Kaap 309: Skeletal system II (Bone formation + clinical correlations)
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
25 Terms
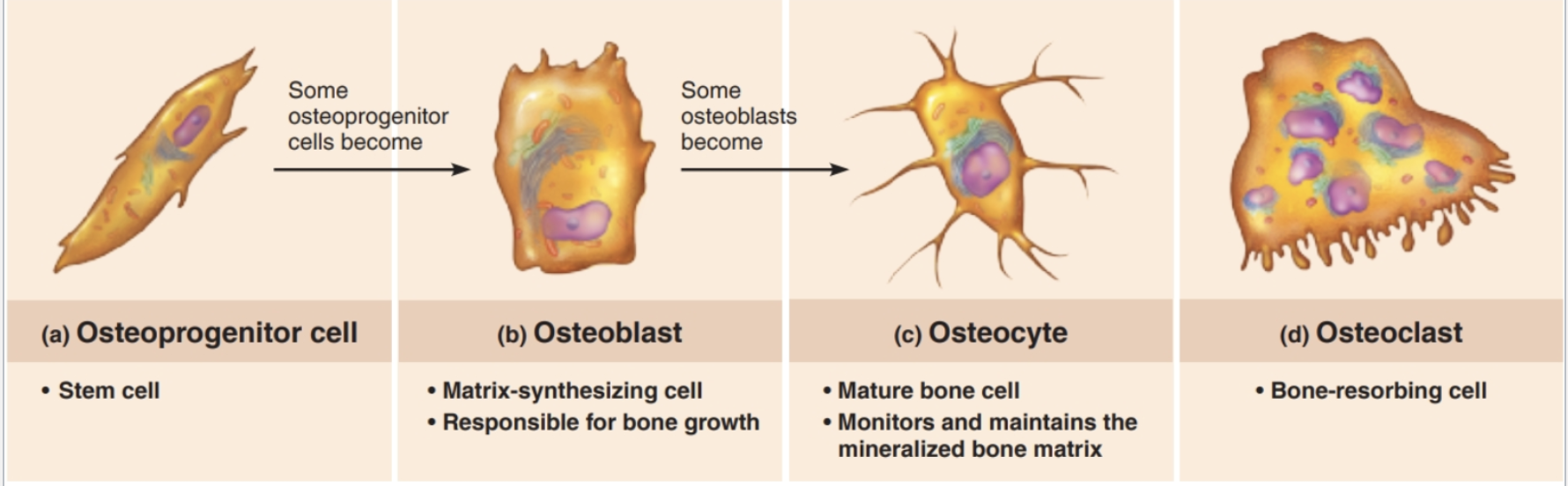
Cells of bone tissue
Cell Type | Description | Main Function |
|---|---|---|
Osteogenic cells | Stem cells found in the periosteum and endosteum | Divide to form new osteoblasts (the “bone builders”) |
Osteoblasts | Matrix-synthesizing cells | Build bone by secreting osteoid → responsible for bone growth |
Osteocytes | Mature bone cells trapped in lacunae | Maintain bone matrix and communicate with other cells to direct remodeling |
Osteoclasts | Bone-resorbing cells (large, multinucleated) | Break down (resorb) bone matrix during growth, repair, and remodeling |
Formation of the Skeleton
All bones begin as fibrous connective tissue or hyaline cartilage models.
Ossification begins around week 8 in utero.
Two types of bone formation:
Intramembranous ossification → forms flat bones (skull, clavicle)
Endochondral ossification → forms most bones (long bones)
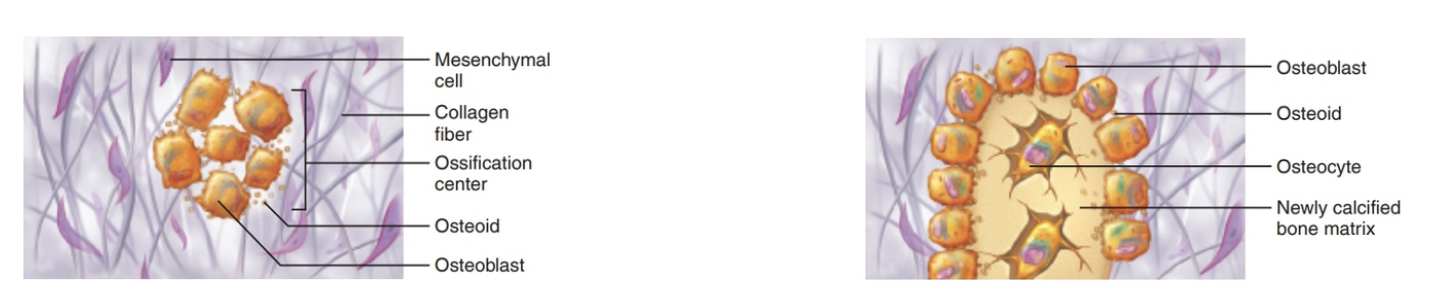
Intramembranous Ossification
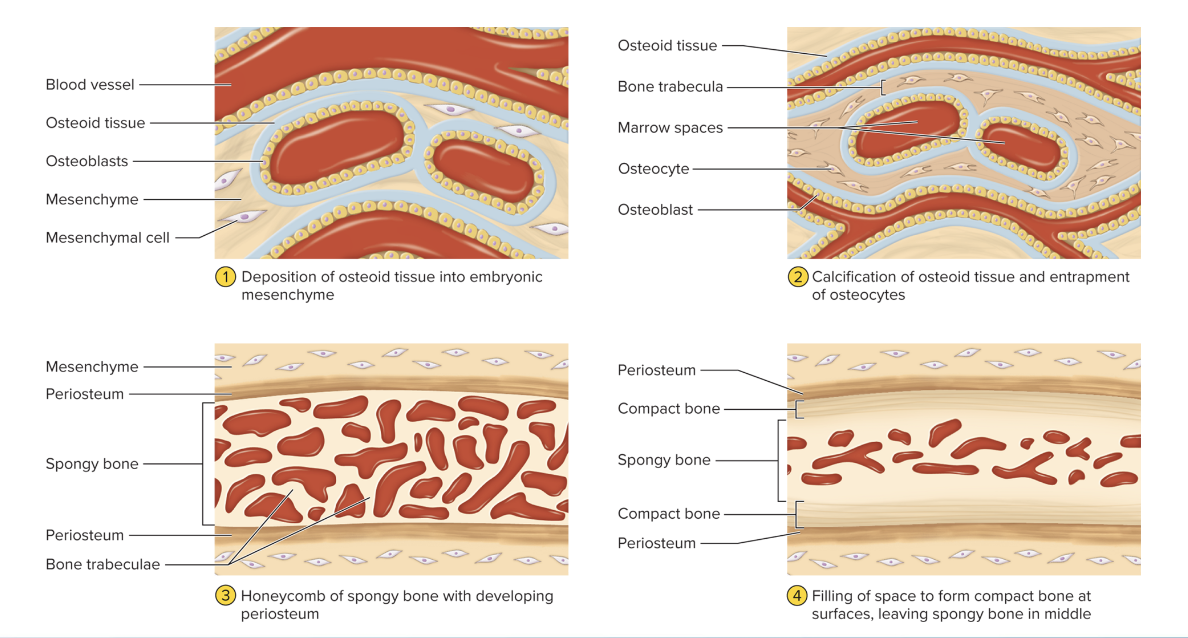
Intramembranous Ossification
Mesenchymal cells cluster
around a vessel and become
osteoblasts
Osteoblasts secrete osteoid
and an ossification center
forms in fibrous connective
tissue.
1. Osteoblasts grow and continue
to secrete osteoid
2. Trapped osteoblasts now
become osteocytes
Intramembranous Ossification
1. Osteoid continues to form
around vessels, forming an
immature spongy bone
2. Mesenchyme adheres to the
external surface and becomes
the periosteum
1. Immature spongy bone
near the periosteum is
remodeled and replaced
with compact bone
2. Central immature spongy
bone matures

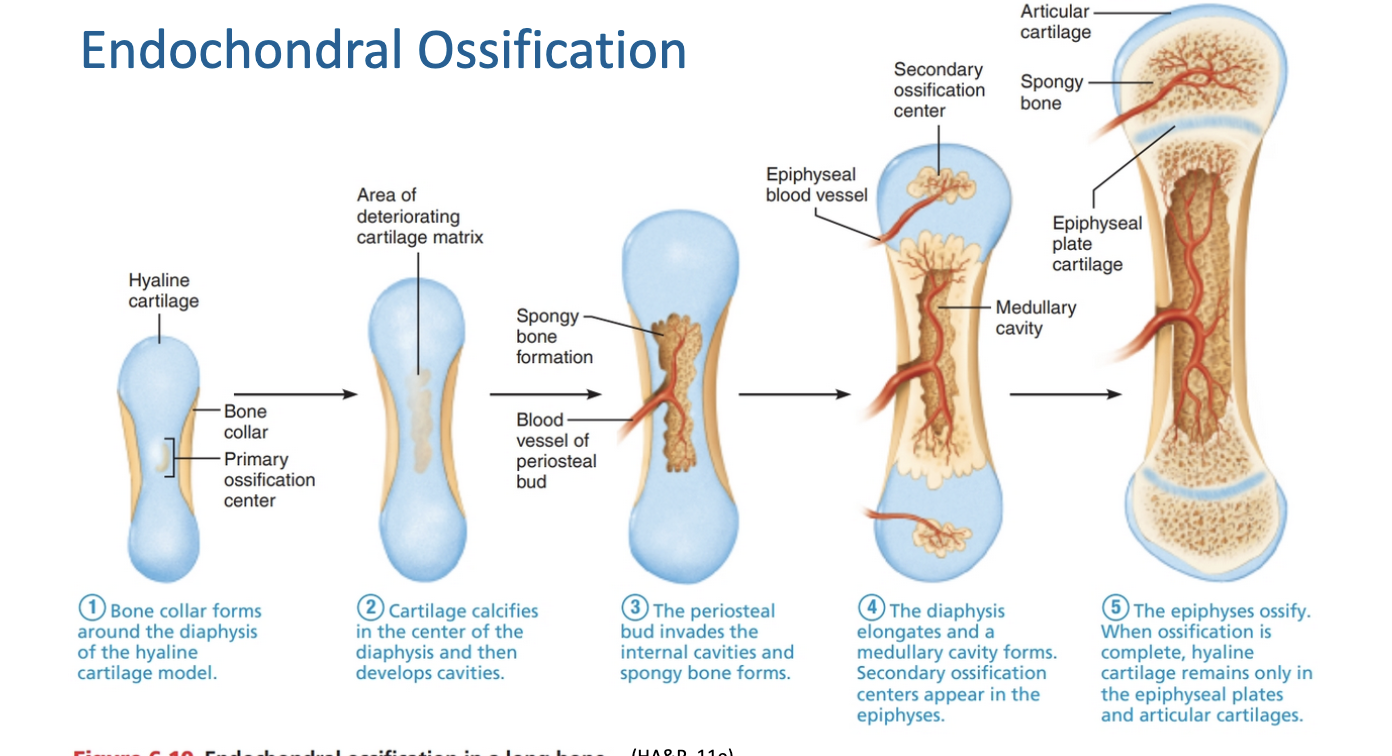
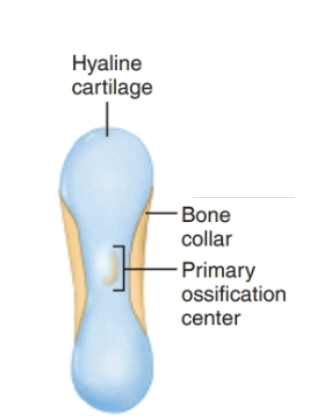
Endochondral Ossification (I)
Mesenchymal cells specialize into osteoblasts
Perichondrium becomes periosteum
Osteoblasts secrete osteoid, creating a bone collar
Chondrocytes left within hypertrophy and become the primary ossification center
Cartilage model
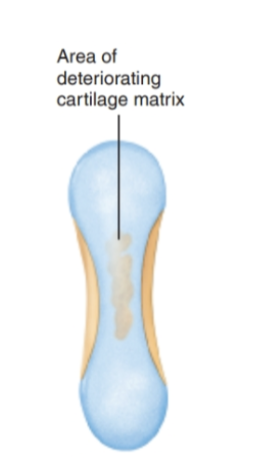
Endochondral Ossification (II)
Chondrocytes from the primary ossification center ossify surrounding cartilage
Chondrocytes die and the matrix begins to dissolve
Cavities are now formed within the model
Remaining cartilage (ends) stay healthy and grow rapidly to elongate the model
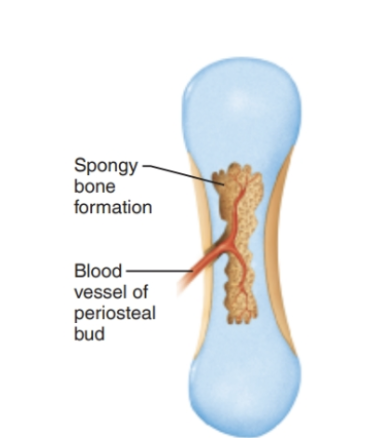
Endochondral Ossification (III)
Cavities are invaded by the periosteal bud
Nutrient a/v/n, red marrow elements, osteoprogenitor cells, osteoclasts
Osteoclasts partially erode the cartilage matrix
Osteoprogenitor cells become osteoblasts → (spongy bone formation!)
Endochondral Ossification (IV)
1. Osteoclasts break down the newly formed spongy bone and open the cavity
2. The epiphyses stay as cartilage ends through birth (growing rapidly)
3. After birth, secondary ossification centers develop at epiphyses
– Short bones only have primary
– Irregular bones have multiple ossification centers
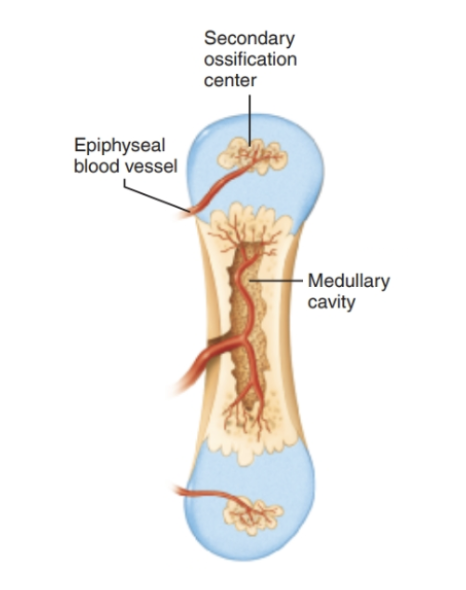
Endochondral Ossification (V)
Secondary ossification mimics that of primary except the spongy bone remains and no cavity is formed
The space between the diaphysis and epiphysis is the epiphyseal plate and is hyaline cartilage
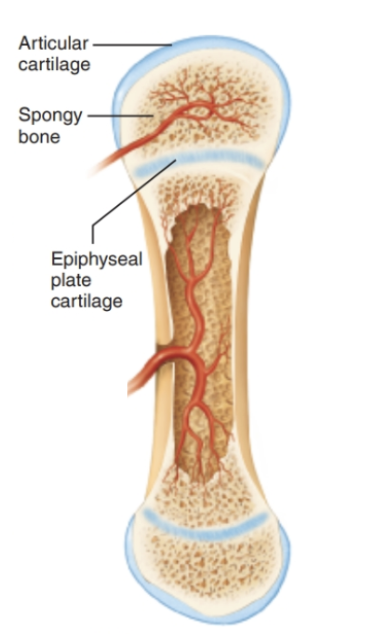
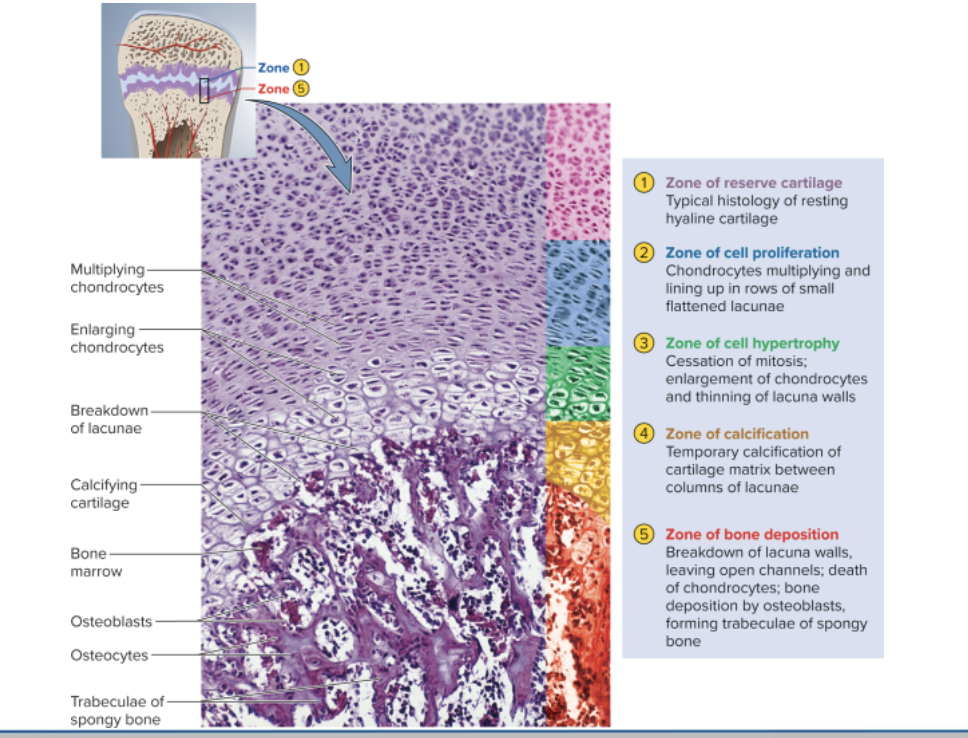
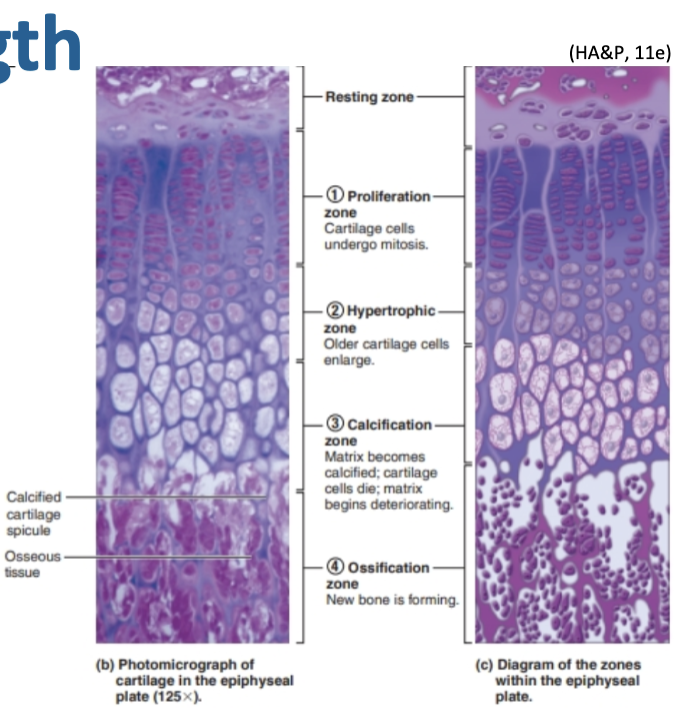
Postnatal growth - length
At the epiphyseal plate:
Proliferation zone: chondrocytes divide
Hypertrophic zone: older chondrocytes enlarge
Calcification zone: matrix calcifies; chondrocytes die
Ossification zone: new bone forms
Postnatal growth - width
Completed through appositional growth
Osteoblasts in the periosteum secrete bone matrix to the external bone surface
Osteoclasts on the endosteal surface remove bone
Remodeling bone
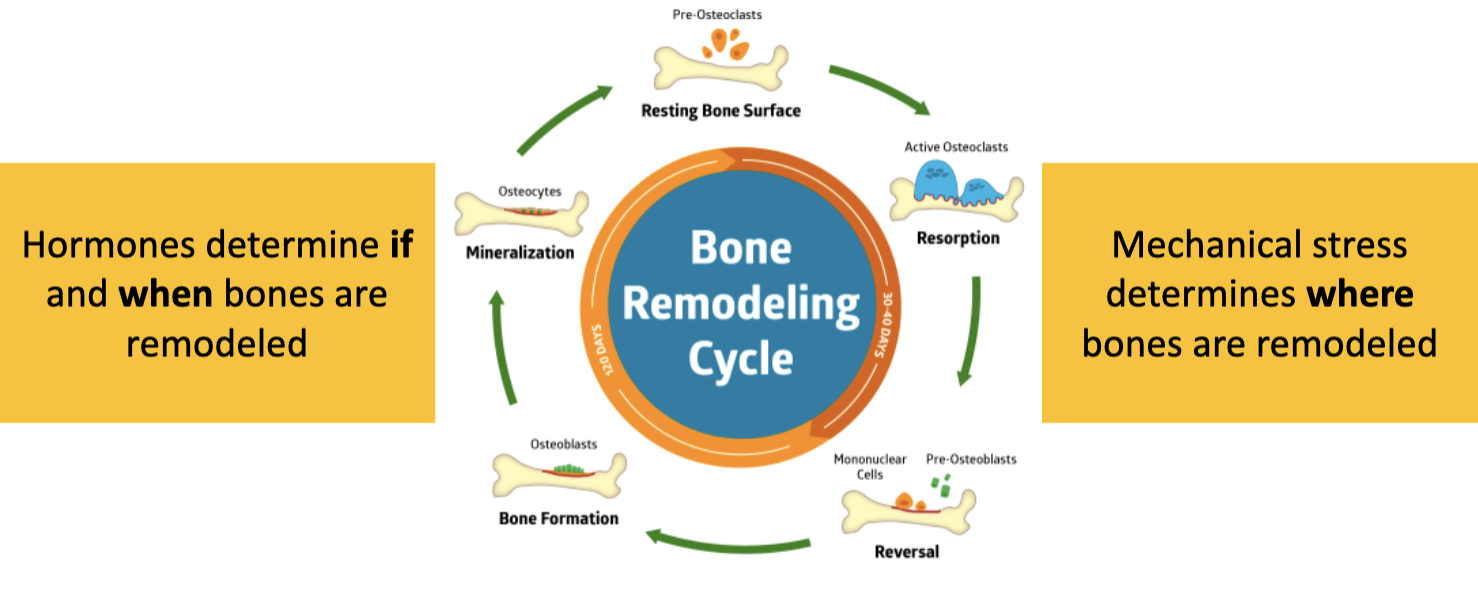
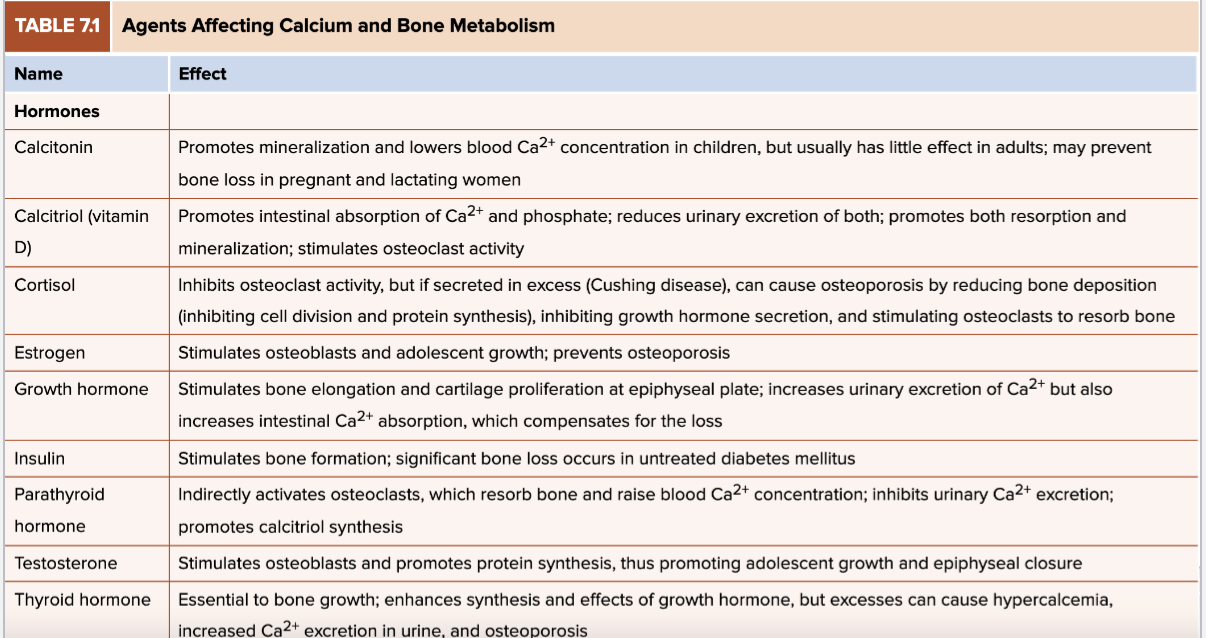
Hormonal influence
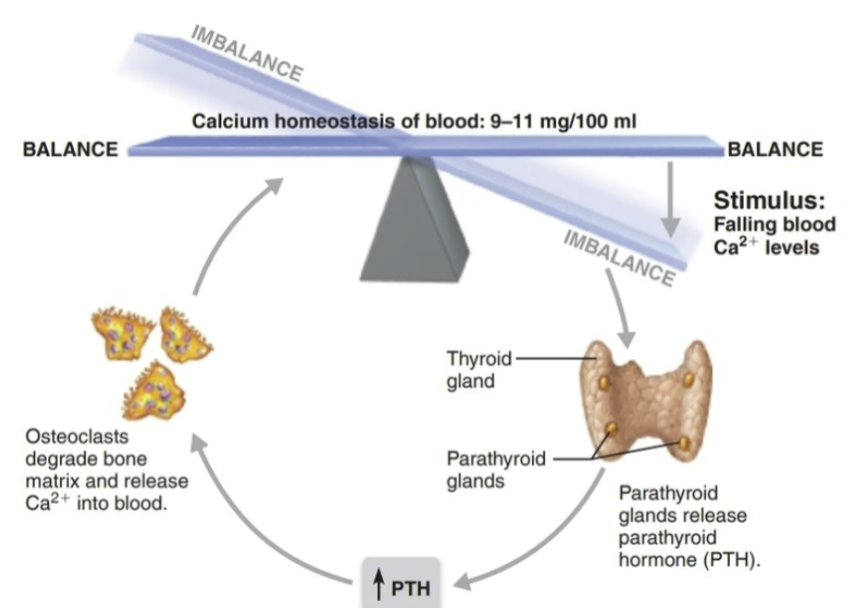
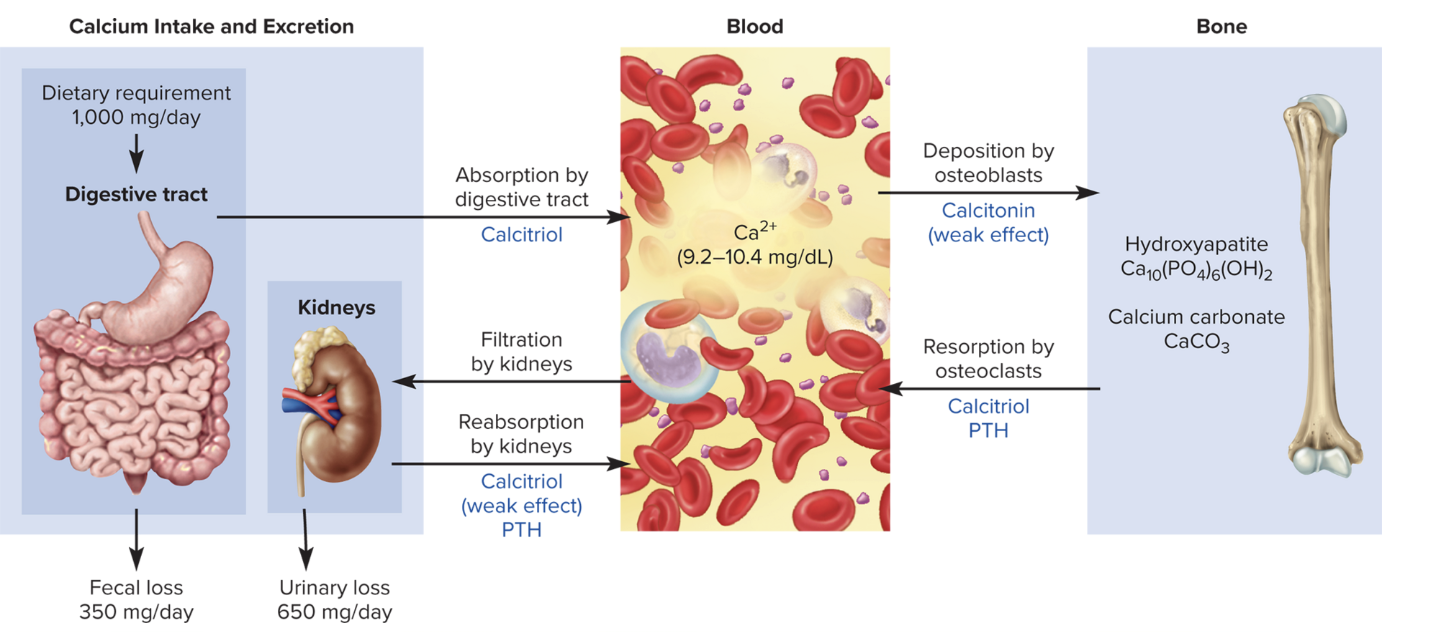
Role of calcium in the body
Homeostasis for maintaining resting membrane potentials
99% of the body’s calcium is stored in bone matrix
Hormones maintain a level of 9–11 mg/dL in the blood
Key hormones: Parathyroid hormone, Calcitriol, Calcitonin
Hormonal influence
hypercalcemia
hypocalcemia
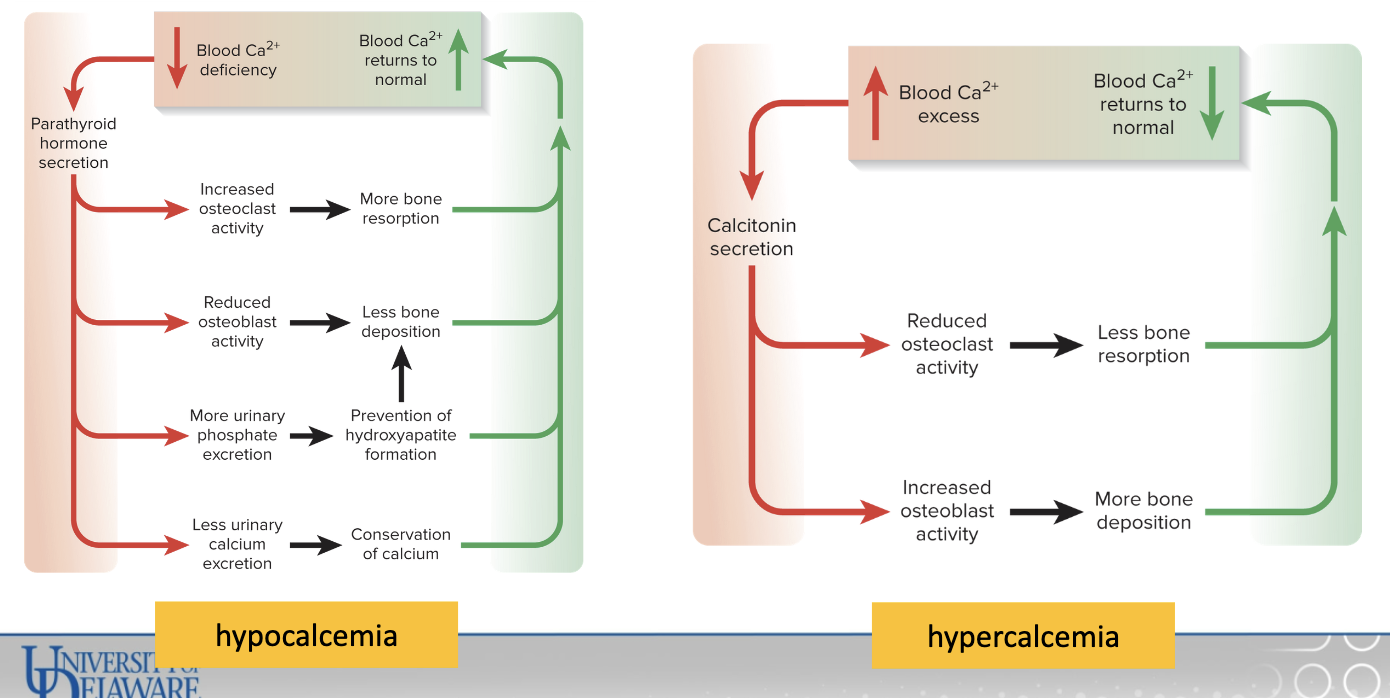
Parathyroid Hormone
secreted by the parathyroid glands
Stimulate the osteoclasts to promote bone resorption
Promotes calcium reabsorption by the kidneys
Promotes final step of calcitriol synthesis in the kidneys
Inhibits collagen synthesis by osteoblasts
Calcitriol & Calcitonin
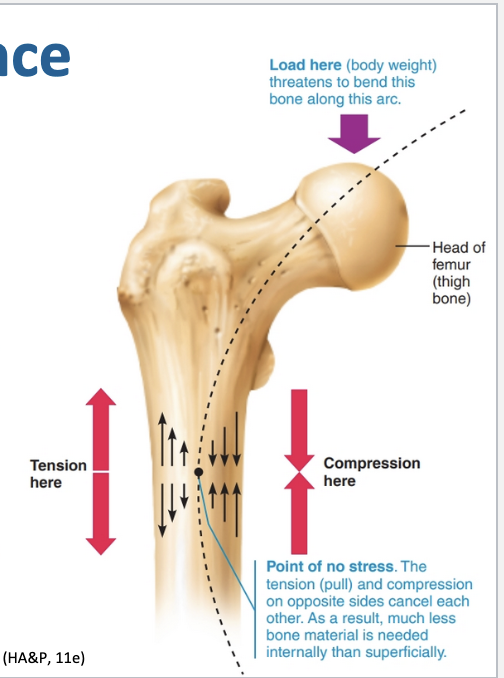
Mechanical stress influence
Wolff’s Law: the body adapts to the forces placed upon it
Fractures
Type | Description |
|---|
Non-displaced | Ends in normal position (Broken but still in place) |
Displaced | Ends out of alignment (Broken and shifted out of place) |
Incomplete | Not fully broken through |
Complete | Fully broken |
Closed (simple) | Skin intact (Break on the inside) |
Open (compound) | Skin penetrated (Break open to the outside) |
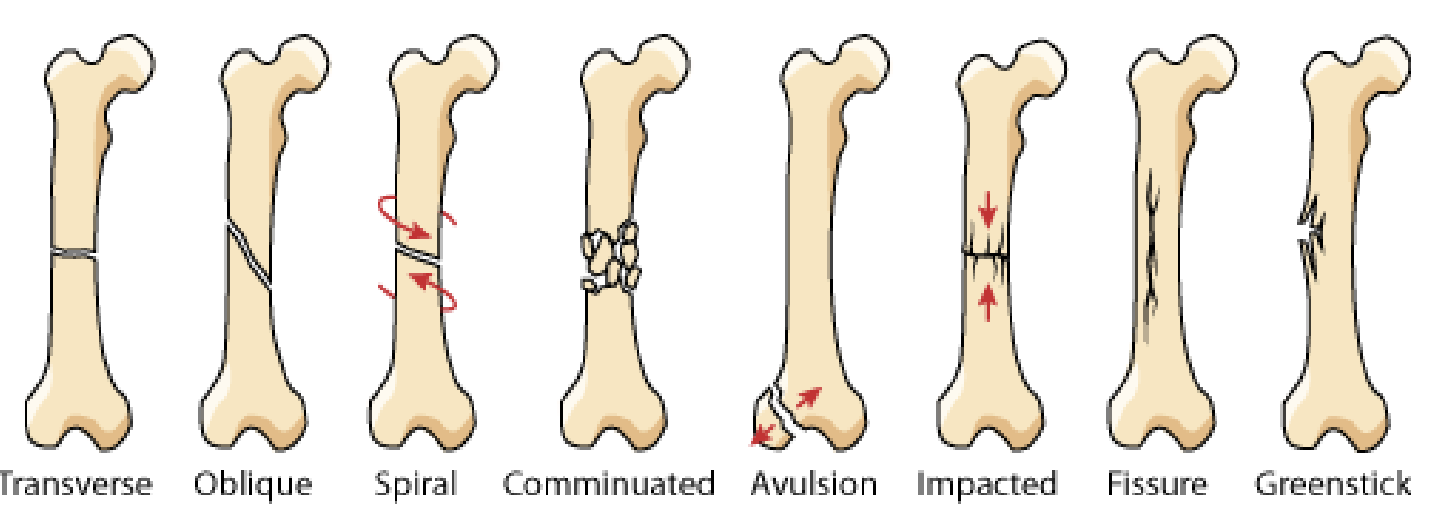
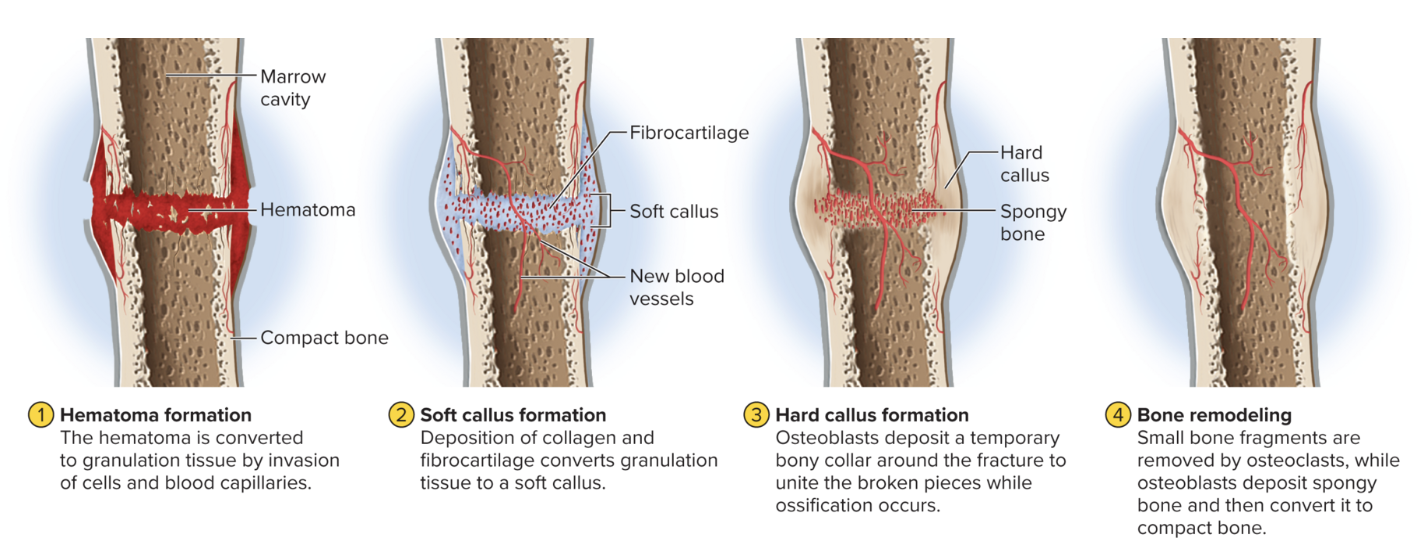
Four stages for traumatic (acute) fracture healing
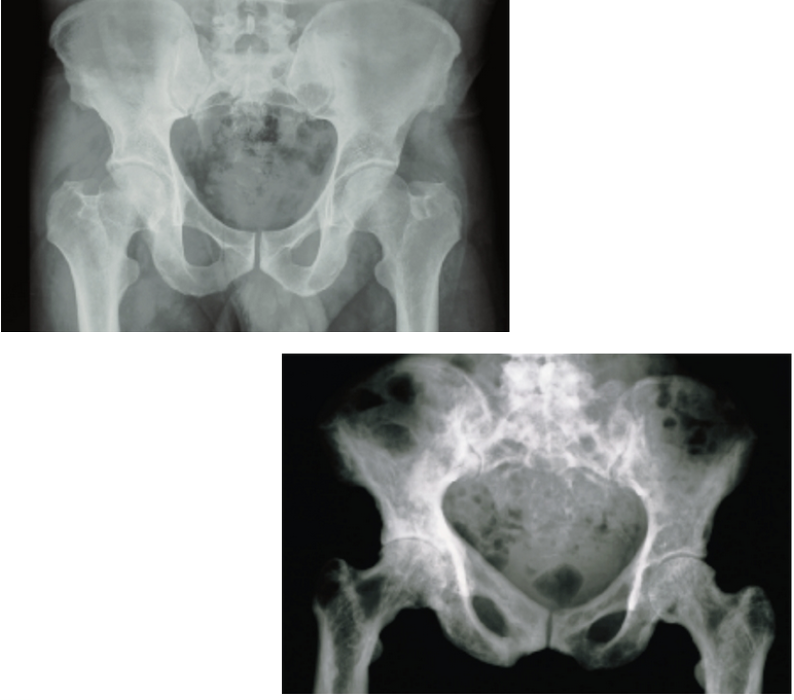
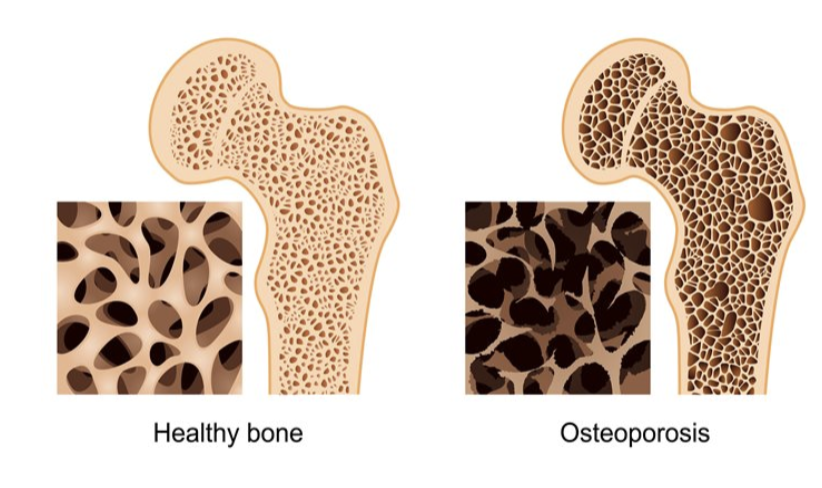
Osteoporosis
Group of diseases in which bone resorption outpaces bone deposit
1 in 3 women over 50 will have a fracture due to osteoporosis
Risk Factors:
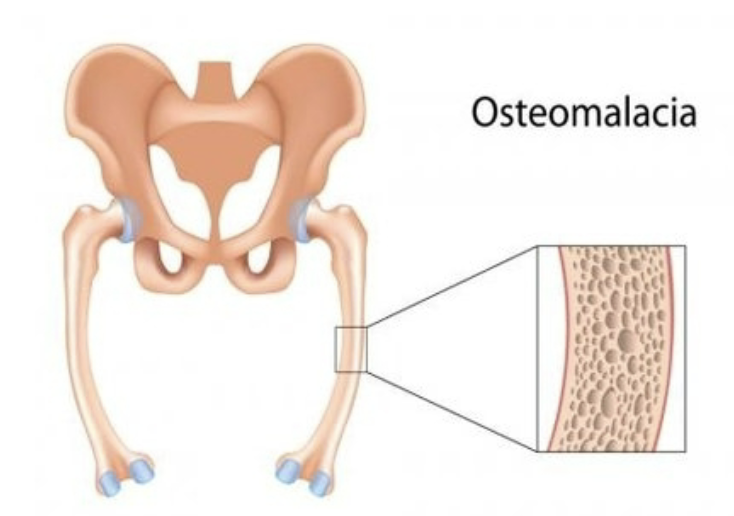
Osteomalacia
Group of diseases in which bones are poorly mineralized
Results in weak and soft bones
Calcium salts not sufficient
Childhood version: Rickets
Bowed legs
Deformities to the skull, pelvis, and ribs
Osteitis Deformans
Haphazard bone deposit and resorption
Abnormally high ratio of spongy bone
Commonly affects the: spine, pelvis, femur, skull
3% of elderly North Americans – rare before 40