Acquired and Congenital Conditions in Newborns
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
59 Terms
What is birth trauma in newborns?
Physical injury sustained during labor and birth, which may be avoidable.
Clavicle
Bone most often fractured during birth as a result of shoulder dystocia or from force of labour. generally the break is in the middle third of the bone.
Limited arm motion
Crepitus over the bone
Absence of Moro reflex on the affected side
What role does ultrasonography play in birth trauma?
It enables antepartum diagnosis of potential birth injuries.
What are some types of skeletal injuries that can occur during birth?
Peripheral nervous system injuries, including Brachial palsy, Erb palsy, Klumpke Palsy, facial nerve paralysis, and phrenic nerve paralysis.
Brachial Plexus Injury
Results from trauma to the spinal roots of the fifth cervical nerve to the first thoracic nerve and alter the normal position and relationship of the arm, shoulder, and neck
Macrosomia and shoulder dystocia are associated with this
The Moro reflex is absent on the affected side in all forms
Erb Palsy (Erb Duchenne Paralysis)
Caused by damage to the upper brachial plexus and usually results from lateral traction of the head and neck away from the shoulder as the fetus goes through the birthing process.
May occur with shoulder dystocia or with a difficult vertex or breech birth.
Clinical Manifestations of Erb Palsy
The clinical manifestations are related to the paralysis of the affected extremity and muscles.
The arm hangs limply alongside the body. The shoulder and arm are adducted and internally rotated; the elbow is extended, and the forearm is pronated, with the wrist and fingers flexed.
In newborns with very severe deficits, the arm may be cooler because of the sympathetic nervous system outflow at T1.
Torticollis is commonly present and almost always with the face turned away from the involved arm

Torticollis
Is a stiff neck that makes it hard or painful to turn your head.
Klumpke Palsy
A less common lower plexus palsy, results from severe stretching of the upper extremity while the trunk is relatively less mobile.
Clinical Manifestation of Lower Brachial palsy
The muscles of the hand are paralyzed, with resultant wrist drop and relaxed fingers. In a third and more severe form of brachial palsy, the entire arm is paralyzed and hangs limply and motionless at the infant’s side.
Goal of treatment of Brachial Plexus Palsies
Prevention of contractures, and maintenance of correct placement
of the humeral head within the glenoid fossa of the scapula.
Complete recovery from stretched nerves usually takes 3 to 6 months.
However, avulsion (disconnection) of the nerves of the ganglia from the spinal cord results in permanent damage. For those injuries that do not improve by 3 to 6 months, surgical intervention may be needed torelieve pressure on the nerves or to repair the nerves with grafting
Care of the Newborn with Brachial Palsy
Focuses on positioning of the affected arm through 90-degree abduction with external shoulder rotation, forearm supination, and extension at the wrist with the palm facing the newborn’s face.
Occupational therapy or physiotherapy, initiated in the second week, involves passive range-of-motion exercises of the shoulder, wrist, elbow, and fingers.
Wrist flexion contractures may be prevented with the use of a wrist splint with padding in the fist.
In dressing the newborn, preference is given to the affected arm. Undressing begins with the unaffected arm, and re-dressing begins with the affected arm to prevent unnecessary manipulation and stress on the paralyzed muscles.
Parent education includes newborn positioning in the football position and avoiding picking up the baby from under the axillae or by pulling on the arms.
Facial Palsy
Pressure on the facial nerve (cranial nerve VII) during birth may result in injury. Most noticeable when the newborn cries.
Clinical Manifestation of Facial Palsy
The primary clinical manifestations are loss of movement on the affected side, such as an inability to completely close the eye, drooping of the mouth, and absence of wrinkling of the forehead and nasolabial fold The mouth is drawn to the unaffected side, wrinkles are deeper on the normal side, and the eye on the involved side remains open.
Often the condition is temporary, resolving within hours or days of birth. Permanent paralysis is rare.
Nursing Care of Neborn with Facial Palsy
Assisting the newborn to suck and helping the parent with feeding techniques.
The newborn may require gavage feeding to prevent aspiration.
Breastfeeding is not contraindicated, but the breastfeeding parent may need additional assistance to help the newborn latch on to the breast.
If the eyelid on the affected side does not close completely, artificial tears can be instilled daily to prevent drying of the conjunctiva, sclera, and cornea. The lid may be taped shut to prevent accidental injury.
Phreni nerve Paralysis
Results in diaphragmatic paralysis. Ultrasonography shows paradoxical chest movement and an elevated diaphragm
Diaphragmatic paralysis often occurs in conjuction with brachial palsy
Usually unilateral, the lung on the affected side does not expand and respiratory efforts are ineffective.
Signs of Possible diaphragm injury
Cyanosis
Respiratory distress
Care for newborn with phrenic nerve paralysis
Same nursing care for infant in respiratory distress
What is hypoxic ischemic encephalopathy (HIE)?
Nonprogressive neurological (brain) impairment caused by intrauterine or postnatal asphyxia resulting in hypoxemia or cerebral ischemia
Hypoxic-ischemic encephalopathy—the resultant cellular damage that causes the clinical manifestations
Hypoxic-Ischemic Encephalopathy
Considered a form of brain injury stemming from perinatal complications Acute placental bleeding or maternal conditions that contribute to placental insufficiency, umbilical cord accidents, abnormal fetal presentation, or prolonged late stages of labour are several factors that may be associated with a reduction in oxygen delivery to the fetus.
Sentinel events including maternal amniotic fluid embolism or uterine rupture are related to moderate or severe __________.
Total body therapeutic hypothermia
Total Body Therapeutic Hypothermia
Provides a mechanism for neuroprotection and reduces the severity of the brain injury in HIE, leading to improved neurological outcomes for many newborns.
Initiation of total body cooling needs to occur in the early stages of injury (first 6 hours after birth) for infants who meet all eligibility criteria
Eligibility Criteria for Total body therapeutic hypothermia
•Gestational age greater than 35 weeks
• Less than 6 hours postnatal age
• Cord or postnatal gas within 1 hour of birth with pH less than 7.0
OR base deficit greater than –16 OR
• APGAR score of 5 or less at 10 minutes and continued need for ventilation
or resuscitation at 10 minutes
• Signs of moderate or severe encephalopathy
Clinical Manifestations of Hypoxic Ischemic Brain Injury
Appears within first 6–12 hours after hypoxic episode
Seizures
Abnormal muscle tone (usually hypotonia)
Disturbance of sucking and swallowing
Apneic episodes
Stupor or coma
Muscular weakness in hips and shoulders (full term), lower-limb weakness (preterm)
Therapeutic Management of Hypoxic Ischemic Brain Injury
Prevent hypoxia.
Provide supportive care.
Provide adequate ventilation.
Maintain cerebral perfusion.
Prevent cerebral edema.
Treat underlying cause.
Administer antiseizure medications.
Initiate therapeutic hypothermia if criteria met.
Germinal Matrix or Intraventricular Hemmorrhage
Hemorrhage into and around ventricles caused by ruptured vessels as a result of an event that increases cerebral blood flow to area
Clinical Manifestation of Intraventricular Hemmorrhage
Most bleeds are initially asymptomatic.
Sudden deterioration in condition if bleed is large:
• Oxygen desaturation
• Bradycardia
• Hypotonia
• Metabolic acidosis
• Shock
• Significant drop in hematocrit
• Tense anterior fontanel
Signs of worsening
hemorrhage:
• Twitching
• Decreased level of
consciousness, stupor
• Apnea
• Seizures
• Full, tense fontanels
Evident on cranial
ultrasonography or
magnetic resonance
imaging
Therapeutic Management of Intraventricular Hemmorrhage
Provide supportive care.
Provide ventilatory support.
Maintain oxygenation.
Regulate fluid, electrolytes, acid–base balance.
Suppress or prevent seizures.
Provide ventricular shunting or drainage of cerebrospinal fluid
Care Management of Intraventricular Hemmorhage
Prevent increased cerebral blood pressure.
Avoid events that may increase or decrease cerebral blood flow (e.g., pain, unnecessary stimulation, endotracheal suctioning, hypoxia, hyperosmolar medications, rapid volume expansion).
Elevate head of bed 20–30 degrees; keep head in midline.
Support family.
Monitor for posthemorrhagic ventricular dilatation after diagnosis.
Provide developmental care and enhancement
What are the two types of newborn infections?
Early onset and late onset infections.
Early Onset Infections
Usually manifests within 72 hrs of birth and often within first 24 hrs of life.
Acquired by vertical transmission through amniotic fluid infection ir from bacterial flora within the mother’s anogenital tract during vaginal birth.
Caused by E-coli, S. aureus, enterococci, Klebsiella, Citrobacter, Enterobacterm, and Streptococcus viridians.
Other pathogens harbored in the vagina include gonococci, Candida albicansm, HSV type 2, and Chlamydia
Associated with Obstetric events such as preterm labour, prolonged rupture of membrane, maternal fever during labour and chorioamnioitis.
Late Onset Infections
Occurs after 72 hrs
Considered to be primarily an infection acquired through the infant’s environment.
Organisms include coagulase-negative staphylococci, Staphylococcus aureus, Klebsiella organisms, enterococci, Pseudomonas, and Candida species.
GBS and E. coli, also frequently identified in ____________, are commonly found to be the cause of septicemia in extremely-low-birth-weight (ELBW) and VLBW infants residing in the neonatal intensive care unit (NICU).
Most common Bacterial organism in preterm infants
E. Coli
Most common bacterial organisms in term infants
Group B Streptococci
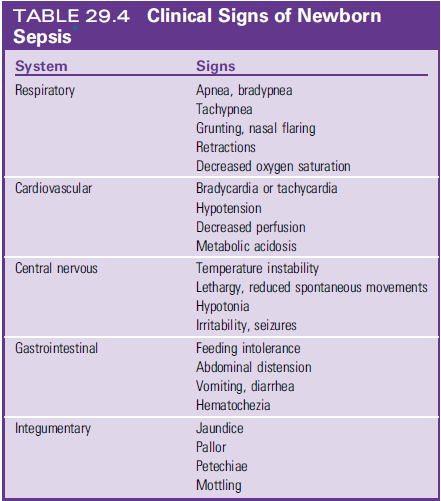
Earliest Clinical Signs of Newborn Sepsis
Characterized by lack of specificity
Lethargy, poor feeding, poor weight, and irritability.
The nurse/ parent may simply note that the newborn is not doing as well as before
Sequelae to Septicemia in Newborn
Icludes
Meningitis
Disseminated Intravascular Coagulation
Pneumonia
Septic Shock
Most Common Signs of Septic Shock
Decreasing oxygen saturation
Respiratory distress
Tachycardia
Evolving features of hemodynamic instability with reduced cardiac output (Prolonged capillary refill, cool extremities, motttling, reduced urine output)
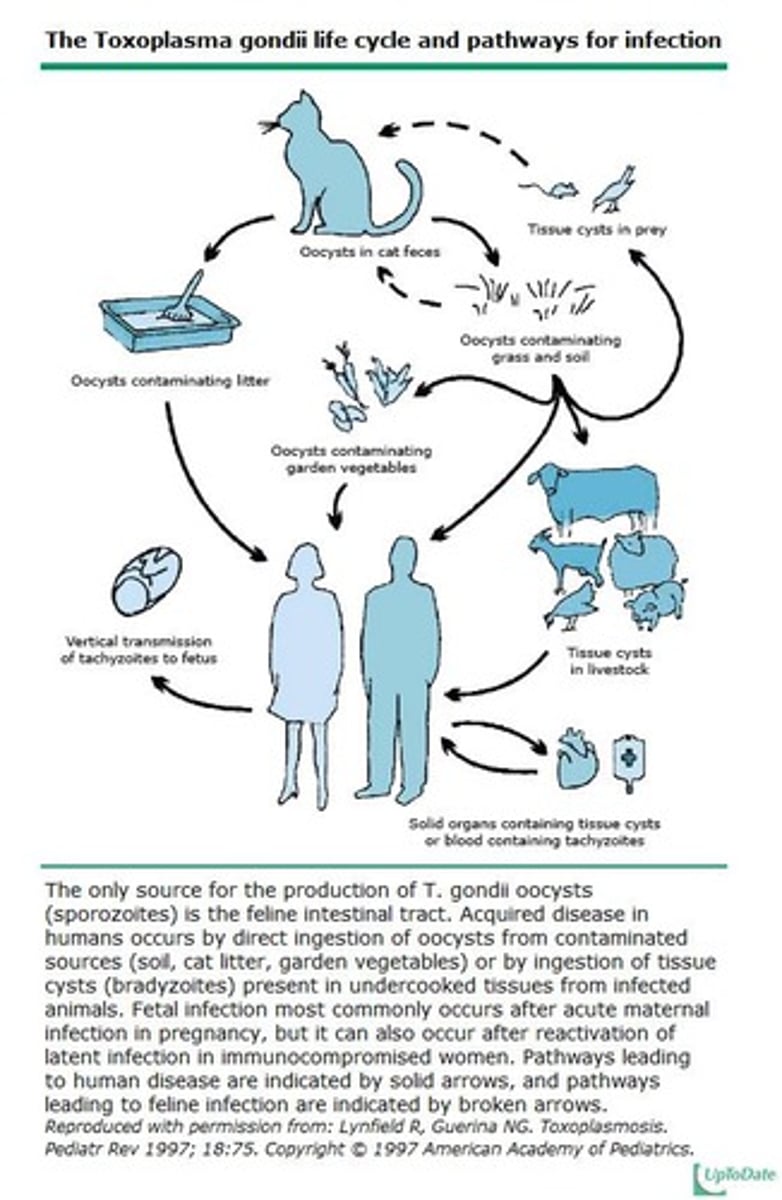
What is the TORCH complex?
Stands for a group of infectious diseases that may contribute to newborn illness and negative long-term sequelae
To determine the causative agent in a symptomatic newborn, tests are performed to rule out each of these infections. The O category may involve testing for several viral infections (e.g., HBV, varicella zoster, measles, mumps, HIV, syphilis, and human parvovirus).
Bacterial infections are not included in the TORCH workup because they are usually identified by clinical manifestations and readily available laboratory tests.
T
Toxoplasmosis
O
Other: HBV, Parvovirus, HIV, West nile
R
Rubella
C
Cytomegalovirus (CMV) Infection
Leading infectious cause of hearing impairment and cognitive delay in infants and children; there is no effective and safe immunization against CMV
Transmitted during the perinatal period
Newborns with congenital CMV may experience intrauterine growth restriction, microcephaly, hepatosplenomegaly, thrombocytopenia, and/or jaundice at birth.
Hearing impairment may not be apparent until after the first year of life
Approximately 20 to 30% of symptomatic infants will die of DIC and liver dysfunction

H
Herpes Simplex
What are the prevention methods for Toxoplasmosis?
Avoid consuming raw or poorly cooked meat, avoid contact with cat feces, and wash vegetables thoroughly.
What are the risks associated with Group B Streptococcus (GBS) in pregnant women?
Can cause urinary tract infections, chorioamnionitis, endometritis, pneumonia, and meningitis.
What is the significance of screening for Hepatitis B in pregnant women?
It allows for early intervention to prevent transmission to the neonate.
What is the risk of chronic Hepatitis B infection in neonates compared to adults?
90% risk in neonates versus 1-5% risk in adults.
What are the steps to prevent HIV transmission from mother to child?
Test mothers for HIV, start antiretrovirals if positive, manage delivery based on viral load, and administer AZT to the baby.
What are the classic symptoms of Congenital Rubella Syndrome (CRS)?
Deafness, cataracts, and cardiac lesions.
What is the most common congenital viral infection?
Cytomegalovirus (CMV).
What are the treatment options for neonatal herpes simplex virus (HSV) infection?
IV Acyclovir and supportive care.
What is the Finnegan Neonatal Abstinence Scoring System used for?
To assess the severity of neonatal abstinence syndrome (NAS) due to opioid exposure.
What are some common congenital anomalies in newborns?
Congenital heart disease, abdominal wall defects, imperforate anus, neural tube defects, cleft lip or palate, clubfoot, and developmental dysplasia of the hip.
What is the most common STI that can affect newborns?
Chlamydia trachomatis.
What are the potential effects of untreated syphilis in pregnant women?
High risk of congenital syphilis transmission, fetal death, and other complications.
What is the treatment for neonatal conjunctivitis caused by Neisseria gonorrhea?
Ceftriaxone or cefotaxime.
What is congenital varicella syndrome (CVS)?
A condition resulting from intrauterine exposure to varicella, affecting infants if maternal infection occurs close to delivery.
What are the features of congenital Zika syndrome (CZS)?
Microcephaly, incomplete brain development, increased muscle tone, club foot, and visual problems.
What is the primary treatment for congenital syphilis?
IV penicillin.
What are the non-pharmacological interventions for managing neonatal abstinence syndrome?
Reducing environmental stimuli, swaddling, rocking, feeding on demand, and clustering care.