Bones and Skeletal Tissue
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
Cartilage
Features between dense CT & bone → tough but flexible
avascular, devoid of nerve fibers
all types are made up of cells encased in small cavities (lacunae) within jelly-like extracellular matrix
ground subsatnce contains lots of the glycosaminioglycans (GAGs): chondroitin sulfate & hyaluronic acid - also chondronectin (adhesive protein)
Collagen fibers (can have some elastic fibers)
up to 80% H2O
Perichondrium
Layer of dense connective tissue surrounding cartilage like a girdle
Helps cartilage resist outward expansion
Contains blood vessels for nutrient delivery to cartilage
In damaged areas, perichondrium can form scar tissue because poorly vascularized cartilage repairs badly
Chondroblasts
immature cartilage cells - actively form cartilage
Chondrocytes
mature cartilage cells - maintain cartilage
Lacunae
Localized clusters of chondrocytes in cartilage
Hyaline Cartilage
Most abundant
Firm support + pliability
lots of collagen
appears glassy blue-white
chondrocytes - only 1-10% of volume
Elastic Cartilage
Like hyaline cartilage, but more elastic fibers
external ear, epiglottis
Fibrocartilage
rows of chondrocytes alternating with rows of thick collagen fibers; great tensile strength
Appositional Growth (Growth of Cartilage)
New matrix laid down on surface of cartilage
Cartilage - forming cells in perichondrium secrete matrix against external face of existing cartilage
Cartilage increases in width
Interstitial growth ( Growth of Cartilage)
new matrix made within cartilage
Chondrocytes within lacunae divide and secrete new matrix, expanding cartilage from within
cartilage increases in length
Cartilage growth ends during adolescence
Bone Tissue
Bone is a living dynamic tissue which respond to its environment:
Bone reacts to amount of force applied by increasing both the density & amount of roughening on bone or decreasing density when force is reduced or eliminated (eg. paralysis) (deposition vs. resorption)
Bone stores calcium - resorbed & transferred to bloodstream when needed
Functions of Bones
Support
Protection
Anchorage & Movement
Mineral storage
Blood cells formation
fat storage
Hormone production (osteocalcin)
Classification of Bones
206 named bones in the human skeleton
Two main groups, divided by location
Axial Skeleton:
Long axis of body
Skull, vertebral column, rib cage
Appendicular Skeleton
Bones of upper and lower limbs
Girdles attaching limbs to axial skeleton
Lots of variation in size/shapes of bones (e.g. pisiform bone vs. femur)
Unique shape of each bone fulfils a particular need
e.g. femur - maximum strength with minimum weight - achieves this with hollow cylindrical design
Classified by their SHAPE and not SIZE
Long Bones
much longer than wide
shaft + 2 expanded ends
mostly compact bone with marrow cavity; spongy bone near joint ends
Irregular Bones
leftovers
complicated shapes: primarily spongy bone + thin covering layer of compact bone
Ex. vertebrae & hip bones
Flat Bones
Thin, flattened & sometimes curved
include ribs, sternum & scapula & most cranial bones
Short Bones
roughly cube-shaped; e.g. wrist, ankle
primarily spongy bone + thin outer layer of compact bone
Sesamoid bones form within tendons - Ex. Patella
Bone Structure
Bones are organs
Bone (osseous) tissue dominates
Also contain nervous tissue, cartilage, dense connective tissue, muscle cells and epithelial cells in its blood vessels
three levels of structure: gross / microscopic / chemical
Compact bone
dense outer layer on every bone that appears smooth and soild
Spongy bone
made up of a honeycomb of small, needle-like or flat pieces of bone called trabeculae
open spaces between trabeculae are filled with red or yellow bone marrow
Structure of short, irregular and flat bones
All have similar structure
thin plates of spongy bone (dipole) covered by compact bone
Compact bone sandwiched between connective tissue membranes
Periosteum covers outside of compact bone and endosteum covers inside portion of compact bone + spongy bone
Bone marrow scattered throughout the spongy bone/ no defined marrow cavity
Hyaline cartilage covers articular surfaces
Diaphysis (Structure of a Typical Long Bone)
tubular shaft of a long bone = long axis of the bone
collar of compact bone surrounding marrow cavity (medullary cavity)
in adults, medullary cavity contains fat (yellow marrow) and is called the yellow bone marrow cavity
Epiphyses ( Structure of a Typical Long Bone)
extremities of a long bone; expanded for articulation with other bones
compact bone externally; interior filled with spongy bone
thin layer of hyaline (articular) cartilage on the outer surface
Epiphyseal Line (structure of a typical long bone)
between diaphysis & each epiphysis
remnant of epiphyseal (growth) plate
Periosteum (structure of a typical long bone)
Covers external surface, 2 layers
Outer fibrous layer
dense irregular connective tissue with Sharpey’s fibers that secure to bone matrix
Inner osteogenic layer
contains primitive osteogenic stem cells that gives rise to most all bone cells
Nutrient foramen
nerve fibers and blood vessels to the shaft
Endosteum
Delicate connective tissue covering trabeculae of spongy bone & lines canals of compact bone
Like periosteum, contains osteogenic cells that can differentiate into other bone cells
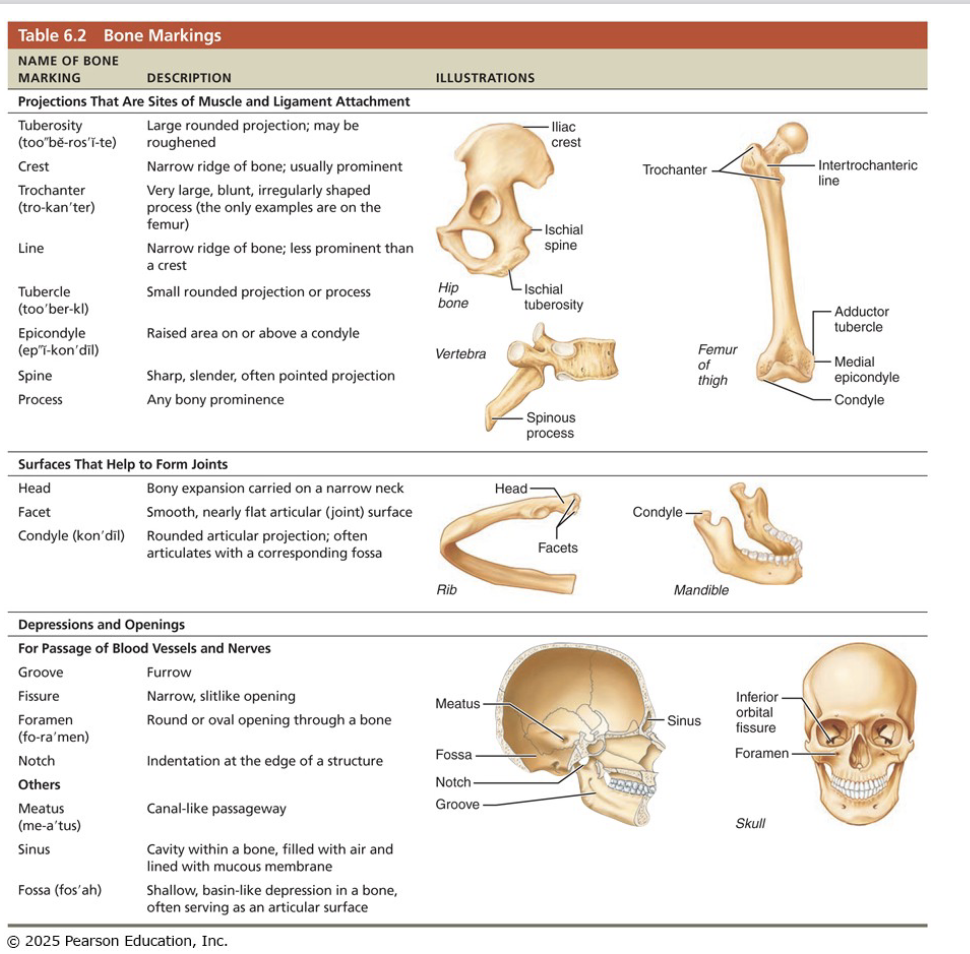
Bone Markings
Sites of muscle, ligament and tendon attachment on external surfaces
Areas involved in joint formation or conduits for blood vessels and nerves
Three types of markings:
Projection: outward bulge of bone
depressions and openings
surfaces
Microscopic Anatomy of Bone
Calcium salts give hardness & strength for support/protection of softer tissues; cavities for fat storage & synthesis of blood cells
Cells of bone tissue
five major cell types, each is a specialized form of the same basic cell types:
Osteoprogenitor (osteogenic) cells
Osteoblasts
Osteocytes
Bone-lining cells
Osteoclasts
Microscopic anatomy of compact bone
Also called lamellar bone
Consists of:
Osteon (haversian system)
Canals and canaliculi
Interstitial and circumferential lamellae
Osteon (Haversian System)
An osteon is the structural unit of compact bone
an elongated cylinder that runs parallel to long axis of bone / acts as tiny weight-bearing pillars
An osteon cylinder consists of several rings of bone matrix called lamellae
Canals and Canaliculi
central (Haversian) canal runs through core of osteon
Contains blood vessels and nerve fibers
Perforating (Volkmann’s) canals: canals lined with endosteum that occur at right angles to central canal
Connect blood vessels and nerve of periosteum, medullary cavity and central canal
Lacunae: small cavities that contain osteocytes
Canaliculi: hairlike canals that connect lacunae to each other and to central canal
Enables communication between all osteocytes of osteon and permit nutrients and wastes to be relayed from one cell to another
Interstitial Lamellae
Some fill gaps between forming osteons; other are remnants of osteons destroyed by bone remodeling
Circumferential Lamellae
Sheets of bone located just deep to periosteum; extend around entire circumference of shaft / Help long bone to resist twisting
Microscopic Anatomy of Spongy Bone
contains trabeculae, lamellarly arranged osteocytes & canaliculi
Trabeculae arranged along lines of stress; hips bone to resist stress
Trabeculae, like cables on a suspension bridge, confer strength to bone
Trabeculae onl a few cell layers thick; contain irregularly arranged lamellae & osteocytes interconnected by canaliculi
there are no osteons
nutrients (fromcapillaries in the endosteum) diffuse through canaliculi from the maroow spaces between the trabeculae to reach the osteocytes
Organic Components (Chemical Composition of Bone)
Includes osteogenic cells, osteoblasts, osteocytes, bone-lining cells, osteoclasts and osteoid
Osteoid, which makes up one-third of organic bone matrix, is secreted by osteoblasts
Consists of ground substance and collagen fibers, which contribute to high tensile strength and flexibility of bone
Inorganic Components (Chemical Composition of Bone)
Hydroxypatites (mineral salts)
Makeup 65% of bone by mass
Consist mainly of tiny calcium phosphate crystals in and around collagen fibers
responsible for hardness and resistance to compression
Bone is half as strong as steel in resisting compression and as strong as steel in resisting tension
Bone Development
Osteogenesis or ossification is the process of bone tissue formation includes:
Formation of bony skeleton in embryos
postnatal bone growth during childhood & adolescence
Bone remodeling and repair throughout life
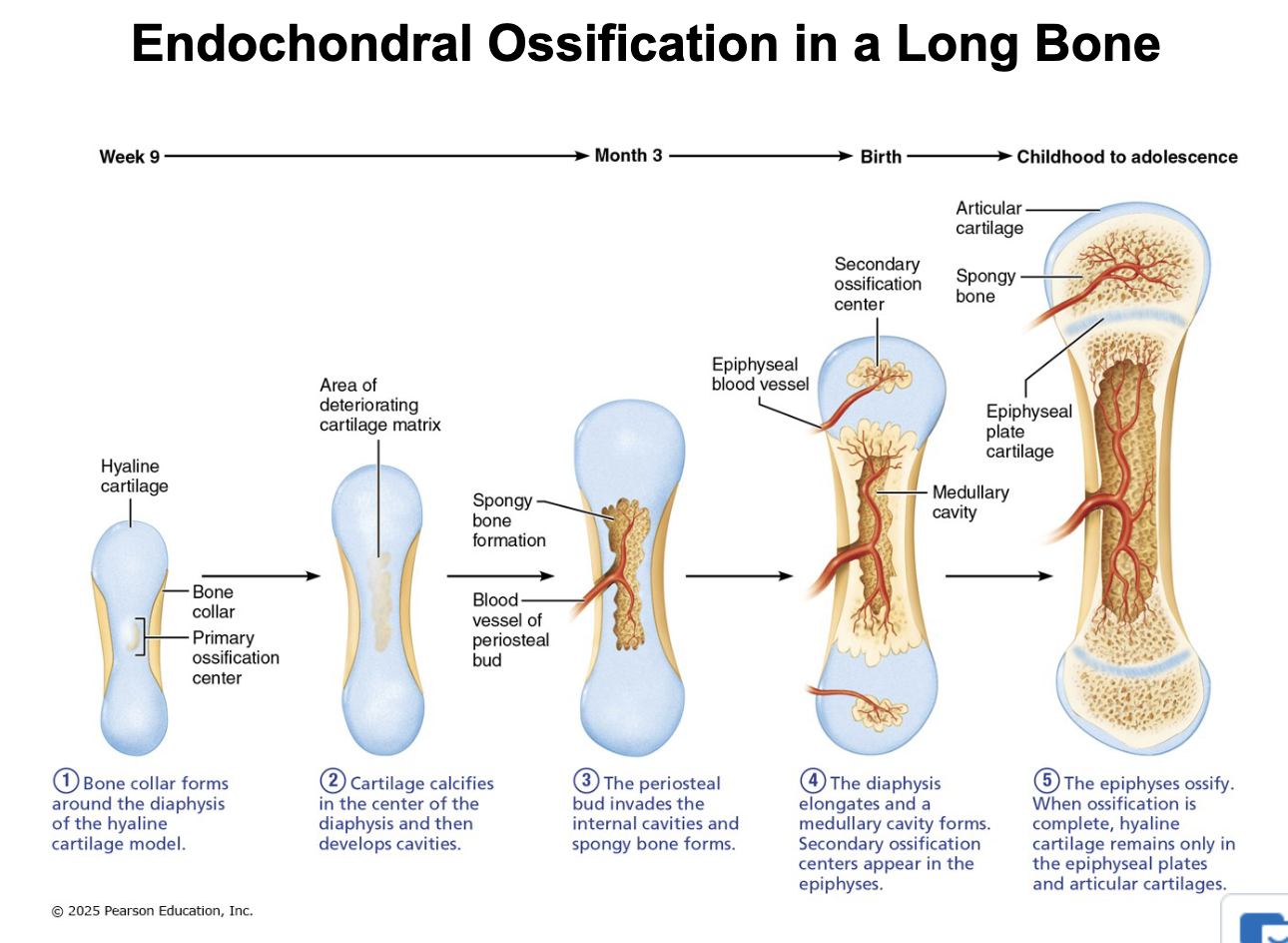
Endochondral Ossification
Bone forms by replacing hyaline cartilage model
Bones are called cartilage (endochondral) bones
Form most of skeleton / all bones below the skull (except the clavicles)
Begins in 2nd month
more complex
Intramembranous Ossification
Bone develops from fibrous CT membrane containing mesenchymal cells
Begins about 8 weeks of development & bones are called membrane bones
Cranial bones of the skull and clavicles - flat bones
NB: in short bones, only the primary ossification centre is formed; most irregular bones are formed using several distinct ossification centres
When secondary ossification is complete, hyaline cartilage remains:
on the epiphyseal surfaces as the articular cartilages
at the junctions of diaphysis and epiphyses where it forms the epiphyseal plates
Intramembranous ossification: begins within fibrous connective tissue membranes formed by mesenchymal cells
Four major steps are involved
Ossification centers are formed when mesenchymal cells cluster and become osteoblasts
Osteoid is secreted, then calcified
Woven bone is formed when osteoid is laid down around blood vessels, resulting in trabeculae
Lamellar bone replaces woven bone, and red bone marrow appears
Postnatal Bone Growth
During infancy & youth, long bones lengthen entirely by interstitial growth of the epiphyseal plates
All bones grow in thickness by appositional growth
Most bones stop growing during adolescence or in early adulthood - some facial bones (eg. nose & lower jaw) continue to grow (almost imperceptibly) throughout life
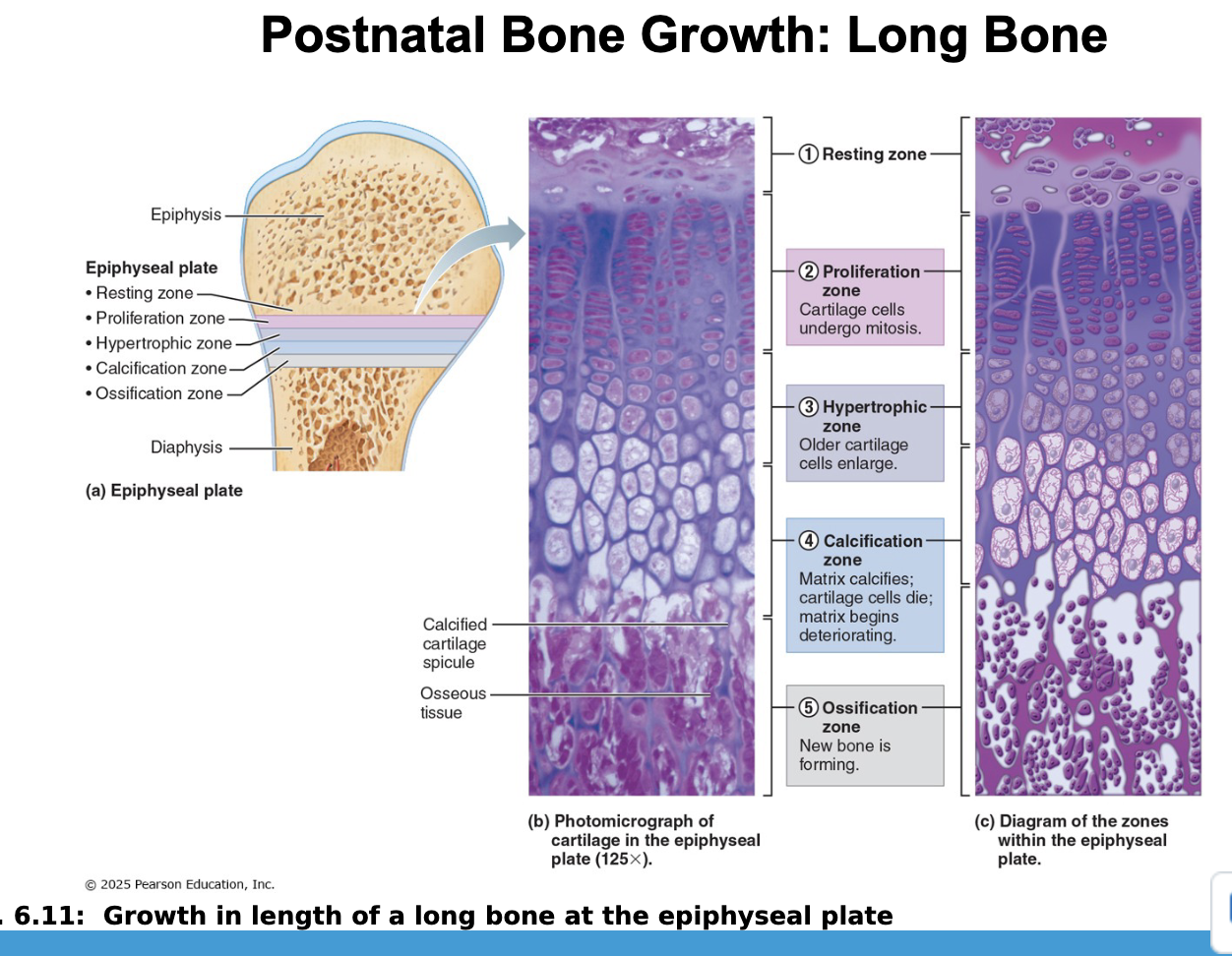
Growth in Length of Long Bones
Epiphyseal plate stays ~ same size throughout childhood & adolescence
Near the end of adolescence, chondroblast divide less often (cartilage cells in zone 2 multiply more & more slowly)
Epiphyseal plate becomes thinner longitudinal growth ends when bone of the epiphysis & diaphysis fuses = epiphyseal plate closure
About age 18 in females and age 21 in males
Growth in Width
growth in width = appositional growth
Bones thicken in response to increased stress from muscle activity or added weight
layers of bone are laid down on top of one another
primarily osteoblasts on periosteal side secreting bone matrix
primarily osteoclasts on the endosteal side remove bone matrix
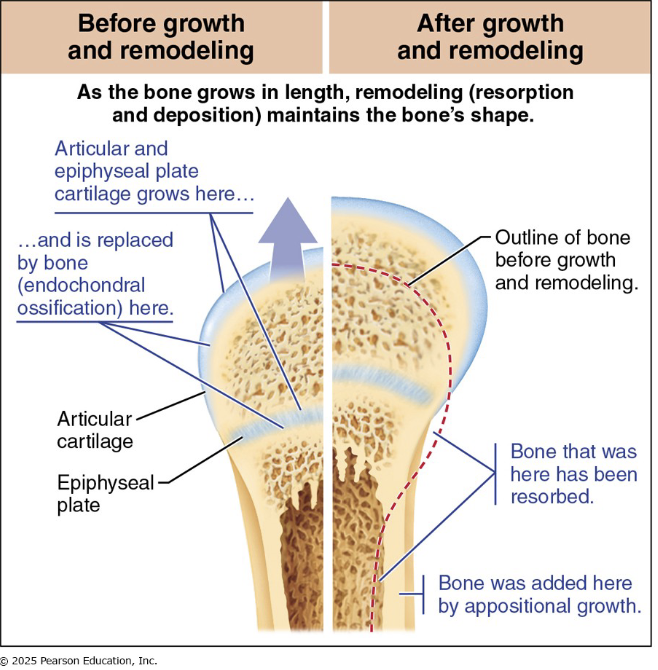
Long Bone Growth and Remodeling During Youth
As the long bone lengthens, the shape of the ends must be altered (remodeling)
Remember that the epiphyseal plates are located in the wider parts of long bones
Bone has to be reshaped to be incorporated into the diaphysis, but the diaphysis also has to be get thicker and stronger as the bone lengthens
In summary, bone is destroyed by osteoclasts and laid down by osteoblasts on both the inner and outer surfaces of a growing long bone
Growth Hormone (Hormonal Regulation of Bone Growth)
Most important hormone in stimulating epiphyseal plate activity in infancy and childhood
Thyroid Hormone (Hormonal Regulation of Bone Growth)
Modulates activity of growth hormone, ensuring proper proportions
Testosterone (males) and Estrogens (females)
At puberty promote adolescent growth spurts
End growth by inducing epiphyseal plate closure
Excesses (eg. acromegaly from too much GH) or deficits (pituitary dwarfism from GH insufficiency) of any hormones cause abnormal skeletal growth
Bone Modeling / Remodeling
Bone remodeling consists of both bone deposit and bone resorption
Occurs at surfaces of both periosteum and endosteum
Remodeling units: packets of adjacent osteoblasts and osteoclasts coordinate remodeling process
About 5-7 % of bone mass is recycled each week
Spongy bone replaced ~ every 3-4 years
Compact bone replaced ~ every 10 years
Resorption is function of osteoclasts
Dig depressions or grooves as they break down matrix
Secrete lysosomal enzymes and protons (H+) that digest matrix
Acidity converts calcium salts to soluble forms
Osteoclasts activation involved PTH (parathyroid hormone)
New bone matrix is deposited by osteoblasts
Osteoid seam
band of unmineralized bone matrix that marks area of new matrix
Calcification Front
Abrupt transition zone between osteoid seam and older mineralized bone
Control of Remodelling
Remodelling is regulated by two control loops
Maintaining Ca2+ homeostasis
negative feedback loop involving Parathyroid hormone (PTH) and Ca2+ in the blood
Keep bones strong: Mechanical and gravitational forces acting on bone drive remodeling to keep bone strong
Calcitonin
Released from parafollicular cells of thyroid gland in response to high levels of blood calcium levels
Effects are negligible, but at abnormally high doses it can lower blood Ca2+ levels temporarily
Bone Repair
Fractures are breaks
During youth, most fractures result from trauma
In old age, most result from weakness of bone due to bone thinning
Repair involved four major stages:
Hematoma Formation
Fibrocartilaginous callus formation
Bony callus formation
Bone remodeling
Key Events in Fracture Repair
Formation of a hematoma - local bone cells are deprived of oxygen and die; inflammation causes pain
Formation of a fibrocartilaginous callus (soft) - invaded by blood vessels that also bring macrophages to clean up the area; osteoclats also resorb damaged bone; fibroblasts, chondroblasts, osteoblasts get busy laying down collagen fibers and tissue components to span the break
Conversion to bony callus - cartilage converted to trabecular bone - complete in ~2 months
Bone remodelling - any extra bony material is removed; outer bone of shaft walls converted to compact bone and bone regains original shape
Final structure resembles original structure
Responds to same mechanical stressors
Osteoporosis
Group of diseases in which bone reorption → bone formation → bone becomes porous
some areas if skeleton especially vulnerable: spine, neck of femur
Risk Facts
Age
post menopausal women
estrogen promotes bone health by restraining osteoclast activity and promoting deposition of new bone
insufficient exercise
diet poor in calcium & protein
smoking (reduces estrogen levels)
Genetics
Dibaetes mellitus