Week 1: Pain Pathways and Central Processing
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
List the regions that send information to the somatosensory system. (5)
1. Skin
2. Muscle
3. Tendons
4. Ligaments
5. Connective tissue
List the stimuli that the somatosensory system detect. (6)
1. Touch
2. Brush
3. Pressure
4. Tickle
5. Temperature
6. Pain
What is the difference between nociception and pain?
Nociception: neural process of detecting harmful stimuli via Nociceptors, which are specialised sensory receptors that respond to noxious stimuli (intense chemical or physical stimuli that signal actual or potential tissue damage). This process involves specific nerve fibres, particularly activating C fibres, which transmit pain signals. THE NEURAL PROCESS
Pain: A feeling/perception of pain that is entirely subjective and has a psychological component. THE ACTUAL FEELING
List the different types of sensory receptors and what they detect. (4)
1. Mechanoreceptors - touch, pressure, vibration
2. Propioceptors - position of body
3. Thermoreceptors - warm, cool, hot
4. Nociceptors - mechanical, thermal, chemical (inflammatory mediators eg. PGs).
What are peripheral receptive fields?
Areas over which you can activate the sensory neurone, giving you a fine discrimination of where the pain is happening.Different area on our body have different sizes of receptive fields
Compare peripheral receptive fields of that to your finger tips vs back/thigs
Small field = finger tips
High precision , so can tell 2 point discrimination on 2 separate point
Bigger field = back , thigh
Low precision , fewer receptor spreads over a large area , so can tell 2 point discrimination on a singular point
What is transduction
When a physical stimulus hits the receptive field, it triggers a process called transduction, where the physical energy is converted into an electrical signal
What is convergence?
Single sensory neurone in CNS can receive inputs from multiple sensory receptors. Allows faithful representation of pain into CNS.
Explain how Mechanoreceptor in the skin will causes an action potential
Mechanoreceptors in the skin is touched → cause deformation of the membrane → open the Na + K channel , but more Na enters in cos of the conc gradient and K leaves→ receptor potential, local depolarisation of the receptive membrane ( non-propagated)→ action potential propagated to the CNS
Give features of the sensory system. (4)
1. Peripheral receptive fields
2. Convergence
3. Convert stimulus to AP
4. Convey intensity + duration of stimulus
Outline the process of transduction. (4)
1. Membrane deforms due to stimulus
2. Na+/K+ channels open
3. Receptor (generator) potential, local depolarisation of receptive membrane
4. AP propagated to CNS.
What determines the intensity of the stimulus? (3)
1. Number of APs
2. Size of responding receptor population
3. No. of fibres activated.
What is recruitment?
Increased number of responsive receptors and fibres due to stronger stimulus. = Activating more sensory receptors and fibres increases signal intensity.
State the sensory and muscle axons associated with proprioceptors, and how this determines their response.
Sensory: A⍺
Muscle: Group I.
Myelinated, largest diameter and fastest speed.
State the sensory and muscle axons associated with mechanoreceptors, and how this determines their response.
Sensory: Aβ
Muscle: Group II
Myelinated, smaller diameter than ⍺ and less speed.
State the sensory and muscle axons associated with nociceptors and thermoreceptors, and how this determines their response.
Sensory: Aδ, C
Muscle: Groups III and IV
C is unmyelinated. Smallest diameter and slowest speed.
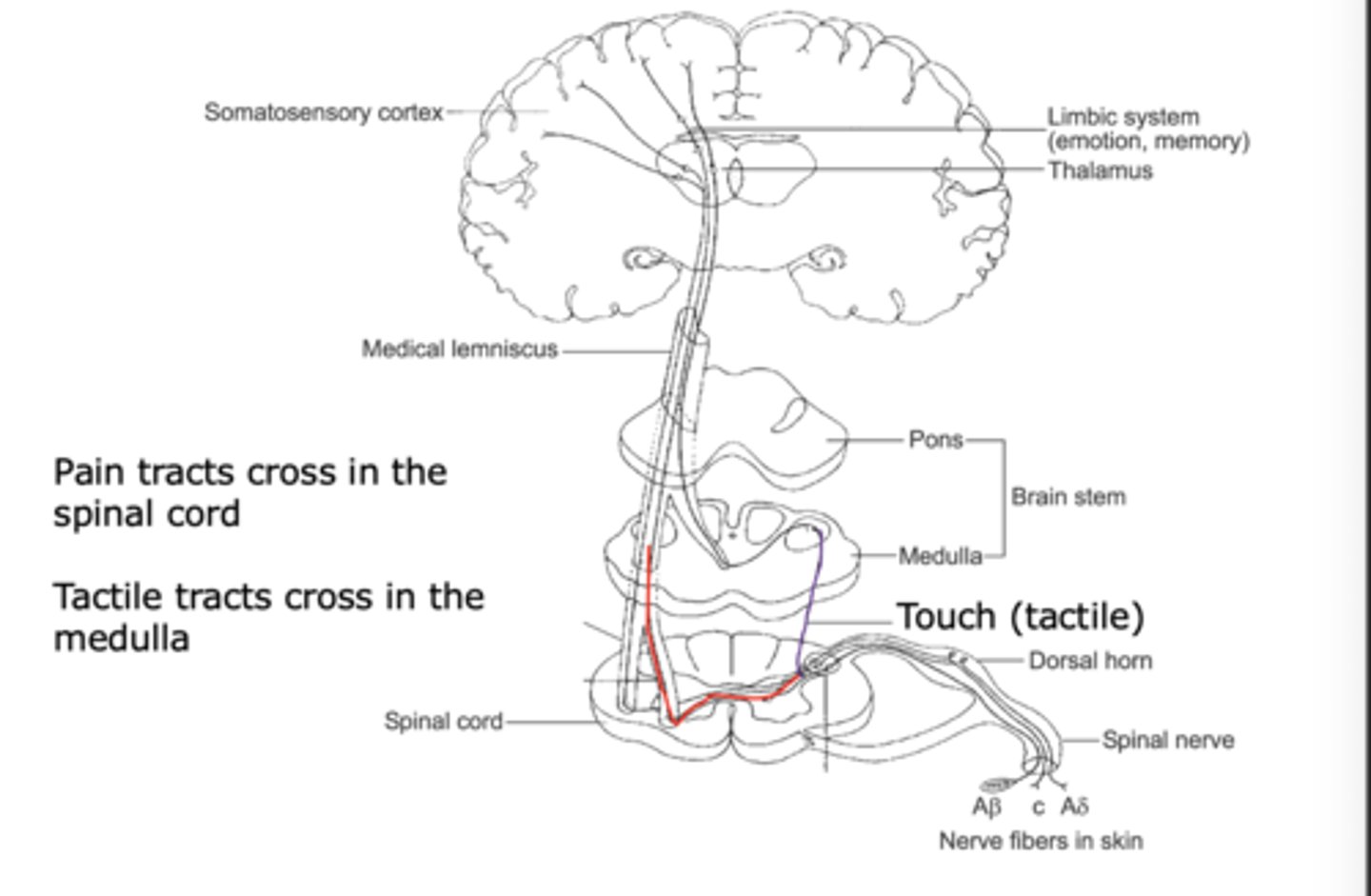
Explain how tactile messages are transmitted. (6)
FOR PROCESSING THE SENSE OF TOUCH
1. Tactile input from Aβ nerve fibres travels up to dorsal horn ipsilaterally.
2. Synapse in the dorsal column nuclei.
3. Cross midline in medulla and become contralateral.
4. Ascend through brainstem in this way as the medial lemnisus.
5. Synapse on cells of the thalamus.
6. Send projections to the primary somatosensory cortex (S-I), postcentral gyrus of parietal lobe.
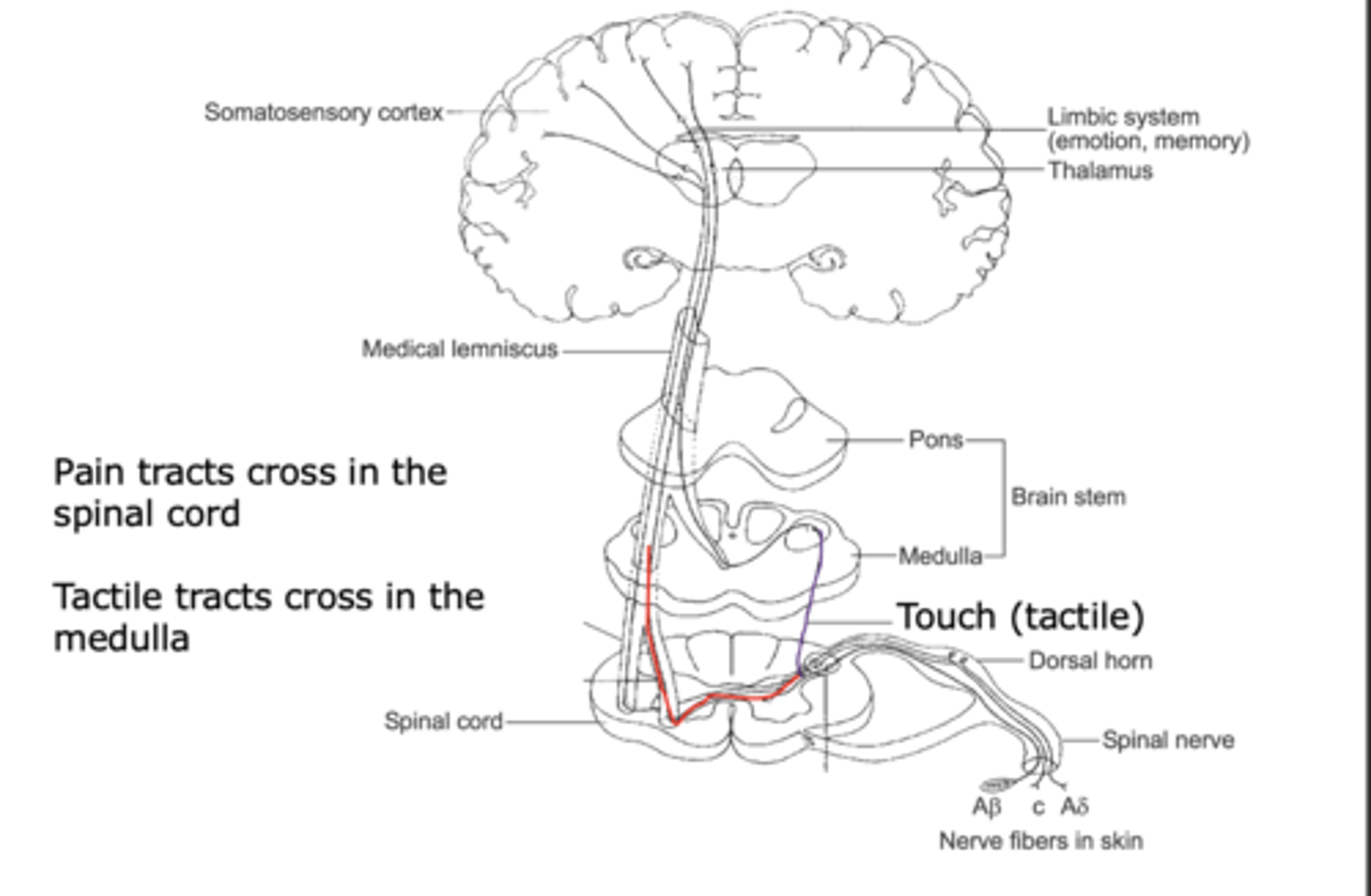
Which cells do tactile messages synapse with in the forebrain?
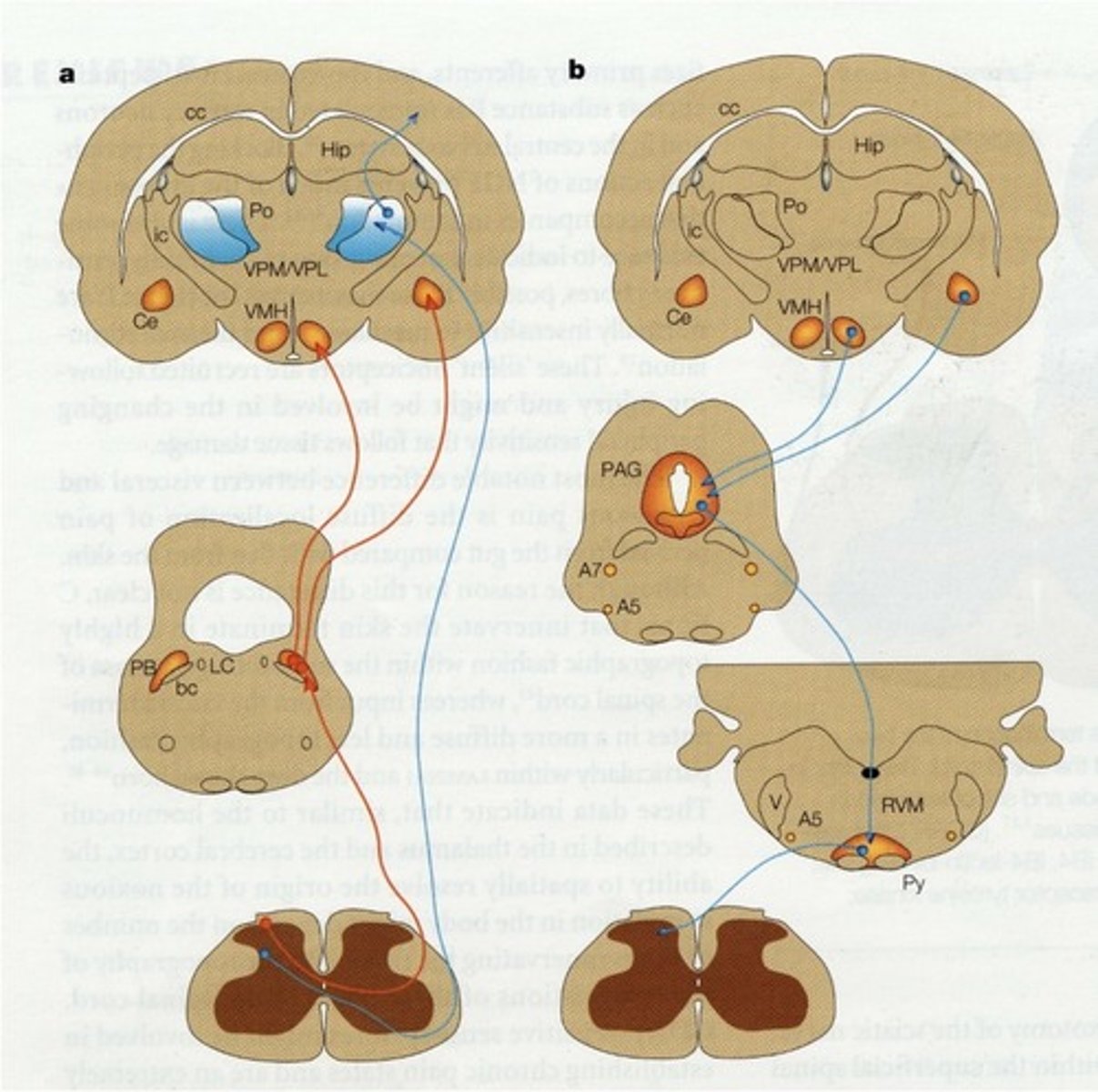
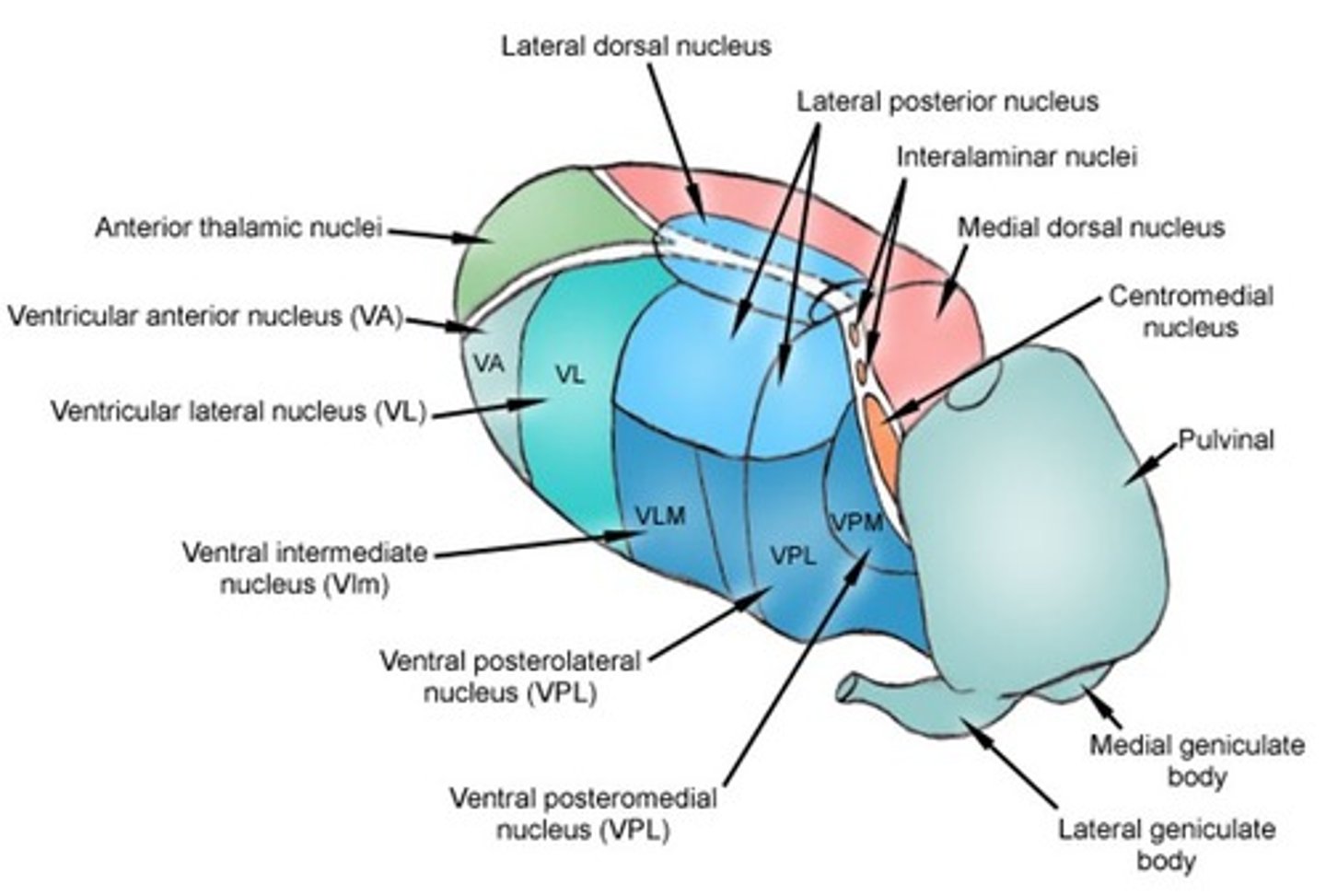
Ventral posterior medial (VPM) and ventral posterior lateral nuclei (VPL) of the thalamus (relays sensory info).
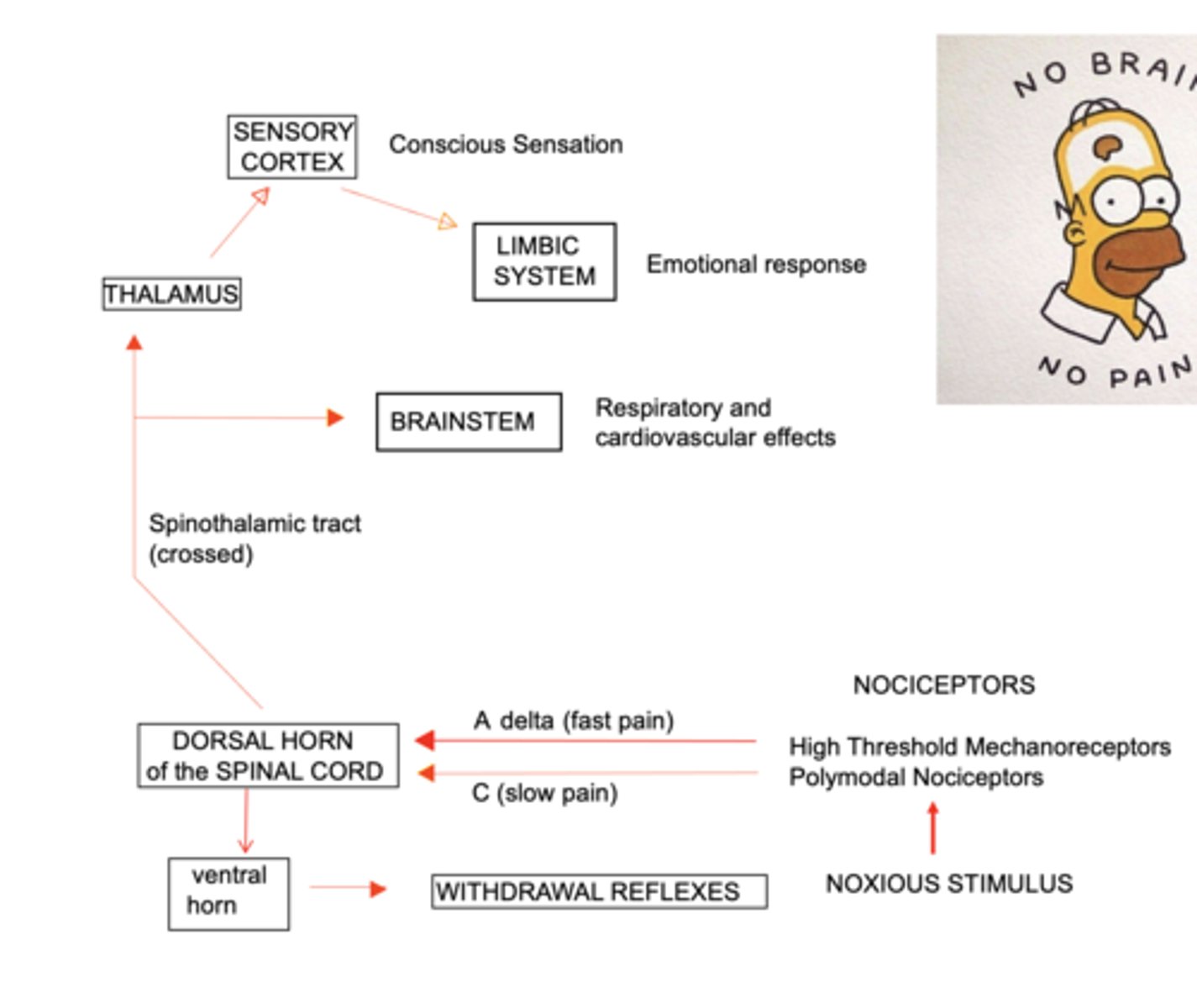
Explain how pain messages are transmitted. (2)
1. Pain input from Aδ and C fibres move contralaterally at level of spinal cord entered
2. Pathways ascend up to somatosensory cortex.
When can one override the immediate feeling of pain after sustaining an injury? (Descending pathway)
Eg. in a bad rugby injury, high endorphin levels can carry you through and the pain may hit much later i.e. you can override reflexes if you need to.
What is the sensory-discriminative component of pain?
Specification and location of pain - you've been hurt and where it is.
What is the emotional-affective component of pain?
Unpleasant emotions (suffering of pain) associated with the nociceptive stimulus.
What is a key issue with finding out if a patient is in pain?
If the patient is non-verbal i.e. cannot verbally communicate due to a disability or other, it does not mean they don't feel pain. We need other ways to assess pain for those who can't express it.
Explain the character and responsiveness of Aβ fibres. (2)
1. Myelinated and fast conduction
2. Response sensitive to glutamate receptor antagonists (AMPA receptor).
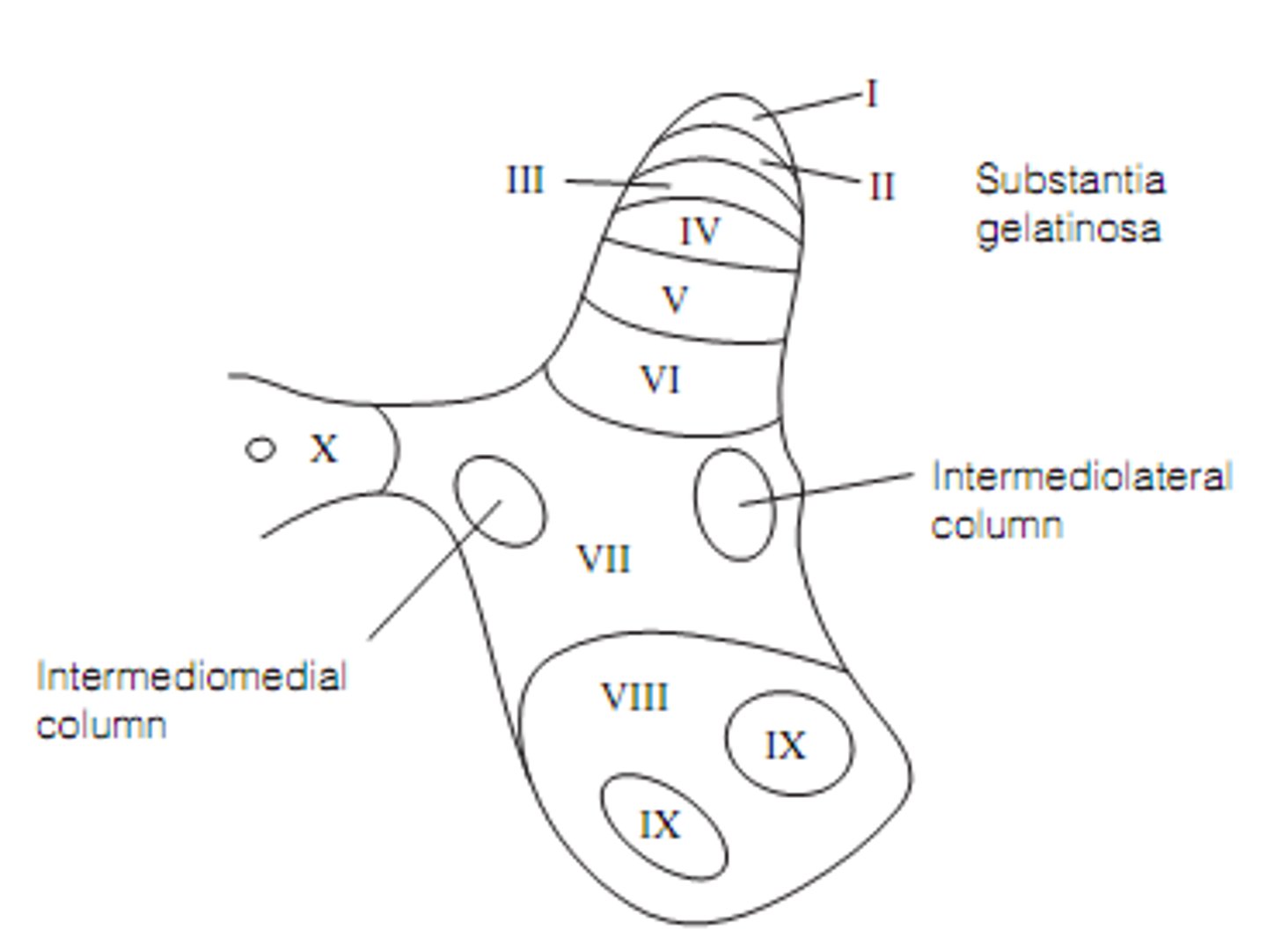
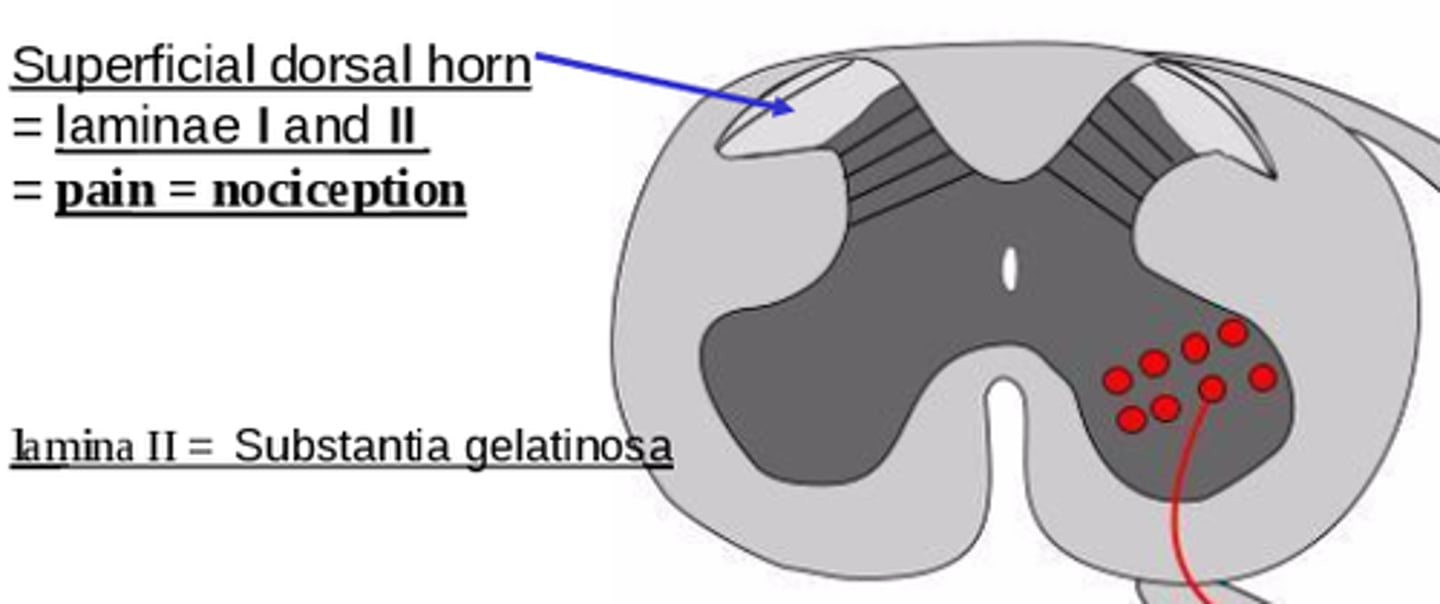
What is the termination site of Aβ fibres?
Point at which it stops to form a synapse
Intermediate lamina (III-IV) of dorsal horn (grey longitudinal column in spinal cord which has 6 laminae).
Explain the character and responsiveness of C-fibres. (2)
1. Unmyelinated, slow conduction
2. Response sensitive to glutamate receptor (AMPA and NMDA receptor) and peptide receptor antagonists i.e. release a combo of neurotransmitters.
What is the termination site of C-fibres?
Superficial lamina (I-II) of dorsal horn.
What types of messages does the dorsal horn of the spinal cord receive? (2)
- Innocuous (Aβ)
- Noxious (C)
Where do nociceptor afferents mainly terminate in the laminae of the dorsal horn?
Superficial - Laminae I and II (the most dorsal laminae).
What do signals from nociceptor afferents activate after terminating?
Second-order neurones in the spinal cord.
How does the spine process nociceptor afferents after they terminate? (2)
1. Nociceptor afferents activate 2nd-order neurones in spinal cord.
2. Projection neurones (from lamina I) project to brain (thalamus) via the spinothalamic tract, a main pain path.
What is the spinal parabrachial path?
A path from the dorsal horn which projects to the limbic system after an afferent terminates, controlling emotional response.
(red line in image)
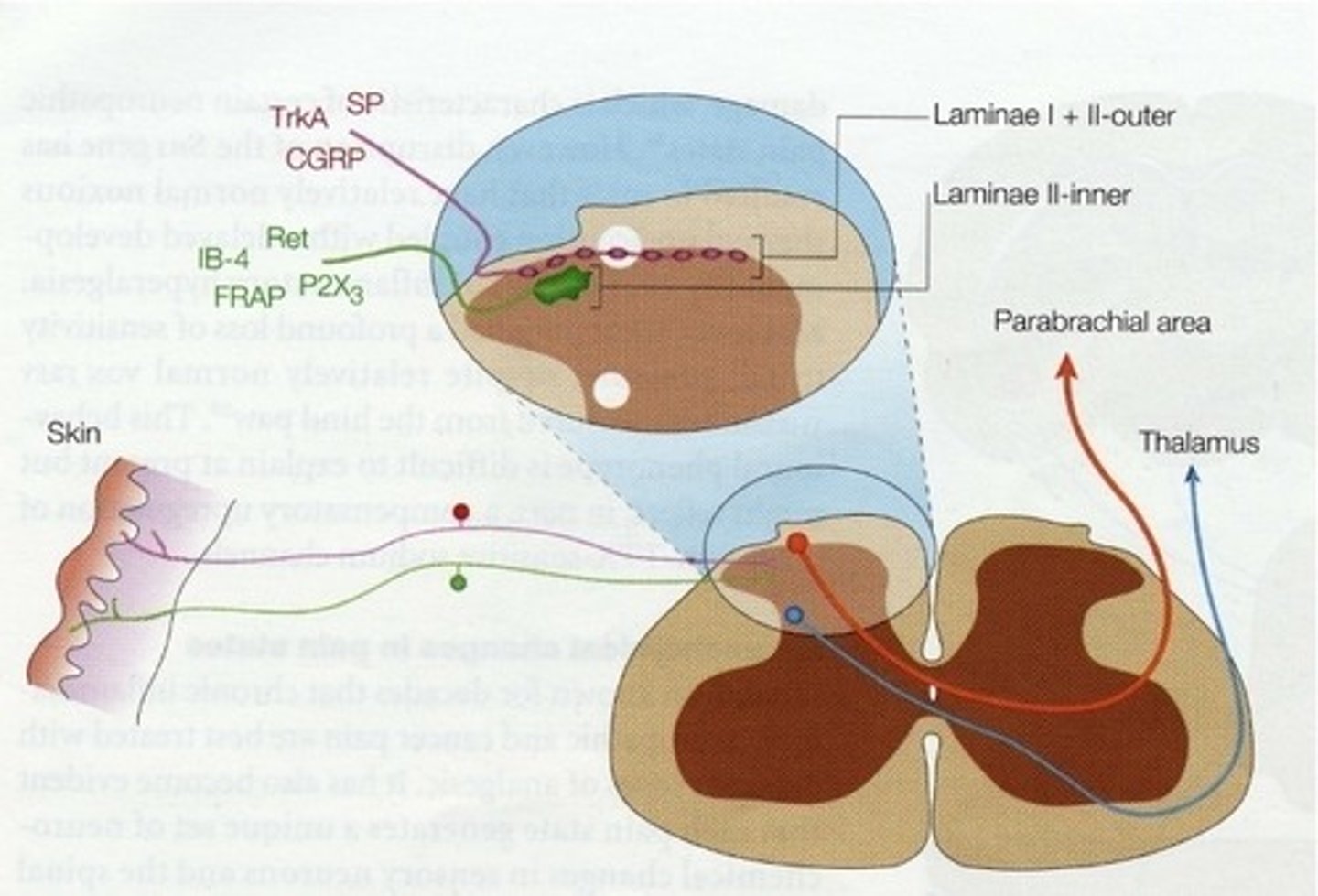
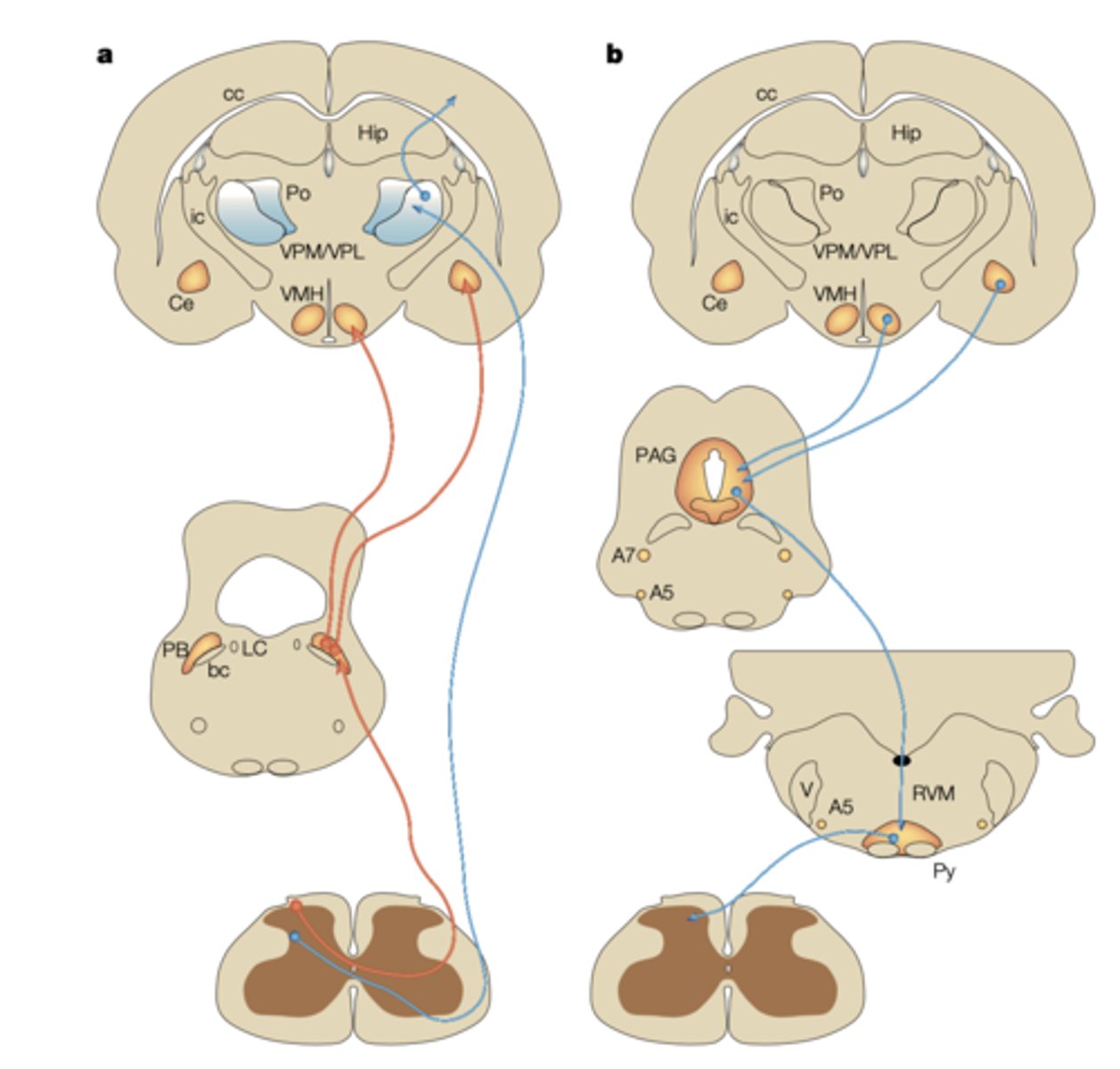
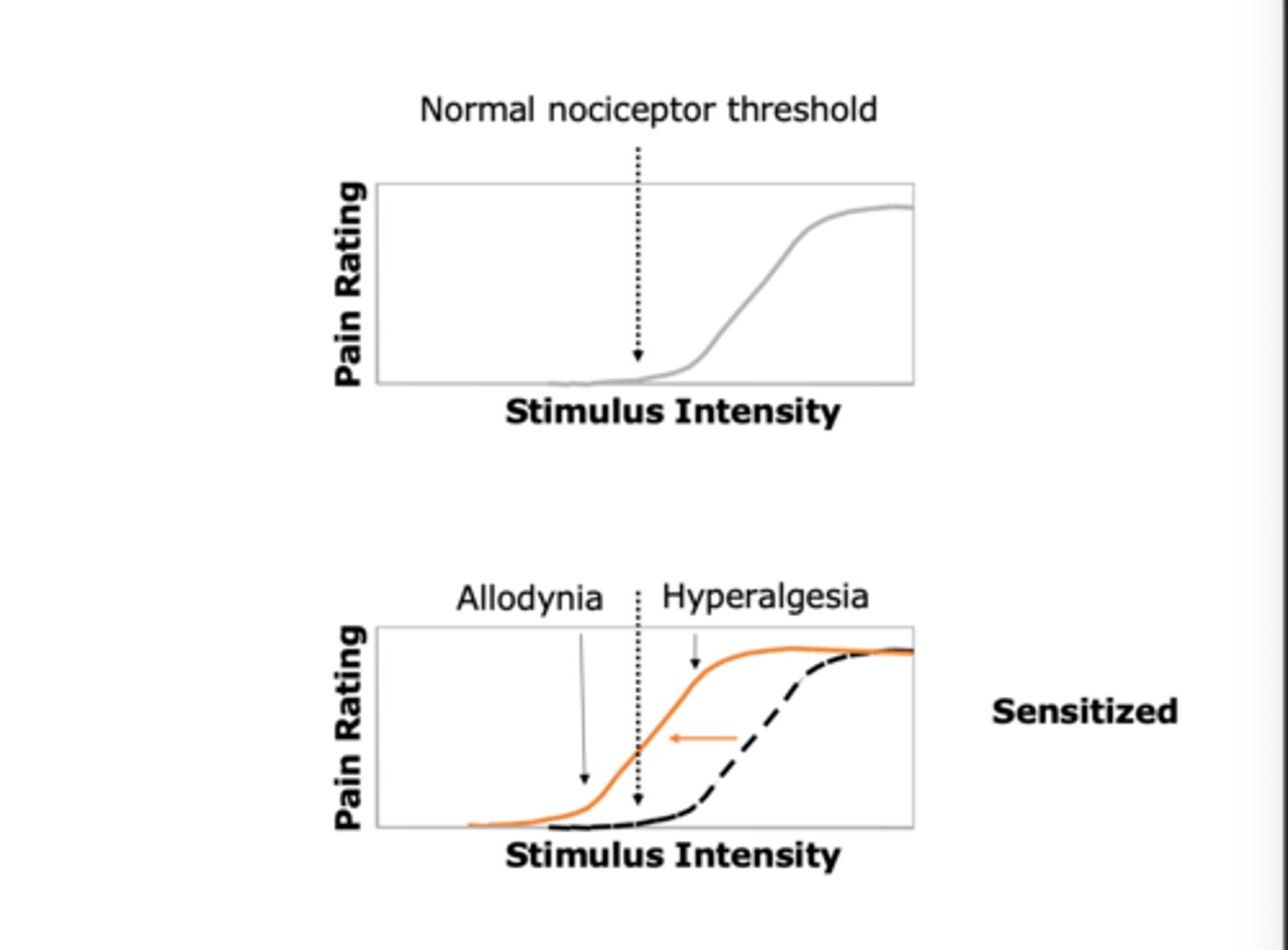
What are the 2 primary ascending nociceptive pathways?
1. Spinoparabrachial path (red) (from sup. dorsal horn) - deals with affect (emotion - limbic system).
2. Spinothalamic path (blue) projecting to cortex - deals with spacial discrimination and affect.
What reflexes can pain signals specifically set up?
Withdrawal reflexes - spinally-mediated nociceptive reflexes that lead to withdrawal from stimulus.
Dorsal horn activates ventral horn, causing reflex.
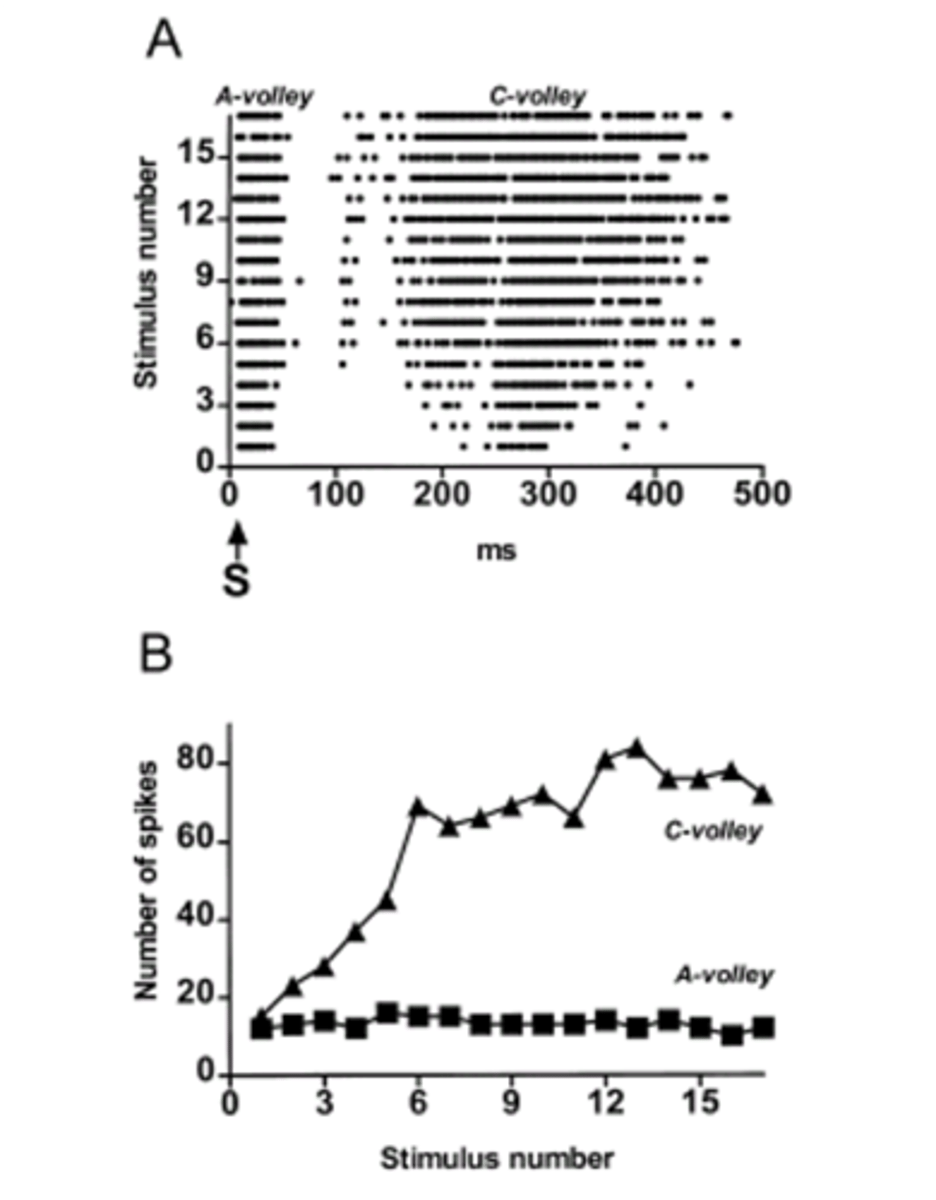
Explain the plasticity of spinal responses. (2)
This means that neuronal responses are not fixed
1. Responses to repeated C-fibre stimulation are not fixed and aren't always proportional to intensity of stimulus.
2. Spinal neurones can become sensitised to the noxious stimulus - central sensitisation.
What is wind-up?
Seen specifically with C-fibres (and thus noxious stimuli), if you keep stimulating at the same intensity in a specific area, the pain increases each time. It is a protective response for noxious stims, and is frequency dependent.
I.E. in graph - for stim no. 9, the A fibre has a short but rapid response, whilst the C fibre has a much larger and prolonged response for the same stim intensity.
What can central sensitization result in ?
Can result in allodynia (pain from non-painful stimuli) and hyperalgesia (exaggerated pain response).
What is central sensitisation?
Prolonged nociceptor input can lead to hypersensitivity from not normally painful stimuli - due to changes in dorsal horn of spinal cord.
What are enhanced responses for a given noxious stimulus associated with?
Repeated higher (0.5Hz) stimulation.
What is allodynia?
Stimuli that usually produce a small pain response now produce a large pain response i.e. previously non-painful stimuli cause pain.
Sensitization results in a leftward shift in the stimulus-response function, where non-painful stimuli become painful (allodynia) and painful stimuli feel much more intense (hyperalgesia)
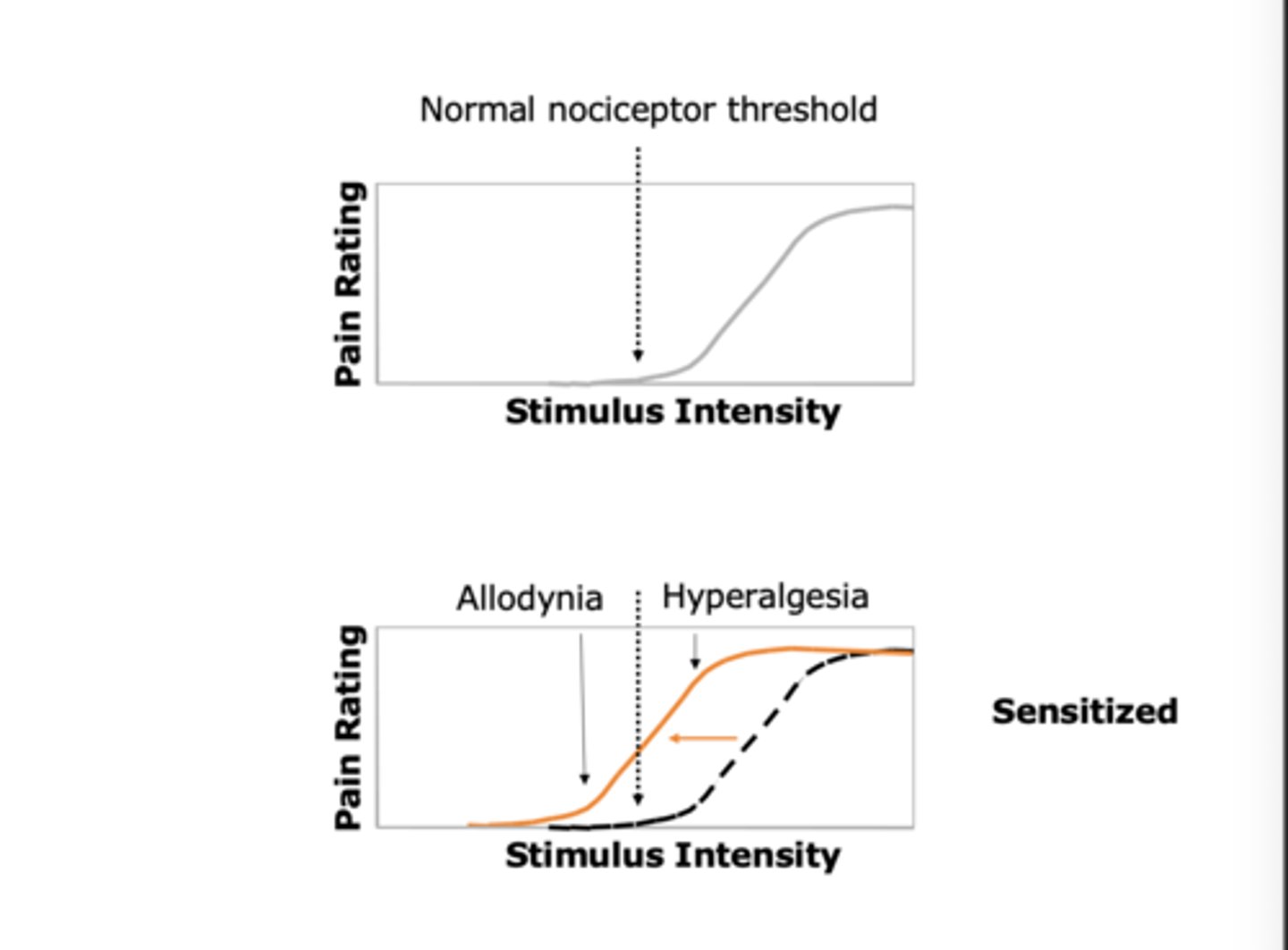
What is hyperalgesia?
Increased sensitivity to painful stimuli.
Sensitization results in a leftward shift in the stimulus-response function, where non-painful stimuli become painful (allodynia) and painful stimuli feel much more intense (hyperalgesia)
What are the ascending pain pathways? (4)
I.E. path with sensory info from body via spinal cord to brain.
1. Spinothalamic tract (SST) from Laminae 1 + 5 to thalamus
2. Post-synaptic dorsal column (PSDC) path
3. Spinoreticular tract (SRT)
4. Spinomesencephalic pathway
Explain the role of the spinothalamic tract
Projects from spinal cord laminae I and V to the thalamus.
Thalamus relays pain to the sensory cortex (conscious sensation) and limbic system (emotional response). = sensory-discriminative aspects of pain (identifying where it hurts and what kind of pain it is). It allows you to localize the stimulus on the body map in the somatosensory cortex
Explain the role of the Spinoreticular tract
from Deep laminae of the spinal cord to reticular formation in the brainstem
Activates brainstem systems controlling BP, respiration, and orientation.
for arousal and motivational aspects of pain. It triggers the "alert" system in the brain, causing changes in blood pressure, respiration, and general orientation toward the painful stimulus
Explain the role of the Spinomesencephalic Pathway tract
Originates from Laminae I to V and goes to the midbrain
Projects to midbrain areas for reflexive responses to pain.
reflexive responses to pain (like turning the head)
What are the components of the brain involved in processing? (4)
1. Brainstem
2. Thalamus
3. Cortex
4. Hypothalamus
What is the role of the brainstem in brain processing?
- Activated via Spinoreticular Tract and branches of Spinothalamic Tract
- Cause changes in BP, respiration and orientation to stimulus.
What is the role of the thalamus in brain processing?
- VPL (ventral posterior lateral nucleus) is the main somatosensory component, but others may be involved.
- Are final relay before signals reach cortex. - Relays signals to the cortex and limbic system.
What is the role of the cortex in brain processing?
Consciously perceive pain and involve limbic system (amygdala, hippocampus, hypothalamus, thalamus etc) for emotional response.
What is the role of the hypothalamus in brain processing?
Drive stress response to noxious stimulus via neuroendocrine changes and other behaviours.
What is the role of the limbic system in brain processing?
Limbic System: Emotional processing of pain
Give an overview of the spinal cord and brain response to a noxious stimulus.
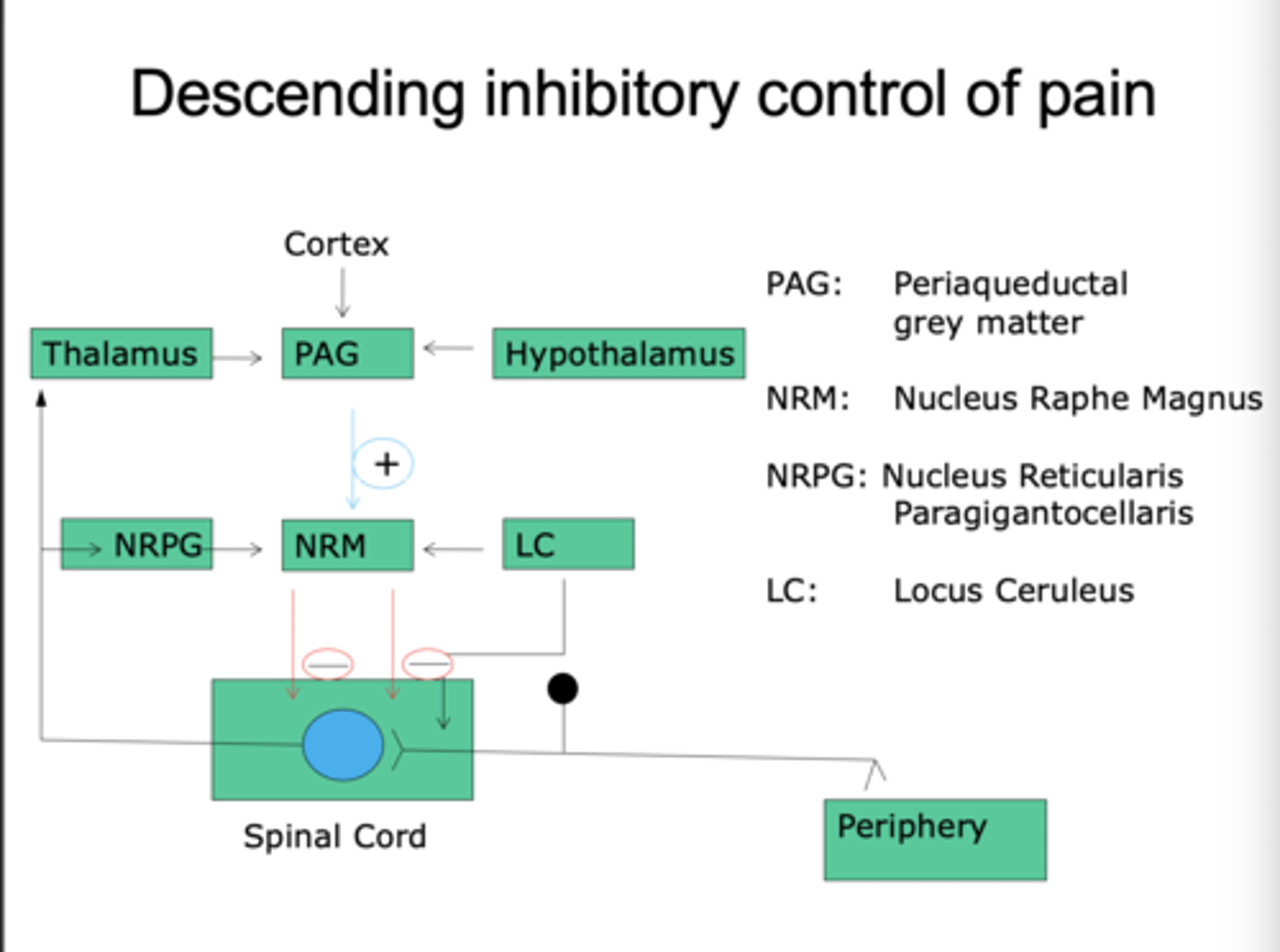
Outline the descending inhibitory control of pain. (4)
This is an excitatory path with inhibitory consequence, inhibiting any further pain response.
1. Starts in cortex, thalamus and hypothalamus.
2. Projects to periaqueductal grey (PAG) matter in midbrain. - this starts the descending pain inhibition
3. PAG sends messengers from nucleus raphe magnus, with contributions from locus coeruleus (which Regulates pain signals) and nucleus reticularis paragigantocellularis (rostral ventral medulla). → →Receives input from the PAG and sends inhibitory signals to the spinal cord.
4. then Inhibits spinal cord response.
Part of fight or flight response, help you override pain and withdrawal reflexes. So we can run away from the danger
Descending pathways inhibit nociceptive transmission in the spinal cord.