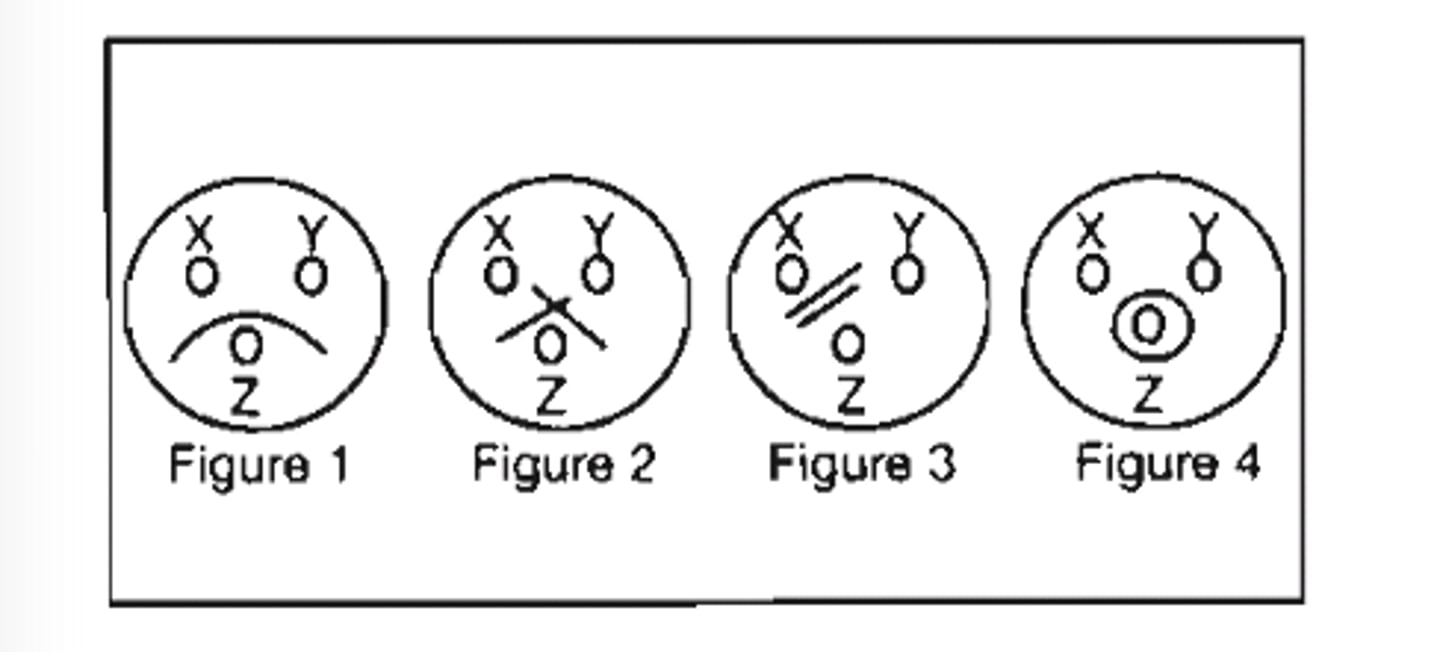
3. (see pic) refer to the following illustration. which of teh ANA patterns shown above would be associated with high titers of antibodies to the Sm antigen?
a. diagram A
b. diagram B
c. diagram C
d. diagram D
c. diagram C
4. Sera to be tested for IFA-ANA 6 days after drawing is best stored at?
A) room temperature
B) 5°C +/- 2°
C) -70°C in a constant temperature freezer
D) -20°C in a frost-free self-defrosting freezer
C) -70°C in a constant temperature freezer
5. Antibodies directed at native DNA are most frequently associated with which pattern of fluorescence in the IFA-ANA test?
A) rim
B) diffuse
C) speckled
D) centromere
A) rim
6. The technologist observes apparent homogenous staining of the nucleus of interphase cells while performing an IFA-ANA, as well as staining of the chromosomes in mitotic cells. This result is:
A) indicative of 2 antibodies, which should be separately reported after titration
B) expected for anti-DNA antibodies
C) inconsistent; the test should be reported with new reagent
D) expected for anti-centromere antibodies
B) expected for anti-DNA antibodies
7. The result of an anti-nuclear antibody test was a titer of 1:320 with a peripheral pattern. Which of the following sets of results best correlate with these results?
A) anti-dsDNA titer 1:80, and a high titer of antibodies to Sm
B) antimitochondrial antibody titer 1:160, and antibodies to RNP
C) anti-Scl-70, and antibodies to single-stranded DNA
D) high titers of anti-SS-A and anti-SS-B
A) anti-dsDNA titer 1:80, and a high titer of antibodies to Sm
8. Systemic lupus erythematosus patients often have which of the following test results?
A) high titers of DNA antibody
B) decreased serum immunoglobulin levels
C) high titers of anti-smooth muscle antibodies
D) high titers of antimitochondrial antibody
A) high titers of DNA antibody
9. Systemic lupus erythematosus patients with active disease often have which of the following test results?
a. high titers of antimicrosomal antibodies
b. high titers of anti-smooth muscle antibodies
c. marked decrease in serum CH50
d. decreased serum immunoglobulin levels
c. marked decrease in serum CH50
10. which of the following is decreased in serum during the active stages of systemic lupus erythematosus?
a. anti nuclear antibody
b. immune complexes
c. complement C3
d. anti DNA
c. complement C3
11. A positive ANA with the pattern of anticentromere antibodies is most frequently seen in patients with:
a. rheumatoid arthritis
b. systemic lupus erythematosus
c. CREST syndrome
d. Sjӧgren syndrome
c. CREST syndrome
12. In the indirect fluorescent anti-nuclear antibody test, a homogenous pattern indicates the presence of antibody to:
a. RNP
b. Sm
c. RNA
d. DNA
d. DNA
13. In the indirect fluorescent anti-nuclear antibody test, a speckled pattern may indicate the presence of antibody to:
a. histone
b. Sm
c. RNA
d. DNA
b. Sm
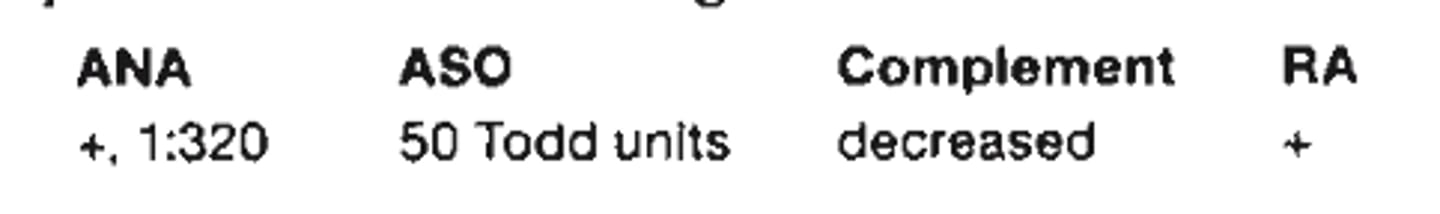
14. (see pic) a patient has the following test results. the above results could be seen in patients with
a. rheumatic fever
b. rheumatoid arthritis
c. lupus erythematosus
d. glomerulonephritis
c. lupus erythematosus
15. Autoantibodies in the absence of Sm are found in patients with:
a. mixed connective tissue disease
b. systemic lupus erythematosus
c. Crohn disease
d. multiple myeloma
a. mixed connective tissue disease
16. to make a presumptive diagnosis of rheumatoid arthritis, which of the following qualitative methods is most sensitive?
a. latex agglutination
b. immunoelectrophoresis
c. RID
d. ELISA
a. latex agglutination
17. Rheumatoid factor reacts with:
A) inert substances such as latex
B) Rh-pos erythrocytes
C) kinetoplasts of Crithidia luciliae
D) gamma globulin-coated particles
D) gamma globulin-coated particles
18. A consistently and repeatedly negative IFA-ANA is:
A) strong evidence against untreated SLE
B) associated with active SLE
C) characteristic of SLE with renal involvement
D) associated with lupus inhibitor
A) strong evidence against untreated SLE
19. Positive rheumatoid factor is generally associated with:
A) hyperglobulinemia
B) anemia
C) decreased erythrocyte sedimentation rate
D) azotemia
A) hyperglobulinemia
20. The following results are from rubella titer performed on acute and convalescent sera using 2-fold serial dilution:
Date tested- 1/23/04
Acute serum titer- 1:8
Convalescent serum titer- 1:32
After evaluating the above results, best interpretation is:
A) results are consistent with active infection with rubella
B) variation in the acute serum titers invalidates these results
C) test should be repeated by a different technologist
D) patient was not infected with rubella
A) results are consistent with active infection with rubella
21. Rheumatoid factors are immunoglobulins with specificitiy for allotypic determinants located on the:
A) Fc fragment of IgG
B) Fab fragment of IgG
C) J chain of IgM
D) secretory of component of IgA
A) Fc fragment of IgG
22. Rheumatoid factor in patients serum may cause a false:
A) positive test for the detection of IgM class antibodies
B) negative test for the detection of IgM class antibodies
C) positive test for the detection of IgG class antibodies
D) negative test for the detection of IgG class antibodies
A) positive test for the detection of IgM class antibodies
23. Rheumatoid factors are defined as:
A) antigens found in the sera of patients with rheumatoid arthritis
B) identical to the rheumatoid arthritis precipitin
C) autoantibodies with spicificity for the Fc portion of the immunoglobulin (IgG) molecule
D) capable of forming circulating immune complexes only when IgM-type autoantibody is present
C) autoantibodies with spicificity for the Fc portion of the immunoglobulin (IgG) molecule
24. Tissue injury in systemic rheumatic disorders such as systemic lupus erythematosus is thought to be caused by:
a. Cytotoxic T cells
b. IgE activity
c. deposition of immune complexes
d. cytolytic antibodies
c. deposition of immune complexes
25. False-positive rheumatoid factor in agglutination and nephelometric methods can be due to elevated levels of:
a. cryoglobulin
b. histidine-rich-glycoprotein
c. aspartame
d. C1q
d. C1q
26. An acute phase protein that binds to the membrane of certain microorganisms and activates the complements system is:
a. C-reactive protein
b. tumor necrosis factor alpha
c. neutrophils
d. kinins
a. C-reactive protein
27. High titers of antimicrosomal antibodies are most often found in:
A) rheumatoid arthritis
B) systemic lupus erythematosus
C) chronic hepatitis
D) thyroid disease
D) thyroid disease
28. which of the following is an organ-specific autoimmune disease?
a. myasthenia gravis
b. rheumatoid arthritis
c. addison disease
d. progressive systemic sclerosis
c. addison disease
29. In chronic active hepatitis, high titers of which of the following antibodies are seen?
A) antimitochondrial
B) anti-smooth muscle
C) anti-DNA
D) anti-parietal cell
B) anti-smooth muscle
30. In primary biliary cirrhosis, which of the following antibodies is seen in high titers?
a. antimitochondrial
b. anti-smooth muscle
c. anti-DNA
d. anti-parietal cell
a. antimitochondrial
31. Anti-RNA antibodies are often present in individuals having an anti-nuclear antibody immunoflurorescent pattern that is:
A) speckled
B) rim
C) diffuse
D) nucleolar
D) nucleolar
32. Anti-extractable nuclear antigens are most likely associated with which of the following anti-nuclear antibody immunofluorescent patterns?
A) speckled
B) rim
C) diffuse
D) nucleolar
A) speckled
33. In an anti-nuclear antibody indirect immunofluorescent test, a sample of patient serum shows a postive, speckled pattern. Which would be the most appropriate additional test to perform?
A) antimitochondrial antibody
B) immunoglobulin quantitation
C) screen for Sm and RNP antibodies
D) anti-DNA antibody using C luciliae
C) screen for Sm and RNP antibodies
34. Anti-glomerular basement membrane antibody is most often associated with this condition:
a. systemic lupus erythematosus
b. celiac disease
c. chronic active hepatitis
d. Goodpasture disease
d. Goodpasture disease
35. A 25-year-old woman is seen by a physician because of Raynaud phenomenon, myalgias, arthralgias and difficulty in swallowing. There is no evidence of renal disease. An ANA titer is 1:5120 with a speckled pattern with mitotic. Which of the following are also likely to be found in this patient?
a. high-level nDNA antibody and a low CH50 level
b. high-level Sm antibody
c. high-level rheumatoid factor
d. high-level ribonucleoprotein (RNP) antibody
d. high-level ribonucleoprotein (RNP) antibody
36. In pernicious anemia, which of the following antibodies is characteristically detected?
a. antimitochondrial
b. anti-smooth muscle
c. anti-DNA
d. anti-parietal cell
d. anti-parietal cell
37. Anti-phospholipid antibodies associated with autoimmune disorders tend to have immunoglobulin (IgG) that belongs to which of the following subclasses?
a. IgG1 and IgG3
b. IgG2 and IgG4
c. IgG1 and IgG4
d. IgG2 and IgG3
b. IgG2 and IgG4
38. The IIF staining pattern on ethanol-fixed leukocytes slides shows a perinuclear or nuclear staining pattern. This pattern is typically due to:
a. C-ANCA
b. LKM
c. P-ANCA
d. GBM
c. P-ANCA
39. The specificity of an immunoassay is determined by the:
a. label used on the antigen
b. method used to separate the bound from free antigen
c. antibody used in the assay
d. concentration of unlabeled antigen
c. antibody used in the assay
40. in assessing the usefulness of a new laboratory test, sensitivity is defined as the percentage of
a. positive specimens correctly identified
b. false positive specimens
c. negative specimens correctly identified
d. false negative specimens
a. positive specimens correctly identified
41. In the indirect immunofluorescence method of antibody detection in patient serum, the labeled antibody is:
A) human anti-goat immunoglobulin
B) rheumatoid factor
C) goat anti-human immunoglobulin
D) complement
A) human anti-goat immunoglobulin
42. which of the following describes an antigen antibody reaction?
a. the reaction is reversible
b. the reaction is the same as a chemical reaction
c. a lattice is formed at prozone
d. a lattice is formed at postzone
a. the reaction is reversible
43. the most common label in direct fluorescent antibody technique (DFA) is
a. alkaline phosphatase
b. horseradish peroxidase
c. fluorescein isothiocyanate
d. calcofluor white
c. fluorescein isothiocyanate
44. A substrate if first exposed to a patients serum, then after washing, anti-human immunoglobulin labeled with a fluorochrome is added. The procedure described is:
A) fluorescent quenching
B) direct fluorescence
C) indirect fluorescence
D) fluorescence inhibition
C) indirect fluorescence
45. Avidity may be defined as the:
A) degree of hemolysis
B) titer of an antigen
C) dilution of an antibody
D) strength of a reacting antibody
D) strength of a reacting antibody
46. In the interpretation of aggutination tests for febrile diseases, which of the following is of the greatest diagnostic importance?
A) anamnestic reactions caused by the heterologous antigens
B) rise in titer of the patient's serum
C) history of previous vaccination
D) naturally occurring antibodies prevalent where the disease is endemic
B) rise in titer of the patient's serum
47. Cholesterol is added to the antigen used in flocculation tests for syphilis to:
A) destroy tissue impurities present in the alcoholic beef heart extract
B) sensitize the sheep RBCs
C) decrease specificity of the antigen
D) increase sensitivity of the antigen
D) increase sensitivity of the antigen
48. The strength of a visible reaction is known as:
A) prozone reaction
B) absorption
C) avidity
D) elution
C) avidity
49. which of the following describes an antigen antibody precipitation reaction of non identity?
a. precipitin lines cross, forming double spurs
b. precipitin lines fuse, forming a single spur
c. no precipitin lines are formed
d. precipitin lines fuse, forming a single arc
a. precipitin lines cross, forming double spurs
50. Which test has the greatest sensitivity for antigen detection?
A) precipitin
B) agglutination
C) ELISA
D) complement fixation
C) ELISA
51. Excess antigen in precipitation gel reactions will:
A) have no effect on the precipitate reaction
B) not dissolve precipitate after formation
C) enhance the precipitate reaction
D) dissolve the precipitate after formation
D) dissolve the precipitate after formation
52. Soluble immune complexes are formed under the condition of:
A) antigen deficiency
B) antigen excess
C) antibody excess
D) complement
B) antigen excess
53. The visible serological reaction between soluble antigen and its specific antibody is:
A) sensitization
B) precipitation
C) agglutination
D) opsonization
B) precipitation
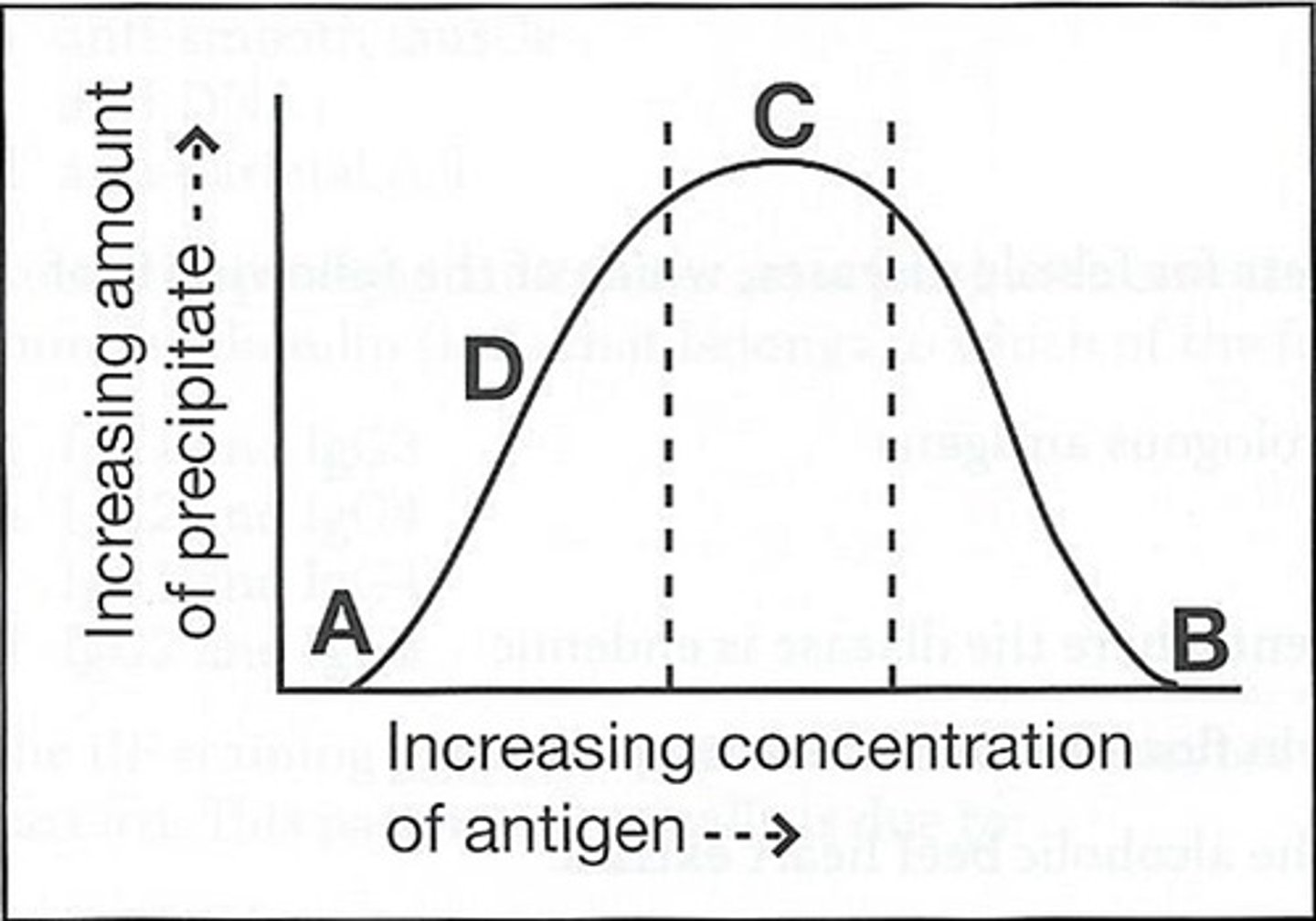
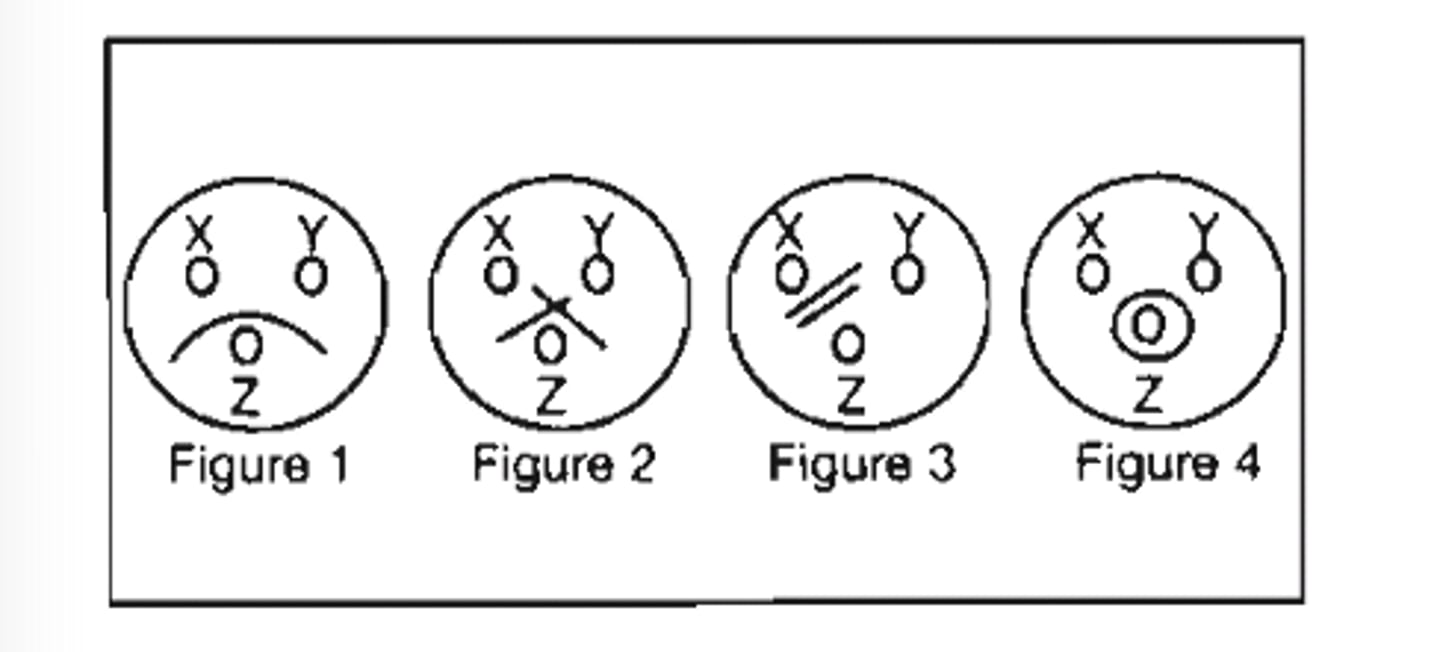
54) (see pic)The curve below was obtained by adding increasing amounts of a soluble antigen to fixed volumes of monospecific antiserum:
The area on the curve for equivalence precipitate is:
a. A
b. B
c. C
d. D
c. C
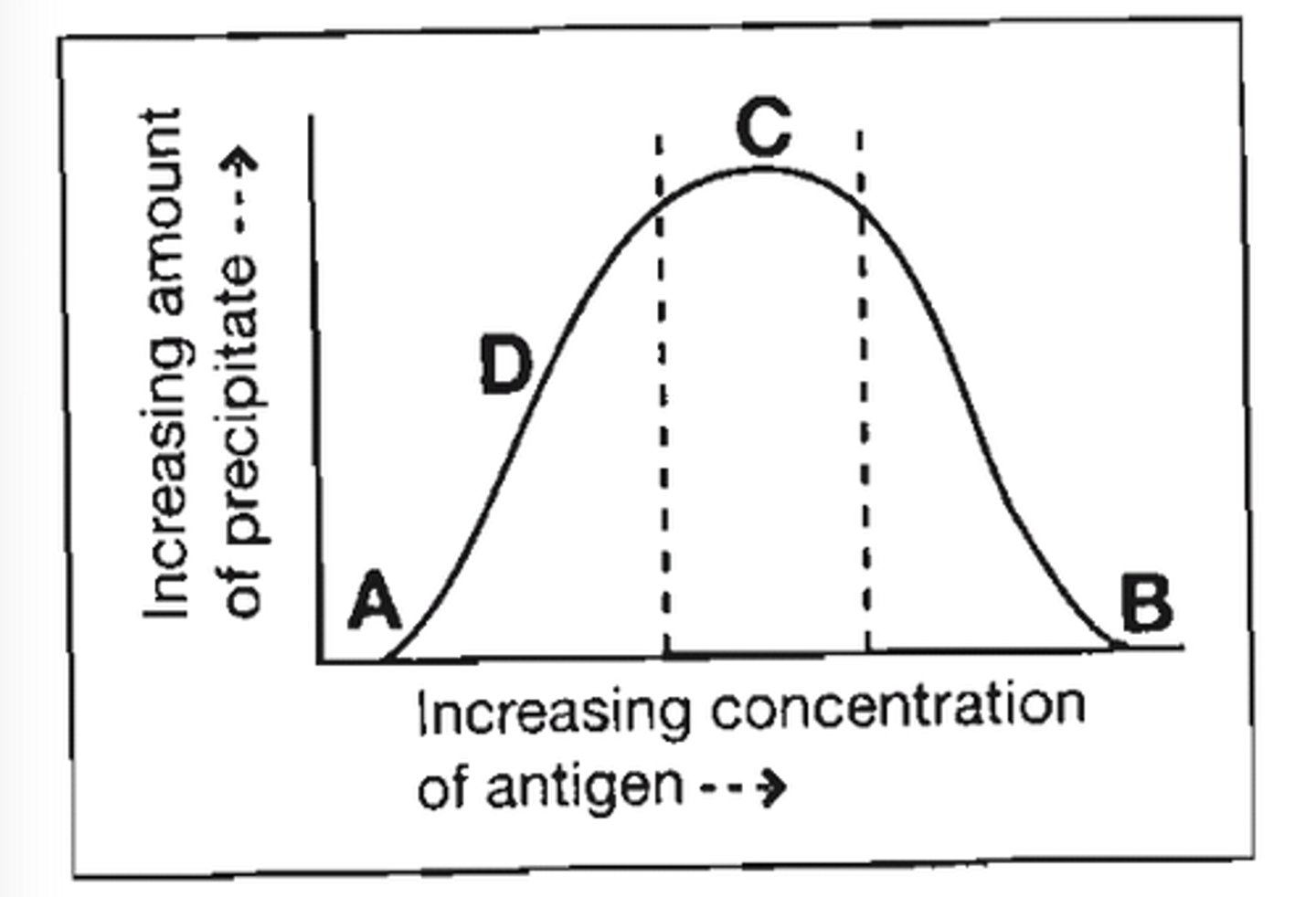
55) (see pic) The curve below was obtained by adding increasing amounts of a soluble antigen to fixed volumes of monospecific antiserum:
The area on the curve where no precipitate formed due to antigen excess is:
a. A
b. B
c. C
d. D
b. B
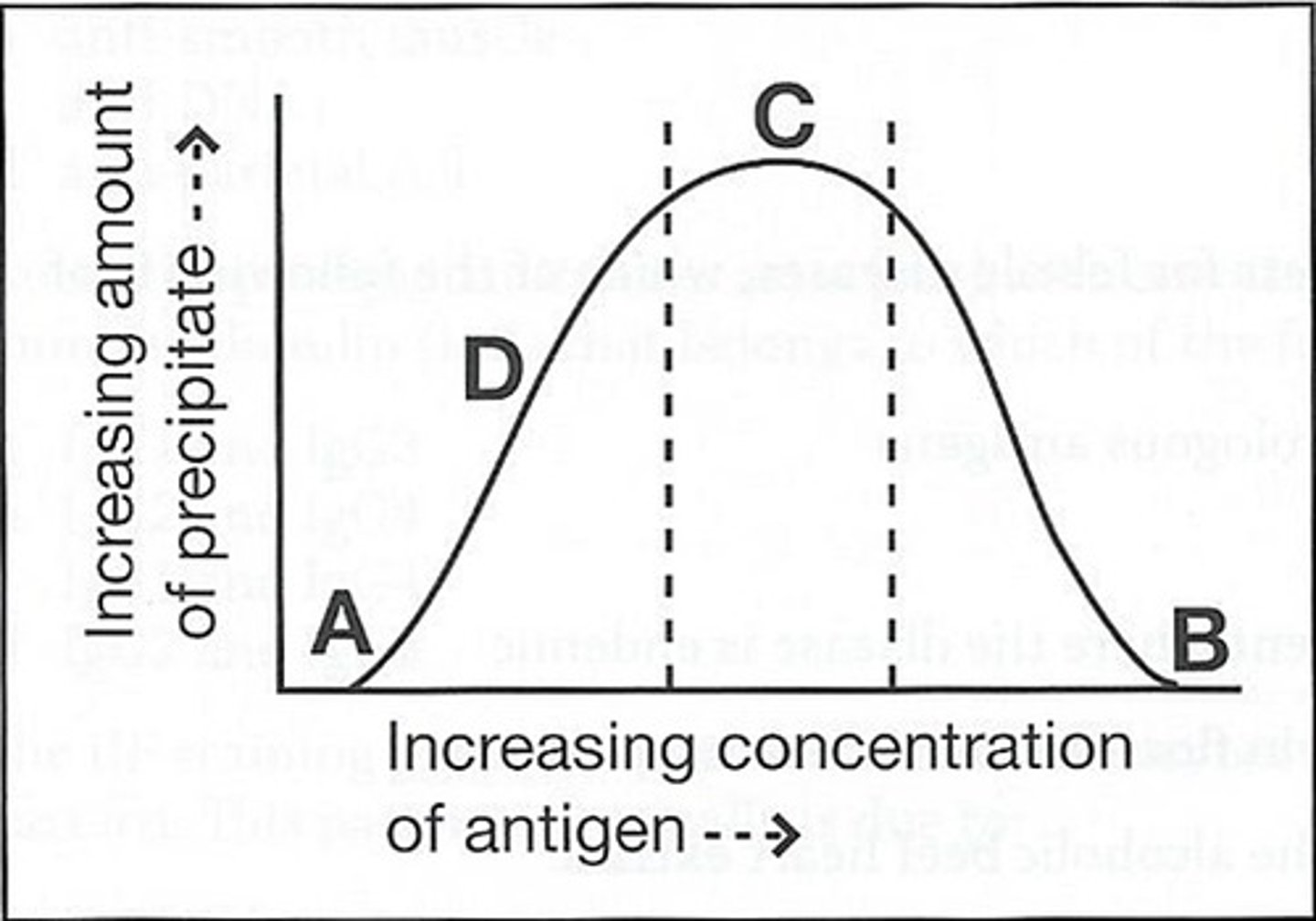
56) The curve below was obtained by adding increasing amounts of a soluble antigen to fixed volumes of monospecific antiserum:
The area on the curve for prozone is:
a. A
b. B
c. C
d. D
a. A
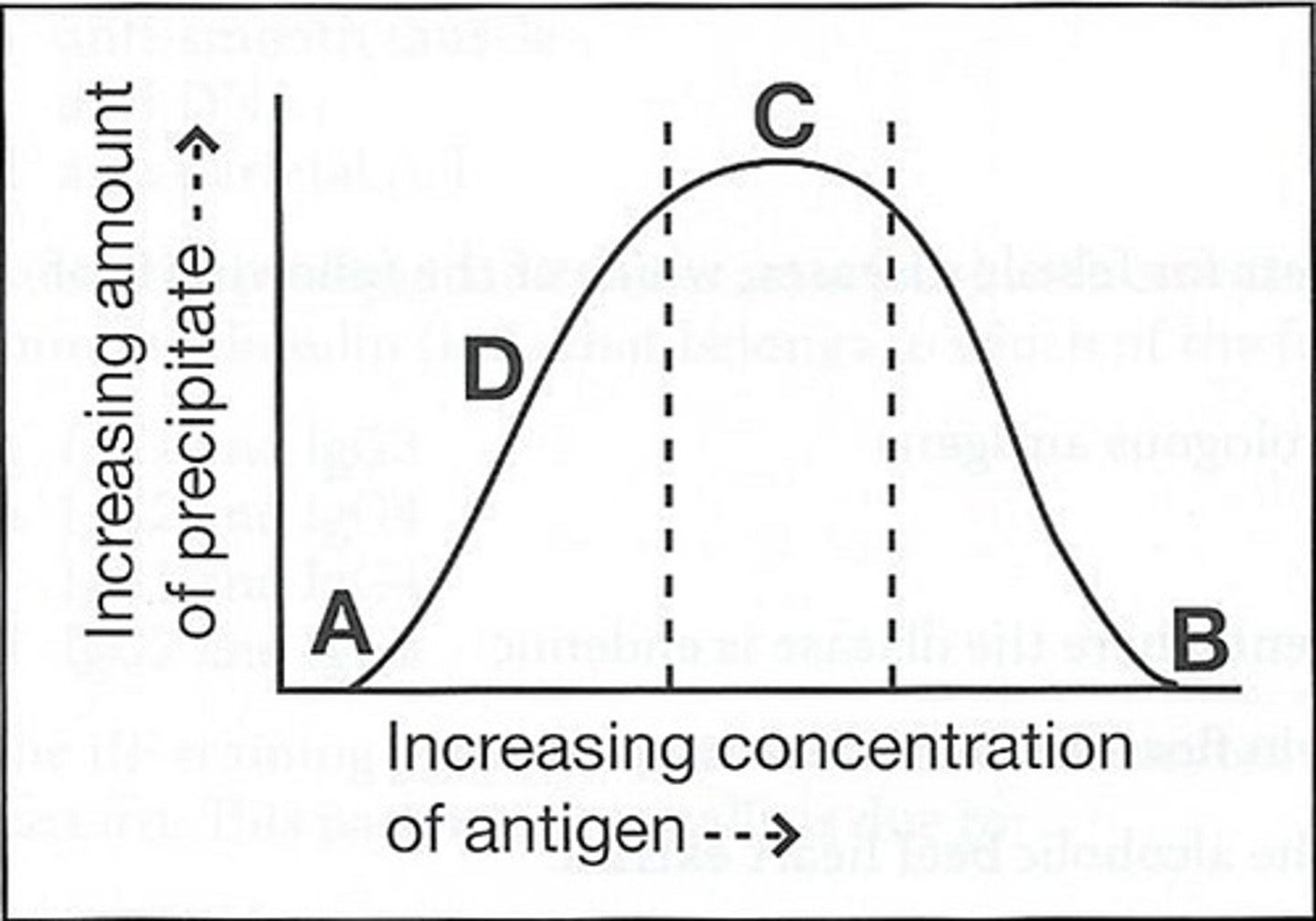
57) The curve below was obtained by adding increasing amounts of a soluble antigen to fixed volumes of monospecific antiserum:
The area on the curve where soluble antigen-antibody complexes have begun to form is:
a. A
b. B
c. C
d. D
d. D
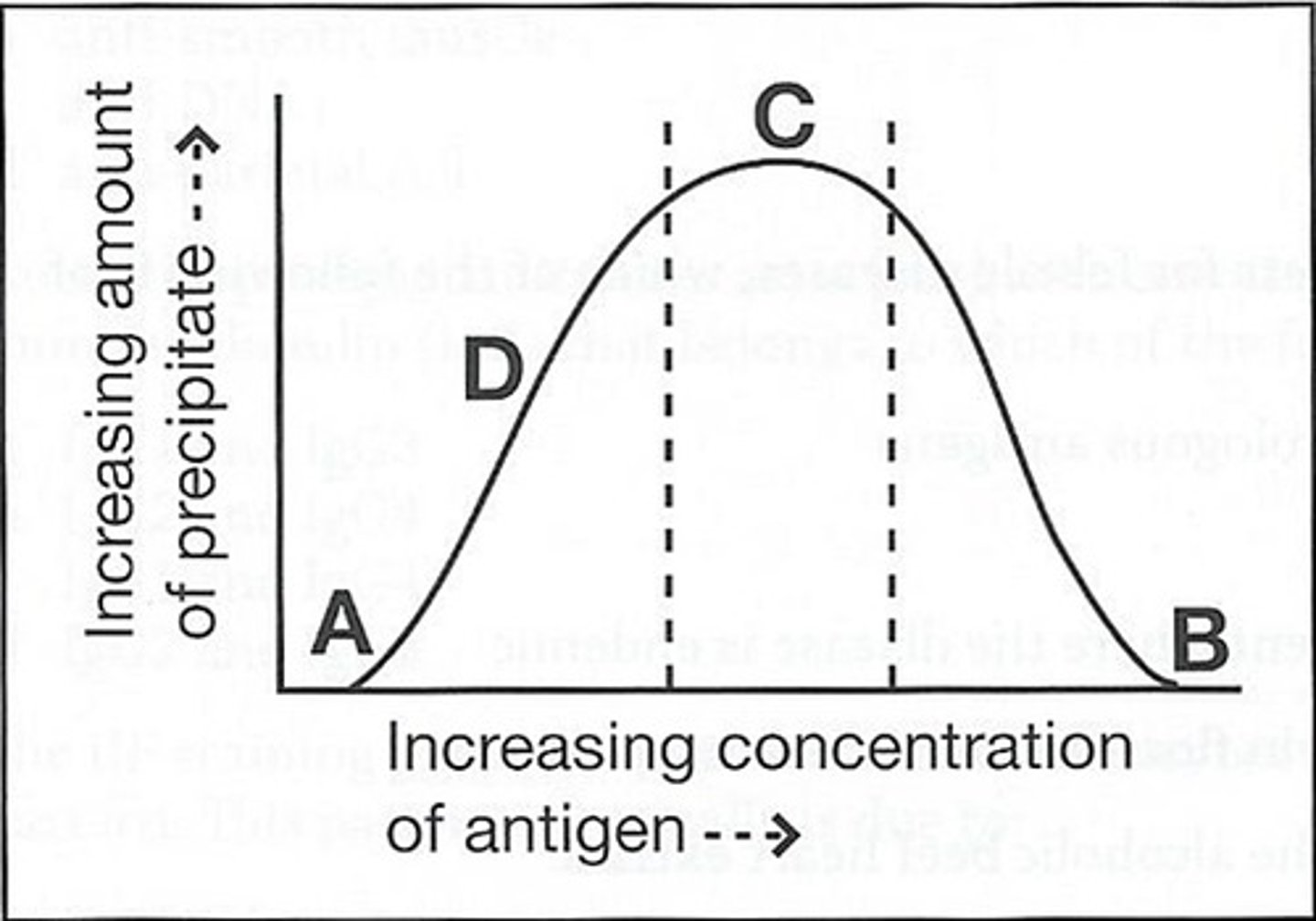
58) The curve below was obtained by adding increasing amounts of a soluble antigen to fixed volumes of monospecific antiserum:
The area in which the addition of more antibody would result in the formation of additional precipitate is:
a. A
b. B
c. C
d. D
b. B
59. refer to the following illustration. which of the above figures demonstrates a reaction pattern of identity?
a. figure 1
b. figure 2
c. figure 3
d. figure 4
a. figure 1
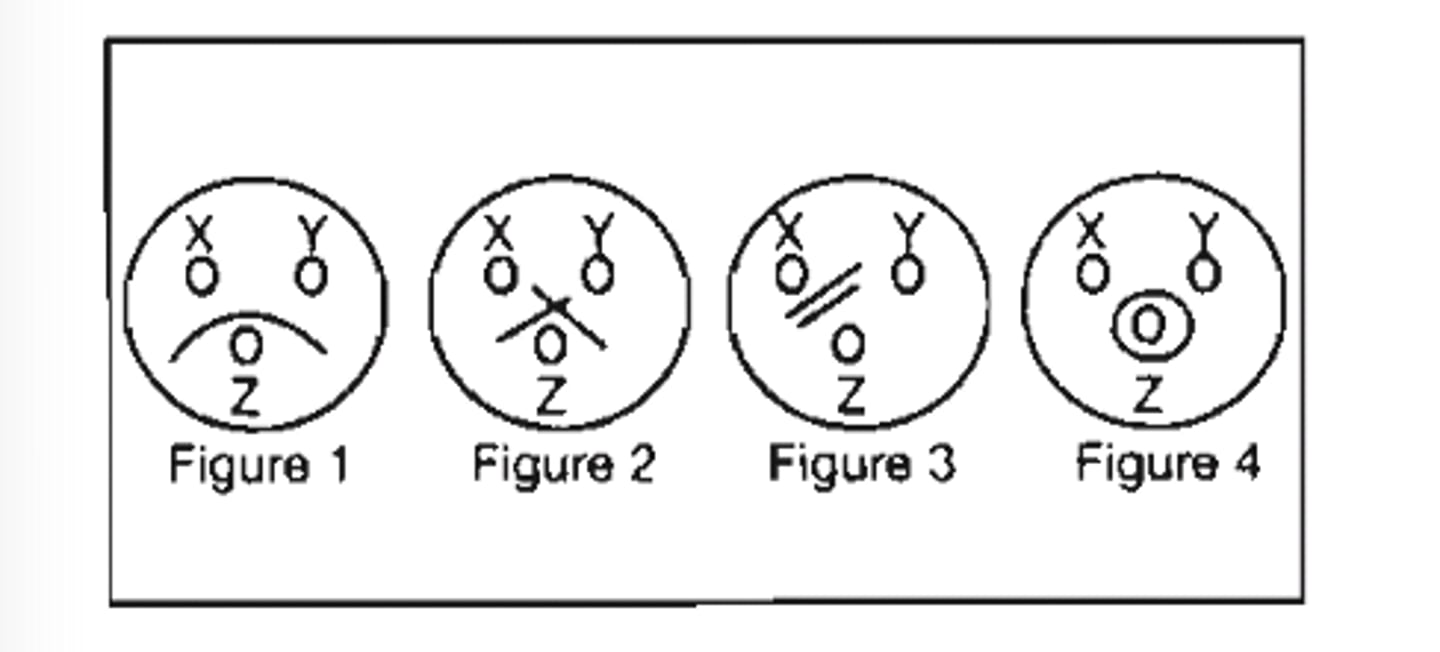
60. refer to the following illustration. which of teh above figures demonstrates a reaction pattern of non identity?
a. figure 1
b. figure 2
c. figure 3
d. figure 4
b. figure 2
61. refer to the following illustration. which of the above figures demonstrates a reaction pattern showing 2 different antigenic molecular species?
a. figure 1
b. figure 2
c. figure 3
d. figure 4
c. figure 3
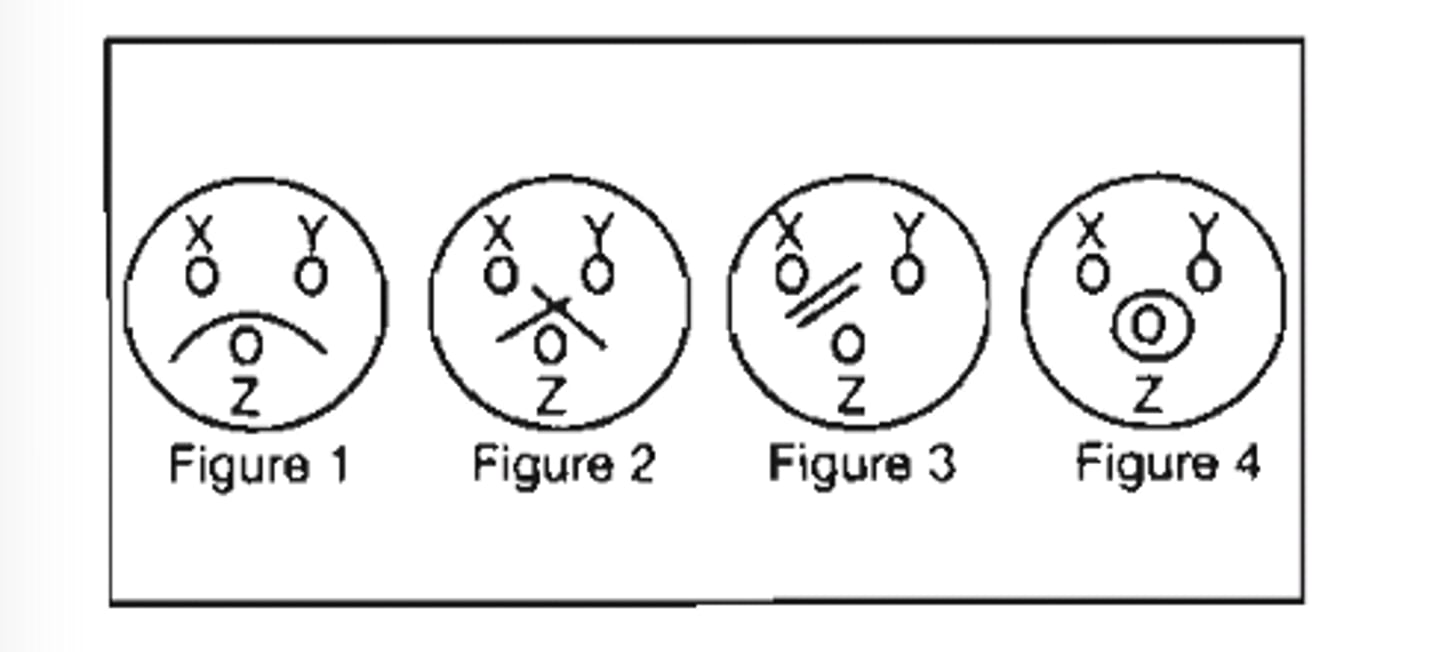
62. Refer to the following illustration:
A nonspecific precipitin reaction is demonstrated is:
a. Figure #1
b. Figure #2
c. Figure #3
d. Figure #4
d. Figure #4
63. A series of 8 tubes are set-up with 0.79 mL of diluent in each. A serial dilution is performed by adding 10µL of serum to the first tube and then transferring 10µL through each remaining tube. What is the serum dilution of tube 7?
a. 1:2.431 × 10^11
b. 1:2.621 × 10^11
c. 1:1.929 × 10^13
d. 1:2.097 × 10^13
d. 1:2.097 × 10^13
64. The enzyme control tube in an ASO hemolytic assay exhibits no cell lysis. What is the most likely explanation for this?
A) incorrect pH of buffer
B) low ionic strength buffer
C) oxidation of the enzyme
D) reduction of the enzyme
C) oxidation of the enzyme
65. The following pattern of aggultination was observed in an antibody titration,
1+, 2+, 4+, 4+, 3+, 3+, 2+, 1+, 1+, 0, 0.
This set of reactions most likely resulted from:
A) faulty pipetting technique
B) postzoning
C) prozoning
D) the presence of a high-titer, low-avidity antibody
C) prozoning
66. In a positive anti-streptolysin O enzyme inhibition test, the patient's:
A) streptolysin "O" enzyme in the patient serum neutralizes the anti-streptolysin "O" reagent, resulting in no hemolysis
B) red blood cells are hemolyzed by the streptolysin"O" enzyme in the reagent
C) anti-streptolysin "O" neutralizes the streptomycin "O" reagent, resulting in hemolysis
D) anti-streptolysin "O" inhibits the reagent streptolysin "O's" resulting in no hemolysis
D) anti-streptolysin "O" inhibits the reagent streptolysin "O's" resulting in no hemolysis
67. Blood is drawn from a patient for serological tests for a viral disease at the time of onset and again 4 weeks later. The results of the test are considered diagnostic if the:
A) first antibody titer is 2x the second
B) first and second antibody titers are equal
C) first antibody is 4x the second
D) second antibody titer is at least 4x the first
D) second antibody titer is at least 4x the first
68. which of the following is most useful in establishing a diagnosis in the convalescence phase of a viral infeciton?
a. slide culture
b. serological techniques
c. shell vial
d culture on McCoy media
b. serological techniques
69. The best method to detect infections due to rubella, epstein-barr, and human immunodefiency viruses is:
A) antigen detection by EIA
B) cell culture
C) antigen detection by Western blot
D) antibody detection by EIA
D) antibody detection by EIA
70. Immunoassays are based on the principle of:
A) separation of bound and free analyte
B) antibody recognition of homologous antigen
C) protein binding to isotopes
D) production of antibodies against drugs
B) antibody recognition of homologous antigen
71. A DPT vaccination is an example of:
A) active humoral-mediated immunity
B) passive humoral-mediated immunity
C) cell-mediated immunity
D) immediate hypersensitivity
A) active humoral-mediated immunity
72. Cells known to be actively phagocytic include:
A) neutrophils, monocytes, basophils
B) neutrophils, eosinophils, monocytes
C) monocytes, lymphocytes, neutrophils
D) lymphocytes, eosinophils, monocytes
B) neutrophils, eosinophils, monocytes
73. The presence of HbsAg, anti-HBc and often HbeAg is characteristic of:
A) early acute phase HBV hepatitis
B) early convalescent phase HBV hepatitis
C) recovery phase of acute HBV hepatitis
D) past HBV infection
A) early acute phase HBV hepatitis
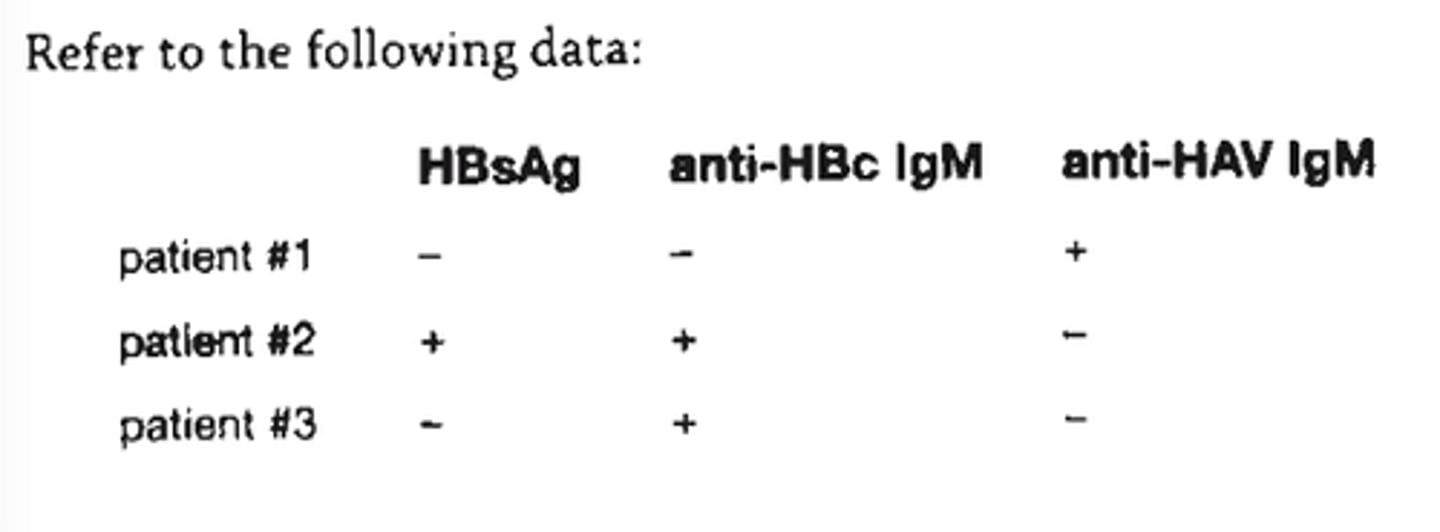
74. (see pic) Refer to the following data:
HBsAg Anti-HBc IgM Anti-HAV Igm
patient #1 - - +
patient #2 + + -
patient #3 - + -
From the test results above, it can be concluded that patient #3 has:
a. recent acute hepatitis A
b. acute hepatitis B
c. acute hepatitis C (non-A/non-B hepatitis)
d. chronic hepatitis B
b. acute hepatitis B
75. The disappearance of HBsAg and HBeAg, the persistence of anti-HBc, the appearance of anti-HBs, and often of anti-AHe indicate:
a. early acute HBV hepatitis
b. early convalescent phase HBV hepatitis
c. recovery phase of acute HBV hepatitis
d. carrier state of acute HBV hepatitis
c. recovery phase of acute HBV hepatitis
76. An example of an organ specific disease with autoimmune antibodies is:
a. Wegener granulomatosus
b. rheumatoid arthritis
c. Hashimoto thyroiditis
d. systemic lupus erythematosus
c. Hashimoto thyroiditis
77. When testing a patient for HIV antibody, which of the following is used to confirm a positive screening test?
A) radioimmunoassay
B) Western blot
C) immunofluorescence
D) ELISA
B) Western blot
78. An example of a live attenuated vaccine used for human immunization is:
a. rabies
b. tetanus
c. hepatitis B
d. measles
d. measles
79. A cold agglutinin titer end point is 1:16 after incubating overnight in the refrigerator and remains 1:16 after warming. The best course of action is to:
a. report the titer as negative
b. report the titer as positive, 1:16
c. repeat the titer with a fresh sample
d. test for antibody specificity
d. test for antibody specificity
80. What kind of antigen-antibody reaction would be expected if soluble antigen is added to homologous antibody?
A) precipitation
B) agglutination
C) complement fixation
D) hemagglutination
A) precipitation
81. The rapid plasma reagin test:
A) is useful in screening for syphilis
B) is useful in diagnosing syphilis
C) does not give false-positives
D) uses heated plasma
A) is useful in screening for syphilis
82. Flocculation tests for syphilis detect the presence of:
A) reagin antibody
B) antigen
C) hemolysin
D) Forssman antigen
A) reagin antibody
83. In the cold agglutination test, the tubes containing the serum and erythrocytes are allowed to stand overnight in the fridge, and results are read next morning. If a disk of the erythrocytes floats up from the bottom of the tube with only the flick of a finger, this is read as a:
A) 4+ reaction
B) 2+ reaction
C) 1+ reaction
D) negative reaction
A) 4+ reaction
84. Flocculation tests for syphilis use antigen composed of:
A) treponema pallidum
B) reagin
C) cardiolipin and lecithin
D) charcoal
C) cardiolipin and lecithin
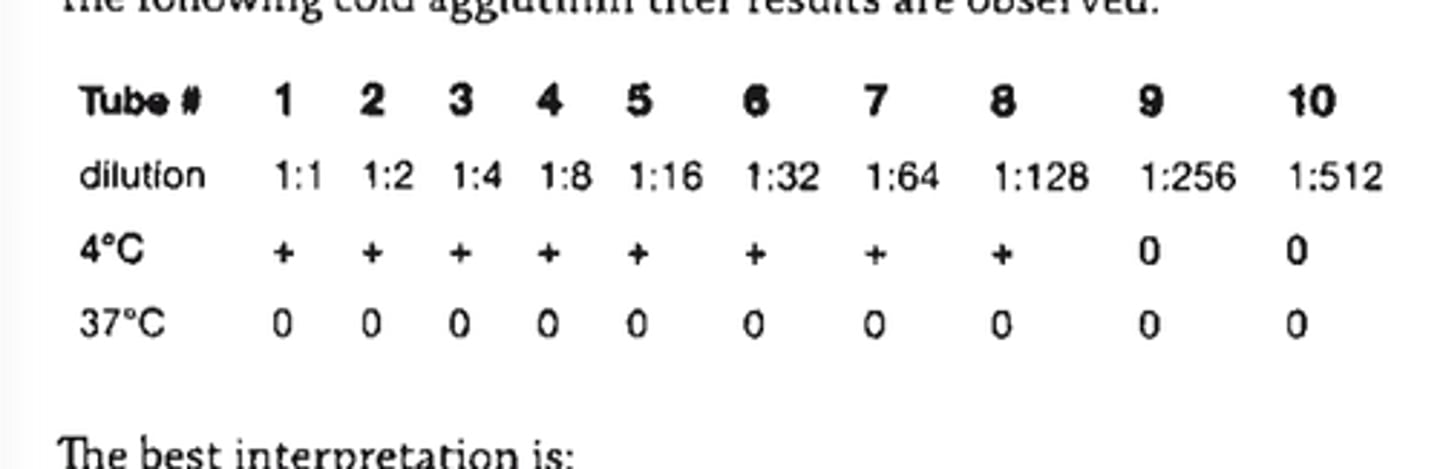
85) (see pic) The following cold agglutinin titer results are observed:
The best interpretation is:
a. positive, 1:128
b. negative
c. invalid because 37 C reading is negative
d. repeat the 4 C readings
a. positive, 1:128
86. A VDRL serum sample is heat inactivated, then placed in a fridge for overnight storage. Before being tested, the serum must be:
A) kept colder than 10° C
B) allowed to equilibrate to room temperature
C) warmed to 37°C
D) reheated to 56°C for 10 minutes
D) reheated to 56°C for 10 minutes
87. Substances that are antigenic only when coupled to a protein carrier are:
A) opsonins
B) haptens
C) adjuvants
D) allergens
B) haptens
88. A haptenic determinant will react with:
a. both T cells and antibody
b. T cells but not antibody
c. neither T cells nor antibody
d. antibody but not T cells
d. antibody but not T cells
89. A serological test for syphilis that depends upon the detection of cardiolipin-lecithin-cholesterol antigen is:
A) FTA-ABS
B) RPR
C) MHA-TP
D) TPI
B) RPR
90. The most important use of a nontreponemal antibody (NTA) test alone is in:
a. establishing the diagnosis of acute active syphilis
b. establishing the diagnosis of chronic syphilis
c. evaluation of the success of therapy
d. determining the prevalence of disease in the general population
c. evaluation of the success of therapy
91. The serological test for syphilis recommended for detecting antibody in Cerebrospinal fluid is:
A) nontreponemal antibody
B) CSF-VDRL
C) FTA-ABS
D) MHA-TP
B) CSF-VDRL
92. In the direct fluorescent antibody test for primary syphilis, spirochetes are detected by addition of labeled antibody to?
a. Treponema pallidum
b. cardiolipin
c. human immunoglobulin
d. nonpathogenic treponemes
a. Treponema pallidum
93. In the FTA-ABS test the presence of a beaded pattern of fluorescence along the treponeme indicates
a. positive identification of Treponema pallidum
b. presumptive diagnosis of active syphilis
c. presence of nontreponemal antibody (NTA)
d. false-positive reaction
d. false-positive reaction
94. The FTA-ABS test for the serological diagnosis of syphilis is:
a. less sensitive and specific than the VDRL if properly performed
b. likely to remain positive after adequate antibiotic therapy
c. currently recommended for testing cerebrospinal fluid
d. preferred over darkfield microscopy for diagnosing g primary syphilis
b. likely to remain positive after adequate antibiotic therapy
95. A 16-year-old boy with infectious mononucleosis has a cold agglutinin titer of 1:2000. An important consideration of this antibody's clinical relevance is the:
a. thermal range
b. titer at 4℃
c. specificity
d. light chain type
a. thermal range
96. What assay would confirm the immune status of hepatitis B virus?
A) HBsAg
B) anti-HBs
C) IgM anti-HBcAg
D) hepatitis C Ag
B) anti-HBs
97. The following procedure has been routinely used for detection of hepatitis B surface antigen (HBsAg) because of its high level of sensitivity:
A) hemagglutination
B) counterimmunoelectrophoresis
C) radial immunodiffusion
D) ELISA
D) ELISA
98. In an indirect ELISA method desiged to detect antibody to the rubella virus in patient serum, the conjugate used should be:
A) anti-human IgG conjugated to an enzyme
B) anti-rubella antibody conjugated to an enzyme
C) rubella antigen conjugated to an enzyme
D) anti-rubella antibody conjugated to a substrate
A) anti-human IgG conjugated to an enzyme
99. A request is received in the laboratory for assistance in selecting the appropriate test(s) for detecting Lyme disease. Which of the following would be suggested?
a. Stool culture should be done to isolate the causative organism.
b. The organism is difficult to isolate, and antibody titers will provide the most help.
c. Borrelia burgdorferi is easily isolated form routine blood cultures.
d. This is an immunologic syndrome, and cultures are not indicated.
b. The organism is difficult to isolate, and antibody titers will provide the most help.
100. A bacterial protein used to bind human immunoglobulins is:
a. HAV antibody, IgA type
b. Escherichia coli protein C
c. Staphylococcal protein A
d. HAV antibody, IgG type
c. Staphylococcal protein A