Lecture 1-4
1/61
Earn XP
Description and Tags
ANSC 320
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
62 Terms
Parturition
expulsion of the fetus and placenta from the uterus (“labor”).
What are the three stages of parturition?
Myometrial Contractions and Cervical Dilation
Expulsion of the Fetus
Expulsion of the Placenta
Write the steps are parturition from longest time to shortest time
Longest: Myometrial Contractions and Cervical Dilation
Expulsion of placenta
Shortest: Expulsion of Fetus
Why does the expulsion of the fetus need to take the shortest amount of time?
fetal hypoxia
Myometrial Contractions
Only occurs after removal of progesterone block
Stimulated by PGF2a, Oxytocin, and E2
High E2 to P4 ration promotes contractions
Ferguson Reflex
Ferguson Reflex
pressure on cervix by fetus stimulates release of oxytocin which will bind to its receptors to simulate myometrial contractions.
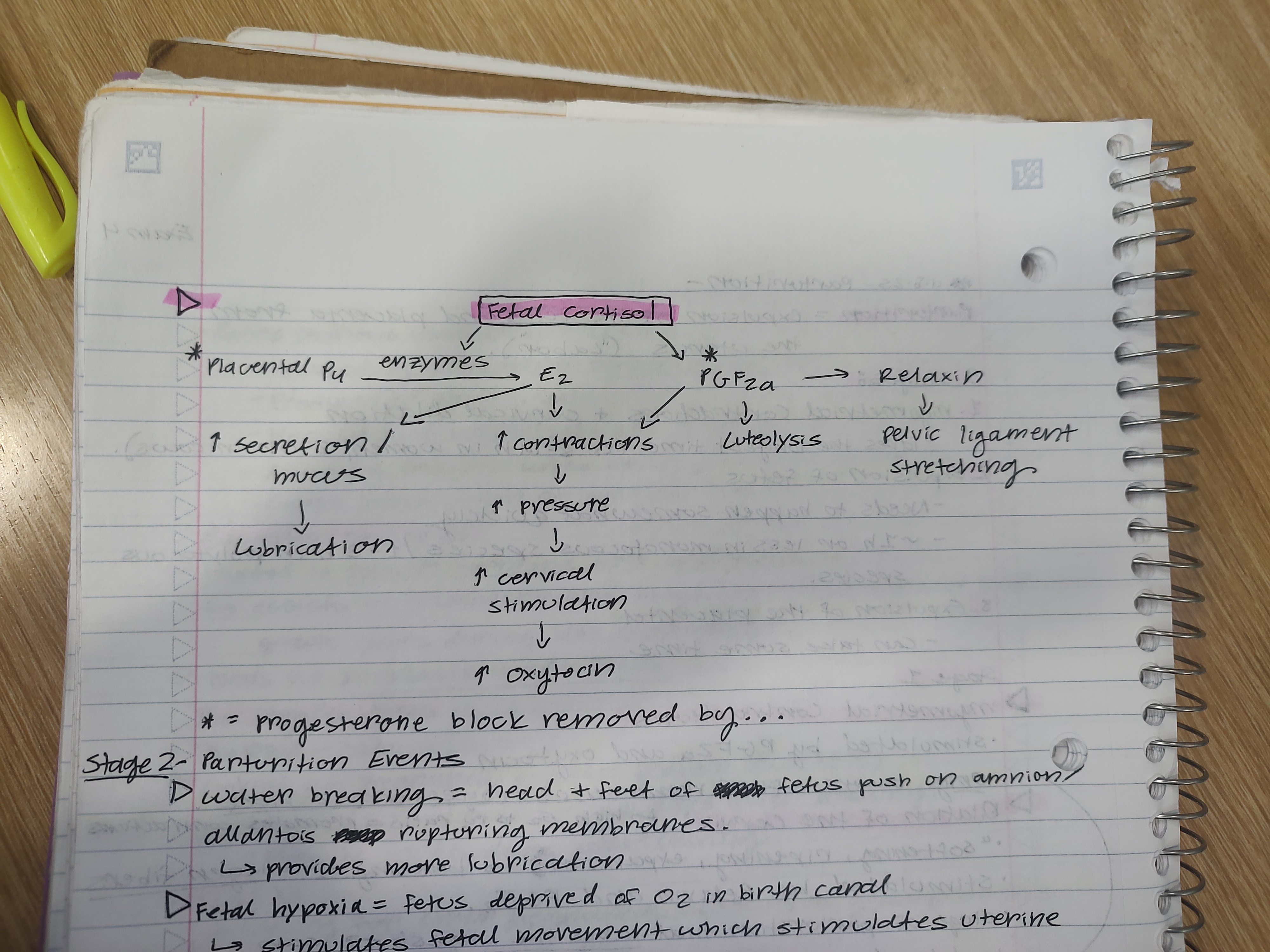
Draw a diagram explaining Fetal Hypothalamo-Pituitary-Adrenal Axis
Hypothalamus
CRH
Anterior Pituitary
ACTH
Adrenal Gland
Fetal Cortisol
Draw a diagram explaining how fetal coritsol induced parturition
Water Breaking
head and feet of fetus push on amnion/allantois, rupturing the membranes
Provides more lubrication
Fetal Hypoxia
when fetus is deprived of O2 in birth canal
stimulates fetal movement which stimulates uterine contractions
How is the placenta released?
chorionic villi are released by vasoconstriction of villi arteries
How is hemorrhaging reduced?
maternal vasoconstriction
Dystocia
difficult birth
Why might dystocia occur?
large fetus
failure of cervical dilation
abnormal presentation of the fetus
Multiple births
What are some “solutions” to dystocia?
Caesarion Section
Symphysiotomy
What are the three ultimate goals of pregnancy hormones?
Growth of endometrial epithelium - histotrophs
Proliferation of myometrium
Development of mammary glands for lactatation
What hormones is required for early embryonic development?
Progesterone
What does progesterone do in pregnancy?
Established uterine quiescence
Inhibits estrogen and oxytocin receptor formation
What are the two sources of Progesterone during pregnancy?
Corpus Luteum - early source of P4
Placenta - in some species, it takes over as primary source for P4
What hormone rises rapidly at the end of pregnancy (gets things “ramped up”)?
Estrogens
What does estrogen do in pregnancy?
Stimulates estrogen and oxytocin receptor formation
Participate in uterine tract motility
Cervical Mucus
Stimulates endometrial, myometrial, and mammary growth
Does estrogen rise rapidly at the end of pregnancy in women?
No it rises throughout the entire gestation period
Human Chorionic Gonadotropin (hCG)
pregnancy-specific hormone
has strong LH activity (binds to LH receptors)
prevents luteal regression
what human pregnancy tests look for
Equine Chorionic Gonadotropin (eCG)
pregnancy-specific hormones
produced by chorion in endometrial cups
produced at attachment
Has LH and some FSH-like activity
Accessory Corpora Lutea → produced P4
Causes luteinization of ovarian follicles
Placental Lactogen
related to growth hormones and prolactin
assists in mammary and fetal growth
Binds to binucleate giant cells
BioPRYN-Lab
cow pregnancy test that looks for Pregnancy Specific Protein B (PSPB).
IDEXX
cow pregnancy test that looks for other pregnancy-associated glycoproteins
Relaxin
relaxes pelvis and cervix
produced by either placenta or corpus luteum (depends of the species)
What are four factors that can influence fetal growth?
Thyroid Hormones
Insulin
Growth Hormone
Alpha-Fetoprotein
Alpha-Fetoprotein
protects female brain from defeminization
When does majority of fetal growth take place?
the last trimester
Thyroid Hormones
skeletal and muscle development
Insulin
increased energy substrate and placental growth
Growth hormone
stimulated fetal growth
What is the main goal of MRP?
to prevent corpus luteum destruction
When does maternal recognition in farm animal occur?
Before strong attachment of the conceptus.
How does MRP work in cows and sheep?
Signal: IFN-t from conceptus
Target: Uterine endometrium
Mechanism: inhibits estrogen and oxytocin receptor formation
Timing: ~ day 12 (sheep); ~ day13-21 (cows)
How does MRP work in horses?
Signal: Unknown; conceptus patrols uterus multiple times a day to trigger MRP
Target: Uterine Endometrium
Mechanism: Diminishes PGF2a production
Timing: ~ day 14-16
How does MRP work in sows?
Signal: Estrogen
Target: Uterine Endometrium
Mechanism: alters direction of PGF2a from uterine vein to uterine lumen where it is destroyed
Timing: ~ day 8-12
How does MRP work in women?
Signal: Human Chronic Gonadotropin (hCG)
Target: Corpus Luteum
Mechanism: hCG binds to LH receptors and overrides PGF2a activity by stimulating P4 production.
Timing: ~ day 7-8
What are the three germ layers that form and what is their function?
Ectoderm - mammary glands
Mesoderm - repro system
Endoderm - primordial germ cells
What are the four Placental Membranes?
Chorion
Yolk Sac
Amnion
Allantois
Yolk Sac
degenerates earlier in mammals
source of blood cells
source of primordial germ cells
Amnion
Non-vascular; fluid-filled (fluid is produced by the fetus)
Protects the fetus by providing a cushion
Allantois
Fluid-filled sac that collects waste from the embryo
Contains blood vessels connecting fetal and placental circulation
Eventually fuses with the chorion to form the allantochorion
Chorion
Outermost layer
Provides attachment to the uterus
Draw a diagram of the 4 layers of the placental membranes
yee
What is the purpose of the umbilical cord?
infiltrates the chorion to form the vascular link between mother and fetus
What is the “free-living” period?
time before the placental membranes form
loose attachment between mother and fetus
What is the placenta?
endocrine organ of highly vascular contact between mother and conceptus
What are the two types of Placentation?
Invasive (Implantation)
Non-Invasive (Attachment)
What is the invasive (implantation) placentation?
embryo invades endometrium and develops in the endometrium
“Interstitial”
ex. humans
What is the non-invasive (attachment) placentation?
chorion and endometrium make physical contact via interlocking microvilli
“Superficial”
ex. Farm Animals
What are the four types of placenta?
Diffuse
Zonary
Cotyledonary
Discoid
Diffuse Placenta
Least invasive attachment
Chronic villi are distributed over the entire surface of the endometrium
ex. Pigs, Horse
Zonary Placenta
primary region of exchange is a band near the middle of the conceptus
ex. dog, cat
Cotyledonary
Non-invasive; chronic villi restricted to cotyledons
Cotyledons and caruncles attach, creating a placentome
Cotyledon
specialized areas on fetal placental membrane
Caruncles
maternal specialized regions on uterus to which cotyledons attach
Discoid
Primary region of exchange is a central disc
Endometrial epithelium grows over placenta
Bidiscoid = 2 central discs
ex. primates, rodents
Epitheliochorial
when 6 layers are separating fetal and maternal blood (less invasive)
Hemochorial
when 3 layers are separating fetal and maternal blood (more invasive)