Energy Balance, Body Mass and Health
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
25 Terms
Energy
The ability to do work (W=Fd)
Form of energy
chemical (form stored in chemical bonds between atoms)
thermal (form which releases heat)
electromagnetic (form which travels in waves)
mechanical (form involved with movement)
electrical (form resulting from movement of charged particles)
Potential energy
form of stored energy
has the ‘potential’ to do work
Kinetic energy
form of energy in motion
kinetic = relating to motion
Units of energy
Kilojoules (kJ)
Kilocalories (Kcal)
Note:
Calories (Cal) x 4.186 = kilojoules (kJ)
Kilojoules (kJ) / 4.186 = Calories (Cal)
Metabolic processes in the body that require energy
Muscle contraction
nerve impulse conduction
Active transport
Digestion
Biosynthesis
Storage of nutrients
Maintenance of body temperature
Metabolic rate
the rate of energy output by the body
Resting metabolic rate (RMR)
Energy cost at rest (energy body needs to perform only essential activities)
Basal Metabolic Rate (BMR)
standardized measure of metabolic rate during complete rest (more restrictive: individual is fasted (12hr), rested (8hr) and inactive but awake)
Total Metabolic Rate (TMR)
BMR/ RMR + energy from output from physical activity (taken over a 24 hour period)
gives us a guide to how much energy to consume to regulate a healthy weight
Determinants of Basal Metabolic Rate
weight
height
surface area (greater SA:vol means more heat loss)
age (younger = more growth + muscle mass)
gender (males = more muscle)
Muscle mass
hormones (thyroid, progesterone)
pregnancy + lactation
stress (increased cortisol = prolonged behavioural response not always immediate)
food-induced thermogenesis (increases rate)
health state
ambient temp
sleep (reduces by 10-15% when you sleep)
Mechanisms to spot the patterns between physical activity levels and total metabolic rate and energy need of the body
PAL trends: numbers how that the person who is less physically active requires less energy
how to measure metabolism
direct calorimetry (calorimetric chamber)
indirect calorimetry (measures oxygen use/ gas exchange)
“foodworks”
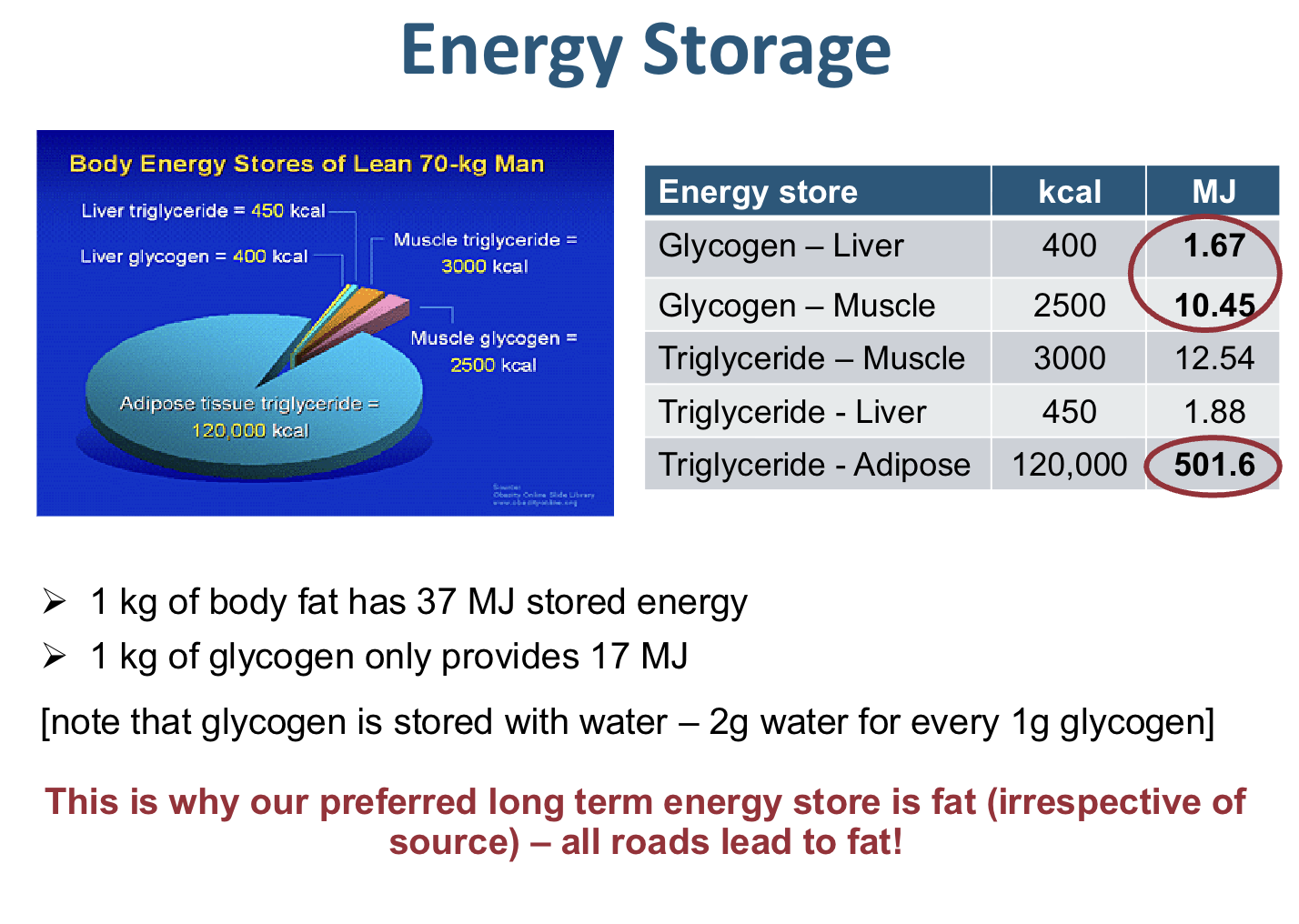
Energy storage
Visceral fat
fat stored between organs that have the most substantial impact on the development on non-communicable diseases
Energy balance
Control of food intake:
➢ Complex homeostatic mechanism with many players
➢ Key role for hypothalamus for controlling feeding behaviour (i.e., the ability to recognise satiety vs. hunger)
➢ Neural signals from digestive tract
➢ Blood borne signals related to body energy stores (e.g., blood glucose)
➢ Other peripheral signals inside the body such as hormones (e.g., insulin, glucagon, leptin and ghrelin)
➢ Body temperature (heat suppresses appetite)
➢ Psychological factors (e.g., stress)
➢ Environmental cues
➢ Health
➢ Ageing
Key objective: to maintain adequate energy stores in the body to
ensure survival
Causes of obesity
genetics
diet composition (increased food intake)
decreased energy expenditure (sedentary lifestyle)
stress/ mental health (eating behaviors)
hormonal effects
psychological factors
metabolic rate
environmental cues (culture and body image)
smoking (cravings often substituted with food)
genetics (the choices that people make can imprint on their future offspring)
Obesity related health issues
Type II diabetes Mellitus
Dyslipidemia
CHD
Cancer
Osteoarthritis
Sleep Apnoea
Physiological factors
joint/ mobility issues
Gall bladder disease
stroke
hypertension
pros and Cons of BMI
Pros:
does not require a skilled healthcare professional
Cons:
does not consider someone’s body composition (they migt have high skeletal muscle but are denoated as obese)
Measurement of BMI
Body composition measured by:
dual energy X-ray absoptiometry (DEXA)
BodPod (air displacement Plethsmograph)
Skinfolds
Bioelectrical Impedance Analysis (BIA)
Metabolic Syndrome
(An increased risk of diseases)
There is a clustering of metabolic abnormalities that increase the risk of a person developing these diseases:
insulin resistance
abdominal obesity
dyslipidemia
hypertension
If we know somebody is at elevated risk of these diseases, we can. prevent/ intervene. Lifestyle modification is important in reversing the pathway of the disease progression
Adipogensis
Surplus energy converted into triglycerides + stored as adipose cells
Energy stores are important during periods of increased demands:
prior to pregnancy
prior to birth
prior to weaning
Influenced by:
neurohormonal factors
genetics
environment
Individual differences
Hormonal Differences:
― Peripheral Adipose: Leptin; Adiponectin; Resistin
― GI Tract: Ghrelin; CCK
― Pancreatic: Insulin
― Central Hypothalamus
➢ Lack of adiposity feedback signal / receptor (in mice)
➢ Leptin → ‘The Lipostat’
Diets
Types: are you trying to reduce overall energy or only certain food groups (and their specific nutrients)
Yo-Yo dieting not effective because they are very restrictive (because it is so far removed from your regular lifestyle that after your motivation wears off, you slip back into old habits). can change body composition (lose weight as lean muscle mass)
Low kilojoule diet cf. low fat / low CHO diet
➢ May not be sustained long-term → Yo-Yo Dieting
➢ ↑ risk of Eating Disorders
➢ ↑ risk of Obesity long-term
➢ Nutritionally deficient in Vitamins & Minerals
➢ High Protein diets → ↑ workload on liver & kidneys
➢ Preoccupation with Weight & not Health
Relationship between fitness, obsesity and risk of non-communicable disease
Normal weight, overweight and obese but still fit all have similar risk to non-communicable disease