CURRENT - bone, lung, lymph, thyroid, parathyroid, renal, cardiac, GIT
1/816
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
817 Terms
what are the functions of the lung?
works alongside airways, blood vessels and muscles to facilitate breathing
responsible for exchanging gases between air and blood
oxygen is absorbed into bloodstream and carbon dioxide is expelled
deoxygenated blood comes from the pulmonary artery (RIGHT VENTRICLE) and returns oxygenated via the pulmonary vein (LEFT ATRIUM)
what are the indications for lung scintigraphy? (3)
checking for presence of PE
checking for residual PE (follow up/resolution scan)
lung quantification
why might lung scintigraphy be used for lung quantification?
if the patient has a mass/section of the lung to be taken out, V/Q scan may be used to assess if the rest of the lungs are receiving sufficient air/blood flow to remove that segment of lung without dangerous effects
when might a department only do a perfusion scan for lung scintigraphy? (no ventilation)
if the patient has lung disease/infection - COVID, avoid contaminating Technegas machine if possible
what stimulates renin release? (3)
juxtaglomerular cells containing beta1 adrenergic receptors, which are activated in the sympathetic nervous system (fight or flight), causing renin release - increased blood pressure and fluid retention
juxtaglomerular cells detecting pressure changes in the afferent arteriole, where decreased pressure promotes secretion
macula densa cells acting as osmoreceptors, detecting low Na+, Cl- and water (suggesting low pressure and low GFR), encouraging renin secretion from juxtaglomerular cells
what old radiopharmaceutical was used for renal scintigraphy, and why was it stopped?
Iodine 131 hippuran / Iodine 123 hippuran
hippuran has a high extraction fraction first pass 85%, but poor image quality
80% tubular secretion, 20% glomerular filtration
what is the renin angiotensin aldosterone system RAAS?
liver produces angiotensinogen
kidneys detect low blood pressure
kidneys produce renin, which converts angiotensinogen to angiotensin I
lungs produce angiotensin converting enzyme ACE, which converts angiotensin I to angiotensin II (vasoconstrictor)
angiotensin II vasoconstricts → increased blood pressure
angiotensin II acts on adrenal glands, secretes aldosterone
aldosterone increases reabsorption of sodium and consequentially water → increased blood pressure
angiotensin II acts on anterior pituitary gland, secretes ADH → increased water reabsorption → increased blood pressure
why might CT be used in lung scintigraphy?
CT is used for anatomical correlation only, not attenuation correction
using CT on the lungs filled with air for the sake of attenuation correction can result in artefacts
what potential radiopharmaceuticals could be used for ventilation imaging in lung scintigraphy? (4)
99mTc Technegas
99mTc DTPA
133 Xenon gas
81m Krypton gas
why isn’t 133 Xenon gas used for ventilation imaging in lung scintigraphy?
complex delivery system, long half life 5.3 days
BUT biological half life 30 seconds - rapid washout hard to image
low photopeak 81keV - anterior image attenuation soft tissue
special equipment xenon trap, negative pressure room, external exhaust for radiation safety
what is ERPF?
renal plasma flow RPF is the volume of blood plasma passing through the kidneys per minute
ERPF, or Effective Renal Plasma Flow, refers to the volume of plasma effectively filtered by the kidneys per unit of time. It's a measure of kidney function. A healthy kidney should have an ERPF of at least 300 mL/min.
what is the normal time to peak in a normal kidney renogram?
3-5 minutes
what is the normal half peak clearance in a normal kidney renogram?
<10 minutes
what is the normal percent retention in a normal kidney renogram?
30%
why is CTPA contraindicated in patients with poor kidney function?
CTPA uses iodinated contrast, which can worsen kidney function, directly damaging renal cells, slowing GFR
Iodinated contrast agents, used in imaging procedures, can cause acute kidney injury (AKI), also known as contrast-induced nephropathy (CIN). While not a shock in the traditional sense of a sudden cardiovascular collapse, CIN can be a serious complication that can lead to prolonged renal dysfunction and even death in severe cases.
why isn’t 81m Krypton gas used for ventilation imaging in lung scintigraphy?
requires 81Rb/81mKr generator that is cyclotron produced - not available in Australia
81mKr has a 13second half life - requires modified acquisition technique
190keV photon requiring ME collimators
how can 99mTc DTPA be used for ventilation imaging in lung scintigraphy, and what is a negative for DTPA?
liquid DTPA can be aerosolised using nebulizer to produce nanoparticles 0.1-0.5micrometres
particles larger than 1-2 micrometres tend to settle out in large airways, limiting ventilation study quality - potentially “shining through” onto subsequent perfusion examination
respiratory airways order (10)
trachea →
main bronchi →
lobar bronchi →
segmental bronchi →
bronchioles →
terminal bronchioles →
respiratory bronchioles →
alveolar ducts →
alveolar sacs (clusters of grapes) →
individual alveoli (individual grapes)
what are the differences between left and right lung? (2)
left lung is smaller (heart sits more on the left) and has 2 lobes
right lung is larger and has 3 lobes
what are the standard radiopharmaceuticals used in lung scintigraphy?
Ventilation: 99mTc Technegas (particle diameter 5-200nm)
Perfusion: 99mTc MAA (macroaggregated albumin)
how is 99mTc Technegas produced for lung scintigraphy?
prepare carbon crucible with ethanol - reduces surface tension
add 99mTcO4 in 0.1-0.2mL (800MBq) - approximately 5-10% is delivered to patient (40-80MBq)
do not let pertechnetate to spill out of crucible - pertechnic gas can be produced creating artefacts
simmer for 6 minutes (70oC) with argon gas
burn crucible at 2500oC - 10 minute window to use Technegas machine
ventilate patient
what is the importance of 99mTc MAA’s particle size in lung scintigraphy?
99mTc MAA maps pulmonary blood circulation, particle size important
too large → block arterioles, gives impression of false positive PE
too small → pass through capillaries, no embedding
what is the typical administered activity of 99mTc Technegas for lung scintigraphy?
usually delivers around 20-40MBq to patient, but ~800MBq is burnt in Technegas machine
what is the typical administered activity of 99mTc MAA for lung scintigraphy?
150-220MBq
what is the count target of 99mTc Technegas for lung scintigraphy?
0.8-1.5k counts
most common target 1k counts
what is the count target of 99mTc MAA for lung scintigraphy?
4-5k counts
what is the required particle number of 99mTc MAA for lung scintigraphy?
200,000-700,000
what is the required particle size of 99mTc MAA for lung scintigraphy?
10-70 micrometres
when should the 99mTc MAA dose be reduced in lung scintigraphy? (4)
pregnant,
child,
right to left cardiac shunt → particles can enter systemic circulation to brain → stroke
pulmonary hypertension → too many capillaries blocked, respiratory distress
how is 99mTc Technegas administered in lung scintigraphy?
Technegas is inhaled using a tube → make sure patient practices breathing - requires a nose clip, or get patient to pinch their nose put patient under scanner to check if their count rate is sufficient (1-2k counts/sec) → if not, breathe more gas in
how is 99mTc MAA administered in lung scintigraphy?
injected intravenously to get embedded into capillary beds
how does 99mTc Technegas localise in the body in lung scintigraphy?
99mTc Technegas is a micro aerosol → C60 carbon atoms surrounding a 99mTc atom
Technegas enters alveoli and is trapped in alveoli walls, gets stuck in surfactant → doesn’t enter bloodstream or get exhaled
Technegas is a Tc99m labelled solid graphite particle in argon carrier gas
no clumping compared to 99mTc DTPA
how does 99mTc MAA localise in the body in lung scintigraphy?
travels through blood stream, gets embedded in pulmonary capillary beds due to its size (particle size 10-90 micrometres) compared to capillary bed size 7-8 micrometres
what is the imaging protocol for ventilation in lung scintigraphy?
a. multiple statics - anterior, RAO, R lat, LPO, posterior, LPO, L lat, LAO → 150k counts/image OR 180 seconds (256x256)
b. SPECT 20secs/frame, 64 frames (32 each head) (128x128) → CT only needed for calculations, not for checking for PE
arms up to reduce attenuation artefacts
what is the imaging protocol for perfusion in lung scintigraphy?
a. multiple statics - anterior, RAO, R lat, LPO, posterior, LPO, L lat, LAO → 500k counts/image OR 120 seconds (256x256)
b. SPECT 10-15secs/frame, 64 frames (32 each head) (128x128) → CT only needed for calculations, not for checking for PE
arms up to reduce attenuation artefacts
what does an optimal lung scintigraphy image look like?
we want homogenous distribution of radiopharmaceutical, but it may be hotter at the base due to gravity, distribution should be matched but oesophageal and stomach activity could be due to swallowing of Technegas
Checking for mismatch of lobes between perfusion and ventilation scan → wedge shaped defects → if there is a cold spot in perfusion where ventilation is normal, it could be acute PE
what is the history of interest for a lung scintigraphy patient? (12)
chest pain,
shortness of breath,
blood thinners,
recent infections regarding lungs,
previous surgery,
long haul flights,
smoking,
history of deep vein thrombosis (DVT),
pregnancy or breastfeeding,
history of cancer,
right to left cardiac shunt (particles can get stuck into brain systemic capillaries → stroke),
pulmonary hypertension (can lead to complete blockage of pulmonary capillaries → respiratory distress),
what is a pulmonary embolism?
when one or more arteries are blocked by a blood clot
what is deep vein thrombosis?
most common source of clots that lead to PE → blood clot (thrombosis) formed in a deep vein → femoral, popliteal or calf vein → most common causes are related to damage to vessel wall, hypercoagulability of blood, regional haemostasis
what are the causes of deep vein thrombosis? (9)
immobility,
medical conditions,
surgery,
pregnancy,
obesity,
smoking,
hormone therapy,
genetic predispositions,
increased d-dimer
what is d dimer and what does increased d dimer mean?
d dimer is a fibrin degradation product → elevated levels suggest presence of abnormal blood clotting process
tested in blood test
negative result excludes presence of blood clot (except patients > 80y/o)
positive result does not confirm a DVT but requires further investigation
what are the causes of increased d-dimer? (7)
malignancy/cancer
trauma
hemorrhage
severe infection/sepsis
autoimmune disorders
COVID-19
DVT(?)
what is the process of a pulmonary embolism occurring?
clot formation begins in deep veins of legs or pelvis → embolisation where clot travels through bloodstream to lungs → blocks pulmonary arteries, impeding blood flow → body reacts with inflammatory responses leading to increased pulmonary vascular resistance and decreased tissue damage → can lead to right heart failure, hypoxemia, sudden death
what does a pulmonary embolism look like in a lung scintigraphy scan?
acute PE perfusion scan shows segmental or subsegmental photopaenic defects, not matched to ventilation study
preserved air flow but blocked blood flow
what does pneumonia look like in a lung scintigraphy scan?
presents as matching defects
inflammation and fluid associated can impair air and blood flow
what is atelectasis?
collapse of alveoli caused by obstruction of airways, compression of lung from air or fluid in pleural space or pressure of tumour outside lung
what does atelectasis look like in a lung scintigraphy scan?
presents as matching defects
what is COAD?
chronic obstructive airways disease
diseases affecting the tubes that carry oxygen and gases into and out of the lungs
preserved blood flow in early disease but blocked/reduced air flow
advanced COPD can result in reduced or abolished function of both air and blood flow
what are the types of COAD? (3)
emphysema
chronic bronchitis
asthma
what is emphysema?
destruction of alveolar walls, traps air in large air sacs → lungs can inflate but do not recoil as well → alveoli collapse → large air sacs get larger, functional alveoli diminish
what is chronic bronchitis?
inflamed bronchial tree, excess mucus production
what does COAD look like in a lung scintigraphy scan?
acute can present as preserved blood flow in early disease but blocked/reduced air flow
advanced can present as matching defects
what is a right to left cardiac shunt?
can see 99mtc MAA in systemic circulation → kidneys, brain → deoxygenated blood recirculates systemically, resulting in low blood oxygen
what is a lung tissue disease?
diseases affecting structure of lung tissue → scarring or inflammation prevents lungs from expanding fully (restrictive lung diseases)
what are the types of lung tissue diseases? (3)
pulmonary fibrosis
cystic fibrosis
sarcoidosis
what is a lung circulation disease?
diseases affecting blood vessels in the lungs → caused by clotting, scarring, inflammation of blood vessels
affects ability of lungs to take up oxygen and release carbon dioxide
what are the types of lung circulation diseases? (3)
pulmonary hypertension
pulmonary oedema
pulmonary embolism
what is lung cancer?
disease caused by uncontrolled cell division in the lungs affecting airways, lung tissue and lung circulation
what is hemostasis?
the physiological process that stops bleeding at the site of an injury while maintaining normal blood flow elsewhere in the circulation
what is the process of hemostasis? (5)
vasoconstriction
platelet plug
coagulation cascade
clot retraction and repair
fibrinolysis
what is CTPA?
Computed Tomography Pulmonary Angiography
specialised imaging technique primarily for diagnosis of pulmonary embolism
advanced imaging method
combines x ray imaging technology with computer processing
generate detailed cross sectional image of the lung’s blood vessels
what are the potential PE treatments? (4)
anticoagulants (warfarin, heparin, aspirin)
thrombolysis (clot dissolving medications)
embolectomy (surgical removal of blood clot)
IVC filter (filter in inferior vena cava to catch blood clots before reaching lungs)
what is the function of the parathyroid hormone?
responsible for calcium homeostasis
works in opposition to calcitonin that decreases blood calcium levels
parathyroid hormone increases blood calcium levels
how does parathyroid hormone increase calcium levels? (3)
parathyroid hormone inhibits osteoblastic activity → increases cytokine release → promotes osteoclast formation → increased bone breakdown → increased calcium phosphate in blood
parathyroid hormones inhibit reabsorption of phosphate in kidneys and increases calcium reabsorption → increased phosphate excretion in urine → increased calcium, decreased phosphate
parathyroid hormone promotes formation of calcitriol hormone (active form of vitamin D)
calcitriol from kidneys travels to gastrointestinal tract → increases dietary calcium absorption
what is the structure of the parathyroid gland?
4 parathyroid glands embedded partially posteriorly in the lobes of the thyroid gland
usually one superior and one inferior gland attached to each lateral thyroid lobe ectopic and additional glands can exist
how does the parathyroid gland develop?
parathyroid gland develops at the same level as the tongue → tongue grows, parathyroid glands descend downwards to behind the thyroid gland
what are some developmental issues with the parathyroid gland?
incomplete or excessive migration can lead to ectopic tissue
inferior parathyroid glands are more likely to be ectopic as they have a greater distance to travel
inferior parathyroid glands develop in a similar position to the thymus and can be embedded within the thymus (intra thymus)
excessive migration → superior mediastinal (upper chest) or pericardiac (around the heart) ectopic tissue
what cells are found in the parathyroid gland?
chief cells and oxyphil cells
what do chief cells do in the parathyroid gland?
synthesise and release parathyroid hormone
what are oxyphil cells in the parathyroid gland?
unknown function of oxyphil cells but are larger than chief cells and contain high numbers of mitochondria → in abnormal glands, oxyphil cells can secrete excess parathyroid hormone
what radiopharmaceuticals are used in parathyroid scintigraphy?
99mTc sestamibi and sometimes 99mTc pertechnetate
what is the purpose of 99mTc pertechnetate in parathyroid scintigraphy?
99mTc pertechnetate can be used to identify thyroid outline → used as subtraction to identify clear parathyroid
what is the administered activity of 99mTc sestamibi in parathyroid scintigraphy?
600-800MBq
what is the administered activity of 99mTc pertechnetate in parathyroid scintigraphy?
~50MBq
how are radiopharmaceuticals administered for parathyroid scintigraphy?
intravenous, potentially use cannula for dual radiopharmaceutical to avoid multiple injections for patient
how does 99mTc sestamibi localise in the body in parathyroid scintigraphy?
99mTc sestamibi is lipophilic and a cation (positively charged)
uptake is high in metabolically active cells with high mitochondria counts (negatively charged)
uptake in any tissue that is mitochondrial rich including cancers
retention dependent on negative electric potentials → mitochondria maintain a highly electronegative potential across inner membrane when metabolically active → good retention of 99mTc sestamibi
oxyphil cells have high mitochondria → good uptake and retention
uptake also occurs in thyroid → difficult to differentiate → sestamibi has greater retention in hyperfunctioning parathyroid glands than thyroid tissue → 10-15 minutes after injection allows sestamibi to wash out from thyroid but retain in parathyroid
peak uptake in parathyroid at 5 minutes but uptake in thyroid is also high → washout from thyroid begins at 10 minutes → complete washout from thyroid at 2-4 hours
what patient preparation is needed for parathyroid scintigraphy?
neck extended using cushion or towel for better view of parathyroid, no mixing up of salivary glands and neck immobilise head gently
drink water before scanning
what is the dual phase 99mTc sestamibi imaging protocol for parathyroid scintigraphy?
early static imaging at 10-15 minutes post injection → early anterior static 300-500kcounts or 5-10 minutes (128x128 or 256x256)
delayed static at 2-3 hours post injection → delayed anterior static 300-500kcounts or 5-10 minutes (128x128 or 256x256)
SPECT/CT can occur during early or delayed imaging or both → 15-25 sec/view 60-120 views (128x128)
what is the dual radiopharmaceutical imaging protocol for parathyroid scintigraphy?
pertechnetate injection and early imaging 10-20 minutes post injection → 300-500k counts or 5-10 minutes 128x128 or 256x256
sestamibi injection and early imaging 10-15 minutes post injection → 300-500kcounts or 5-10 minutes (128x128 or 256x256)
DO NOT MOVE PATIENT BETWEEN IMAGES TO ALLOW FOR SUBTRACTION
delayed static 2-3 hours post injection → 300-500k counts or 5-10 minutes (128x128 or 256x256)
SPECT/CT can occur early and/or delayed → 15-25 sec/view 60-120 views (128x128)
how do we analyse dual phase 99mTc sestamibi images in parathyroid scintigraphy?
compare early and delayed images → 99mtc sestamibi uptake occurs in thyroid gland in early imaging
thyroid adenomas can accumulate and retain 99mtc sestamibi
how do we analyse dual radiopharmaceutical images in parathyroid scintigraphy?
use digital subtraction or compare visually complete or partial washout of thyroid gland can be seen on delayed imaging abnormal parathyroid tissue shows increased sestamibi uptake persisting after subtracting thyroid tissue
tc99m sestamibi - tc99m pertechnetate = hyperfunctioning parathyroid tissue only
what is the history of interest for a parathyroid scintigraphy patient?
99mTc pertechnetate
blood tests? check for medications regarding thyroid or anything with iodine → hypothyroidism hormone medications, antithyroid hormone medications for hyperthyroidism, CT scans with iodine, iodine vitamin, supplements, medications, recent
cold or flu, cough? check for breastfeeding, if yes avoid
99mTc sestamibi
may be recommended to cease calcimimetics, calcium supplements and vitamin D therapy for 1-4 weeks for improved sensitivity
what is hyperparathyroidism?
high secretion of PTH
leads to hypercalcaemia (calcium levels are too high)
normal PTH levels 1-7pmol/L
abnormal increase in calcium reabsorption in kidneys, increased absorption of calcium in gastrointestinal tract
what is primary hyperparathyroidism?
abnormality in parathyroid gland itself → adenoma (85%) or hyperplasia (15%) → abnormal increase in number and function of osteoclasts → osteoporosis
what is secondary hyperparathyroidism?
over secretion of PTH in response to abnormally low calcium due to other pathologies → renal failure, gastrointestinal malabsorption, vitamin D deficiency
what is tertiary hyperparathyroidism?
continuous PTH secretion even after secondary hyperparathyroidism condition is resolved
what are the causes of primary hyperparathyroidism? (3)
parathyroid adenoma
parathyroid carcinoma
parathyroid hyperplasia
what is a parathyroid adenoma?
benign non cancerous tumours which are a result of abnormal cell growth and proliferation (usually chief cells, but can also be oxyphil cells)
what is a parathyroid carcinoma?
malignant, very rare, 1%, can be either cell or mixed composition, autonomous function, likely to cause symptomatic hyperparathyroidism
what is parathyroid hyperplasia?
hyperplasia and/or hypertrophy, most commonly chief cells, often a multi gland disease with all 4 glands becoming overactive, most commonly due to overgrowth of normal tissue in response to chronically reduced calcium levels by untreated secondary conditions (aka tertiary hyperparathyroidism) → overcompensation becomes permanent
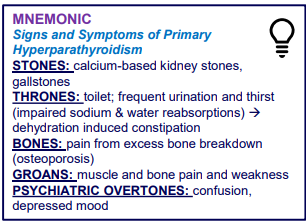
MNEMONIC FOR PRIMARY HYPERPARATHYROIDISM
what is hypoparathyroidism?
PTH secretion too low
results in hypocalcaemia
normal PTH levels 1-7pmol/L
what are the causes of hypoparathyroidism? (3)
most commonly due to accidental removal or damage of parathyroid glands during thyroid surgery, but can also be caused by autoimmune disorders or congenital abnormalities
what are the symptoms of hypoparathyroidism?
can result in cardiac arrythmias or osteopenia, spontaneous firing of neurons, muscular dysfunction (all require calcium)
what are the functions of thyroid hormone? (3)
thyroid hormone raises basal metabolic rate → increases metabolism → increased breakdown of carbohydrates, lipids, proteins
thyroid hormone increases beta adrenergic receptors → increased and more forceful heart rate, increased blood pressure and vasodilation
thyroid hormone allows for bone growth and development through osteoclast and osteoblast activity activation
what is the negative feedback loop of thyroid hormone production?
hypothalamus releases thyrotropin releasing hormone → anterior pituitary releases thyroid stimulating hormone → thyroid gland releases thyroid hormone
how does the thyroid gland develop?
first endocrine developed during foetal growth at base of tongue → as tongue grows, thyroid gland descends to neck, connected to tongue via thyroglossal duct that degenerates
what is the structure of the thyroid gland?
endocrine gland inferior to the larynx and above the sternum
consists of 2 lateral lobes either side of the trachea, connected by the isthmus
what are some formation issues with the thyroid gland?
incomplete degeneration of thyroglossal duct leads to pyramidal lobe (50% of people)
failure of descent or excessive migration leads to ectopic tissue (outside normal anatomic position)
excessive migration at any level behind the sternum is called retrosternal thyroid tissue
what cells are found in the thyroid gland?
follicular cells and parafollicular cells (c cells)