OCTH 246 Final Exam
1/296
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
297 Terms
Tetraplegia
Quadriplegia
The paralysis (of any degree) of all four limbs and trunk.
Cervical injury to vertebrae C1-C7 (spinal nerves C1-8).
Paraplegia
Paralysis of LE's with involvement of trunk or hips (depending on level of lesion).
Thoracic injury to vertebrae T1-T12, lumbar injury to vertebrae L1-L5, and lumbo-sacral canal injury (cauda equina syndrome).
Spinal cord injury
Injury to the spinal cord or spinal nerve roots that results in temporary or permanent change in an individual's motor, sensory, and/or autonomic function.
Common causes: Car accidents, falls, violence, sports injury, medical/surgical complications
Average age: 47 years
Happens more to males > females
Typical LOS in rehab: 31 days. Discharged to home or SNF
40-45% will require some assistance with ADLs after discharge
Types of injuries that result in SCI:
- Transient concussion - Transient disturbance of SC function, w/ or w/o vertebral damage or no demonstrable pathological changes. Resolves w/in 48 hrs, extreme vibration, no neuropathic changes
- Laceration - Stabbing or broken spinal bones, bone fragments
- Compression of the cord substance - Swelling or anoxia
- Transection of cord - A tear w/in the SC as a result of a sig traumatic injury
- Contusion - Bruising w/ bleeding, leads to edema, ischemia, and hypoxia
Level of injury
Damage to cord usually occurs between two vertebrae. Spinal nerves exist cord above the area where vertebrae meet and are "spared". For C5-C6 injury, muscle and sensory areas innervated at C6 and above would be functioning. Most common cervical spine injury at C5-6.
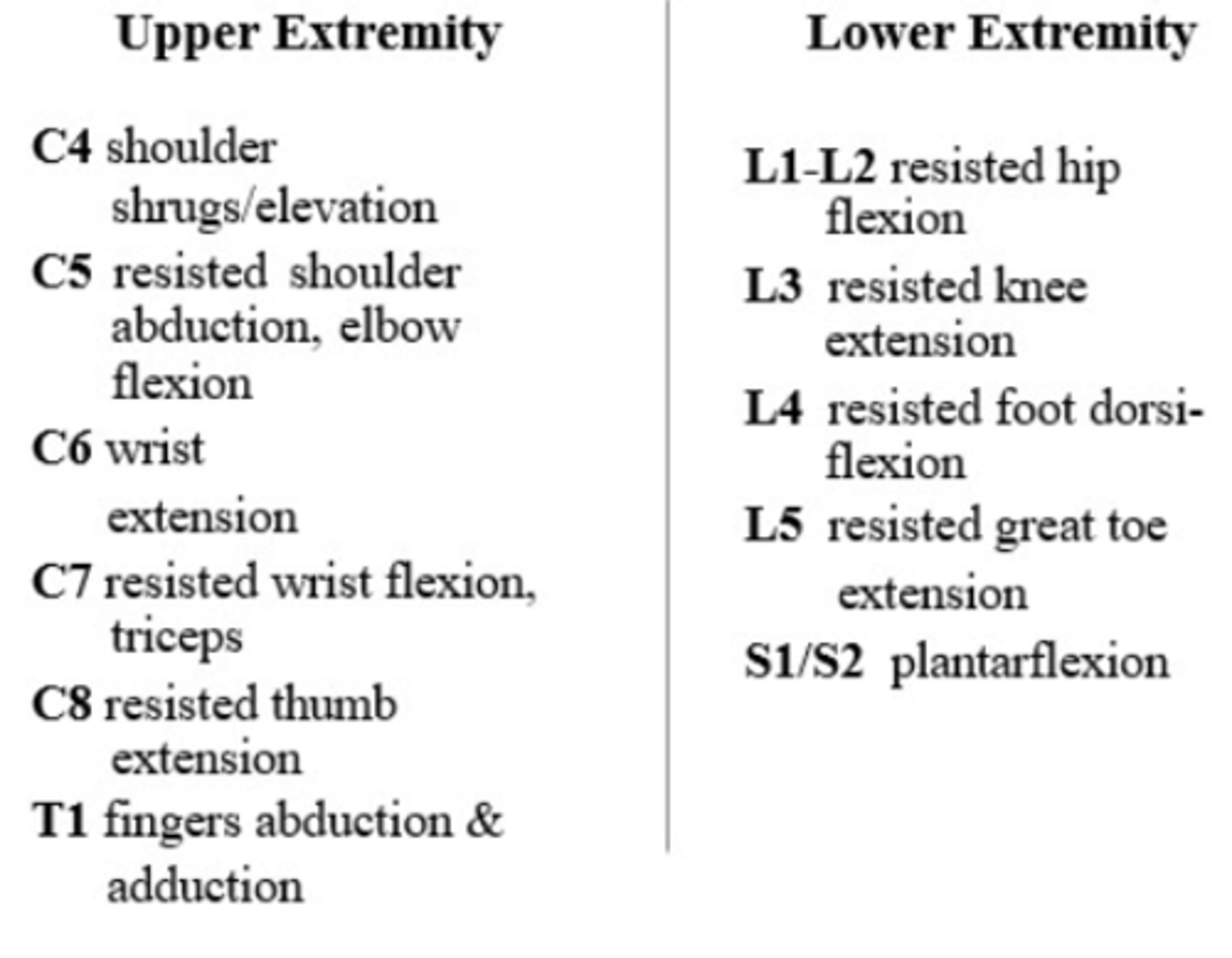
Quick Muscle Screen
Complete vs. incomplete injuries
Determined based on whether the individual has voluntary motor control or sensation in the anal area (S4-S5 segments of the spinal cord).
Complete injuries: Total paralysis and loss of sensation in all ascending and descending spinal tracts below level of injury
Incomplete injuries: Some preservation of sensory or motor nerve pathways below the level of lesion.
ASIA Impairment Scale (AIS)
American Spinal Cord Injury Association neurological classification system used to determine level of impairment to the spinal cord after an injury.
Results are based on:
• sensory testing of each dermatome for right and left sides
• manual muscle testing for right and left sides
AIS A SCI
Complete SCI
No motor or sensory function is preserved at S4-S5. May have preservation of strength or sensation below the neurological level of injury - referred to as the zone of partial preservation (ZPP)
AIS B SCI
Incomplete SCI
Sensory incomplete; indicates that there is sensation, but not motor control, below the neurological level of injury, including at S4-5.
AIS C SCI
Incomplete SCI
Motor incomplete; indicates that there is motor function preserved below the neurological level of injury; and more than half of the key muscles below the neurological level have a muscle grade of < 3 (Fair)
AIS D SCI
Incomplete SCI
Motor incomplete; indicates that there is motor function preserved below the neurological level of injury, and more than half of the key muscles have a muscle grade of 3 (Fair) or more
AIS E SCI
Incomplete SCI
Indicates that the individual tests as having normal sensation and motor control
Central Cord Syndrome (CCS)
Most common incomplete SCI, which occurs when there is more damage in the center of the cord than in the periphery. Damage is most frequently a result of a cervical hyperextension injury (such as falls).
Symptoms: Paralysis that is greater in the hands and arms than in the trunk and legs; bladder dysfunction; sensory loss below the level of injury; painful sensations - tingling, burning, dull aching
Common causes: Posttraumatic contusion and syringomyelia, and intrinsic spinal cord tumors
Brown-Sequard Syndrome (Lateral Damage)
Results when only one side of the cord is damaged, as in a stabbing or gunshot injury. Motor paralysis and deficits in kinesthesia (awareness of body positioning and movement) and proprioception occur below the level of injury, on the ipsilateral side. Loss of pain, temperature, and touch sensation occurs on the contralateral side.
Common causes: Penetrating injuries, lateral compression from tumors, and MS
Anterior Spinal Cord Syndrome
Results from injury that damages the anterior spinal artery or the anterior aspects of the cord. Involves paralysis and loss of pain, temperature, and touch sensations. Proprioception is preserved.
Common causes: Anterior spinal artery infarct, trauma, and MS
Posterior Spinal Cord Syndrome
Results from injury that damages the posterior spinal artery or the posterior aspects of the cord. Involves impairments of proprioceptive and vibration sense, two-point discrimination, and to a more variable extent, sense of deep touch and pressure below the level of injury
Conus Medullaris Syndrome
Involves injury of the sacral cord (conus) and lumbar nerve roots within the neural canal, which usually results in an areflexic bladder, bowel, and lower extremities
Cauda Equina Syndrome
Involve peripheral nerves rather than directly involving the spinal cord. Usually occurs with fractures below the L2 level. Results in a flaccid-type paralysis. This injury is associated with a better prognosis for recovery (peripheral nerves possess a regenerating capacity that the cord does not). Patterns of sensory and motor deficits are highly variable and asymmetric
Medical and surgical management of SCI
When someone is injured, they need immediate emergency services, which consists of spinal stabilization, airway and ventilation support if needed, treatment/management of associated trauma, and treatment of spinal shock signs. Then, a neurological assessment is performed (consists of physical exam, MRI, and CT). Finally, surgery is done for spinal decompression, realignment, and stabilization
Orthosis
A brace that is used to stabilize the spinal column to promote healing at the injury site and support the affected body parts for functional rehabilitation. There are different types of braces, depending on the type of injury
Spinal shock
Occurs around 24 hours to about 6 weeks post injury. Bowel and bladder atonic, deep tendon reflexes are decreased, sympathetic functions disturbed (low BP, decreased HR, no perspiration below level of lesion). Follow spinal shock, patient may develop hyperactive DTR, spasticity, muscle spasms. This is due to loss of CNS inhibition to reflex arc
Bowel and bladder function for people with SCI
Spastic bladder and bowel in injuries above T12 (refers to sphincters and muscle). Flaccid bowel and bladder in injuries at L1 and below.
Pressure injury
One type of complication that can occur with SCI patients. A pressure injury is localized damage to the skin and/or underlying soft tissue usually over a bony prominence or related to a medical or other device. Skin may be intact or have open ulcer. May or may not be painful. Results from intense and/or prolonged pressure or pressure in combination with shear. Tolerance of soft tissue for pressure and shear may also be affected by microclimate, nutrition, perfusion, co-morbidities and condition of the soft tissue.
At-risk factors: Sitting too long on skin
What makes it worse: Under/overweight, heat, shearing on skin
Orthostatic hypotension
One type of complication that can occur with SCI patients. Sudden decrease in BP, usually positional. Due to loss of muscle tone in abdomen and LE.
Symptoms: Dizziness, nausea, loss of consciousness, "can't see", "see stars"
Treatment: Recline person, elevate feet
Prevention: Abdominal binder, compression stockings, ace wrap LE before sitting up. Sit up gradually
Autonomic dysreflexia
One type of complication that can occur with SCI patients, considered a medical emergency. Reflex reaction of ANS in response to bladder or bowel irritation, injury, pain stimulus. HIGH BP LOW HR
Symptoms: Severe headache, perspiration, chills, nasal congestion, face reddened (sometimes only one side), anxiety, tachycardia
Treatment: Immediately keep patient upright, remove restrictive clothing, drain urinary catheter or check for other physical problems
Decreased vital capacity
One type of complication that can occur with SCI patients. Seen in cervical and high thoracic injuries. Limited chest expansion and decreased ability to cough.
Symptoms: Decreased overall endurance
Risk: Respiratory infections
Treatment: Good pulmonary "toilet", avoid infections, flu vaccine
Heterotopic ossification
One type of complication that can occur with SCI patients.
Ectopic bone - bone that forms in abnormal locations, such as soft tissue around hip and knee, sometimes elbow.
Early signs/symptoms: Swelling, warmth, decreased ROM
Treatment: Medications (cautious PROM), surgery (often recurs)
Osteoporosis
One type of complication that can occur with SCI patients. Decrease in bone density or mass. Increased risk of bone fracture, deformity, and loss of height. In SCI, due to loss of weight-bearing and pull on the bone. Prevention influences weight bearing in standing frames or braces.
C1-C4
Innervation: C1-C3 innervates neck muscles; C4 innervates with diaphragm.
Movement: Neck flexion, extension, and rotation; scapular elevation; inspiration.
Weakness: Paralysis of trunk, UE/LE; inability to cough; endurance and VC low; may require ventilator.
Functional outcomes: Will be dependent on almost everything, including toileting, bathing, grooming, driving. Can become independent in communication and mobility of powered wheelchair using face, lips, and chin control and adapted equipment.
Equipment: Powered wheelchair with recline/tilt. Should have cushions/padding and headrest. Transfer lifts, ventilators, speech devices, orthosis for positioning.
C5
Innervation: C5 innervates with deltoid (shoulder)
Movement: Shoulder flexion, abduction, extension; elbow flexion; supination; scapular adduction and abduction
Weakness: Absent elbow extension, no pronation, no wrist and hand movement. Total paralysis of trunk and LE; elbow contractures (results in loss of motion and difficulty performing ADLs)
Functional outcomes: Requires assistance for grooming, bathing, and toileting. Requires assistance w/ UE dressing and dependent for LE dressing. Can feed, dress, and use phone, computer, and write with adapted equipment. Can drive with specially adapted van.
Equipment: Powered w/c, U-cuff, mobile arm support, UE positioning orthosis, dorsal cock-up splint, MAS
C6
Innervation: C6 innervates with the wrist
Movement: Scapular protraction, some horizontal adduction, supination, radial wrist extension
Weakness: Absent wrist flexion, no elbow extension, no hand movement, total paralysis of trunk and LE, presence of tenodesis
Functional outcomes: Some assist with meal preparation. Total assist for all other homemaking. Independent for bowel routine, but may need some assistance. Independent driving in adapted vehicle and may need assistance for w/c loading. Can use communication devices with adapted equipment. Can be independent w/ adapted equipment for feeding and grooming. Independent w/ UE dressing, but assistance needed for LE dressing. May require some assistance w/ UE and LE bathing w/ adapted equipment
Equipment: W/c - light, adjustable; tenodesis splint; orthosis focused on wrist; bladder management through catheters
C7 and C8
Innervation: C7 innervates triceps. C7 and C8 innervates fingers
Movement: Elbow extension, ulnar wrist extension, wrist flexion and extension, thumb flexion/extension/abduction.
Weakness: Paralysis of trunk and LE, limited grasp, release and dexterity secondary to partial intrinsic muscles of the hand
Functional outcomes: Independent light meal prep and homemaking, some to total assistance for complex meal prep and heavy housecleaning. Independent w/ driving, but need to take precautions about risk factors and use adapted vehicle. Independent in feeding, grooming, dressing, and toileting. Independent w/ equipment for bathing.
For C7 - independent in use of communication devices
Equipment: Manual w/c on level/unlevelled surfaces. Transfer bath bench. Adaptive aids for bowel management. Adapted vehicle. C7 may use short opponens orthotic device
T1-T9
Innervation: T1 innervates hand. T2-T12 innervates intercostals (trunk). T7-L1 innervates abdominals.
Movement: UE fully intact. Limited trunk stability. Endurance increased secondary to innervation of intercostals.
Weakness: Lower trunk paralysis. Total LE paralysis. Decreased balance
Functional outcomes: Independent w/ driving, but need to take precautions about risk factors and use adapted vehicle. Independent in communication, feeding, grooming, dressing, and toileting.
Equipment: Can use manual w/c on level/unlevelled surfaces
T10-L1
Innervation: T2-T12 innervates intercostals (trunk). T7-L1 innervates abdominals. T11-L2 innervates ejaculation.
Movement: Good trunk stability
Weakness: Paralysis of LE
Functional outcomes: Independent w/ driving, but need to take precautions about risk factors and use adapted vehicle.
Independent in communication, feeding, grooming, dressing, and toileting. Independent w/ bathing w/ equipment.
Equipment: Orthosis (only for T8-L3): KAFO w/ forearm crutches or walker. Independent at w/c level; possible ambulation
L2-S5
Innervation: L2 innervates ejaculation and hips. L3 innervates quadriceps. L4-L5 innervates hamstrings - knee. L4-S1 innervates foot. S2 innervates penile erection. S2-S3 innervates bowel and bladder
Movement: Partial control of LE (wide range of ambulation potential)
Weakness: Partial paralysis of LE, hips, knees, ankles, foot
Functional outcomes: Independent w/ driving, but need to take precautions about risk factors and use adapted vehicle
Independent in communication, feeding, grooming, dressing, and toileting. Independent w/ bathing w/ equipment
S2 and below is independent in all ADLs listed.
Equipment: Orthosis (only for L4-S1: AFO w/ forearm crutches or walker
Transfer lift
Equipment designed to assist in lifting and transferring users with mobility problems.

Benefits & influences on leisure participation
Psychosocial
- Increased sense of self-worth
- Experience of choice
- Increased socialization, opportunities for friendship
- Skill development (coping, attention span, interpersonal, etc.)
- Increased tolerance of groups, others
- Intellectual stimulation, creativity
- Stress reduction
- Opportunities for leadership
- Release of hostility/aggression
Physical
- Motor skill development
- Vestibular/other sensory stimulation
- Strength, ROM, endurance
- Balance
- Cardiovascular
- Opportunities for grading activities
Influences on leisure choice: Culture, ethnicity, gender, age, rural/urban, cost, physical/cognitive abilities, family participation, weather, climate, etc.
Consequences of injury or illness on client and leisure participation
- People with disabilities are less likely to engage in leisure activities after therapy is over
- Social isolation
- Changes in relationships
- Lack of ability to perform preferred activities (cognition/physical)
- Difficulty traveling
- Inability to creatively express self
- Feeling less "capable"
- Money
- Time
- Depression
Leisure evaluation and intervention
Evaluate for following information in order to determine leisure areas:
- Demographic
- Social history
- Education history
- Occupational history
- Military involvement
- Community and spiritual engagement
- Typical routines
- Interest and hobbies
- Mealtime interests
- Abilities - sensory-motor, cognitive, psychosocial
Leisure interest assessments
- Occupational profile
- COPM
- Role checklist
- Activity Card Sort
- Play and Laughter Assessment
- Modified Interest Checklist
- Leisure Attitude Measurement Scale
- Leisure Motivation Scale
- Quality of Life Scale
OT intervention:
Therapeutic use of leisure that is motivating and fun (as a means); voluntarily engaging in leisure occupations after therapy intervention is over (as an ends)
Social isolation and disability
Adults with chronic disabilities have fewer opportunities to form meaningful relationships. Primarily interact with family members, caregivers, or health professionals. Loneliness can negatively affect mental and physical health (depression, anxiety, low self-esteem)
Role of OT in social participation
Education and training: Education about social norms and roles and social skills training for lifelong adaptation and success in social participation.
Consultant: Enhance performance of client or organization. Services may be direct or indirect.
For people w/ disabilities:
Sensitivity to cultural, physical, social, personal, temporal, and virtual contexts and environments. Includes habits, roles, routines, and rituals. Direct services include screening, formal assessment, intervention plan development, discharge planning, education, and implementation of maintenance plan that matches client's purpose.
Sleep
State characterized by changes in brain wave activity, breathing, heart rate, body temperature, and other physiological functions. Period of reduced activity, associated w/ posture (lying down, eyes closed for humans). Decreased responsiveness to external stimuli. Easily reversible (as differentiated from hibernation or coma).
Benefits of sleep
Increased alertness, energy, happiness; ability to function; improved mood
- Restorative benefits - muscle growth, tissue repair, protein synthesis, growth hormone release occur mostly during sleep. Body clears adenosine accumulation from cells
- Brain plasticity - critical role for development in infants and children, helps with learning and consolidation of memory and forgetting (arguments for both REM and non-REM sleep being involved in memory)
Drowsiness
Last step before falling asleep, may indicate that you are seconds from a disaster (i.e., car accidents)
Health and personal consequences of insufficient sleep
Health consequences:
HTN, obesity risk, diabetes risk, decreased cognition, mood changes, decreased pain tolerance, increased risk for falls/other injuries
Personal consequences:
Reduced information retrieval, information reception - focus, attention, vigilance, memory encoding, interpretation of events, decision-making, planning; fatigue, exhaustion, decreased performance, negative impacts on mood
Epworth Sleepiness Scale
Subjective measure of sleepiness. Scores range from 0-24. The higher the score, the higher the "daytime sleepiness". A score higher than 11 may indicate sleep disorder or medical condition, and client should see MD.
Insomnia
Most common sleep disorder; defined as difficulty falling asleep and/or difficulty staying asleep and/or waking up too early AND next day consequences.
Causes: Stress, anxiety, depression; changes in work schedule; medical conditions; poor sleep habits
Comorbidities: Cardiovascular disease, pulmonary disease, GI, endocrine, cancer, renal, neurologic (AlzD, PD), pain from any source, urologic, SCI
Notable sleep disorders
Hypersomnia (long sleeper, narcolepsy)
Obstructive sleep apnea (central sleep apnea)
Circadian rhythm sleep-wake disorders
Parasomnias (sleepwalking, sleep eating, sleep terrors, REM sleep behavior disorders, nightmares, confusional arousal)
Sleep movement disorders (restless leg syndrome, leg cramps, bruxism, periodic limb movements)
OTs role in sleep and rest
Use knowledge of sleep physiology, sleep disorders, and evidence-based sleep promotion to address ramifications of sleep insufficiency or sleep disorders on occupational performance and participation. Interventions include:
- Educating clients about sleep misconceptions
- Addressing secondary conditions (i.e., pain, decreased ROM, depression, anxiety)
- Health management (smoking, caffeine, diet, exercise)
- Predictable routines
- Address sensory disorders
- Managing pain and fatigue
- Barriers to ADL, esp. Bed mobility and toileting
- Sleep hygiene routines
- Coping skills, manage stress
- Cognitive restructure
- Modify environment
- Advocate for laws, work/schedules to protect workers
Influences on sleep
Sleep schedule, bed, partners, pets, exercise activity, psychological state, sleep medicine, age, gender, genetics, cultural norms, social context, light/circadian drive, sleep environment
HOPE model
Developed as a teaching tool to help medical students, residents, and practicing physicians begin to process of incorporating a spiritual assessment into medical interviews. Allow for open-ended exploration of an individual’s general spiritual resources and concerns and serves as a natural follow-up to discussion of other support systems.
H: Sources of hope, meaning, comfort, strength, peace, love and connection - what gives you strength or helps you get through this?
O: Organized religion - Do you have a community to talk to?
P: Personal spirituality and practices - What do you like to do to give you strength?
E: Effects on medical care and end-of-life issues - Does it ever seem too much?
Spiritual distress
People are able to deal with great physical and emotional trauma, but they might be unable to bear a sense of meaningless...when they believe they are no longer needed, that they can no longer contribute, or that their life has no meaning
OT and spirituality interventions
Build rapport through discussions about spirituality. No action - there may be no "answer". Offer presence, understanding, acceptance, compassion. Prevention - identify and mobilize spiritual resources. Functional activities include preparing special foods, ritual actions or dance, prayer, walking or navigating aisles, etc.
Effects of SCI on sexuality
General: Decreased sexual satisfaction, frequency of sexual activities and interest in sexual activities.
Physiological: What impacts sexuality - level of injury (motor and sensory), complete or incomplete, comorbidities or pain, spasticity, bowel and bladder function
Psychological: What impacts sexuality - Pre-injury considerations, beliefs about sexuality, level of sexual desire, relationships pre- and post-injury, and self-concept
OT and sexuality interventions
Increase awareness of their own and partner's body sensations; learn to enjoy their own and other's body; develop greater satisfaction in physical experience together; enhance intimacy - emotionally and physically; increase ability to talk openly about sexual thoughts and feelings; develop trust so they can talk openly about other options for sexual behaviors
PLISSIT model
P: Obtaining permission from the client to initiate sexual discussion
LI: Providing the limited information needed to function sexually
SS: Giving specific suggestions for the individual to proceed with sexual relations
IT: PRoviding intensive therapy surrounding the issues of sexuality for that client
May add EX- prefix: Ensure permission
The Recognition Model
Recognition of the service user as a sexual being (affirming, normalizing, validating). Sensitive, permission giving strategies. Exploration of sexual problem/concern (any team member with skills or specialist). Address issues that fit within team's expertise and boundaries. Referral when necessary, including advocacy when resources are unavailable.
Pressure sore
Also called pressure ulcer, decubitus ulcer, decubiti bedsore, or skin breakdown. An area of the skin or underlying tissue (muscle, bone) that is damaged due to loss of blood flow to the area.
Causes of pressure sores
- Too much pressure on the skin for too long due to sitting or lying too long in one position or no padding
- Shearing
- Trauma - including abrasion, friction, bump, or falls
Risk factors for pressure sores
- Loss of muscle mass
- Being over- or underweight
- Decreased circulation (due to blood flow to the paralyzed limbs decreasing, edema or swelling, smoking, and diabetes, high blood pressure, and high cholesterol)
- Illness or poor overall health
- Moisture
- Dry, flaky skin
- Aging
- Previous skin breakdown
- Spasticity
- Extreme heat or cold
- Alcohol (or drug) use
- Depression
Pressure relief
Weight shifts by moving or lifting self to prevent pressure sores. Pressure reliefs should be done every 15-30 minutes for at least 30-90 seconds. If unable to perform independently, instruct caregiver to do it consistently.
Skin inspection
Check skin a minimum of twice a day (morning and bedtime). Look for changes in skin color (redness or darkening), blisters, bruises, cracked, scraped, or dry skin. Feel for hardness, swelling or warmth that may signal skin breakdown. Areas with highest risk for pressure sores are the bones closest to the surface of the skin - bony prominences (sacrum, coccyx, heel of foot, ischium, trochanter, elbow, knee, ankle, toes and bony areas of the food, back of the head).
Padding, positioning, and turning in bed for SCI skin care
Use regular schedule of turning at night. Depending on weight and skin tolerance, your turning schedule may vary from every 2 to every 6 hours. When turning, lift rather than slide across sheets. Use pillows and foam pads to protect bony areas. Avoid elevating the head of your bed, which adds pressure to buttocks and lower back areas.
Keep skin clean and dry for SCI skin care
Bathe daily w/ mild soap and warm water. Immediately wash and dry skin and change clothes after leakage of stool or urine.
Pressure mapping
Therapist creates a pressure map during a seating evaluation. Puts map above cushion and under your buttocks to see where your pressure-sensitive areas are.
Clothing, hydration, nutrition, sun exposure, temperature, and circulation for SCI skin care
Wear loose fitted clothing. Drink enough water everyday and avoid caffeinated drinks. Eat a balanced diet. Avoid getting sunburned. Avoid frostbite and burns - more susceptible. Quit smoking and keep as active as possible.
Tilting or reclining for SCI skin care
Power tilt wheelchair used for regular pressure relief. Tilt system will tilt the wheelchair between 25-65 degrees to relieve pressure. Recline system will affect vertical pressure and horizontal pressure. Elevate leg rests to reduce pressure in lower extremities during recline.
Pressure relief - Leaning from side to side
Lock wheels and move one armrest away to side. Hold onto remaining armrest and lean body to opposite side for 30-90 seconds. Regain upright position and repeat on other side.
Pressure relief - Leaning forward
Lock wheels. Bend forward and bring chest to knees for 30-90 seconds. Return to upright position.
Pressure relief - Independent push-ups
For clients who can extend their elbows and lift their body weight (people w/ injury at C7 and below). Grip arm rest and lift up completely off the seat for 60 seconds.
First signs of pressure sore
Reddened, discolored, or darkened area of the skin. For an African American's skin, it may look purple, blueish, or shiny. May feel hard and warm to touch.
Initial pressure sore - what to do
Remove pressure from the reddened area for 10-30 minutes. If skin color doesn't return to normal, stay off the area.
Blanching test
Used to test skin for pressure sore. Press on the red, pink or darkened area with your finger. Area should go white. Remove the pressure and the area should return to red, pink, or darkened color within a few seconds, indicating good blood flow. If it remains white, blood flow has been impaired and damage has begun.
Stage 1 pressure sore
Signs: Skin is not broken but is red or discolored; may show changes in hardness or temperature. When you press on it, it stays red and doesn’t lighten or turn white (blanch). The redness or change in color doesn’t fade w/in 30 minutes after pressure is removed
Healing time: Reversed in about 3 days if all pressure is taken off the site
Stage 2 pressure sore
Signs: The topmost layer of skin (epidermis) is broken, creating a shallow open sore. The second layer of skin (dermis) may also be broken. Drainage (pus) or fluid leakage may or may not be present
Healing time: Three days to three weeks
Stage 3 pressure sore
Signs: Wound extends through the dermis (second layer of skin) into the fatty subcutaneous (below the skin) tissue. Bone, tendon, and muscle are not visible. Look for signs of infection (redness around edge of sore, pus, odor, fever, or greenish drainage from the sore) and possible necrosis (black, dead tissue)
Healing time: One to four months
Stage 4 pressure sore
Signs: The wound extends into the muscle and can extend as far down as the bone. Usually lots of dead tissue and drainage are present. There is a high possibility of infection
Healing time: Anywhere from three months to two years
Suspected deep tissue injury
Purple or maroon localized area of discolored intact skin or blood-filled blister due to the damage of underlying soft tissue from pressure and/or shear. Area may be surrounded by tissue that is painful, firm, mushy, bloody, warmer, or cooler as compared to nearby tissue. For darker skin tones, may include a thin blister over a dark wound bed. Wound may further evolve and become covered by thin eschar (scab)
Unstageable pressure sore
Full thickness tissue loss in which the base of the ulcer is covered by slough (dead tissue separated from living tissue) of yellow, tan, gray, green, or brown color, and/or eschar (scab) of tan, brown, or black color in the wound bed.
Possible complications of pressure sores
Can be life threatening. Infection can spread to blood, heart, and bone. Amputations. Prolonged bed rest can keep you out of work, school, and social activities for months. Autonomic dysreflexia. Higher risk for respiratory problems or UTIs. Costly treatment.
Major Depressive Disorder (MDD)
Psychological disorder involving a significant depressive episode and depressed characteristics, such as lethargy and hopelessness, for at least two weeks.
Diagnostic criteria:
- Depressed mood most of the day, nearly every day (e.g., feels sad, empty, hopeless) or observation made by others (e.g., appears fearful)
- Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day
- Significant weight loss when not dieting or weight gain
- Insomnia or hypersomnia nearly every day
- Psychomotor agitation or retardation nearly every day (observable by others, not merely subjective feelings of restlessness or being slowed down)
- Fatigue or loss of energy nearly every day
- Feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day
- Diminished ability to think or concentrate, or indecisiveness, nearly everyday (either by subjective account or as observed by others)
- Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation w/o a specific plan, or a suicide attempt or a specific plan for committing suicide
Impact of MDD on functioning
- ADLs - Reduced participation in self-care activities
- IADLs - Reduced motivation, interest, or pleasure in IADLs (i.e., home management, pet care, meal prepping/eating, religious/spiritual expression)
- Health management - Decreased engagement in exercise, medication management, communication w/ doctors/therapists
- Rest and sleep - Habits and routines don't facilitate sleep, problems falling asleep or staying asleep
- Education/work - Increased absences, incomplete tasks/assignments, reduced attention, motivation, and pleasure
- Play and leisure - Withdrawal from meaningful and pleasurable activities, decreased flexible thoughts, unable to tolerate frustrations or losses
- Social participation - Increased isolation, avoidance of interacting with others
Bipolar I Disorder
Requires symptoms to meet the full criteria for what is known as a manic episode. The patient does not have to experience depression to be diagnosed with Bipolar I, but many people with the diagnosis experience both kinds of mood episodes.
- May or may not have hypomania or MDD, psychotic features, or rapid cycling, be seasonal, or have remission
May include:
Hypomania - Min. 4 days; persistent, elevated activity, three or more of the symptoms described before; social/work function okay
MDD - 5 symptoms: Anhedonia/depressed mood, weight loss/loss of appetite, insomnia/hypersomnia, fatigue or low energy, feelings of worthlessness/guilt, problems concentrating, suicidal ideation or attempt
Manic episode
Diagnostic criteria includes:
- Abnormal, persistent elevated, expansive or irritable mood
- Abnormal, persistent increased goal-directed activity or energy
- One week duration (min.)
- At least three symptoms:
-> Inflated self-esteem, euphoria/grandiosity
-> Decreased sleep
-> Excessive talkativeness/pressure to speak
-> Distractibility
-> Increased goal directed activity or psychomotor agitation, impulsive
-> May have psychotic symptoms
Psychotic symptoms
Hallucinations - things that aren’t real to others (voices, things, sensations)
Delusions - unshakeable belief in something that isn’t real, true, or likely to happen
Paranoid delusions - money is being taken from them, someone is coming to get them
Incoherent or irrational thoughts and speech - speech rapid and hard to follow, lose track of train of thought
Lack of awareness - don’t realize their behavior isn’t within normal bounds and that people don’t see the things they see
Triggers to bipolar manic episode
- Changes to sleep pattern or lack of sleep. Increased change postpartum
- Emotionally charged situations with significant people in their lives
- Change in relationship status, divorced, widowed, child leaves home, or other
- Drug or alcohol abuse or single episode of high intoxication
- Medications
- Change in season - seasonal depression
- Job loss
- Death of a loved one
Impact of bipolar I disorder on functioning
ADLs - Difficulty sequencing and sustaining attention to self-care activities
IADLs - Decreased focus and attention on IADL activities (i.e., meal preparation); decreased ability to engage in IADL activities (i.e., care of pets home environment); symptoms impact ability to engage in IADL occupations (impulsivity, thought disorganization, illogical decisions); Increased pleasure from neutral stimulus and exaggerated pleasure from a preferred stimulus; Increase social participation w/ potential for high-risk situations; increased engagement in goal-directed behavior
Bipolar II disorder
A disorder characterized by alternating periods of extremely depressed and mildly elevated moods
One hypomanic episode and one major depressive episode (lasting 2+ weeks). Individual has never had a manic episode.
Co-morbid conditions - substance use disorder, anxiety, lifetime suicide risk
Bipolar disorder - etiology, prognosis, and prevalence
Prevalence: No gender differences; avg. age of diagnosis is 25 years old
Etiology: Biological/genetic
Prognosis: Most often chronic. 50% w/ 1 manic episode have a second. Early onset leads to more difficult course. Often recurring episodes. Interaction w/ judicial system - 13% w/ mania.
Treatment for bipolar disorder
- Medication - Lithium or SSRIs (both have risk factors, such as drowsiness, decreased awareness, weight changes, possible kidney or thyroid disorders, etc. that can impact functioning)
- Electroconvulsive therapy - reserved for severe cases
- Therapy - Group therapy, family therapy, CBT, etc. In combination w/ medication
Cyclothymic disorder
Hypomania and depressed mood (not MD episode) alternate. Less severe, has symptoms most of the time.
Considerations - Greater risk for developing Bipolar I and II; mood swings may affect family, social, and work relationships; substance use may increase if person self-medicates
Role of OT in intervention - Coping w/ chronic illness, time management, help w/ self-esteem
OT role in mental health (general)
Initial evaluation - occupational profile, assessments focused on occupational needs
Intervention - Assists with groups (skills, leisure, socialization); Provides 1:1 as needed; Creates a safety plan and day use plan prior to discharge
Role of OT in MH intervention for bipolar disorder
Acute care - provide structured environment, improve focus, setting limits to contain impulses (mania)
Chronic care - Learn signs of impending shifts in mood, managing medication, evaluate/treat cognitive dysfunction
Role of OT in MH intervention for depression
- Management of ADL and IADL (self-care, work, leisure, sleep, sexual occupations)
- Re-establish habits, roles, and routines (parenting, etc.)
- Compensate for cognitive slowing
- Social and communication skills
- Activities to improve self-esteem and increase motivation (including spiritual practices)
- Creative activities to express emotions
- Structuring work tasks
Bipolar related terms
Affect - Display of emotions
Anhedonia - Lack of interest in previously pleasurable activities
Avolition - Lack of drive or ambition to complete tasks
Dysphoria - Depressed or negative mood
Euphoria - Highly elevated, exaggerated mood
Flight of ideas - Rapidly changing, disconnected thoughts
Grandiosity - Inflated sense of self-esteem or importance
Psychomotor agitation - Increased purposelessness movements, agitated (writing hands, fidgeting, pacing)
Psychomotor retardation - Abnormally slowed or reduced movements or speech
Group vs. individual intervention for MH
Group - Primary means of intervening w/ patients. Areas of occupations addressed include ADLs, rest and sleep, play, leisure, and social participation. Performance skills targeted include emotional regulation, cognitive skills, communication, and social skills. Performance patterns addressed include habits, routines, roles, and rituals
1:1 - Evaluation focused on individual needs (COPM, OSA, MOCA). Focus on supporting occupational participation, safety awareness, communication
Partial Hospitalization Program (PHP)
Medicare defines PHP as a minimum of 4 days/20 hours of group/week.
Patients enter PHP through community referral or direct referral from the hospital. More stable than inpatient patients, but are still at high risk for self-harm. Attend daily groups and make plans for their evenings/weekends.
Intensive Outpatient (IOP)
Medicare defines IOP as a minimum of 11 hours of group/week.
Patients drop down to IOP as they stabilize and can manage w/ less supervision and support. Continue to work w/ individual providers and utilize other support groups.
5150
A person w/ a mental illness can be involuntarily detained for a 72-hour psychiatric hospitalization if they are a danger to others (imminent threat exists), danger to self (life threatening danger to self), or is gravely disabled (unable to care for basic needs of self).
Limb loss
80% lower limb loss; 10% upper limb loss; 10% multiple limb loss
Typical causes: Congenital, illness, and injury
Acquired limb loss causes: 54% is vascular disease/PVD; 45% is from trauma; 2% is from cancer.