Lesson 104 - Small Herbivore Dental Disease, Gastrointestinal Syndrome, and Intro to Rabbit Medicine
1/131
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
132 Terms
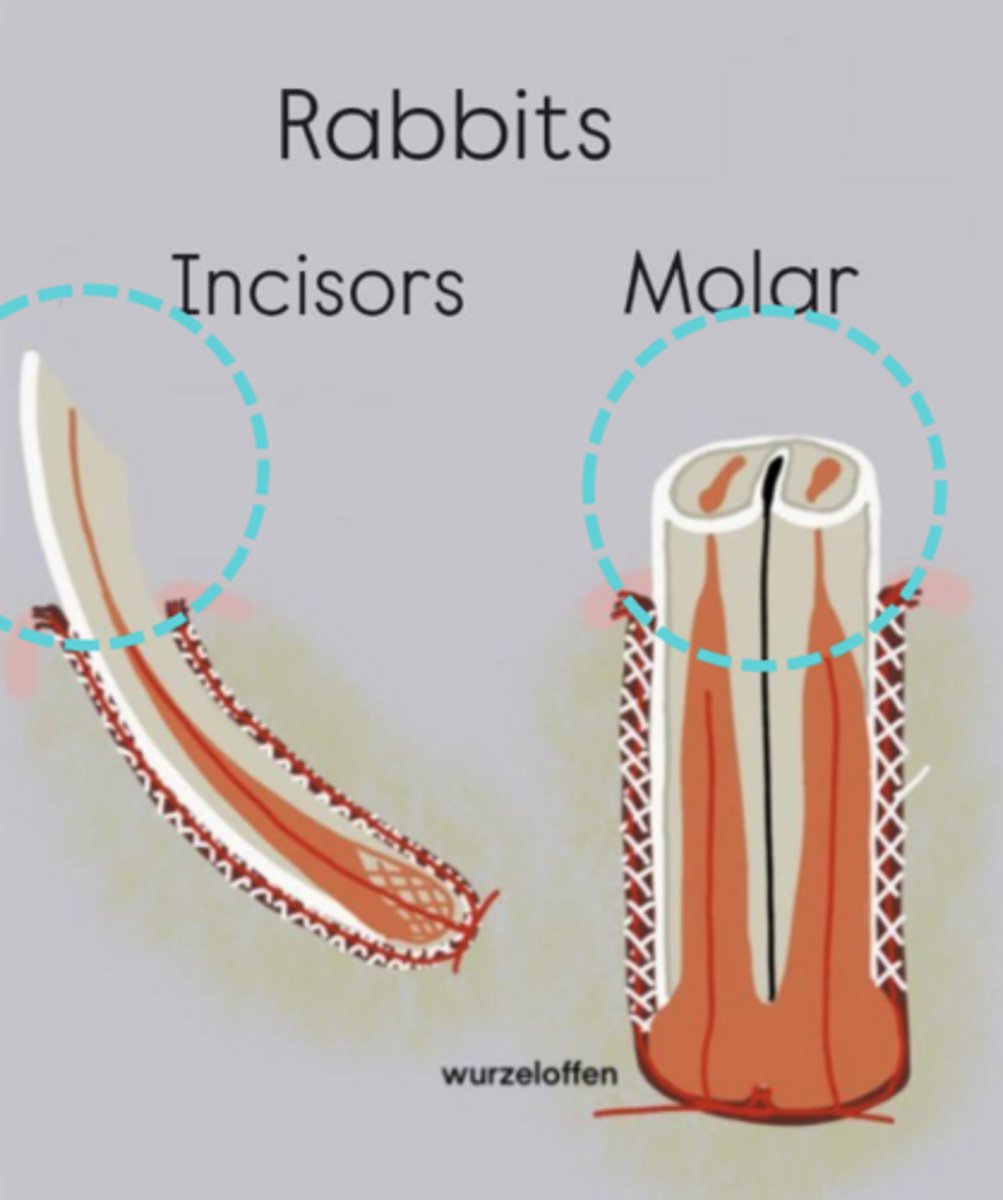
What part of the tooth is being circled?
clinical crown

What part of the tooth is being circled?
reserve crown
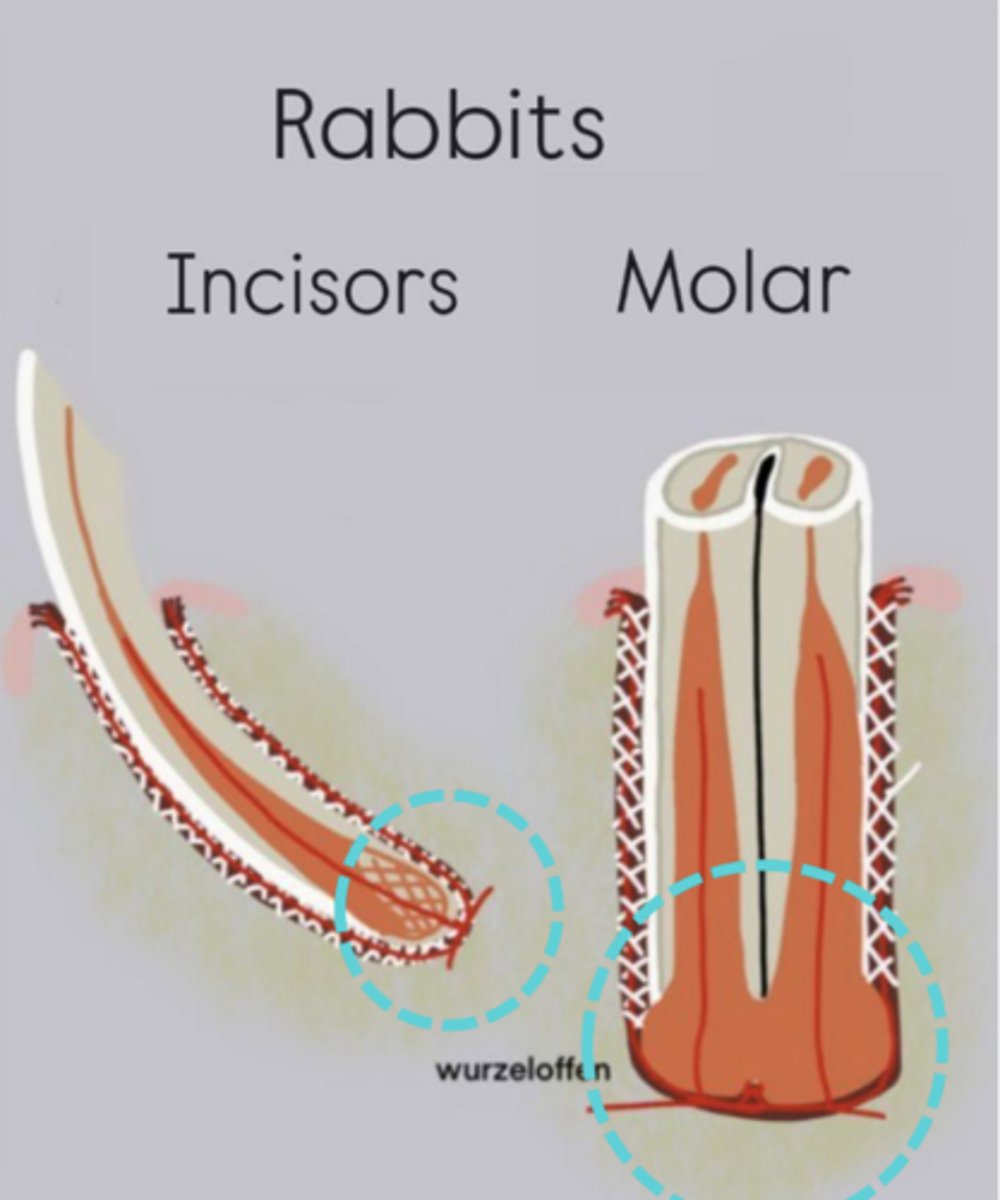
What part of the tooth is being circled?
apex
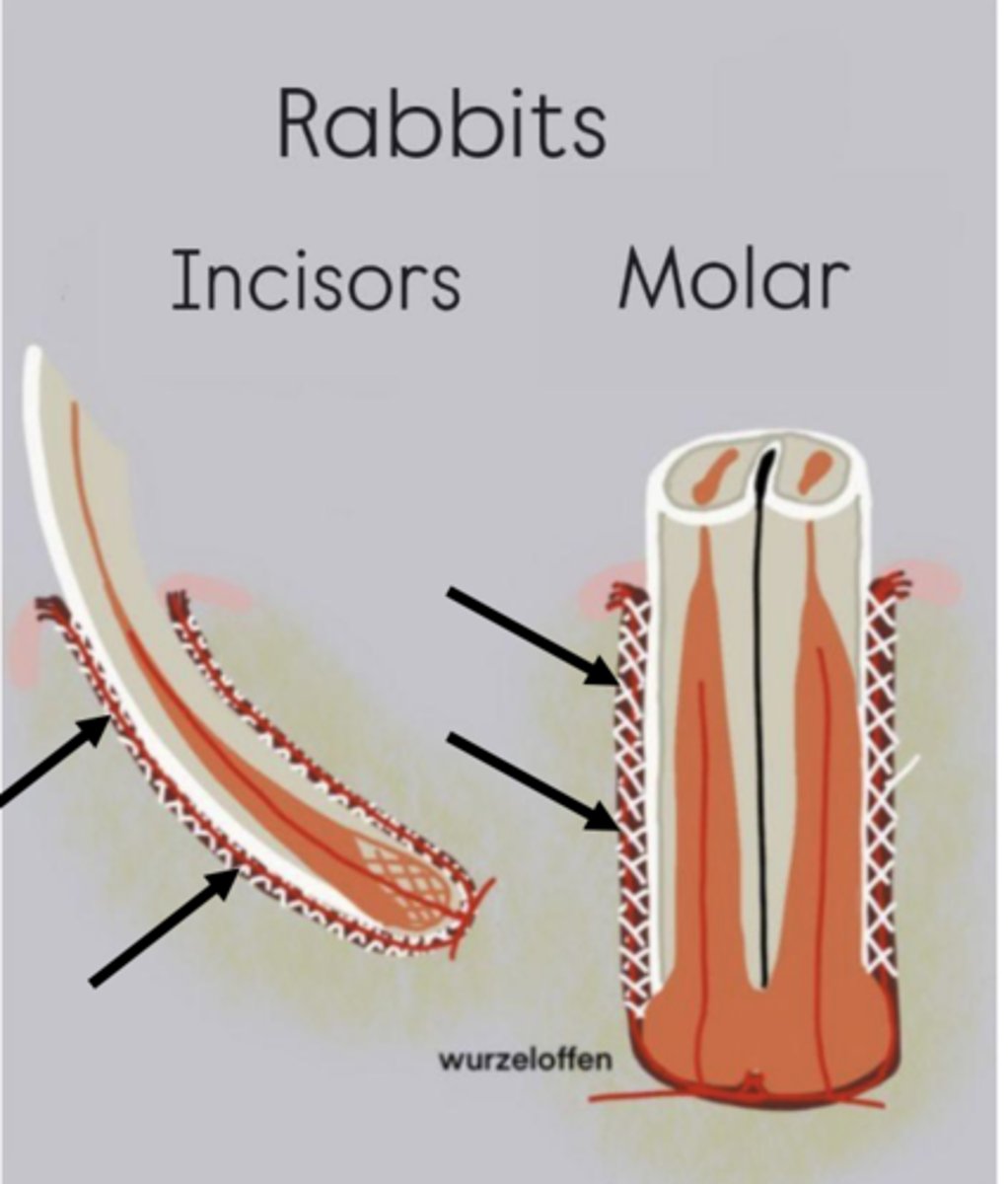
What part of the tooth are the arrows pointing to?
periodontal ligament
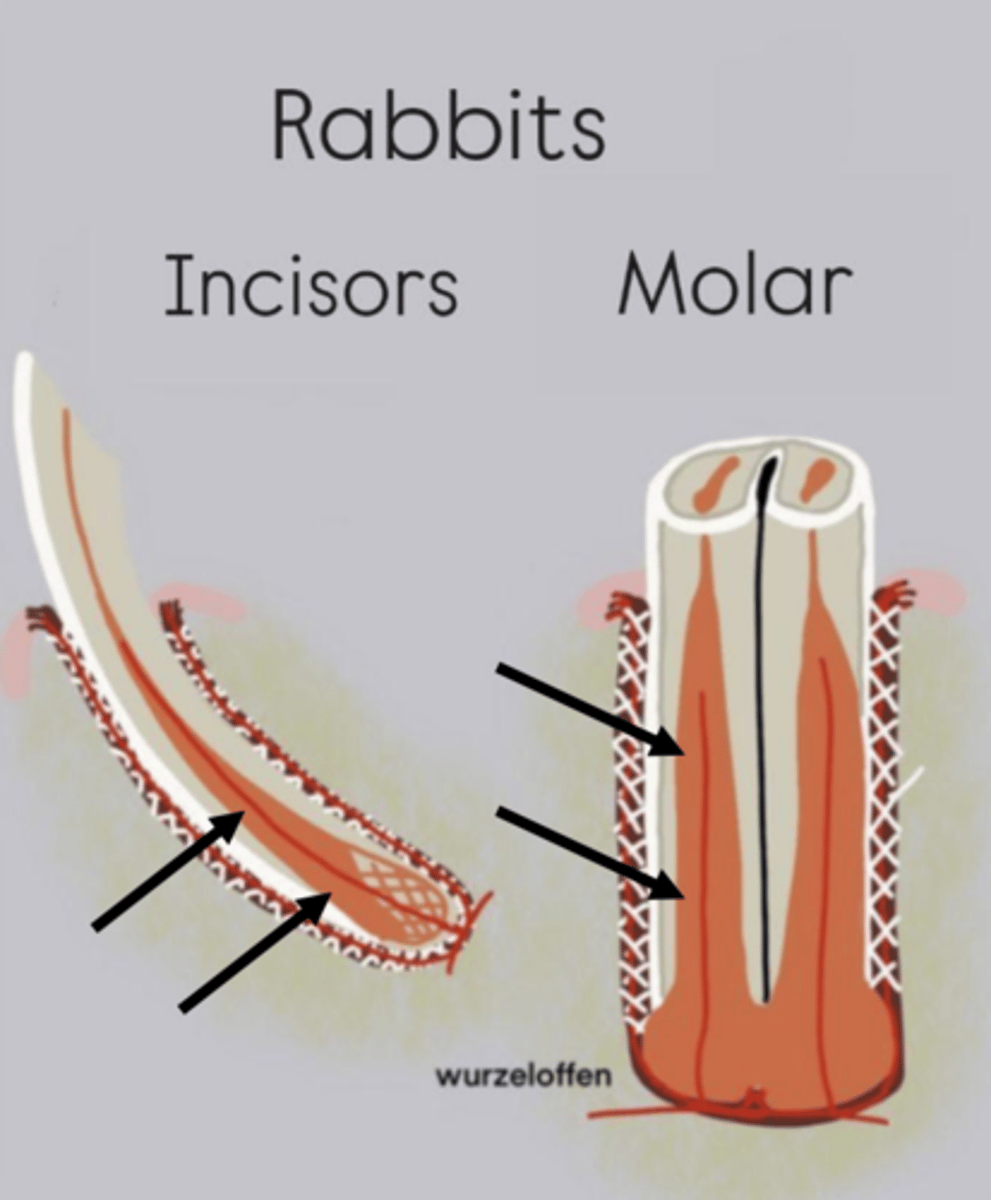
What part of the tooth are the arrows pointing to?
pulp cavity
What are the characteristics of the clinical crown?
1. above gumline
2. occludes with opposite teeth to grind food
3. only in contact with opposing teeth when chewing, not at rest
4. labial aspect of incisor is harder than lingual aspect, so occlusal surface is chiseled as it wears
What are the characteristics of the reserve crown?
1. developing portion below the gumline
2. eventually becomes clinical crown
3. contains pulp cavity
4. anchored to alveolar bone by periodontal ligament
What are the characteristics of the apex?
1. end of tooth opposite the occlusal surface
2. contains apical bud
3. essential for life long growth of tooth
What is the apical bud?
proliferative zone that houses stem cells that can make new odontoblasts and other dental tissues
What are the characteristics of the periodontal ligament?
1. anchors reserve crown to alveolar bone
2. can withstand momentary stress, but not prolonged
3. will give way with just a few grams of compressive force over prolonged period (damage to tooth apex)
What are the characteristics of the pulp cavity?
1. contains odontoblasts, vasculature, and nervous tissue
2. provides nutrition, oxygen, hydration, sensory, and immune function to the developing tooth
What is the progression of dental disease as rabbits age?
1. insufficient cheek tooth wear causes crown on crown contact
2. apical tooth compression damages apical bud (new tooth formation slows or stops)
3. alveolar bone remodels and apical elongation often occurs
4. bacteria invade the apex and cause infection/abscess when new clinical crown ceases to erupt

What is being shown here?
overgrown, maloccluded incisors
What happens when rabbits/rodents have overgrown incisors?
1. cannot cut large items such as leafy greens and whole vegetables into small pieces that can be passed back to the molars and chewed
2. cannot properly groom themselves
How are overgrown incisors treated?
incisors must be trimmed repeatedly, sometimes with sedation/anesthesia, and sometimes without
What is a permanent resolution for overgrown incisors?
incisor extraction using purpose-built rabbit/rodent dental instruments
What do rabbits and rodents without incisors eat?
can still eat pellets, hay, veggies with long narrow stems, and produce that has been cut into small pieces
What are the clinical signs of cheek tooth maloclusion (points/spurs)?
1. decreased droppings
2. weight loss
3. lethargy
4. unkempt
5. behavior change
6. vocalization
How can you diagnose cheek tooth maloclusion (points/spurs)?
physical exam including intraoral exam with bivalve or otoscope using "burrito" wrap restraint
Where do maxillary tooth points/spurs tend to form?
buccal aspect of teeth
Where do mandibular tooth points/spurs tend to form?
lingual aspect of teeth

What kind of tooth point/spur is this?
maxillary

What kind of tooth point/spur is this?
mandibular
What species are affected by tooth malocclusion (points/spurs)?
all species with elodont cheek teeth
What is a common sequela to cheek tooth malocclusion?
secondary moist dermatitis from excessive drooling
How can cheek tooth malocclusion be treated?
1. regular tooth trimming
2. rongeur
3. dental burr
What are common clinical signs of an odontogenic abscess?
1. eye bulging
2. dry cornea with no PLR
3. dark, loose maxillary cheek teeth
4. advanced dental disease
What are the two kinds of odontogenic abscesses?
maxillary or mandibular

What kind of odontogenic abscess is shown here?
maxillary

What kind of odontogenic abscess is shown here?
mandibular
What species mostly get odontogenic abscesses?
rabbits and hystricomorphs
How are odontogenic abscesses treated?
ppening, flushing, wound packing and removal of diseased teeth usually necessary indicated (enucleation may be necessary, but not always)
What is the prognosis of odontogenic abscesses?
1. varies by lesion severity
2. incisors malocclusion frequently requires repeat trimming
3. progressive and non-reversible
4. mild cases can be managed by intermittent trimming and filing of the teeth
5. removal of loose or infected teeth, and treatment of odontogenic abscesses are frequently indicated with advanced disease
6. prognosis for return to normal is poor
What is the goal of odontogenic abscess treatment?
provide the animal with a good quality of life by minimizing discomfort, maintaining body condition, and enabling the pet to eat on its own if possible
How can odontogenic abscesses be prevented?
1. course diet, high in fiber and low in simple carbohydrates
2. parents who produce prognathic young should be removed from the breeding program (particularly rabbits)
3. long-stem grass hay intake should be offered ad lib, and a moderate amount of pellet and greens should be offered daily
4. treats such as dried fruit and yogurt drops should be minimized or eliminated
5. complete physical exam and laboratory database are recommended every 6-12 months
6. any suspicion of dental disease should indicate a closer oral examination while sedated
7. skull imaging (radiographs, CT scan) aid in early detection of dental disease
Which species eat primarily the leaves and stems of plants, are dependent on the hindgut for digestion and nutrient production, have a functional cecum, and are considered hindgut fermenters?
degu, chinchilla, prairie dog, guinea pig, and rabbit
Which species consume the energy dense portions of plans in additional to non-plant food sources (are omnivorous), and thus are less dependent on the hindgut digestion and nutrient production?
hamsters, gerbils, rats, and mice
What anatomical feature is a component of the rabbit digestive tract?
3 multiple choice options
Sacculus rotundus
What are the characteristics of gastrointestinal syndrome?
1. symptom, not a disease
2. can occur at any age
3. no breed or gender predilections
4. indicates that factors governing GI motility are out of order
What is the purpose of long-stemmed hay and and course roughage in the diet?
promote gut motility in a way that finely-ground hay fiber does not
What is the pathophysiology of gastrointestinal syndrome?
1. inadequate long-stemmed course fiber
2. altered cecal fermentation, pH, and substrate production
3. negative effect on enteric microflora
4. low fiber, high carbohydrate diet that threatens favorable microorganisms and promotes bacterial pathogens and toxin production
5. bacterial dysbiosis
What is bacterial dysbiosis?
disruption of normal GI microflora
What can bacterial dysbiosis cause?
1. diarrhea (acute, chronic, intermittent)
2. enterotoxemia
3. ileus
4. excessive gas production
5. gas accumulation
What species can get bloat?
rabbits, guinea pigs, chinchillas
What are the characteristics of bloat?
1. can't vomit or eructate
2. small volume gas normal
3. peristalsis eliminates
What are the characteristics of bloat with gastrointestinal stasis?
1. excessive gas production
2. lack of peristalsis
3. stomach, intestines become distended
What happens when there is adequate fiber in the diet?
normal GI motility and resistance to GIS
What happens when there is insufficient fiber in the diet?
subclinical hypomotility and susceptibility to GIS
What dietary factors contribute to GIS?
commercial pellets, cereal products, high carbs, high sugar
What are some potential triggers for GIS?
1. inappetence or anorexia from pre-surgical fasting, sudden diet changes, concurrent illness, or starvation
2. dehydration from sipper malfunction, bad tasting water, or a careless mistake
How does stress have a negative effect on GI motility?
increased adrenal epinephrine inhibits peristalsis
What does the autonomic nervous system regulate?
gut motility, flight response, and brief massive adrenal bursts (not prolonged events)
What are some common causes of stress?
1. dental disease
2. metabolic disease
3. pain
What is the typical treatment plan for a mild case of GIS from an abrupt diet change where the patient is stable?
send home with syringe feeding, fluids, and an appetite stimulant, and return to familiar diet formula
What is the typical treatment plan for a severe case of GIS with acute onset and liver enzyme elevations (most likely from liver lobe torsion)?
1. fluids
2. surgery
3. post-op support
4. assisted feeding
5. analgesia
6. antinausea
7. prokinetics
8. discharged in 24h
9. hospitalization
What dietary factor is most important in stimulating normal gastrointestinal motility in small herbivores?
long-stem, course fiber
What does the prognosis of GIS depend on?
severity and underlying cause
What is the prognosis of mild GIS with chronic symptoms due to inappropriate diet?
excellent to good, and diet correction often leads to complete recover
What is the prognosis of moderately severe, acute GIS that require hospitalization?
good to fair, and the patient usually improves after several days of intensive supportive care and is discharged for additional care at home
What is the prognosis of advanced GIS cases that went unnoticed for several days prior to presentation?
poor
What complications of GIS make treatment unrewarding?
hepatic lipidosis, shock, etc.
How can GIS be prevented?
1. strict feeding of diets containing adequate amounts of indigestible coarse fiber (long-stemmed hay) and low simple carbohydrate content
2. clean water is always available and is presented in a familiar manner (sipper vs. bowl)
3. daily exercise to prevent obesity
4. minimize changes in the daily routine that might cause stress in small herbivores and avoid sudden changes to the diet
5. use only broad-spectrum antibiotics such as trimethoprim-sulfas, fluoroquinolones, chloramphenicol, aminoglycosides, azithromycin, and metronidazole
6. discontinue antibiotics if soft stools or other GI signs develop
7. use drugs that can depress GI motility with caution in small herbivores
8. avoid over-fasting patients prior to surgery, control perioperative pain and stress, and encourage patients to eat as soon as possible following surgery
9. make sure all post-op patients are eating and passing feces prior to release
How many incisors are present in rabbits?
4
When does ovulation occur in rabbits?
induced by breeding (no estrus cycle)
What is rabbit nutrition like?
1. Graze and browse
2. Undigestible fiber stimulates peristalsis
3.. Cecotrophy after fermentation ("pseudorumination")
4.. Grass hay ad lib
5. Pelleted diet
6. Avoid grain, seed, starch and sugar
7. Fresh water ad lib
What is the GI transmit time in rabbits?
4-5 hrs
What part of the rabbit GI system retains soluble contents?
cecum
What part of the rabbit GI separates and eliminates insoluble fiber (the hard feces)?
large intestine
What is the rabbit genus?
Oryctolagus cuniculus, and belongs to the order Lagomorpha
Where can rabbits be kept?
indoors or outdoors
What are two of the greatest hazards to rabbits?
electrical cords and poisonous plants
How do intact adult male rabbits mark their territory?
deposit strong-smelling feces
What temperature extreme do rabbits tolerate better?
cold better than heat
What is the optimal temperature range for rabbits?
between 39-82°F (4-28°C)
What should outdoor housing for rabbits provide?
adequate shade, protection from the wind, and safety from predators
What are the characteristics of rabbit housing?
1. indoor rabbits caged and let out for supervised exercise in "rabbit proofed" area
2. like to chew and scratch objects
3. generally litter trained
4. outdoor rabbits housed in hutches
5. solid or wire flooring
6. wire flooring needs solid areas
7. straw, newspaper pellets, or wood shavings make suitable bedding
8. rabbits housed indoors should each have their own cage
9. if caged together, each rabbit should have its own hide box
10. generally social but fights occasionally occur
Why does flooring need to be kept clean and dry?
avoid pododermatitis ("sore hocks")
What can rabbits transmit to guinea pigs (should not be housed together)?
bordetella bronchiseptica
An 8-month-old intact female rabbit was placed in a cage in the shade outdoors. However, her owners forgot about her for a couple hours, the shade moved, and she was in direct sunlight for an undetermined period. When they discovered her, she was recumbent, panting, and salivating. At presentation the patient's pinnae are very red, she appears weak. What is your presumptive diagnosis?
heat stress
What causes heat stress in rabbits?
1. little protection from high temperatures
2. only sweat from glands around their lips
3. ineffective at panting
4. do not increase their water intake in response to high temperatures
5. dissipate heat from their ears
6. actively seek shade to conserve water
7. shelter from direct sunlight is essential for rabbits housed outdoors in the summer
8. cool drinking water must always be available
What are the clinical signs of heat stress in a rabbit?
1. Rapid shallow breathing
2. Salivation
3. Lethargy
4. Weakness
5. Incoordination
6. Reddening of the pinnae
7. Delerium
8. Convulsions
9. Rectal temp >105°F (40.5°C)
How is heat stress treated in rabbits?
1. Gradual cooling
2. Wet the ears
3. Wet towels
4. Fans
5. Ice packs/bottles
6. Fluids at room temp
7. Monitoring rectal temp
What is a secondary issue that can be caused by heat stress?
GIS
What is the prognosis of heat stress in a rabbit?
poor

A 2 y/o intact female rabbit presents for favoring its right forelimb. On exam, excoriations, alopecia, scabs and swelling of various degrees are present on all feet. What is the presumptive diagnosis?
pododermatitis
What is ulcerative pododermatitis?
sore Hocks from pressure necrosis, trauma due to rough, wet, unsanitary floor, thumping
What predisposes rabbits to ulcerative pododermatitis?
obesity, wire cages, large breed, preserve thick fur on soles feet
What are the characteristics of ulcerative pododermatitis?
1. Decubital ulceration
2. Staph aureus, other infections
3. Heal slowly
4. Culture/sensitivity
5. Aggressive wound care/bandages, antibiotics

A 4 y/o spayed female Netherland dwarf presents for moist skin between the chin and dewlap. Affected hair is greenish and has a slightly sweet odor. Based upon the clinical presentation, microbe is likely the cause of the secondary infection?
pseudomonas
Why are water bottles or crocks with high sides recommended for rabbits?
rabbits tend to hang their dewlaps in the water when they drink
What happens when the sides of the rabbit's water bowl are too low?
chronic wetting of the dewlap can result in moist dermatitis and secondary Pseudomonas infection (affected fur may turn greenish in color)
What can a wet chin, neck, and dewlap also be associated with in rabbits?
dental disease, oral ulceration, and jaw abscessation
What is moist dermatitis (urine scald)?
dermatitis around the vent region in rabbits with redundant skin, or in rabbits that sit where they urinate

10-month-old intact male New Zealand White rabbit is part of a drug study. Staff lost their grip on him when picking him up, the rabbit kicked, vocalized ("screamed"), and was paraplegic immediately after. What is the presumptive diagnosis
spinal fracture
What makes rabbits prone to spinal fractures?
1. skeletal mass of rabbits represents 8% of bodyweight, and muscle comprises more than 50%
2. powerful hind legs and can kick violently
3. kicking can result in vertebral fracture, and damage to the spinal cord can result
What is the most commonly fractured vertebra in rabbits?
7th lumbar vertebra
What is another relatively common fracture seen in rabbits?
tibia
What is an abscess?
localized collections of pus caused by infection, frequently seen in rabbits due to dental disease, trauma, or bacterial spread
What is cuterebriasis?
parasitic infestation caused by Cuterebra fly larvae, typically found in rodents and rabbits, leading to swelling, tissue damage, and a draining wound
What is otoacariasis?
ear condition caused by Psoroptes cuniculi mites, commonly seen in rabbits, resulting in itching, inflammation, and crusting