Mucosal immunology
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
31 Terms
What is a mucosal surface?
a membrane that lines various cavities in the body and covers the surface of internal organs.
It consists of one or more layers of epithelial cells overlying a layer of loose connective tissue.
Mucosal immunity’s responsabilities
Protects against infection
Determines relative risk
Limits harmful immune responses
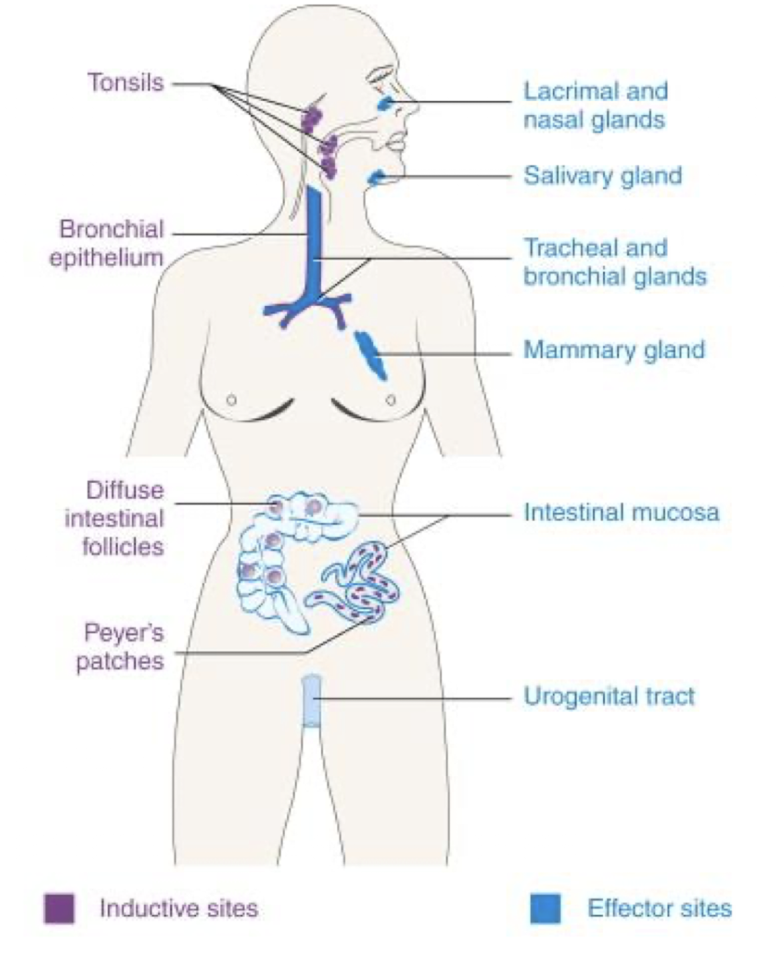
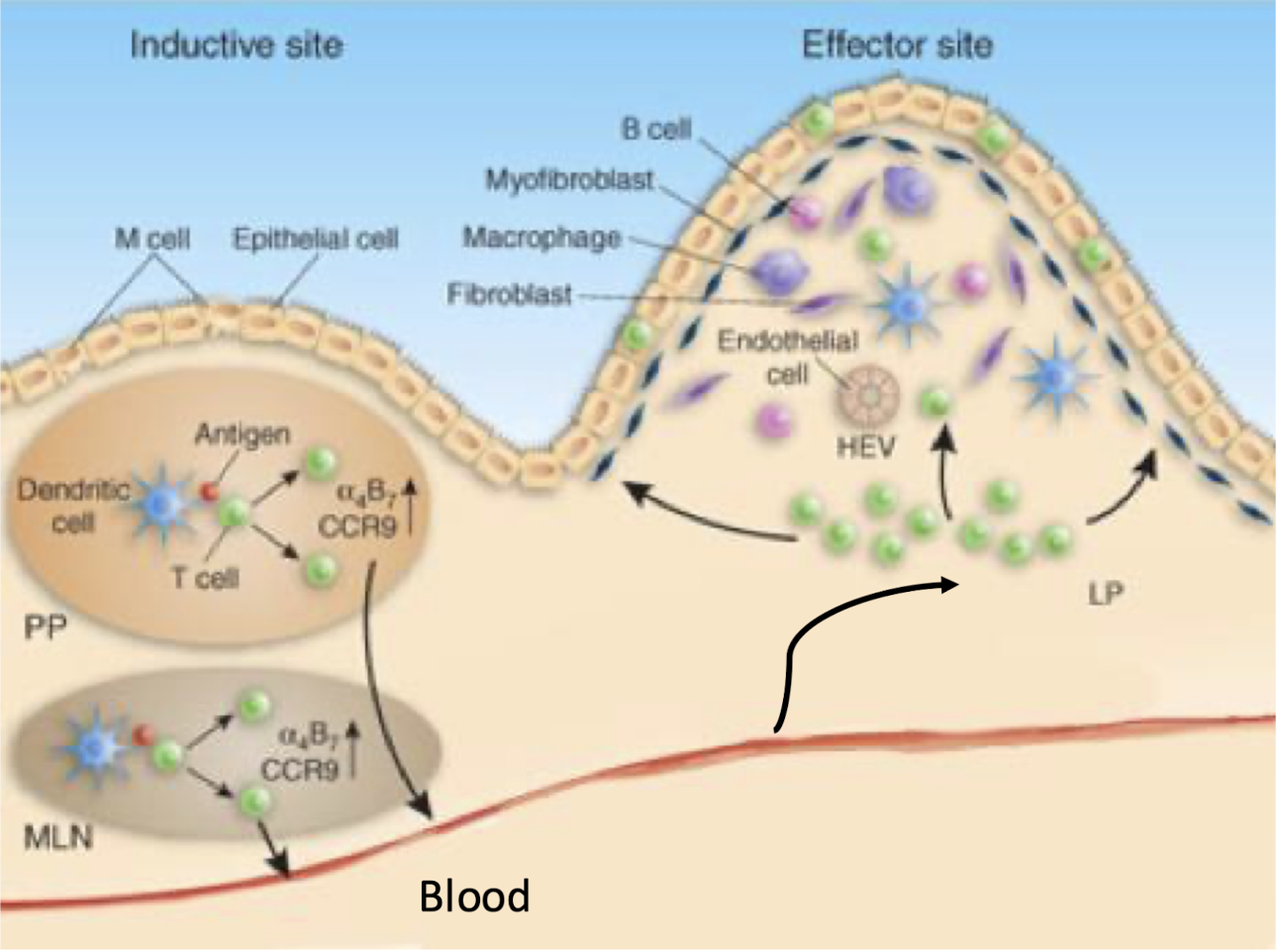
What are the inductive and effector sites of the mucosal immune system?
Inductive sites: NALT, tonsils/adenoids, BALT, GALT, Peyer’s patches, solitary nodules, appendix.
Effector sites: nasal mucosa, upper respiratory tract, lacrimal & salivary glands, mammary glands, intestines, genitourinary tract.
What challenge must mucosal immunity balance?
Immune Surveillance = detect & eliminate pathogens
Oral tolerance = avoid reacting to harmless food/self antigens
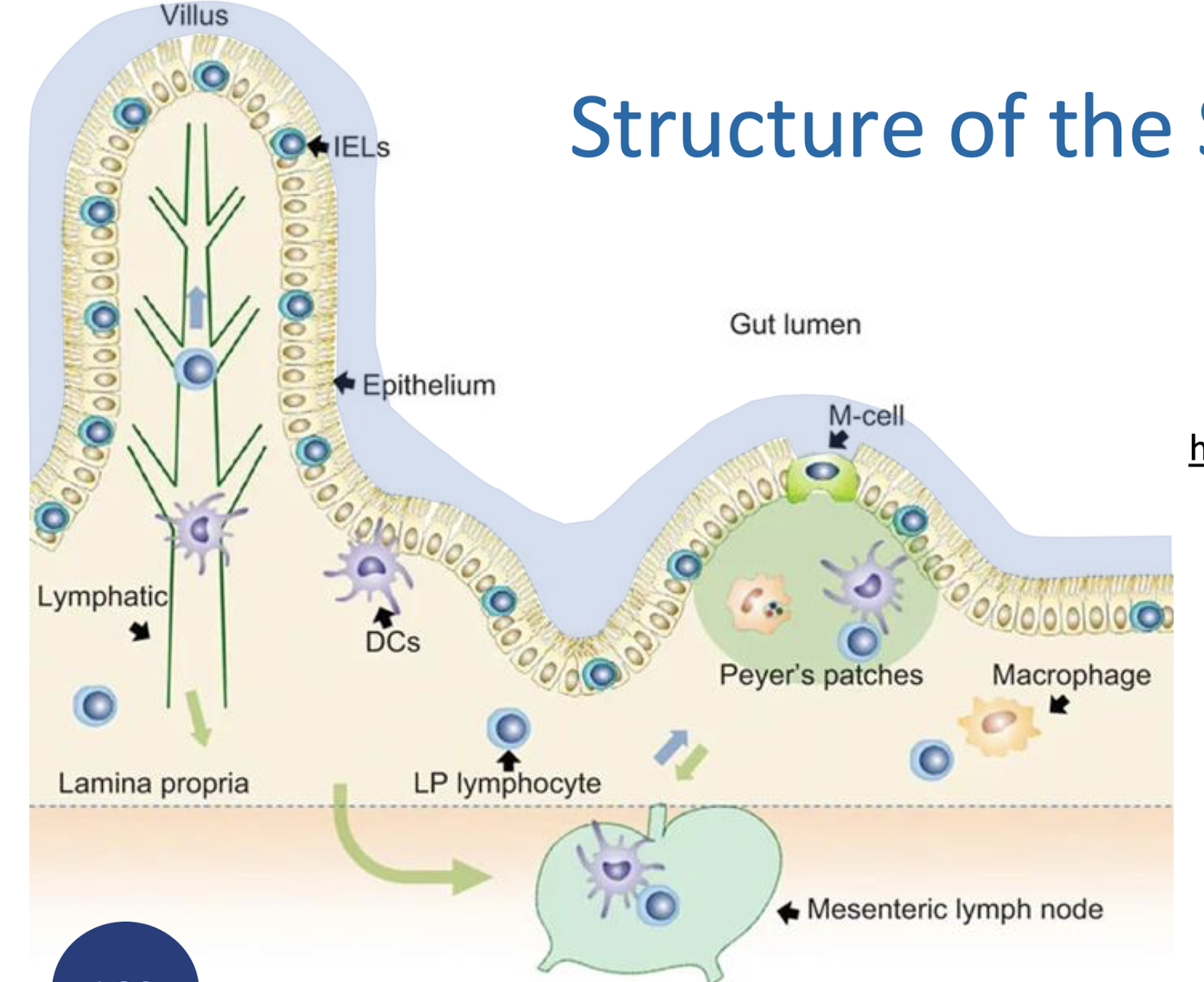
What are key structural components of the small intestine mucosal system?
Mucous Gel Layer (MGL)
Glycocalyx
Epithelium
Lamina propria
Draining mesenteric lymph nodes
What are the components & functions of the Mucous Gel Layer (MGL)?
Components:
Water
Secreted mucins
Tethered mucins
Trefoil factors
Functions:
Protective barrier
Molecular sieve
Lubrication
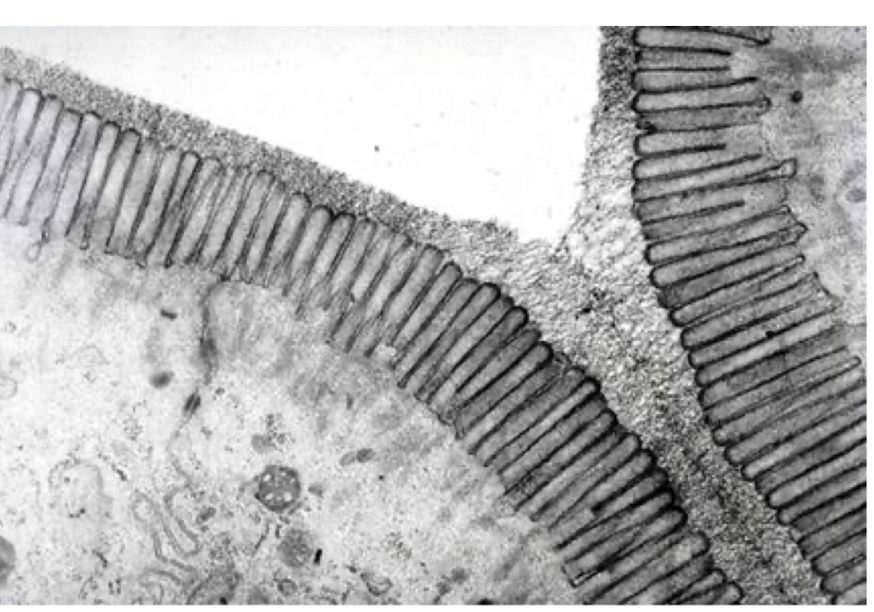
What is the glycocalyx and what are its functions?
A carbohydrate-rich coating on epithelial cells.
Functions:
Recognises luminal antigens
Protective coating for bacteria
Supports epithelial adhesion
What are the five epithelial cell types of the gut?
Absorptive enterocytes
Goblet cells
Enteroendocrine cells
Paneth cells
Stem cells
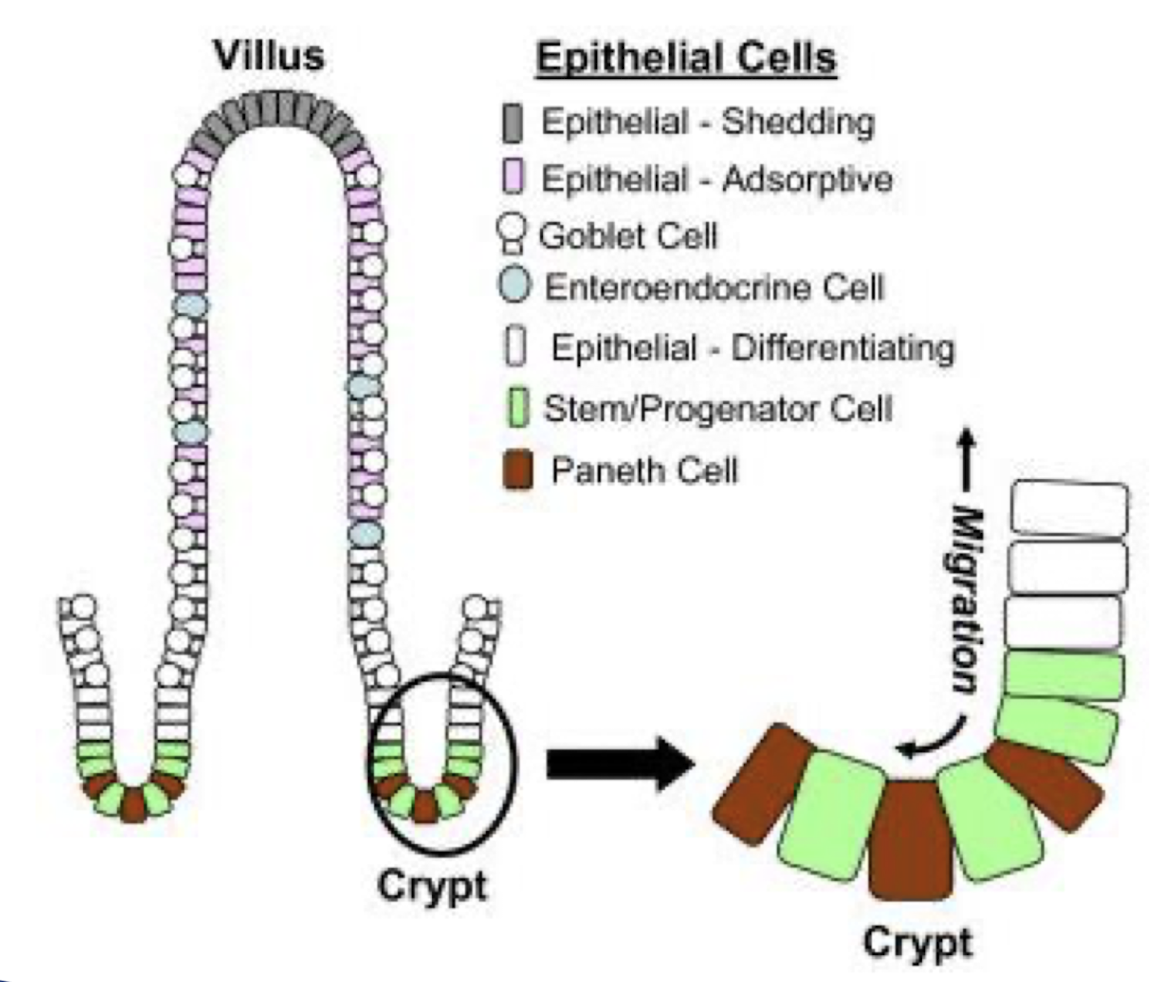
Absorptive enterocytes
- Absorb water/nutrients/fat micelles/vitamins
- Secrete water as part of Enteric Tear Mechanism
Enteroendrocrine cells
Secrete digestive hormones e.g. CCK (cholecystokinin) which regulate digestive processes and coordinate gut function.
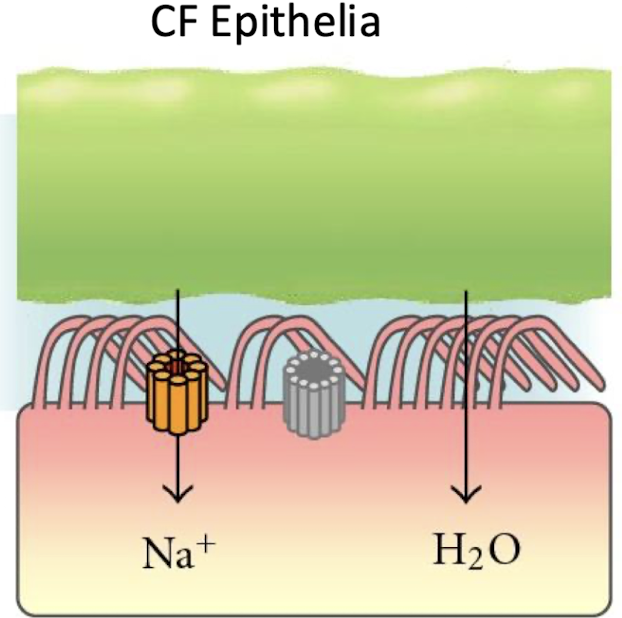
What is the Enteric Tear Mechanism?
Enterocytes secrete water via CFTR- mediated chloride efflux; this “tear” flushes microbes away.
Loss of this mechanism predisposes to disease.
CFTR - Cystic fibrosis transmembrane conductance regulator

What are the three main antigen classes in the gut?
Microbiome-derived antigens
Dietary antigens
Self antigens (e.g., anoikic epithelial cells)
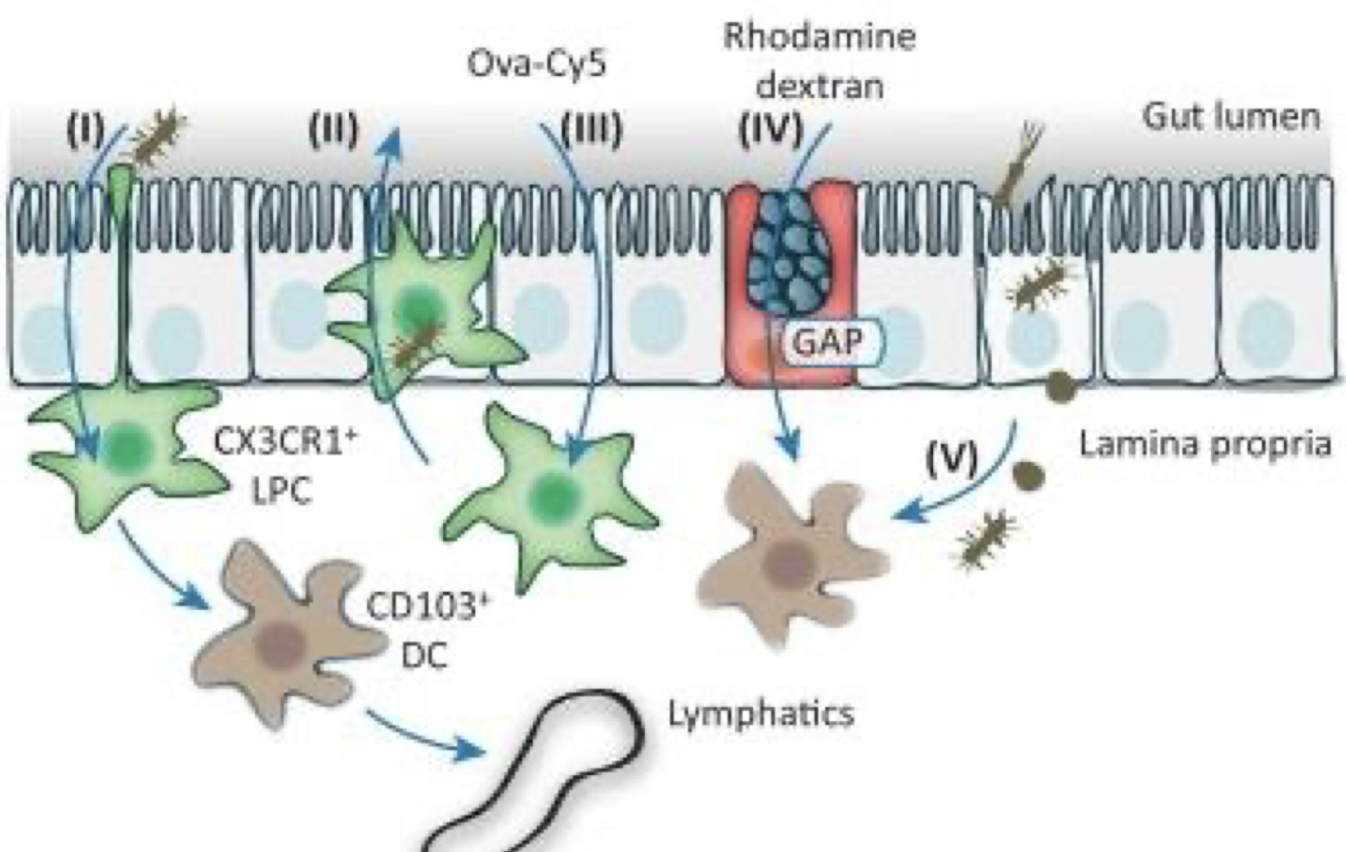
What are the five mechanisms of antigen sampling?
1. Tissue-resident phagocytes expressing CCR CX3CR1 extend dendrites into the lumen.
2. CX3CR1+ LPCs cross the epithelium.
3. Soluble antigens diffuse across the epithelium.
4. Goblet-cell-associated antigen passages (GAPs) deliver Ag
5.DC acquisition via apoptotic phagocytic cell uptake or membrane fragment handover
What is oral tolerance?
Induction of regulatory immune responses in Peyer’s patches and mesenteric nodes to prevent activation against harmless dietary or commensal antigens.
Describe the three steps towards neutrophil degranulation (NETosis)
Immune trigger (DAMPs/PAMPs)
Chemoattractant signalling (e.g., Leukotriene B4, complement derived C5a)
Degranulation → NET release

What are common mucosal immune diseases?
Gastric ulcer
Cystic fibrosis
Coeliac disease
Crohn’s disease
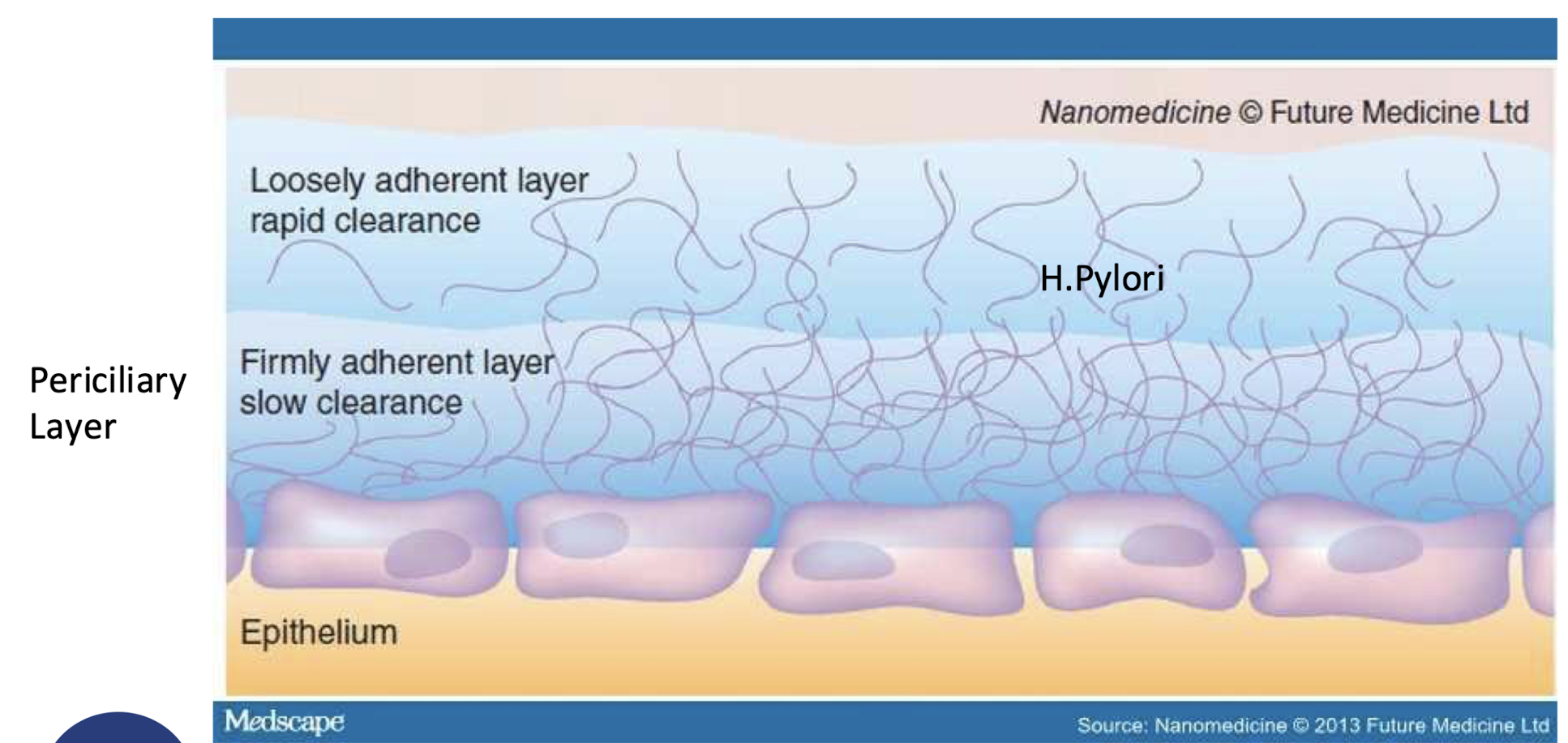
Name the six causes of gastric ulcer
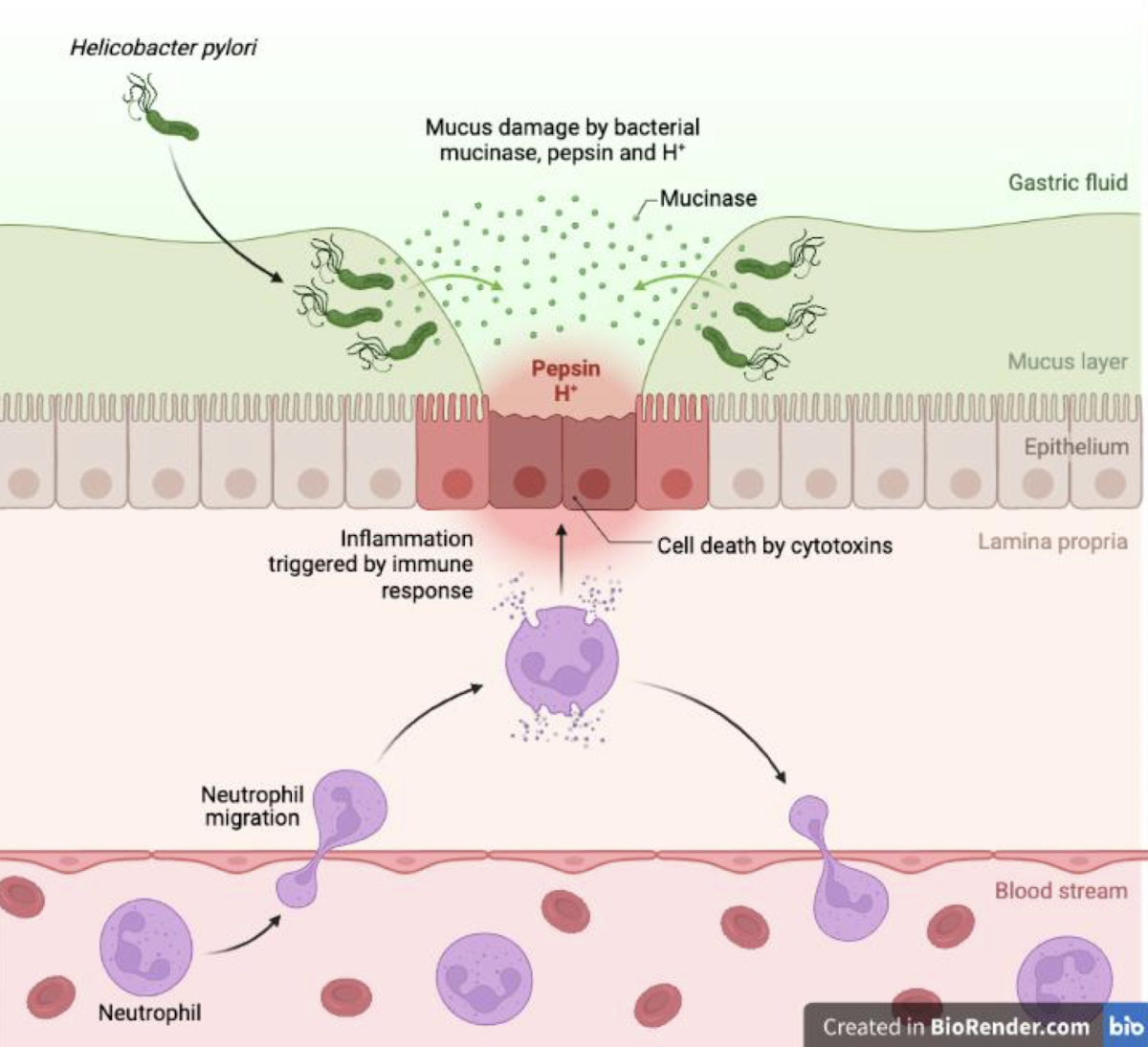
H. pylori
NSAIDs (Non-steroidal Anti-Inflammatories)
Stress
Smoking
Alcohol
Genetics
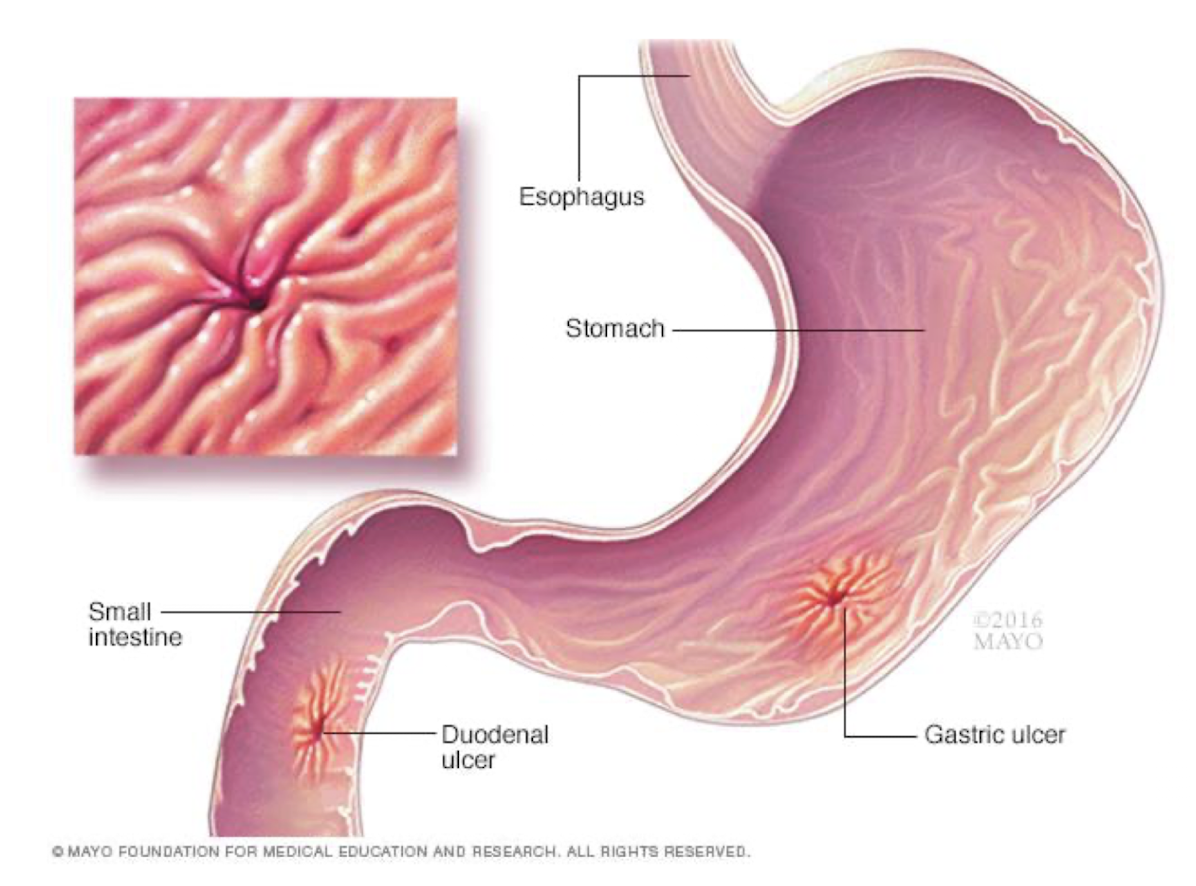
What is “triple therapy” for gastric ulcers?
Proton-pump inhibitor (omeprazole/lansoprazole)
Clarithromycin
Amoxicillin
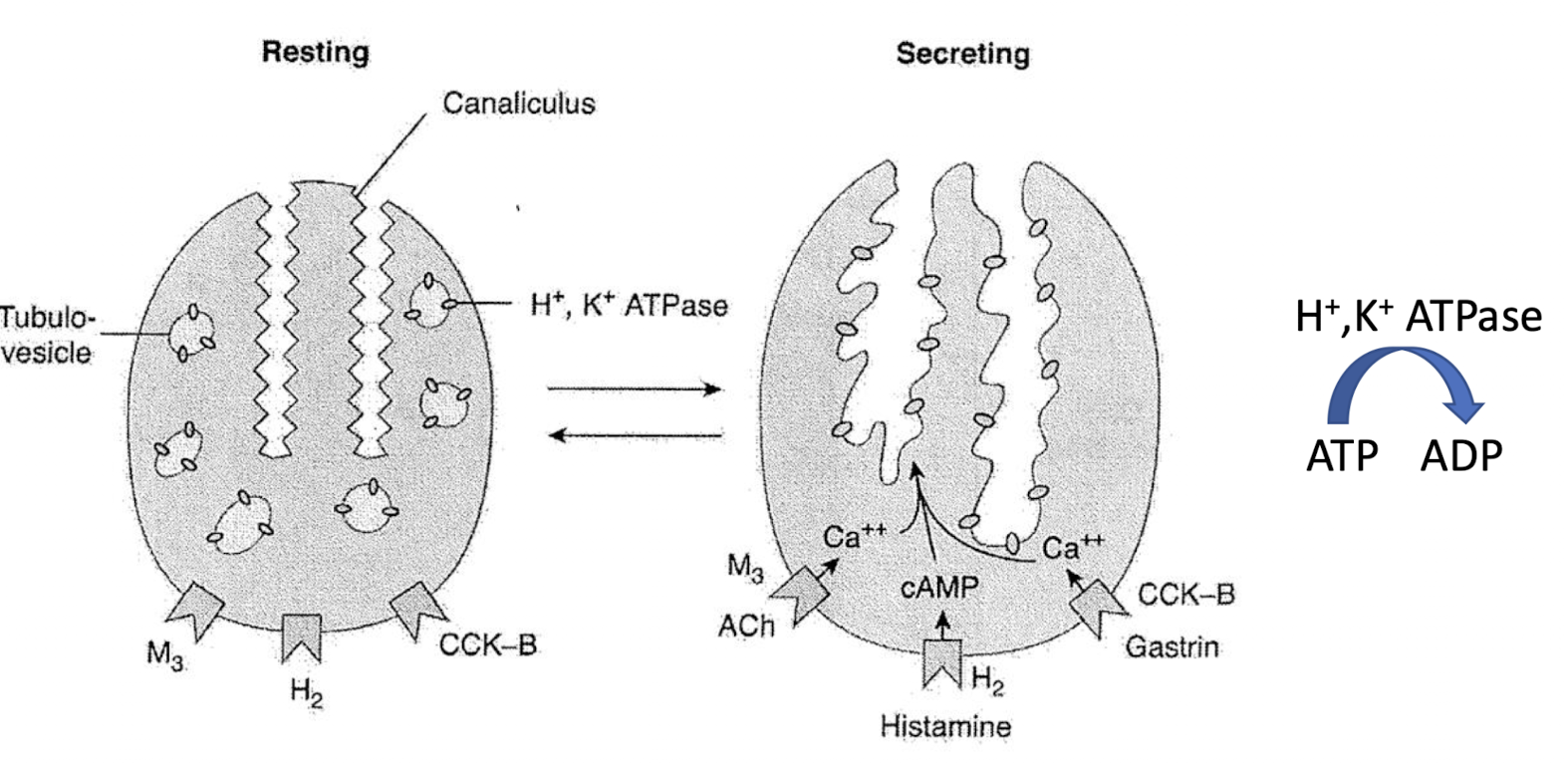
Gastric ulcer mechanism
Cystic fibrosis transmembrane conductance regulator (CFTR)
Membrane protein and chloride channel in vertebrates that is encoded by the CFTR gene.
The CFTR gene codes for an ABC transporter-class ion channel protein that conducts chloride ions across epithelial cell membranes
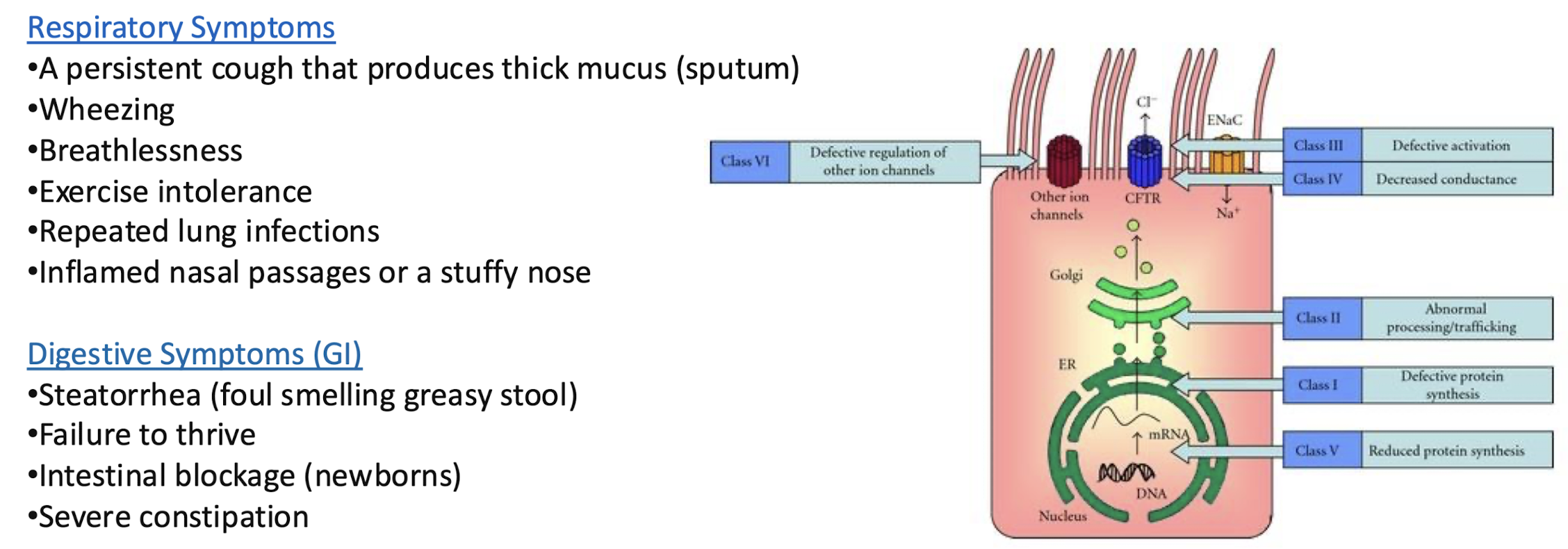
List 10 common symptoms of cystic fibrosis
Respiratory Symptoms
• A persistent cough that produces thick mucus (sputum)
•Wheezing
•Breathlessness
•Exercise intolerance
•Repeated lung infections
•Inflamed nasal passages or a stuffy nose
Digestive Symptoms (GI)
•Steatorrhea (foul smelling greasy stool)
•Failure to thrive
•Intestinal blockage (newborns)
•Severe constipation
List three treatment options for cystic fibrosis
mucolytics, antibiotics, gene therapy
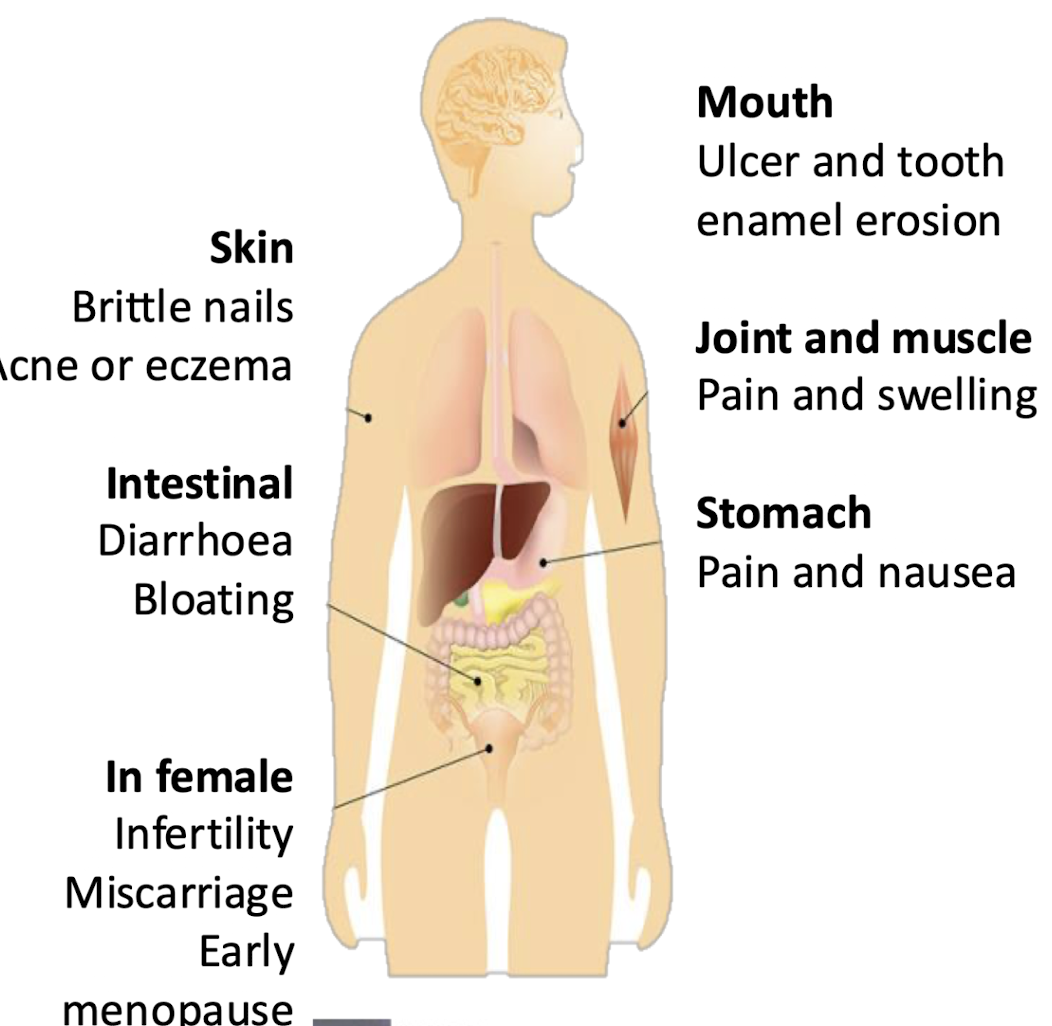
What are the main symptoms of coeliac disease?
Mouth ulcers, enamel loss, joint pain, skin rashes, diarrhoea, bloating, (in women) infertility, miscarriage, etc.
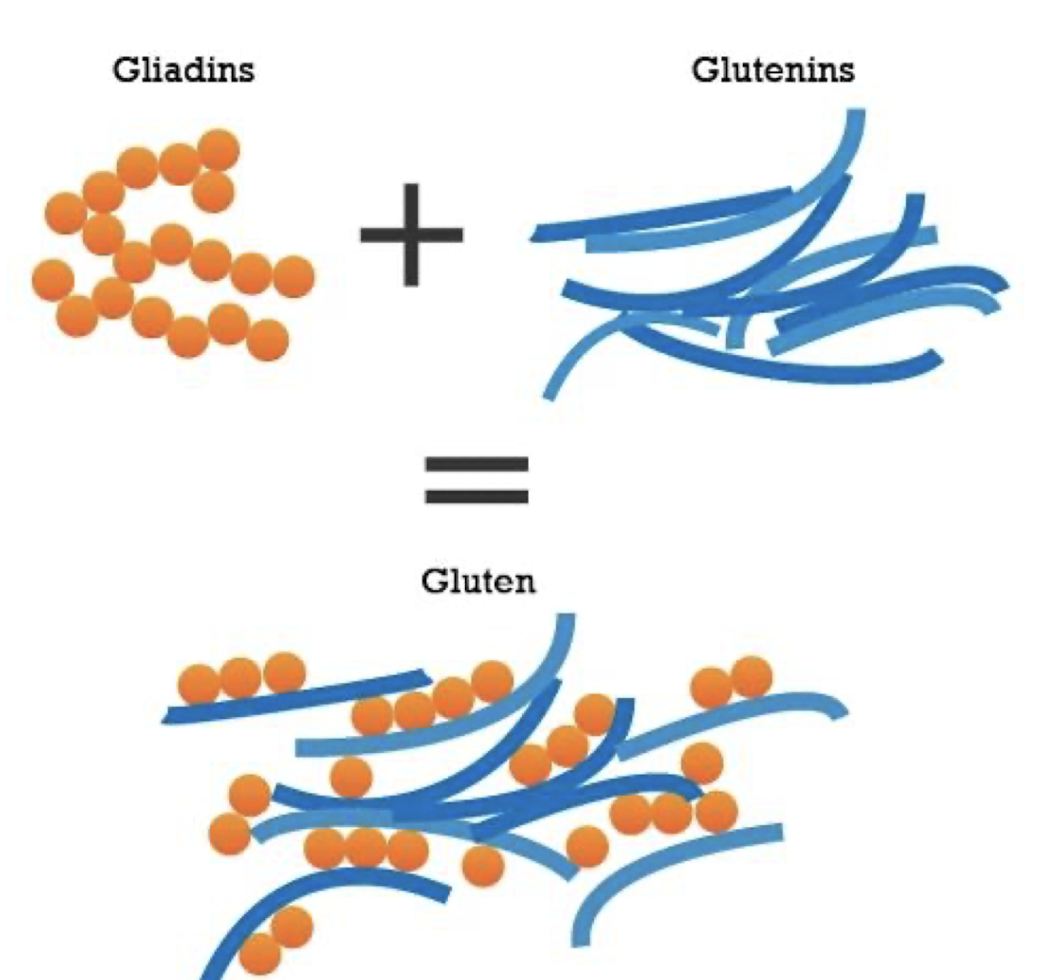
what 2 components make up gluten?
Gliadin and glutenin.
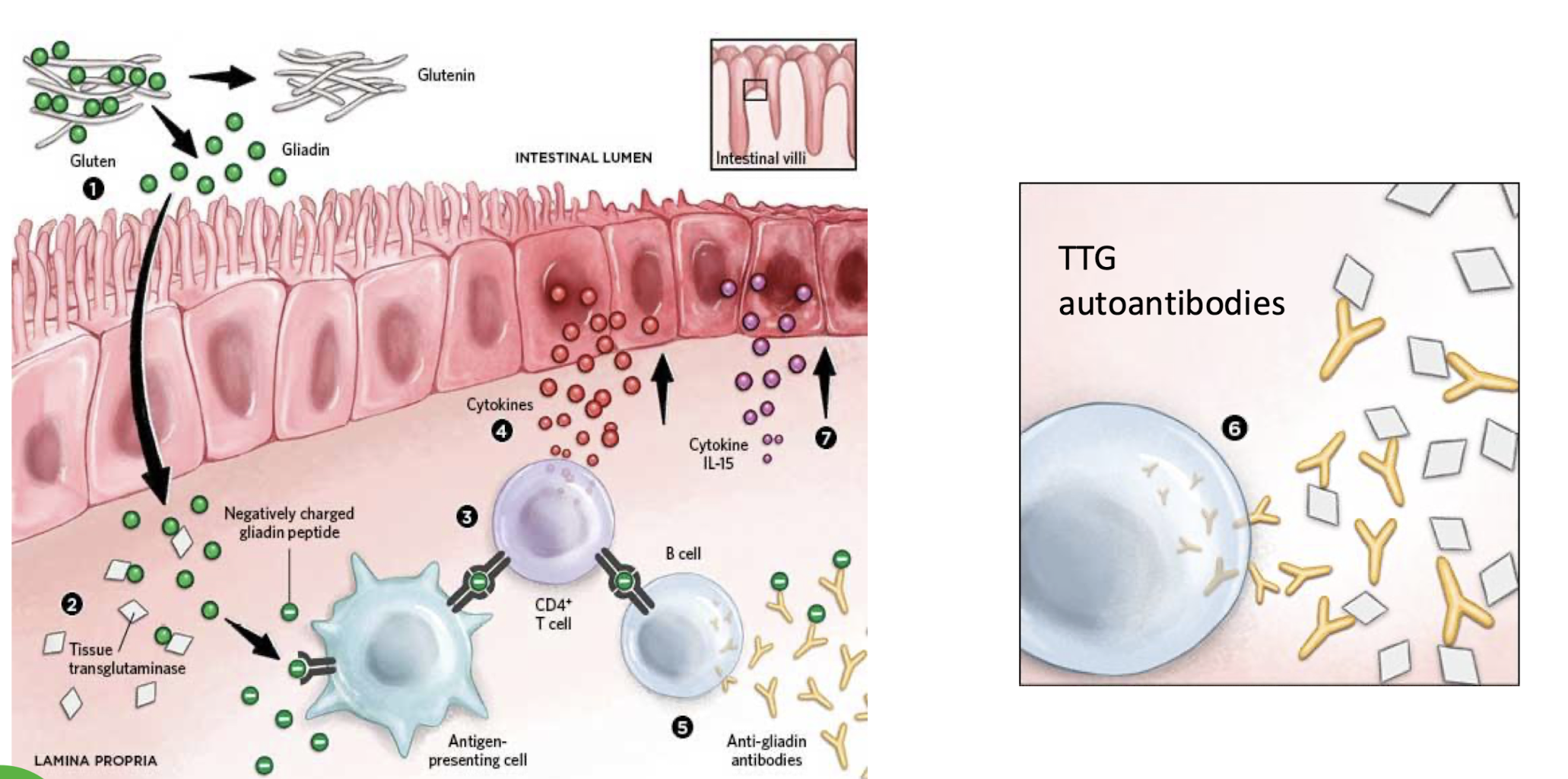
List the 7 steps of Celiac Disease progression
Gliadin exposure
Deamidation by tissue transglutaminase
Activation of antigen-specific T cells i.e. CD4+ by APC that detect - charged gliadin peptide
Cytokine release i.e. IL-15
Anti-gliadin Ab formation
Production of autoantibodies against transglutaminase
Intestinal mucosal damage and villous atrophy
What are the four susceptibility factors for IBD?
1. Genetics Susceptibility
2. Barrier disruption
3. Excessive Neutrophilia
4. T cell miseducation
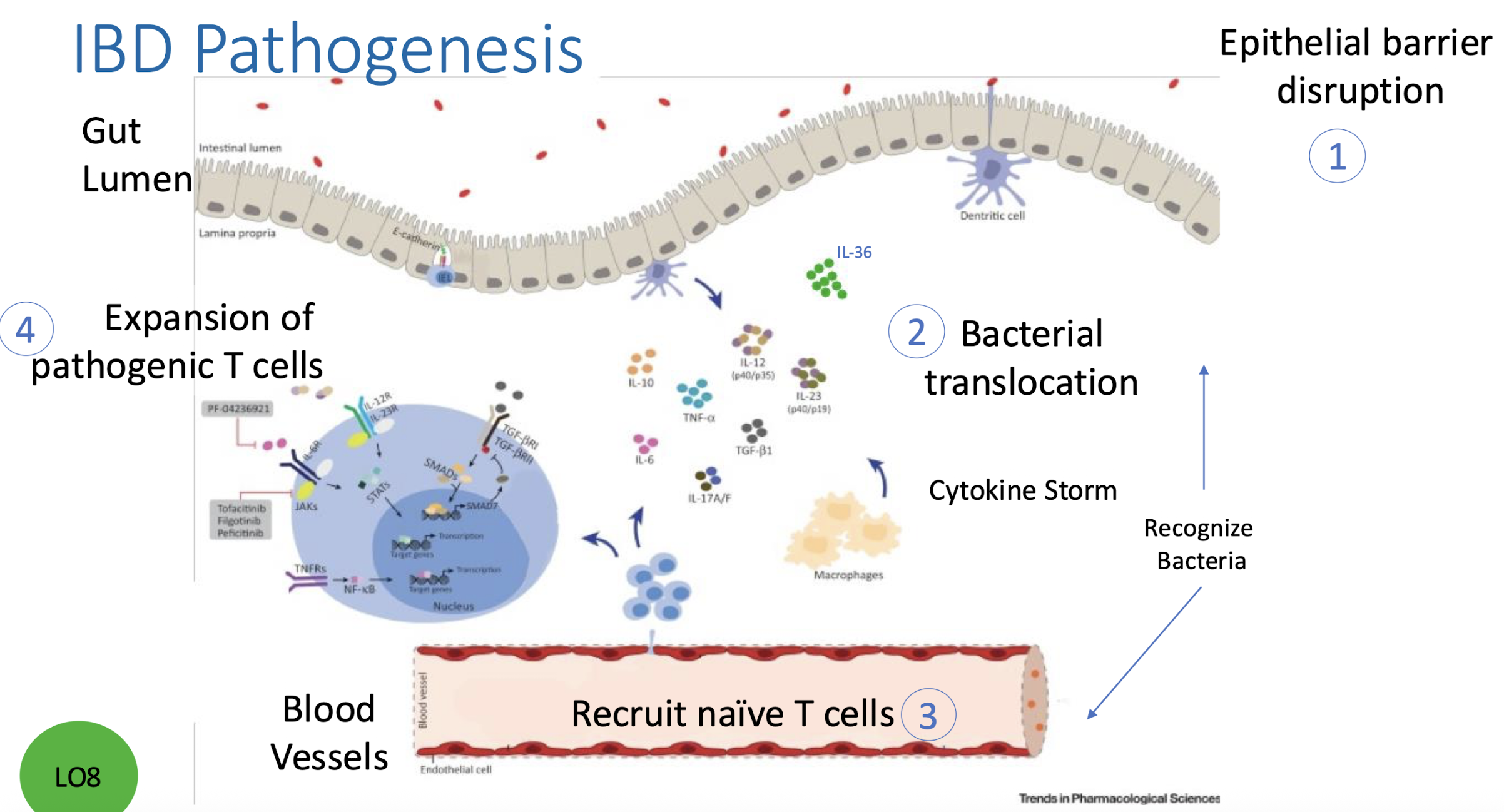
What are the four steps of IBD pathogenesis?
Epithelial barrier disruption
Bacterial translocation + recognition
Naïve T-cell recruitment in blood vessels
Cytokine storm by MP + expansion of pathogenic T cells
Therapeutic Targeting for IBD
1. Genetics: Bone marrow transplant effective in very early onset IBD
2. Microbiome: Use of Antibiotics /FMT
3. Immune System: Cytokine blockade/Leukocyte Trafficking/Cytokine Production
4. Environment: Dietary restriction
What are the 3 anti-TNF therapies + how do they differ?
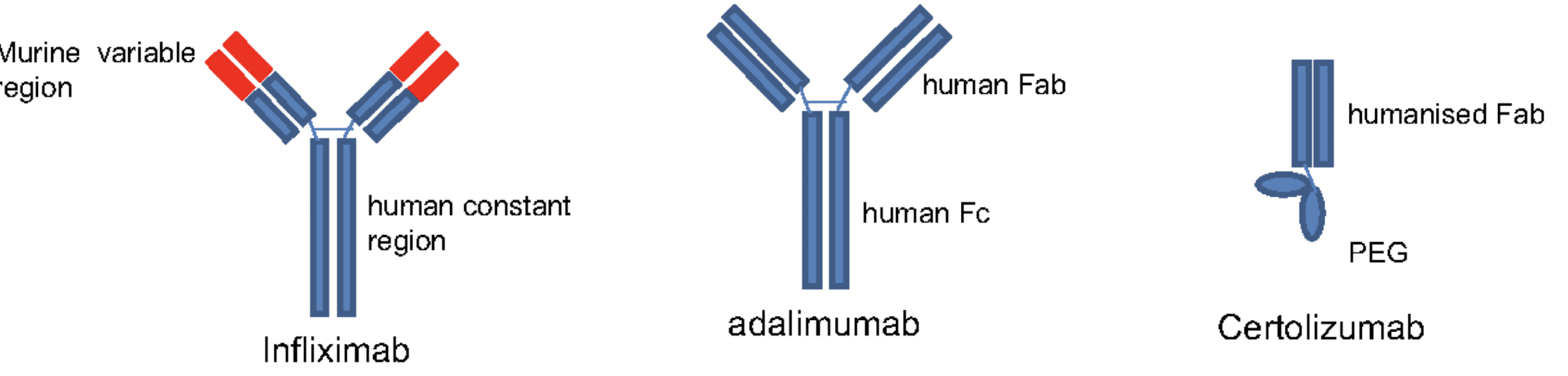
Drug | Type | Notes |
|---|
Remicade | Humanized antibody | IV infusion; 12-mo loss of efficacy |
Humira | Fully human | Injectable |
Cimzia | PEGylated Fab | No Fc region → lower clearance |
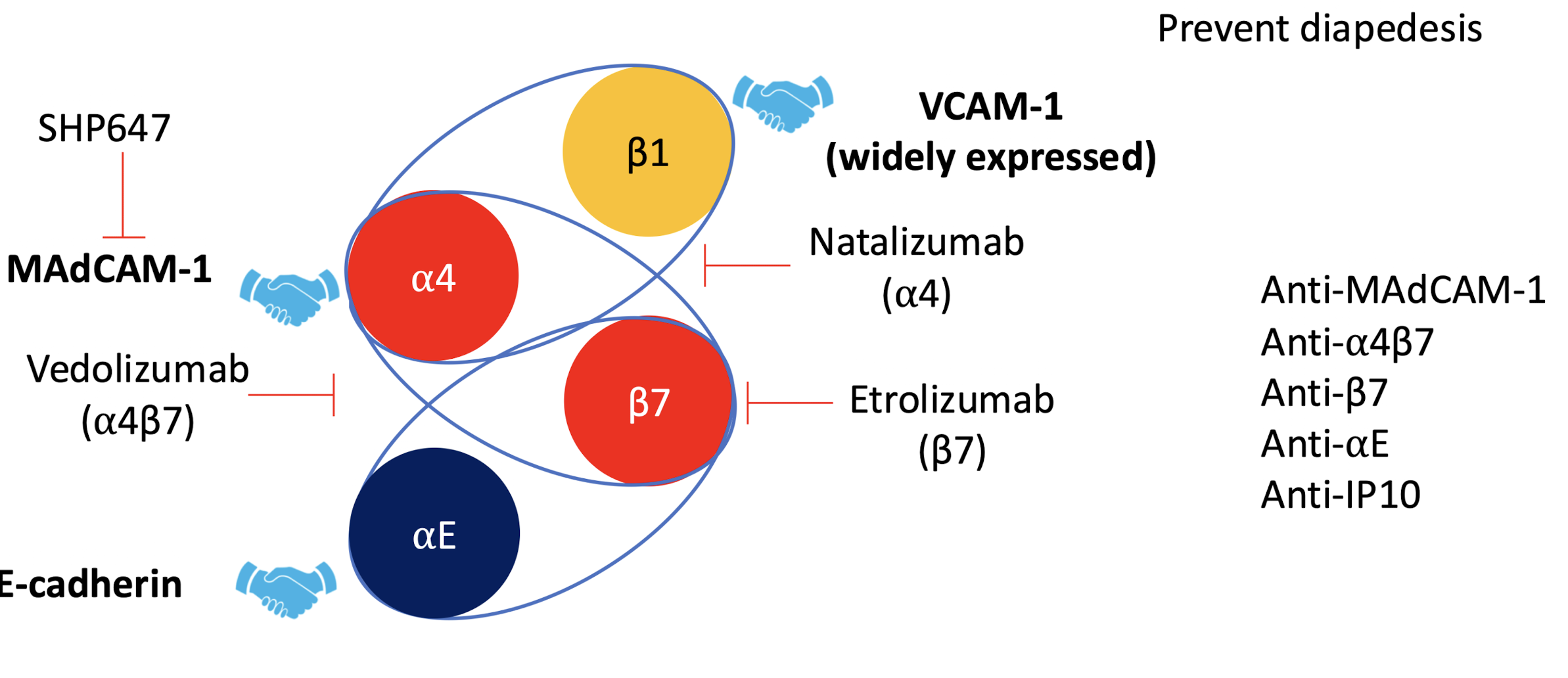
What integrin-based therapies block leukocyte recruitment?
Vedolizumab (α4β7)
Etrolizumab (β7)
Natalizumab (α4 )
Anti-MAdCAM-1
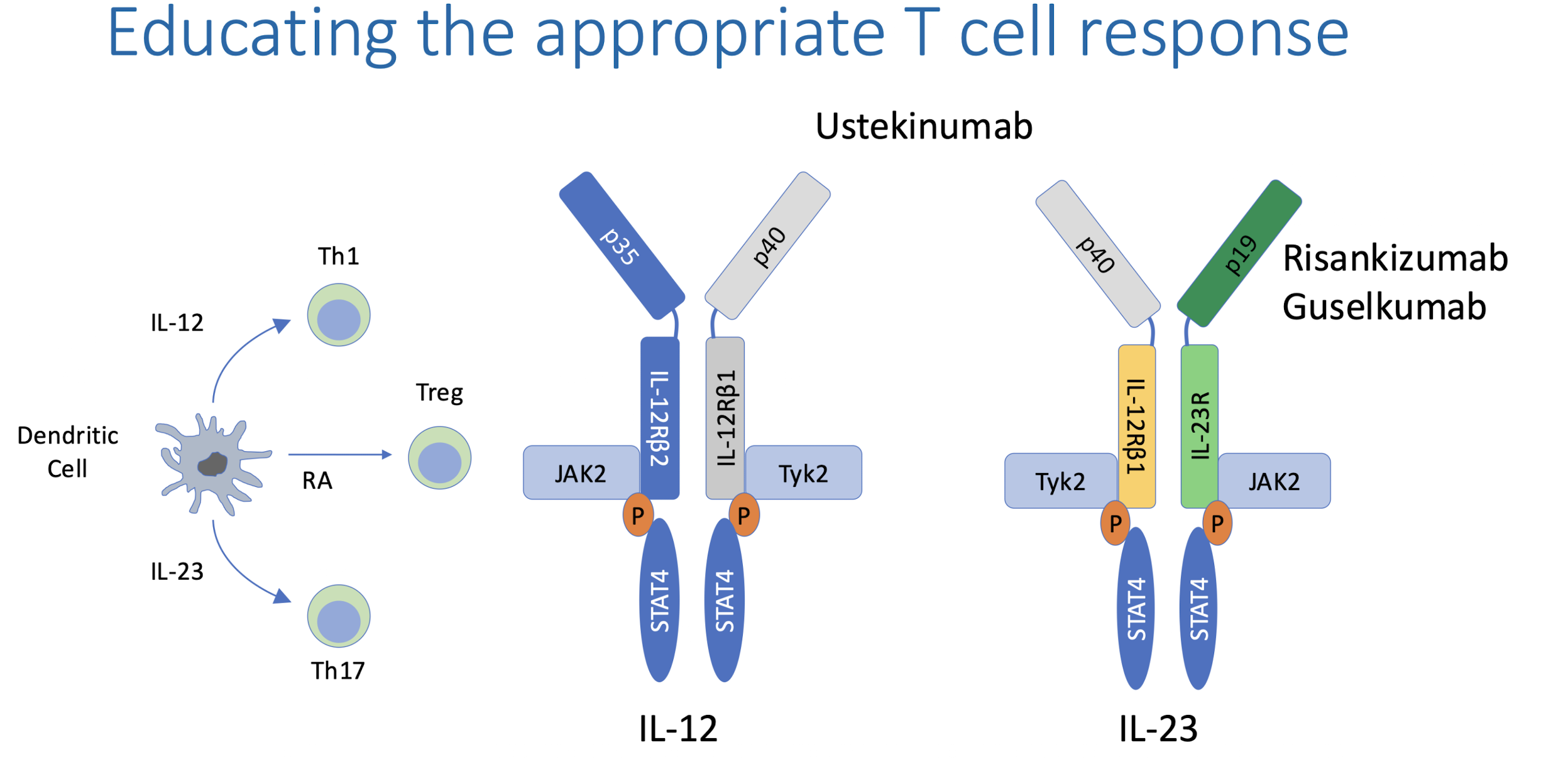
How does cytokine milieu determine T-cell fate?
IL-12 → Th1 (via STAT4)
IL-23 → Th17
Antibodies blocking these pathways include Ustekinumab (IL-12) , Risankizumab, Guselkumab (IL-23)