Physiology Lab Exam 1
1/244
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
245 Terms
Outer wall of eye formed of _ distinct layers
Three (Fibrous tunic, Vascular tunic, Sensory Tunic)
Outermost layer of the eye
Fibrous tunic
Fibrous connective tissue, poorly vascularised. Has 2 regions: the sclera and the cornea
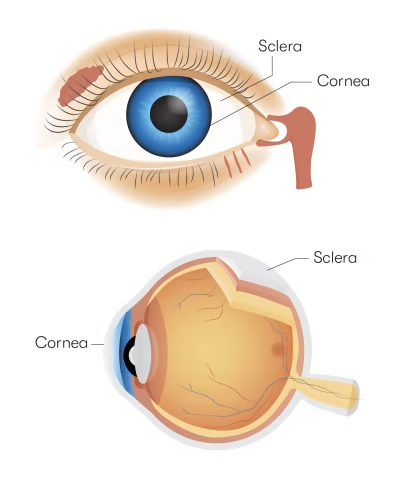
Sclera
The ‘white of the eye’ = the posterior 5/6 of the fibrous tunic. ~0.5mm thick.
Densely packed collagen fibers with few elastic fibers
Maintains shape of the eyeball and protects from injury
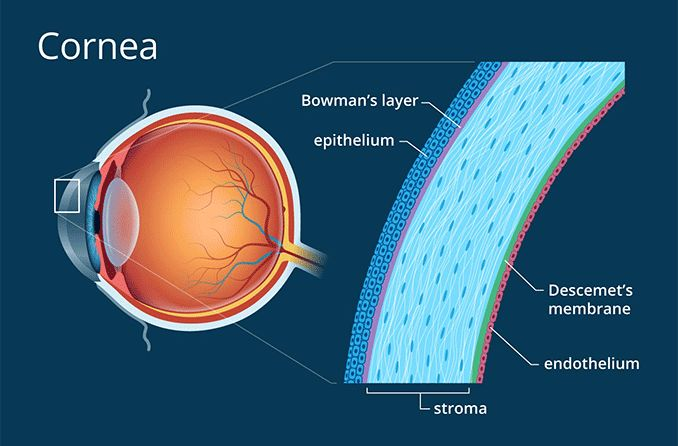
Cornea
Anterior 1/6 of the fibrous tunic
Transparent, ~0.8mm thick
Small collagen fibers, few elastic fibers and many proteoglycans
Inner surface = simple squamous epithelium, outer surface = stratified squamous
Protects internal structures, contributes to refractive power
Middle layer of eyeball
Vascular tunic (aka uvea)
3 regions: choroid, ciliary body and iris
Choroid
Vascular tunic layer
Thin membrane, posterior 5/6 of eye, incomplete where optic nerve exits
loose connective tissue, blood vessels and melanocytes.
Supply nutrients and oxygen to outer retina
Ciliary body
Vascular tunic layer
Continuous w choroid, anterior, encircles periphery of lens
Ciliary processes that secrete aqueous humor into anterior segments
Ciliary muscles that control shape of lens (smooth muscles)
Suspensory ligaments extend from ciliary processes to lens, maintain in upright position
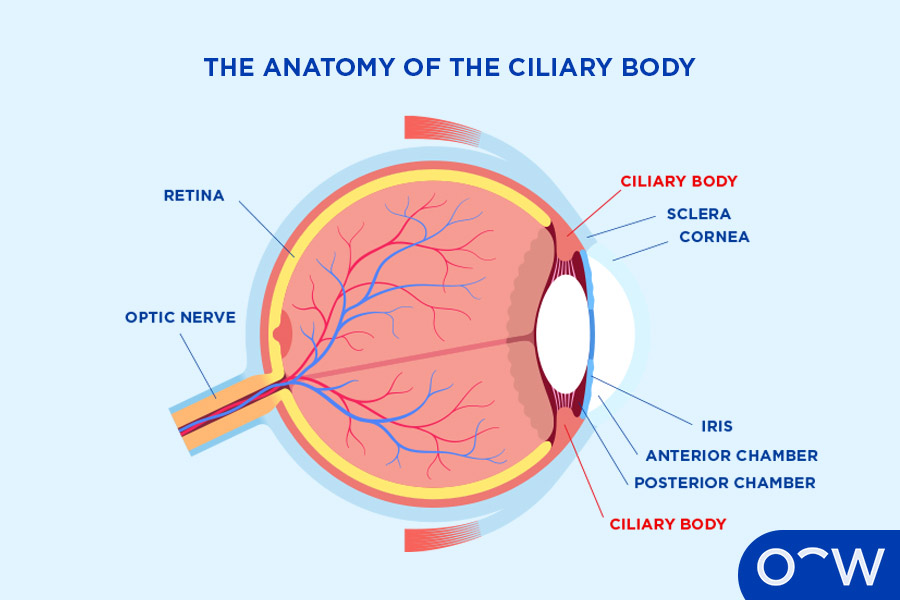
Iris
Vascular tunic layer
Pigmented sheath hangs from ciliary body, encircling most of lens.
Loose connective tissue, smooth muscles fibers, melanocytes
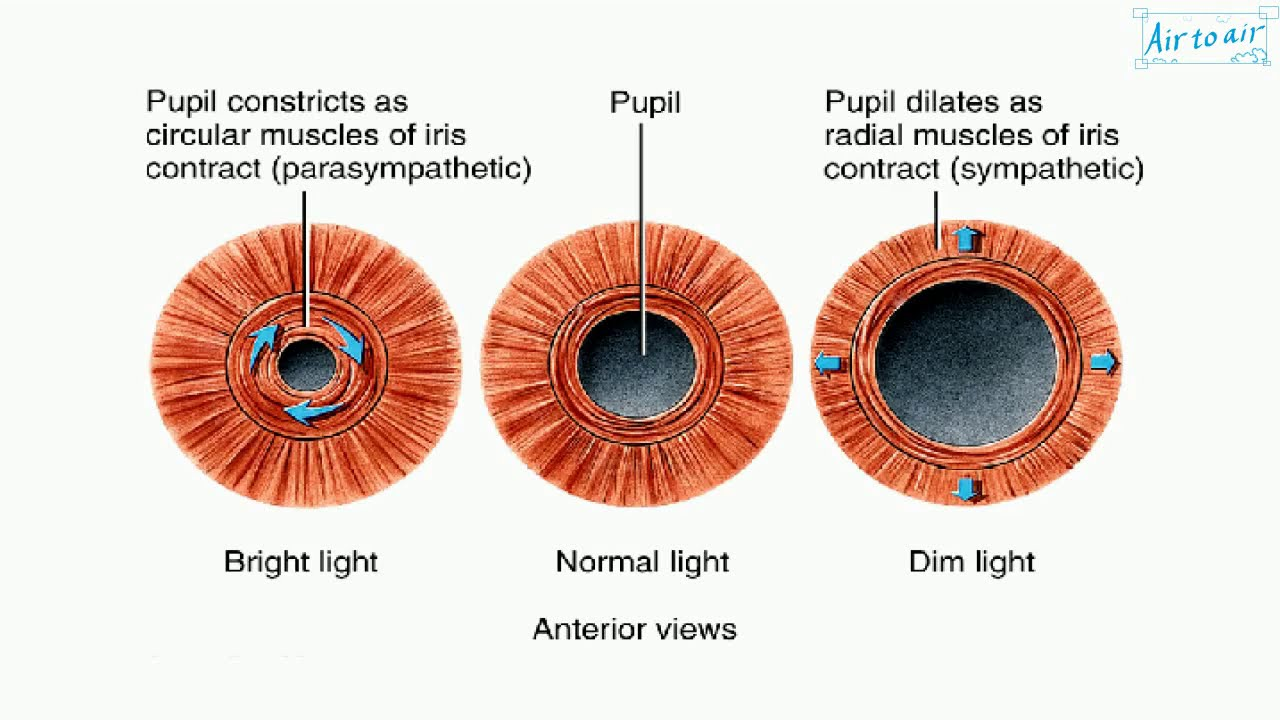
Central opening = pupil
Muscle allows to vary in size
Sphincter pupillae muscles constrict the pupil
Dilator pupillae muscles increase size of pupil
Innermost layer of eyeball
Sensory Tunic or Retina
Two layers (not fused and can come apart)
Condition where two layers of retina come apart
Detached retina
Pigmented layer
One layer of cuboidal epithelium in the retina
Contains melanin
Adjacent to choroid, extends anteriorly to cover ciliary body and posterior iris
Neural layer
In retina layer
Anterior to pigmented layer, extends to margin of ciliary body (area called the ora serrata)
Composed of 3 layers of neurons:
Photoreceptors
Bipolar cells
Ganglion cells
Photoreceptors
Deepest in the neural layer, adjacent to the pigmented layer.
Convert light into electrical impulses, pass to bipolar cells
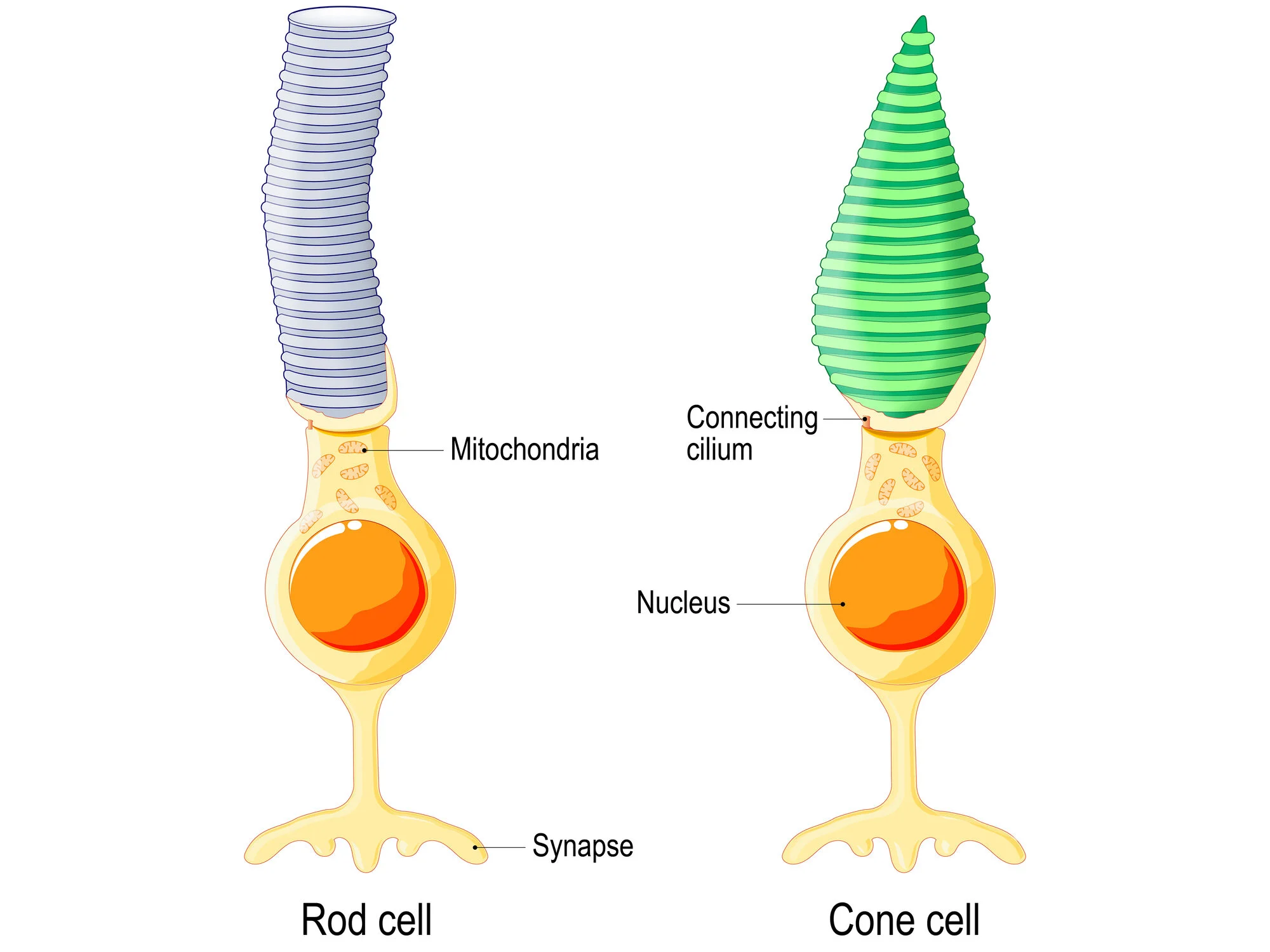
2 types = rods and cones
Bipolar cells
Receive electrical impulse from photoreceptors and pass to ganglion cells
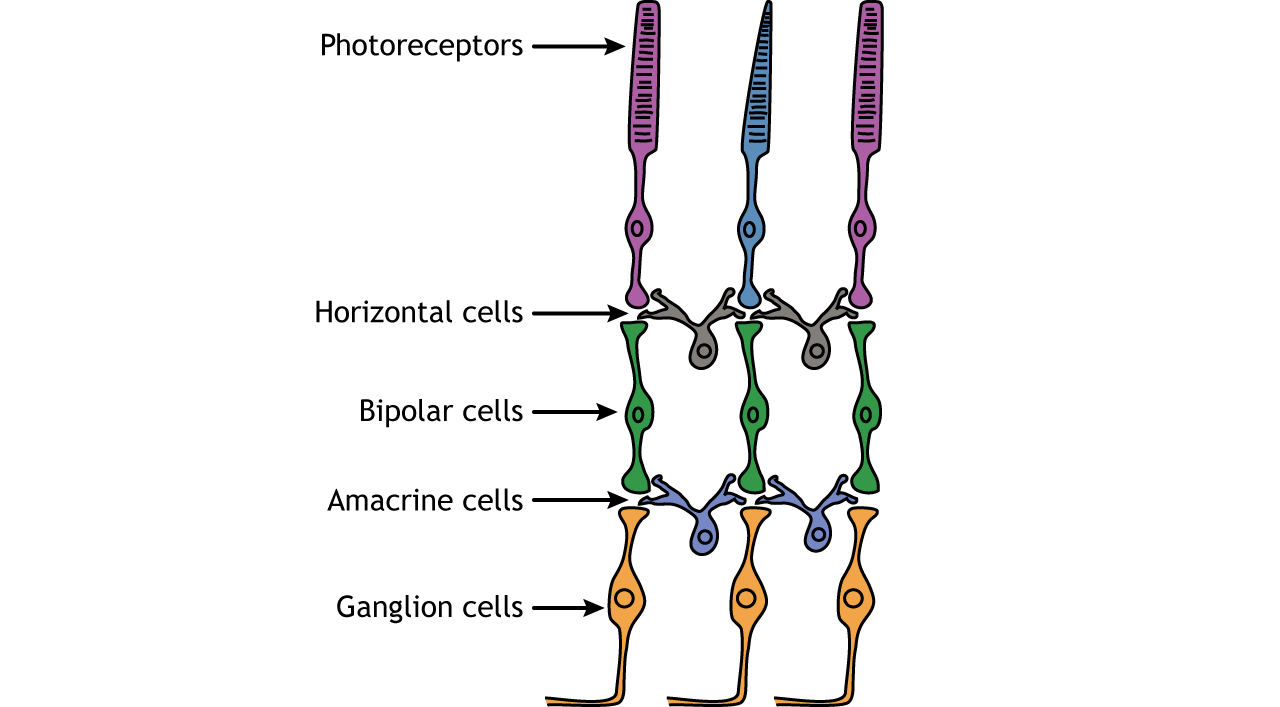
Ganglion cells
Most anterior of neural retina.
Long axons, make 90º turn at inner face of retina
All axons ultimately merge at posterior eye to from optic nerve to brain
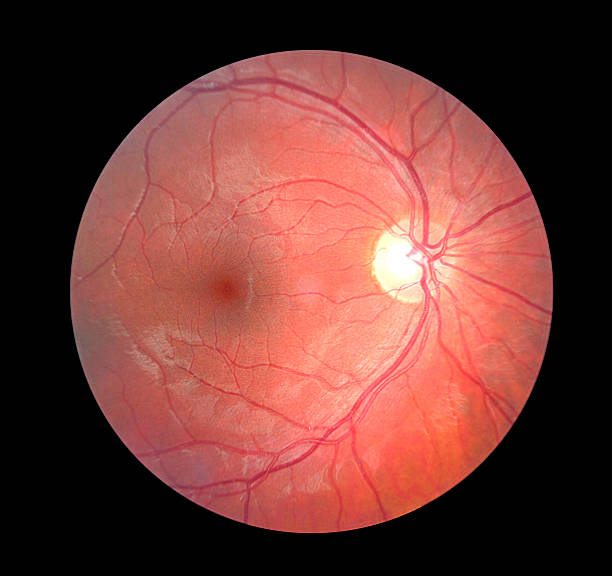
Device used to observe the fundus (posterior inner eye wall)
Opthalmoscope
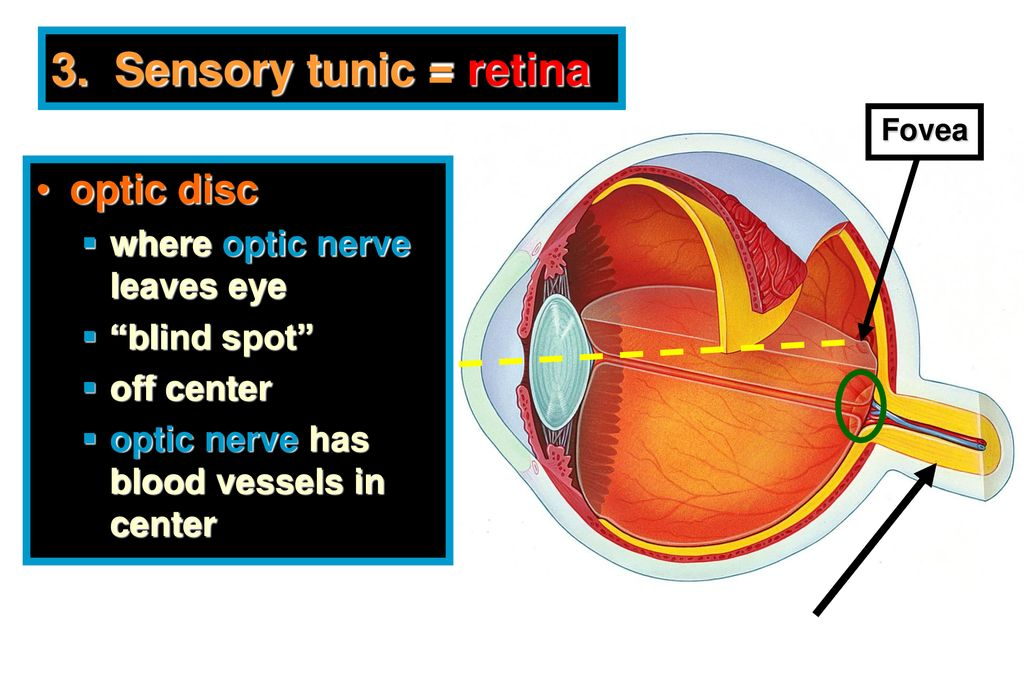
Optic disc
Where optic nerve exits eye (blind spot)
Appears as round yellow region in opthalmoscope
Macula lutea
Round reddish region in opthalmoscope
Contains fovea centralis
Eye examination
Subject sits and looks at distant object over examiner’s shoulder. Observe right eye with your right eye and vice versa. Opthalmoscope turned on and held at arms lenght, directed so light is shining into subjects pupil and observe.
Yellow is optic disc, red is macula lutea, pink is everywhere else. Arteries brighter red than veins
Why do we not see our own optic veins/arteries?
Our brain suppresses the images in normal line of vision
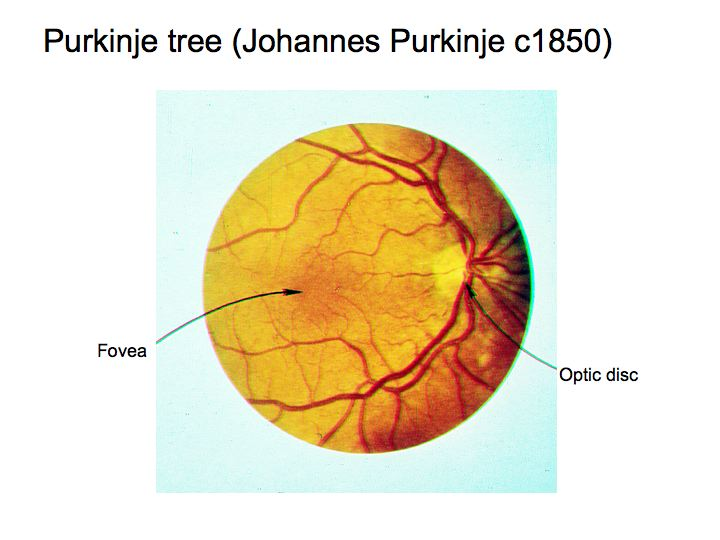
Purkinje Tree exams
Close eyes, hold light next to eyelid at 45º angle and move it from side to side. The branching image is the Purkinje tree
The 6 extrinsic eye muscles originate on the ___ _____ and insert on the ______
bony orbit
sclera
Retinal disparity
Difference in images perceived by either retina. Helps in 3-dimensional vision.
What maintains eyes in midline position
Antagonistic ocular muscles
Nystagmus
When tone of one eye muscle is weak: Eye slowly drifts in one direction then quickly corrects itself. Controlled by vestibulo-ocular reflex
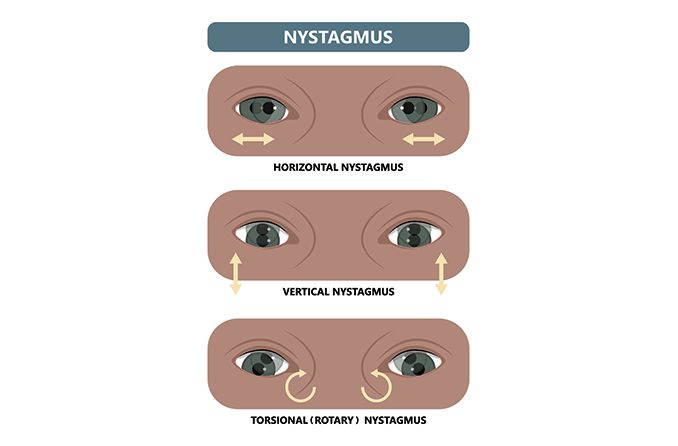
Nystagmus test
Hold pencil 1 meter from bridge of subject nose. Move 30cm to each side then up/down. Hold in each position ~5 sec. Observe movements noting presence/absence of nystagmus (oscillations of eye, slow one way, fast in opposite)
Myopia
Nearsightedness
When distant object brought to focus in front of retina
Usually due to elongated eyeball
Corrected with concave lens
Hyperopia
Farsightedness
Image brought to focus behind retina
Usually due to shortened eyeball
Convex lens used
Emmetropia
Normal vision acuity
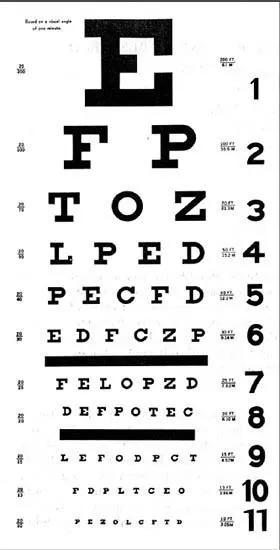
Snellen eye chart
Visual acuity test chart. stand 20 feet from eye chart, cover one eye and attempt to read each line
Person with normal vision can read 20/20 line at 20 feet.
Person with 20/40 visual acuity must stand 20 feet away from a line that a normal person can read at 40 feet
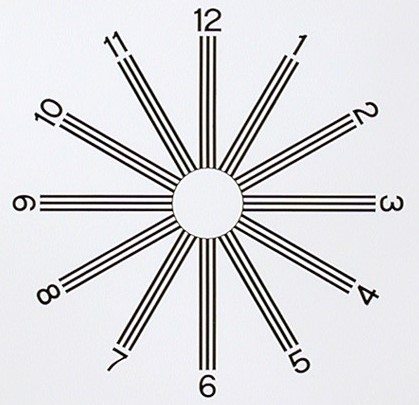
Astigmatism
Visual defect due to abnormal curvature of cornea or lens.
Refraction of light in horizontal plane is different than in vertical plane.
Astigmatism test chart - stand 3 to 4 feet from astigmatism, cover one eye, stare at center
Retinal image 4 processes
1. Refraction of light rays.
2. Accommodation of the lens.
3. Modification of the pupillary diameter.
4. Convergence of the eyes.
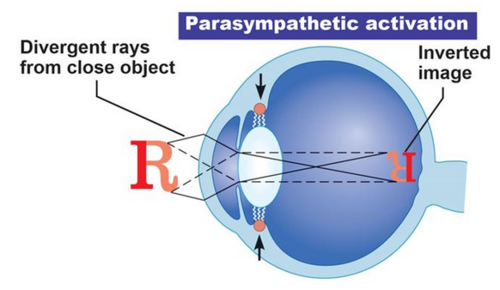
Refraction of light rays
Bending light rays.
Image light refracted by cornea, lens, and humors of eye to form inverted image on retina.
Strength of lens can be changed by making more or less convex. Higher degree convexity, greater strength of lens.
Strength of lens measured in ________
Diopters
Strength = 1/focal length (m)
Accommodation of the lens
Altering the degree of convexity of the lens to focus image
Greater curve = more light bends
When ciliary muscle relaxed, suspensory ligaments tighten and pull lens = convexity decreases (flatter). Distant objects focused (think like pulling a bow and arrow).
When ciliary muscles contract, suspensory ligament loosens = convexity increases (rounder), near objects (<20 ft) focused

Accommodation (eye)
Ability of the eye to focus on different distances from the lens
Which requires greater degree of convexity, near or far object?
Near object, has more obliquely directed rays
Presbyopia
Elasticity of lens decreases with age, loss of ability to accommodate (literally means “old vision” “Presbus = old man”)
Near point of vision test
Place meter stick under one eye, close opposite. Hold pencil at arm’s length slowly bring pencil toward eye. Record distance at which object out of focus. Repeat for other eye
Accommodation test
Focus on distant object.
Place pencil ~ 25cm in front of eyes
shift focus to pencil
close eyes for 30-60 sec
open and note whether pencil or distant is in focus (Should be the “big picture” in focus)
Depth of focus
Greatest distance an object can move and still remain in focus. Main factor is pupil size (small pupillary diameter = depth of focus is greater due to more accurately focused light at centre of pupil)
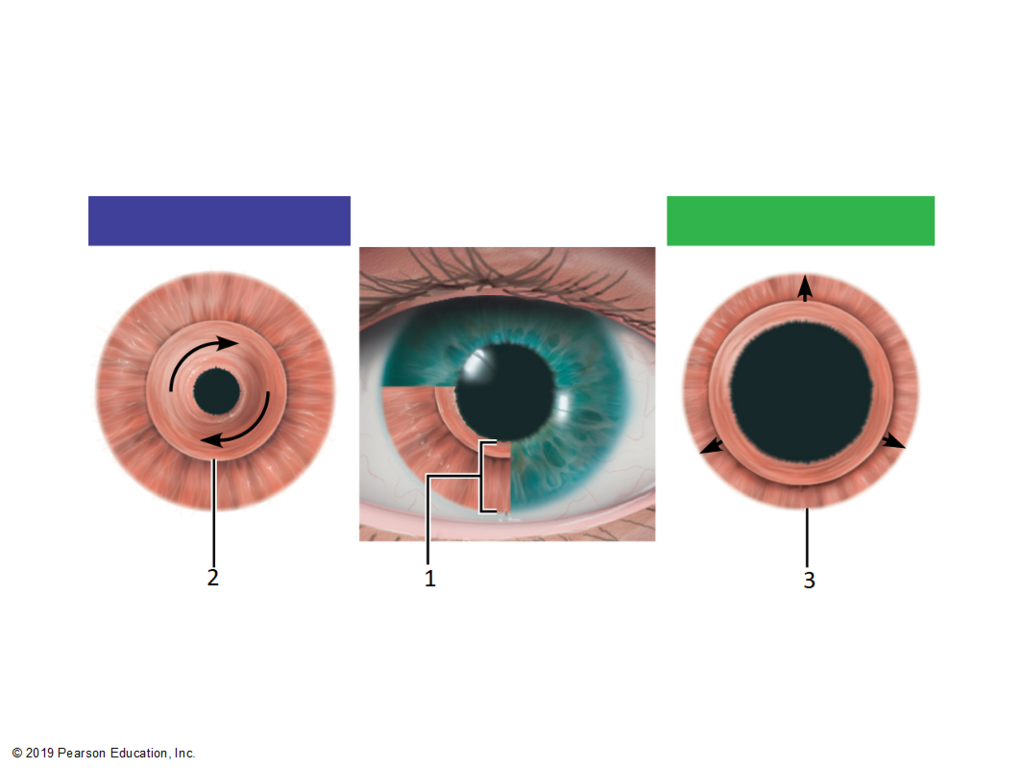
Sympathetic vs Parasympathetic pupillary movement?
Sympathetic NS controls the dilator pupillae (contraction for fight or flight)
Parasympathetic NS controls sphincter pupillae (dilation)
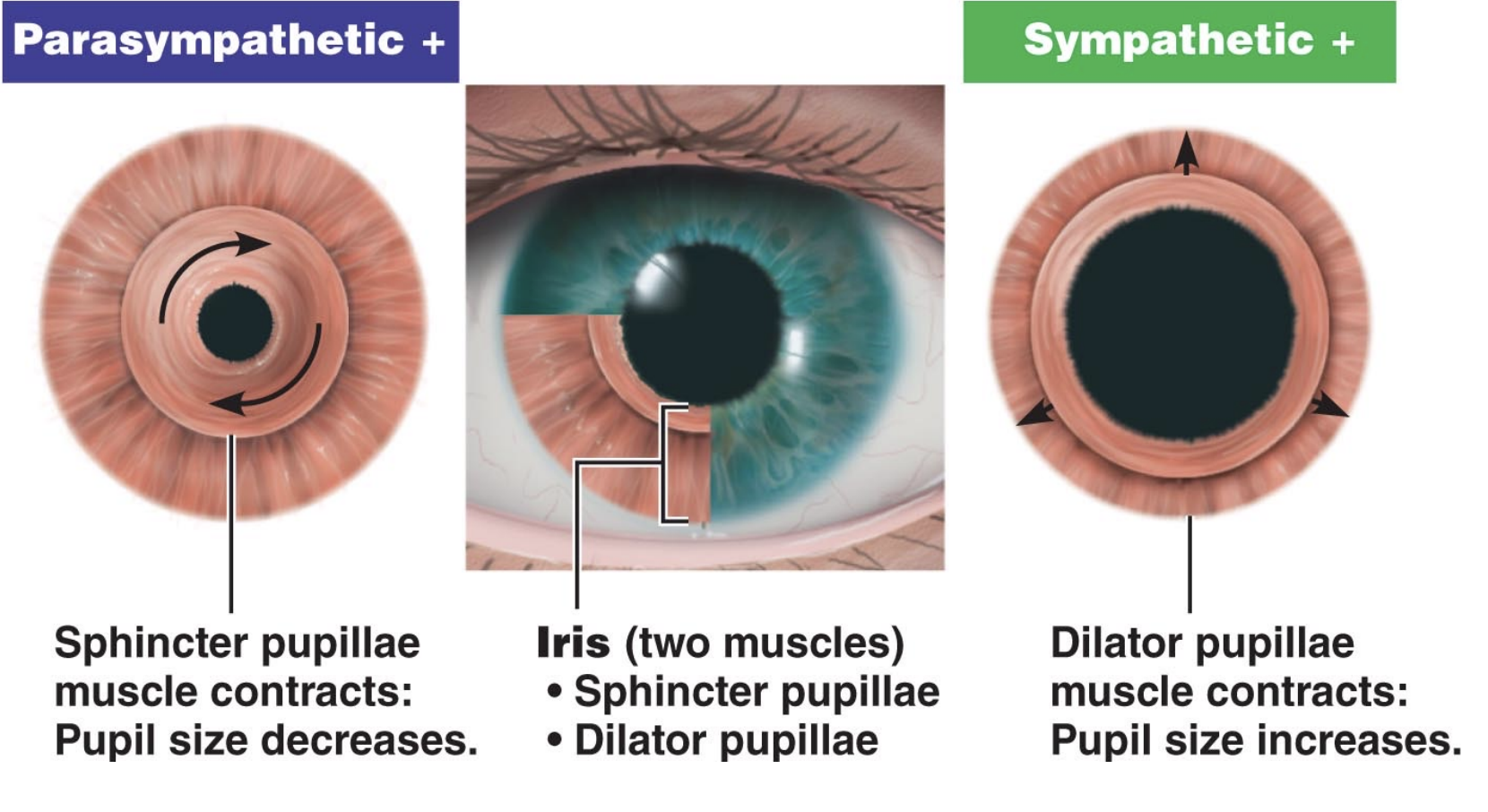
Pupillary reflex
In response to light, pupil constricts
Same eye = direct light reflex
Other eye = consensual light reflex
Pupillary diameter test
Focus on tip of pencil as slowly brought from 1m in front of you to bridge of nose. Note size of pupils (should constrict)
Do not perform facing window
Consensual Light reflex test
Shine narrow beam of light from right side of subjects eye into right eye. Note changes in both eyes (should constrict)
Do not perform facing window
Extrinsic vs Intrinsic eye muscles
Extrinsic muscles move the eye (originate outside the eye)
Intrinsic muscles control pupillary dilation (contained within the eye entirely)
Convergence
Movement of eyes medially to ensure light rays of near object hit same spot on the retina
Accomplished by actions of extrinsic eye muscles
Convergence test
Focus on tip of pencil as slowly brought from 1m in front of face to bridge of nose. Eyes converge/rotate medially
Approximately how many rods in each eye?
120 million
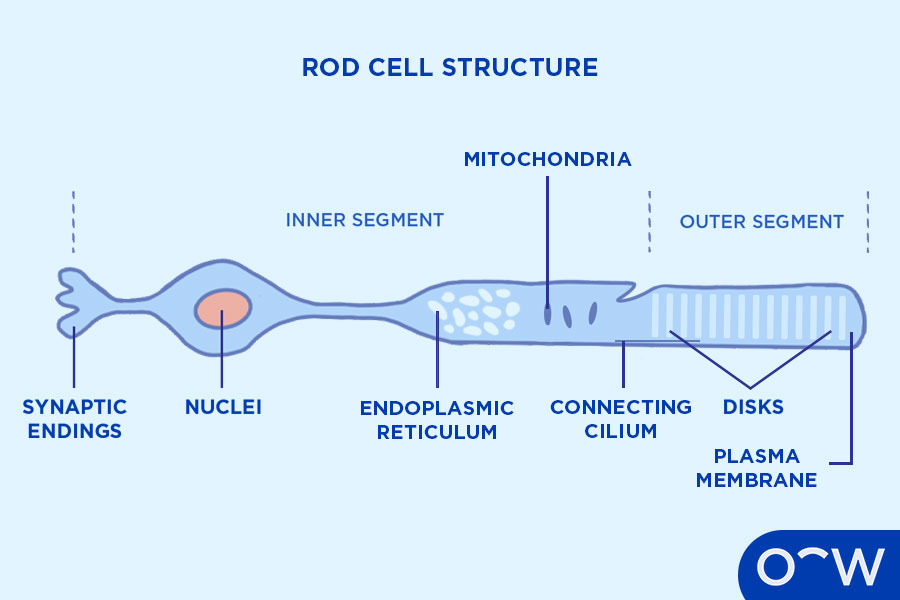
Rods are found everywhere on the retina except the _____ _________
fovea centralis
Rods three functions
Night (scotopic) vision - rods are much more sensitive to light than cones.
Black-and-white vision - pigment found in rods = only perceive black white and shades of grey
Peripheral vision - rods perceive images outside direct line of vision (outside fovea centralis)
Photochemical reaction when light hits rods
Bleaching:
rhodopsin pigment dissociates to form retinal pigment and opsin protein. Leads to hyperpolarisation, triggering chain of graded potentials. Inactive period follows.
Pigment found in rods
Rhodopsin
Breaks down into retinal and opsin
Vitamin required to restore retinal to rhodopsin in rods
Vitamin A
What causes inactive period after stimulation of rod cell?
Rhodopsin has to be reformed after “bleaching”
Positive afterimage of bright light + cause?
Bright image of light seen
Due to continued firing of rods
Negative afterimage of bright light + cause?
Dark image of bulb
Due to bleaching of visual pigment of rods
Afterimage test (for rods)
Stand 30cm from white light lamp
Stare at bulb for 30 sec
Turn light off and close eyes at same time
First image you see should be similar
second image should be different
How many cones in each retina?
7 million
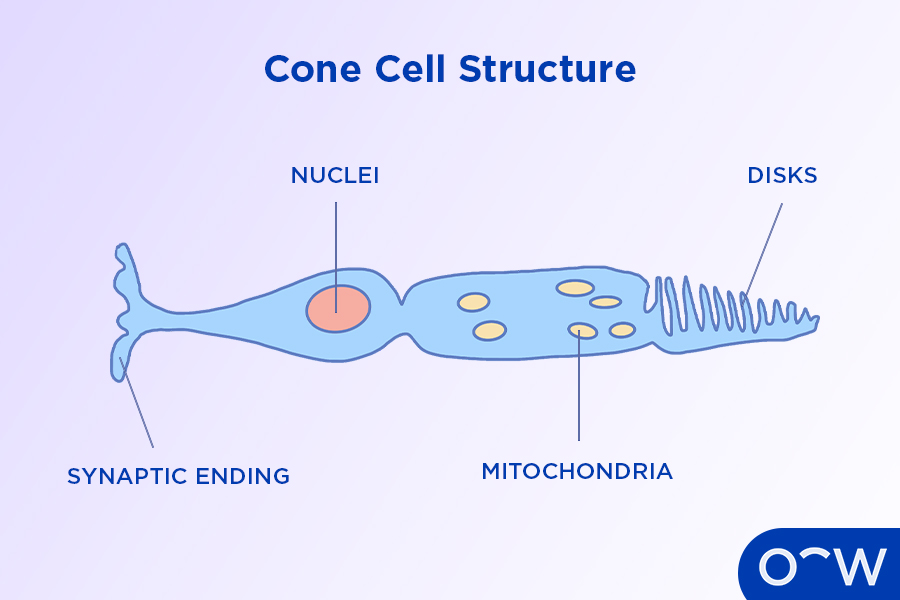
Where are cones found? and where are they MOST concentrated?
Found in the macula lutea highest conc. at the fovea centralis, decreases as you move away
How many cones found in the fovea centralis
~35 thousand within the 1.5mm diameter
Cones three functions?
Day (photopic) vision - cones require relatively bright light to function
Color vision - various pigments in cones perceive colour
Visual acuity
Why are images focused on fovea centralis the sharpest? (4 reasons)
This is where image focuses when eyes look directly at it
Many densely packed cones
Overlying layers of cells (bipolar/ganglion) are displaced to sides of fovea, allowing unimpeded light to cones
Generally, only one cone synapses with one bipolar cell in this region
Young-Helmholtz theory of color vision
3 systems of cones responding respectively to red, green, and blue light. All other colors seen by brain are interpretations of mixtures of impulses. Color discrimination impaired if one system of cones bleached by continued viewing of object of that color.
Afterimage test (for cones)
Stare at small red square for 1 minute on large sheet of black paper.
Suddenly shift gaze to sheet of white paper.
Positive afterimage is similar
Negative afterimage is different
May see negative afterimage first if fatigue sets in
Relative Positioning of Rods and Cones on Retina test
Subject sits approx 15 cm from black board at left side. Make white chalk X on board immediately in front of subject’s right eye.
Subject close left eye and stare at X with right eye throughout test
Slowly move white paper disc into field of vision from right side, around 2m away
Mark on board for each disc when first becomes visible to subject. Repeat w red green and blue
SHOULD have white further out (before the halfway point) and colours closer as rods are peripheral and cones are central
Trichromancy
No loss of color vision
Color blindness
Impaired color discrimination. Hereditary condition affecting 8% of males and 0.5% of females.
Deuteranomaly
Reduced ability to see green light (most common type, X-linked)
Protanomaly
reduced sensitivity to red light, X-linked
Tritanomaly
Reduced sensitivity to blue light (extremely rare, NOT X-LINKED) Difficult to distinguish blue+yellow, violet+red, blue+green
Monochromacy (Achromotopsia)
Complete loss of color vision, extremely rare, only sees white, greys, and blacks
Color blindess tests
Cambridge color test online
Liquid filling the internal (posterior) cavity of the eye?
Vitreous humor
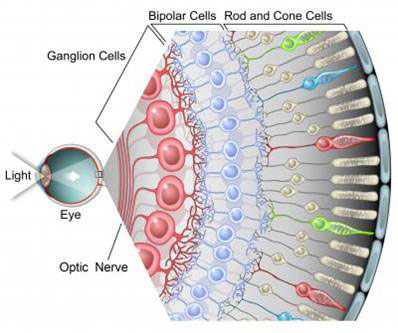
Passage of light in eye?
Through pupil
through lens and vitreous humour
pass through neural retina, past ganglion cells then bipolar cells
hits photoreceptor cells = bleaching
Passage of graded potential in neural retina
After bleaching occurs, photoreceptors pass graded potentials anteriorly to a bipolar cell then to a ganglion cell.
Action potential generated by ganglion cell, travels down axon to the brain
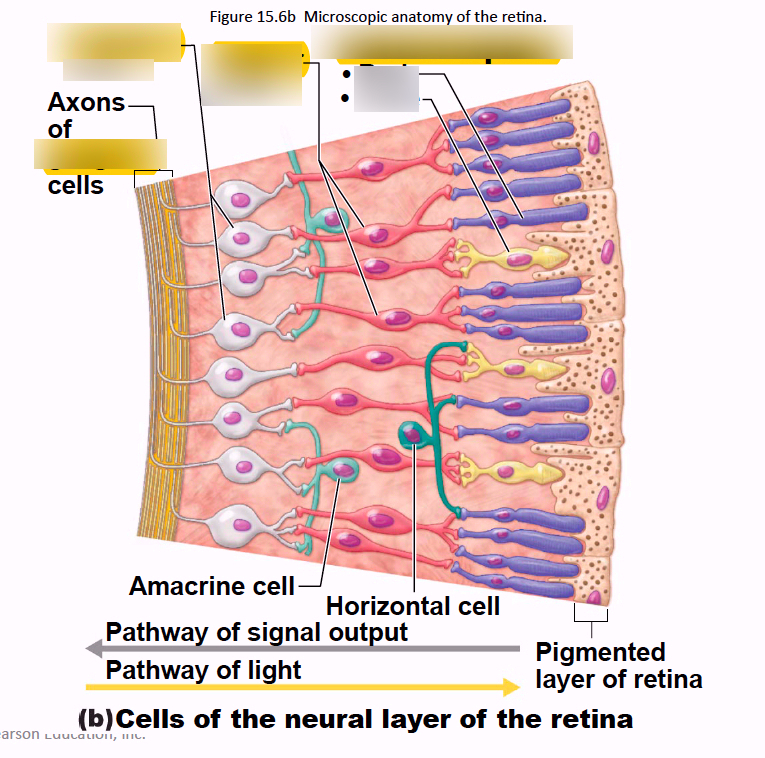
Axons of all ganglion cells gather posteriorly to form _____ _____
Optic nerve
Point where optic nerve leaves the eye?
Optic disc (the blind spot)
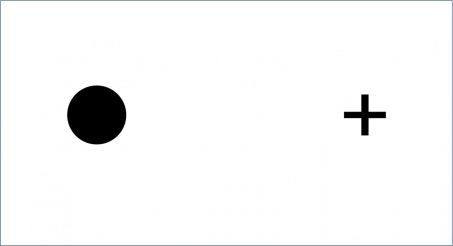
Blind spot test
Hold the diagram about 20in from face with left eye closed. focus on circle lined up with right eye. Slowly bring page closer to face until cross disappears. Then move until cross reappears. Repeat with left eye
Why don’t we always have a blind spot in our vision?
Due to overlap with our other eye, they cover each others blind spots. When one eye is closed, the brain “fills in the gap” using context of surrounding view.
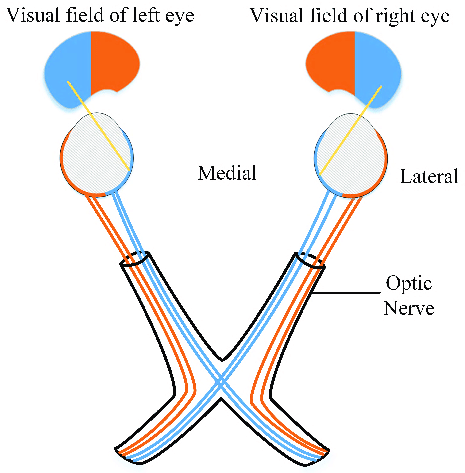
Where do the two optic nerves meet?
Optic chiasma
Axons from the [medial or lateral] region of each eye cross over at the optic chiasma?
The medial region
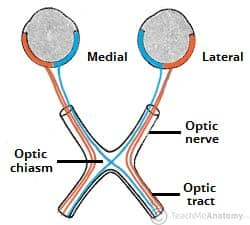
Axons from the [medial or lateral] region of each eye do NOT cross over and continue to same side of brain?
Lateral region
Refresh! Tract versus Nerve??
A tract is a collection of axons in the CNS, a nerve is a collection of axons in the PNS
Right optic tract
Formed of fibers from the medial half of left eye and lateral half of right eye.
Left Optic tract
Formed of fibers from the medial half of the right eye and lateral half of left eye.
Lateral geniculate body
Region where most optic tract axons end, found in the thalamus (the relay station between the eye and the visual cortex)
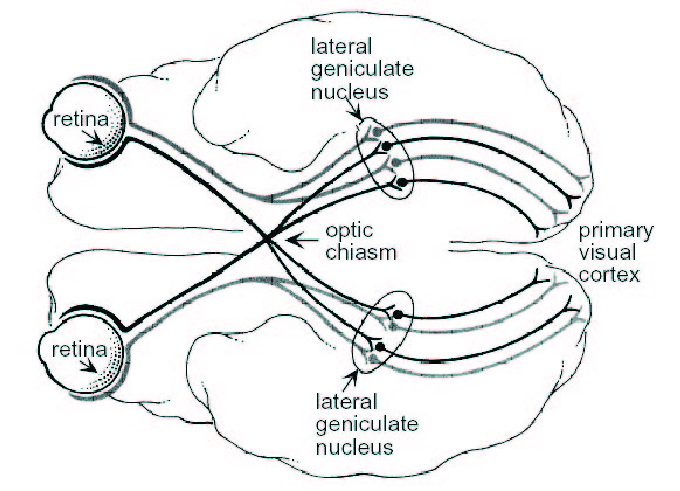
Function of axons that don’t end at the lateral geniculate body?
Function in visual reflexes
Neurons of the lateral geniculate body form fibers of _____ __________ that project to the _______ ______ ______ in the occipital lobe
optic radiations to the primary visual cortex
Visual cortex function?
Integrates retinal messages into single message, translates into mental image and relays to other parts of brain where it is acted upon or ignored.
Binocular vision
Type of vision in humans. Although both eyes look in approx same direction they see slightly different images, but there is overlap.
Provides humans with stereopsis, 3D vision and accurate spatial + depth perception
Depth perception test
Drop pencil into narrow neck bottle with both eyes open. Repeat with one eye open.
Clinical Significance: to determine if the subject has difficulty integrating the overlapping images from the left & right visual fields
Confrontational visual field exam (Donder’s test)
Subject covers one eye stares straight ahead at dark background. Examiner stands out of sight, moves bright object out of visual field laterally. Subject signals when no longer visible in their peripheral view. Repeated for other eye.
Clinical Significance: a visual field test used to determine if the subject suffers from deficits in their peripheral vision
Amsler grid test
Place grid on flat surface. Stand above grid at normal reading distance. Test one eye at a time, focus on centre dot. Note if lines appear straight or they appear broken, distorted, blurred or gaps.
Clinical Significance: to determine if the subject suffers from macular degeneration, glaucoma, and/or a detached retina. Will not be accurate if astigmatism is present but NOT used to test for astigmatism.
Diplopia
“double vision” caused by lack of integration of binocular views from each eye in brain.
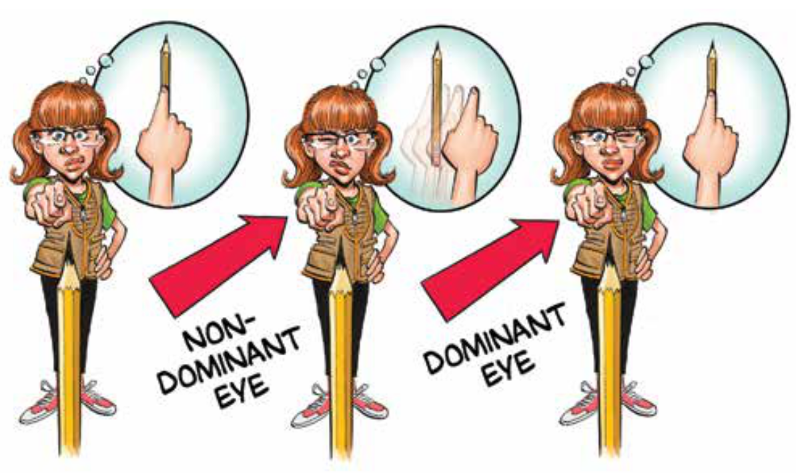
Dominant eye test
With both eyes open, hold a pencil in front of you, lined up with object in the distance. Close one eye, open it, close the other. The eye that allows you to keep the pencil in line with the object is your dominant eye.
Two Types of muscle filaments
Actin (thin) and Myosin (thick)
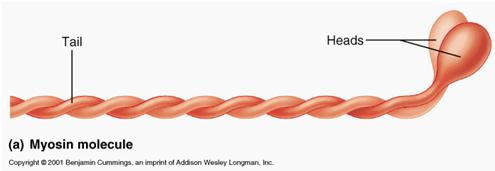
Thick filament
Consists of many myosin molecules whose heads protrude at opposite ends of the filament.
Myosin molecule (5 parts)
Head, tail, flexible hinge region, ATP-binding site, Actin-binding site
Thin filament
Two strands of actin subunits twisted into a helix + two types of regulatory proteins (troponin and tropomyosin)