Chapter 14: Cardiovascular Physiology単語カード | Quizlet
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
80 Terms
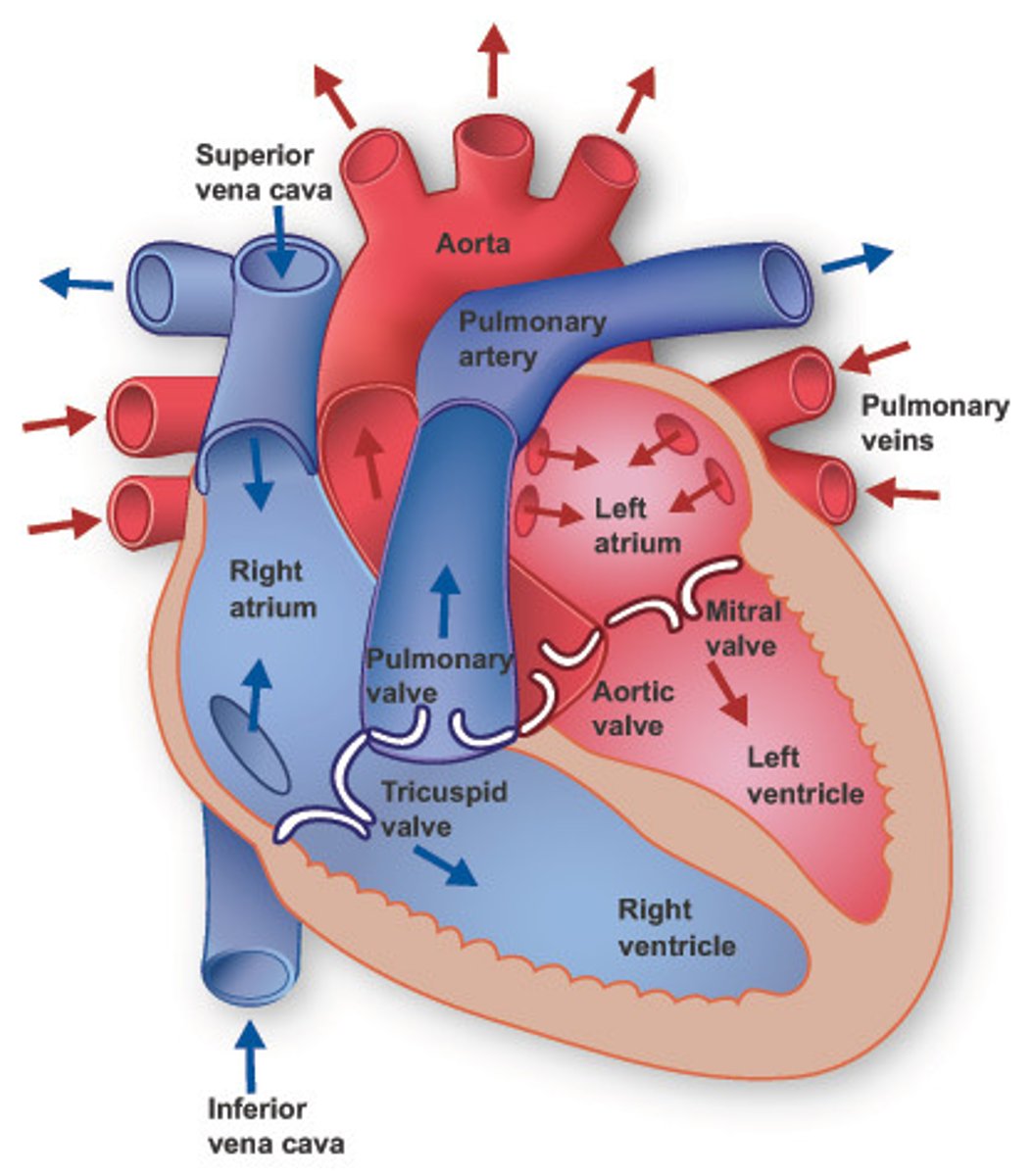
transportation
- nutrients from outside of the body to cells
- cell to cell transport
- wastes produced by cells
What is the function of cardiovascular system?
vasculature
(arteries, capillaries, veins)
heart
(2 atria, 2 ventricles)
double pump
valves
(veins and heart)
one way flow
What is the cardiovascular system composed of?
arteries
takes blood away from heart
veins
takes blood back to heart
capillaries
microscopic vessel through which exchanges take place between the blood and cells of the body
right atrium → right ventricle → pulmonary trunk (arteries) → lungs → pulmonary veins → left atrium
RA →RV →PT →L →PV →LA
What is the flow of blood in the pulmonary circulation?
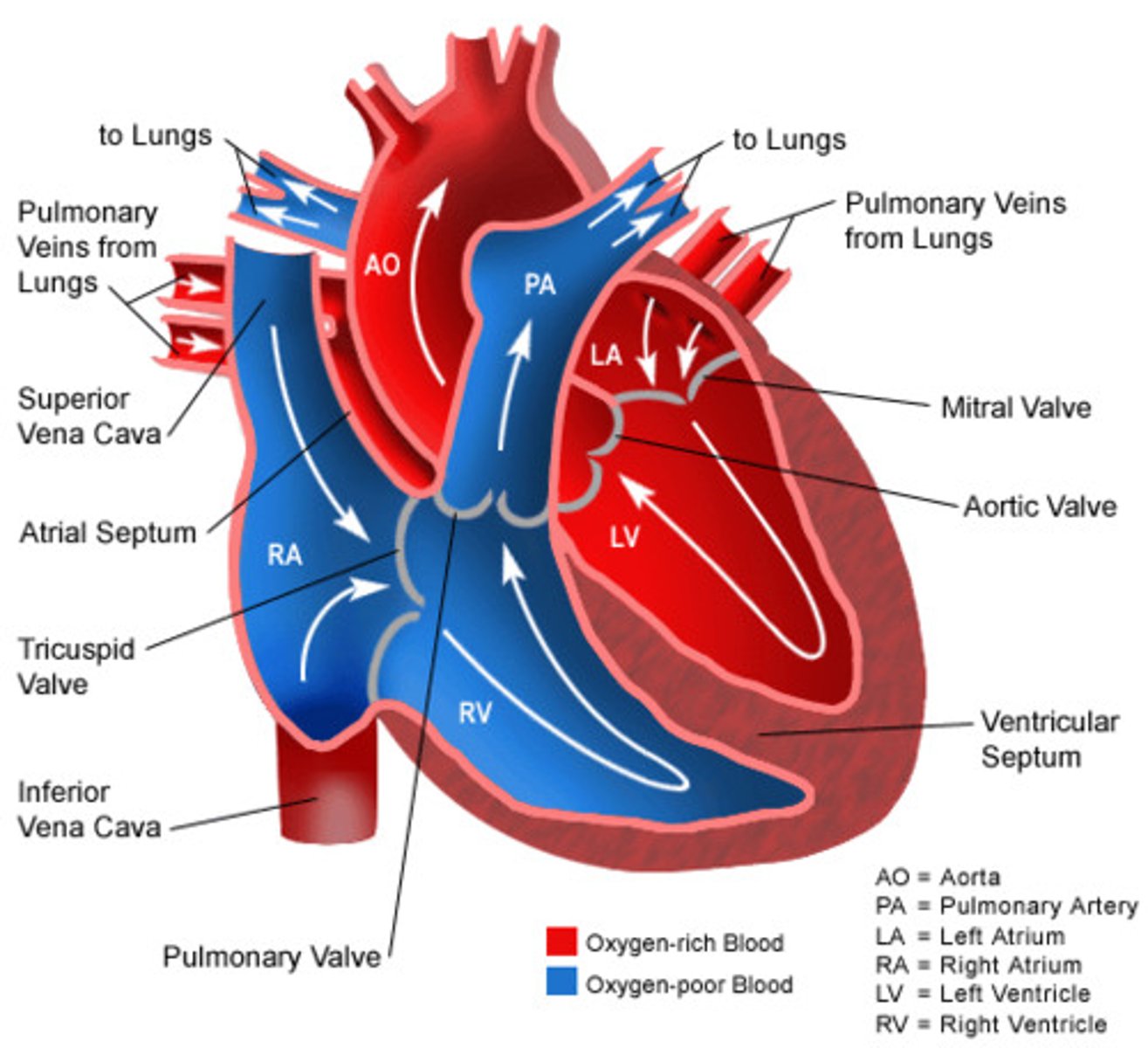
left atrium → left ventricle → aorta (arteries) → systemic tissues → vena cavae → right atrium
LA →LV →A →tissue → VC →RA
Normal pathway: artery →capillary →vein
What is the flow of blood in the systemic circulation?
artery →capillary →portal vessel →capillary →vein
there are portal systems in:
- GI tract and liver
- kidneys
- hypothalamic-hypophyseal portal system
What is the flow for portal systems?
Where are portal systems?
flow
movement of fluid
follows pressure gradient
follows pressure gradient (∆P)
(high P → low P)
Left ventricle → Right Atrium
flow is proportional to ∆P
What is the relationship of flow and change in pressure ∆P?
∆P = P1 - P2
How do you find ∆P?
lateral pressure
hydrostatic (hydraulic pressure) (fluid is not moving, force is exerted equally in all directions)
exerted on walls of vessels - pressure against walls
decreases due to friction
driving pressure
pressure from ventricular contraction (left ventricle)
pressure gradient
∆P = P1 - P2
Flow is proportional ∆P
(↑ ∆P → ↑ F)
Flow is measured in mmHg/mL/min
There is also resistance to flow
Resistance opposes flow - makes it harder for blood to flow
Flow is inversely proportional to resistance
↑ R → ↓ F
What is resistance and how does it relate to flow?
- vessel radius
↑ vessel radius → ↓ R (bigger the size of vessel, easier it is for blood to flow)
- blood viscosity
↑ viscosity ↑ R
(the thicker the blood is, the harder it is to flow)
- vessel length
↑ length ↑ R
(the further it takes blood to flow, the harder it is)
**radius is the only thing that is inversely proportional to resistance**
What are factors affecting resistance?
flow rate (Q)
measured in L/min or mL/min
it is volume per time; how much is moving in a time
average Q for 70 kg man at rest = 5L/min
velocity of flow (v)
Measured in cm/min or mm/sec
it is distance per time; how fast it is moving in a time
v = Q/A
- proportional to flow rate
- inversely proportional to area
Flow = ∆P/R
Flow: movement of blood
- directional flow from ventricle toward atrium
∆P: change in pressure
- difference in pressure from point A to point B
R: resistance
- impedance to flow
What is the relationship of flow, ∆P, and R?
MAP
mean arterial pressure
- pressure generated by ventricular contraction
- arteries maintain pressure during ventricular
- in periphery (organs and tissues)
CO = cardiac output
- volume per time
R = peripheral resistance
- impedance to flow
MAP = CO x R
How do you find MAP?
pericardium
epicardium
myocardium (cardiac muscle)
endocardium
What are the three layers of the heart?
(outer most to inner most)
tricuspid & bicuspid valves
What are the AV (atrioventricular) valves?
pulmonary and aortic valves
What are the SL (semilunar) valves?
innervates entire heart
- Norepinephrine: B1 adrenergic receptors
- Epinephrine (adrenal medulla): B1 adrenergic receptors
Describe the sympathetic innervation of the heart.
Vagus and cranial nerve X
primarily innervates the atria
- ACh: muscarinic receptors
Describe the parasympathetic innervation of the heart.
coronary circulation: coronary arteries and veins supply blood to the heart muscle
systemic blood flow
Where does the heart's blood supply come from?
its ability to contract without any outside signal; accounted for by myocardial cells specialized to generate APs spontaneously
What is a unique property of the heart?
Autorhythmic cells
Contractile cells
What are the 2 types of cardiac muscle cells?
autorhythmic cardiac cells
Pacemakers
also called conductor cells
Generate and conduct action potential
Cell structure:
- small
- few contractile fibers
- no organized sarcomeres
contractile cells
Myofibers
generate force
Cell structure:
- branching
- striated
- sarcomeres
- Intercalated disks
- Desmosomes: strong connections that tie adjacent cells together, allowing force created in one cell to be transferred to the adjacent cell
- Gap junctions: electrically connect cardiac muscle cells to one another. Allow waves of depolarization to spread rapidly from cell to cell so that all heart muscle cells contract simultaneously.
- smaller SR
- less Ca2+ storage
- larger and branching T-tubules
- many mitochondria
- usually uninucleate
1. ) Force developed is proportional to the # active crossbridges
- proportional to the amount of Ca2+ entering
- Effect Ca channel blocker on heart? low force contraction
2.) Sarcomere length at onset of contraction
- frank-starling law of the heart: ↑ length → ↑ force (to a maximum)
- the more blood that fills the ventricles, the more the heart stretches, the more force is used to pump blood out
What two factors impact cardiac contractility?
Myocardial Contractile cells Action potential info
Similar to neurons and skeletal muscle. The rapid depol. phase of the AP is the result of Na entry and the steep repol. phase is due to K leaving the cell.
Has a longer AP due to Ca2+ entry
Resting membrane potential (4): -90mV
Rapid depol. (0): voltage gated Na channels open: 20 mV
Initial repolarization (1): voltage gated Na channels inactivate; fast voltage gated K channels open
Plateau phase (2): voltage gated Ca channels open; fast voltage gated K channels close
Rapid repolarization (3): slow voltage gated K channels open; voltage gated Ca channels close

The influx of Ca2+ during the plateau phase lengthens the total AP duration. (normal AP of skeletal = 1-5ms; AP here = 200 ms or more)
longer AP helps prevent tetanus: important because cardiac muscles must relax between contractions so ventricles can fill with blood
refractory period and contraction end almost simultaneously, no summation occurs; inability to develop tetanus
What is the duration of the AP of the myocardial contractile cells?
How is it possible for autorhythmic cells to develop APs spontaneously?
Pacemaker potential:
They have unstable "resting" membrane potential (starts at -60mv and slowly drift upward toward threshold)
- If channels: when cell membrane potential is -60mV
- these are permeable to both K and Na open.
- allow current to flow aka funny
- voltage gated Na and K channels
- Na movement>K movement
- Some depolarization
- If channels close
- T type voltage gated Ca channels open
- membrane potential steadily moves toward threshold
Action potential:
- rapid depol: when L type voltage gated Ca2+ channels open
- rapid repol: slow voltage gated K channels open
- L type voltage gated ca2+ channels close
Resting membrane potential: unstable vs stable
Generation: autorhythmic vs. stimulated
Voltage gated channels and ion movement in rapid depolarization: Ca2+ vs. Na ions
Shape: classic vs plateau
A comparison of Conduction (autorhythmic) cells vs. contractile cells
Sinoatrial Node (SA)
pacemaker; 90-100 bpm
- depolarization begins here
- in the right atrium
- branched INTERNODAL pathway connects the SA node to the AV node.
- atrial contractile cells: contract top to bottom
Atrioventricular Node (AV)
25-40 bpm
- group of autorhythmic cells near the floor of the Right Atrium
- transmit across fibrous skeleton
- AV node delay: slower transmission
- allows atria to complete contraction before ventricular contraction
From the AV node, depol. moves into ventricles.
Purkinje fibers: specialized conducting cells in the ventricles
Purkinje fibers transmit electrical signals rapidly down the AV bundle( aka bundle of His) in the ventricular septum (divides into right and left bundle branches)
These continue down toward the apex and branch into smaller purkinje fibers that spread outward among contractile cells.
contract from apex to base
After the AV node, where does the depolarization signal move to?
SA node fires AP and depol. spreads to adjacent cells through gap junctions. Electrical conduction is rapid through internodal conducting pathways but slower through the contractile cells of the atria.
SA - Internodal pathway - AV - Purkinje - AV bundle - R&L bundle branches - smaller purkinje fibers - contractile cells at apex
contract apex to base
Overview of how electrical signal travels
electrocardiograms (ECG or EKG)
the use of surface electrodes to record internal electrical activity because salt solutions, such as our NaCl-based ECF, are good conductors of electricity.
they show the summed electrical activity generated by all heart cells
Einthoven's Triangle
basic shape of the heart
standard bipolar limb leads
- 3 electrodes: negative, positive, ground
- current moves from negative to positive
- same polarity: positive deflection
- opposite polarity: negative deflection
- perpendicular: no deflection
Lead I
right (-) arm to left (+) arm
Lead II
right (-) arm to left (+) leg
most closely follow general electrical axis of the heart
Lead III
left arm (-) to left leg (+)
Electrical events drive mechanical events in heart.
Which comes first? Electrical or mechanical events in the heart?
P wave: atrial depolarization
QRS complex: ventricular depolarization & atrial repolarization
T wave: ventricular repolarization
Waves of the ECG
cardiac cycle
all electrical and mechanical events that occur from the onset of one heart beat to the onset of the next heart beat.
- ECG, systole and diastole, valve opening and closing, blood flow
P wave: atrial depolarization
P-Q or P-R segment: conduction through AV node and AV bundle. (atria contract)
Q wave
R wave: Atrial repolarization
S wave
S-T segment: ventricles contract
T wave: ventricular repolarization
What are the electrical events of the heart?
from the beginning of one P wave to the next or
from the peak of one R wave to the peak of the next.
normal heart rate = 60-100 bpm
How can you calculate heart rate from an ECG?
one-way flow of blood
What is the function of valves in the heart?
Open
- pressure atria > ventricles
Closed
- pressure atria < ventricles
What is the pressure in the atria vs ventricles when the AV valves are open vs closed?
Open
- pressure ventricles > great artery
Closed
- pressure ventricles < great artery
What is the pressure in the great artery vs ventricles when the SL valves are open vs closed?
Atria: relaxed and filling
Ventricles: relaxed and passively filling (80%)
this is where the S3 heart sound is heard
the AV valves are open and the SL valves are closed
Describe late atrial diastole/ventricular diastole
Atria: contraction and emptying
Ventricles: relaxed and final filling - 20%
this is where the S4 heart sound is heard
the AV valves are still open and SL valves are still closed
Describe atrial systole/ventricular diastole
Describe Atrial Diastole/early ventricular systole
Atria: relaxed and filling
Ventricles: isovolumetric contraction (volume of blood not changing)
Valves
AV valves close, SL valves still closed
- S1 heart sound is heard
Describe atrial diastole/ ventricular systole
Atria: relaxed and filling
Ventricles: contraction and ejection
Valves:
AV still closed, SL valves open
Describe atrial diastole/ ventricular diastole
atria: relaxed and filling
ventricles: isovolumetric relaxation
valves:
- AV valves still closed, SL valves close
S2 heart sound (dub)
P wave: SA node and atrial depolarization: atrial systole begins
P-R segment: AV node delay - AV node and AV bundle, completion of atrial systole
QRS complex: beginning of Q to end of S
- ventricular depolarization - ventricular systole begins
- atrial repolarization - atrial diastole
ST segment
- end of S to beginning of T wave
- isoelectric: ventricles fully depolarized- ventricular systole
T wave: ventricular repolarization: ventricular diastole begins
QT interval: beginning of Q to end of T wave: depolarization and repolarization of ventricles
- long QT syndrome: prolonged QT interval = ventricular tachyarrhythmias and potential sudden death
- ventricular fibrillation
- short QT syndrome - shortened QT interval = ventricular tachyarrhythmias and potential sudden death
- ventricular fibrillation
ST interval: end of S to end of T
U wave: usually absent:
- repolarization of interventricular septum
- may be related to hypercalcemia, hypokalemia, or hyperthyroidism
T-P segment: electrically quiet, mechanically quiet - atrial and ventricular diastole
Electrical and Mechanical events
stroke volume (SV)
volume of blood ejected by ventricular systole
ml/beat
End Diastolic Volume (EDV)
volume of blood at the end of ventricular diastole
- passive filling and atrial systole
mL
End Systolic Volume (ESV)
volume of blood remaining in each ventricle after systole
mL
SV = EDV - ESV
at rest 70 mL = 135 mL - 65 mL
What does Stroke Volume (SV) equal?
Cardio Output (CO)
L/min pumped by each ventricle
RV volume = LV volume
CO = HR x SV
Cardiac output = heart rate x stroke volume
average resting CO = 72 bpm x 0.07 L/beat = 5 L/min
increased HR = Increased CO
increased SV = increased CO
CO = HR x SV
How do you find CO?
after blood loss
When can heart rate increase but stroke volume decrease?
after blood loss
well conditioned heart
When can heart rate decrease but stroke volume increase?
Tonic control: SA rate is about 100 bpm, normal resting heart rate is 70 bpm.
Vagus nerve innervates; ACh and muscarinic cholinergic receptors
- increase K permeability which hyperpolarizes cell
- decrease Ca permeability: takes longer to depolarize
decrease conduction velocity and increase AV nodal delay
no major effect on contractility
How is the heart rate regulated by the parasympathetic system?
catecholamines NE (neurons) and E (adrenal gland) and B1 receptors
- increase activity of If channels which increases Na and Ca permeability which depolarizes faster
increase conduction velocity
increase contractility
- increase Ca permeability
How is the heart rate regulated by the sympathetic system?
1. ) Length: tension and Frank-Starling mechanism
- preload: EDV (ventricular return)
- increase EDV which increases sarcomere stretch which increases force of contraction which increases SV
- vasoconstriction of veins
- skeletal muscle pump
- respiratory pump: alters abdominal vs thoracic pressure
2.) Sympathetic input to ventricles
- increased contractility
- increased ejection fraction which increases SV
- EF = SV/EDV
- also get an increased rate of contraction
3. ) Afterload
- combined load of EDV and arterial resistance
- increased afterload = decreased SV
- can occur w/some cardiovascular diseases
What three factors affect the regulation of stroke volume?
Normal = 60-100 bpm
Tachycardia >100 bpm
Bradycardia < 60 bpm
what is sick sinus syndrome: alternate between too fast and too slow
What are arrhythmias associated with the SA node?
heart block
interrupted communication between SA and AV nodes
- 2:1 heart block: 2 P waves for every QRS complex
- complete heart block: occurs when the electrical signal can't pass normally from the atria, the heart's upper chambers, to the ventricles, or the lower chambers. may result if the AV node is damaged.
filibrillation
uncoordinated myocardial contractions
- atrial: AF or Afib: increased risk of heart attack and stroke
- ventricular: VF or V fib: immediately life threatening
artificial pacemaker: node ablation
defibrillators:
AED: automated external defibrillator
ICD: implantable cardiac defibrillator
Nodal ablation: (burn the node that is firing wrong)
- SA node
- AV node
What is the treatment for fibrillation?
valve defects: insufficient, stenotic
septal defects: atrial septal defect, ventricular septal defect, AV septal defect (between RA and LV)
timing
What can cause murmurs?
insufficient valve
allows back flow
often hear a lower pitched gurgle type murmur
stenotic valve
A valve that does not open properly
often hear a higher pitched whistle type murmur
Open: stenotic AV valves
Closed: insufficient SL valves
During ventricular diastole: Which valves should be open? Which valves should be closed?
Open: stenotic SL valves
Closed: insufficient AV valves
During ventricular systole: Which valves should be open? Which valves should be closed?
What is hypertrophic cardiomyopathy?
thickening of the walls
improper tissue structure
consequences: inefficient beats, decreased coronary blood flow.