MLS2 Exam 1: Endocrine
1/473
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
474 Terms
insulin is released by what in response to ?
Released by β-cells of the pancreas in response to ↑ plasma glucose levels
insulin binds to _______ on target tissues on adipose tissue, liver, skeletal, muscle
insulin receptors
what is insulins effect on adipose tissue?
Enhances glucose uptake by adipocytes
↑ Lipogenesis & ↓ Lipolysis
what is the most sensitive pathway of insulin action?
Inhibition of lipolysis in adipose tissue
what are the effects of insulin on skeletal muscle?
Enhances glucose uptake by skeletal myocytes
↑ Glycogenesis & ↓ Glycogenolysis
↑ Protein synthesis & ↓ protein breakdown
glucose uptake by hepatocytes is insulin-mediated t/f
false
what are the effects of insulin on the liver?
↑ Glycogenesis
↓ Glycogenolysis
↑ Lipogenesis
"Low insulin sensitivity" =
insulin resistant
insulin resistance (IR)
a state in which a given concentration of insulin produces a less-than-expected biological effect
what does IR result in?
hyperinsulinemia
as levels of insulin increases, what happens to the receptors?
decrease
how does IR affect adipose tissue?
Impaired insulin-stimulated glucose uptake by adipocytes
↓ Lipogenesis & ↑ Lipolysis
The "downward spiral" of lipolysis seen in IR and adipose tissue =
lipotoxicty
how does IR affect skeletal muscle?
Impaired insulin-stimulated glucose uptake by skeletal myocytes
↓ Glycogenesis & ↑ Glycogenolysis
↓ Protein synthesis from AA
↑ protein breakdown into AA
As in adipose tissue, any insulin receptor stimulation that DOES occur in skeletal muscle is muted/attenuated which ?
perpetuates the cycle of IR
IR & its resulting hyperinsulinemia still stimulates the liver to ?
↑ Glycogenesis & ↓ Glycogenolysis
↑ Lipoprotein (VLDL) formation
When glucose is unavailable to tissues for fuel, the liver makes alternative sources of energy. what 2 process are increased?
↑ Gluconeogenesis
↑ Ketogenesis
what are the 3 physiologic ketones produced by the human body?
Acetone
Acetoacetic acid/acetoacetate (AcAc)
β-hydroxybutyric acid/β-hydroxybuterate (β-HBA)
what is the largest risk factor for IR?
metabolic obesity
obesity is the state of excess adipose tissue mass and an increase in what 3 things?
number of adipocytes (hyperplasia)
lipid deposition within adipocytes (adipocyte hypertrophy)
tissue macrophages within adipose tissue
what does true "obesity" imply?
↑ morbidity & mortality
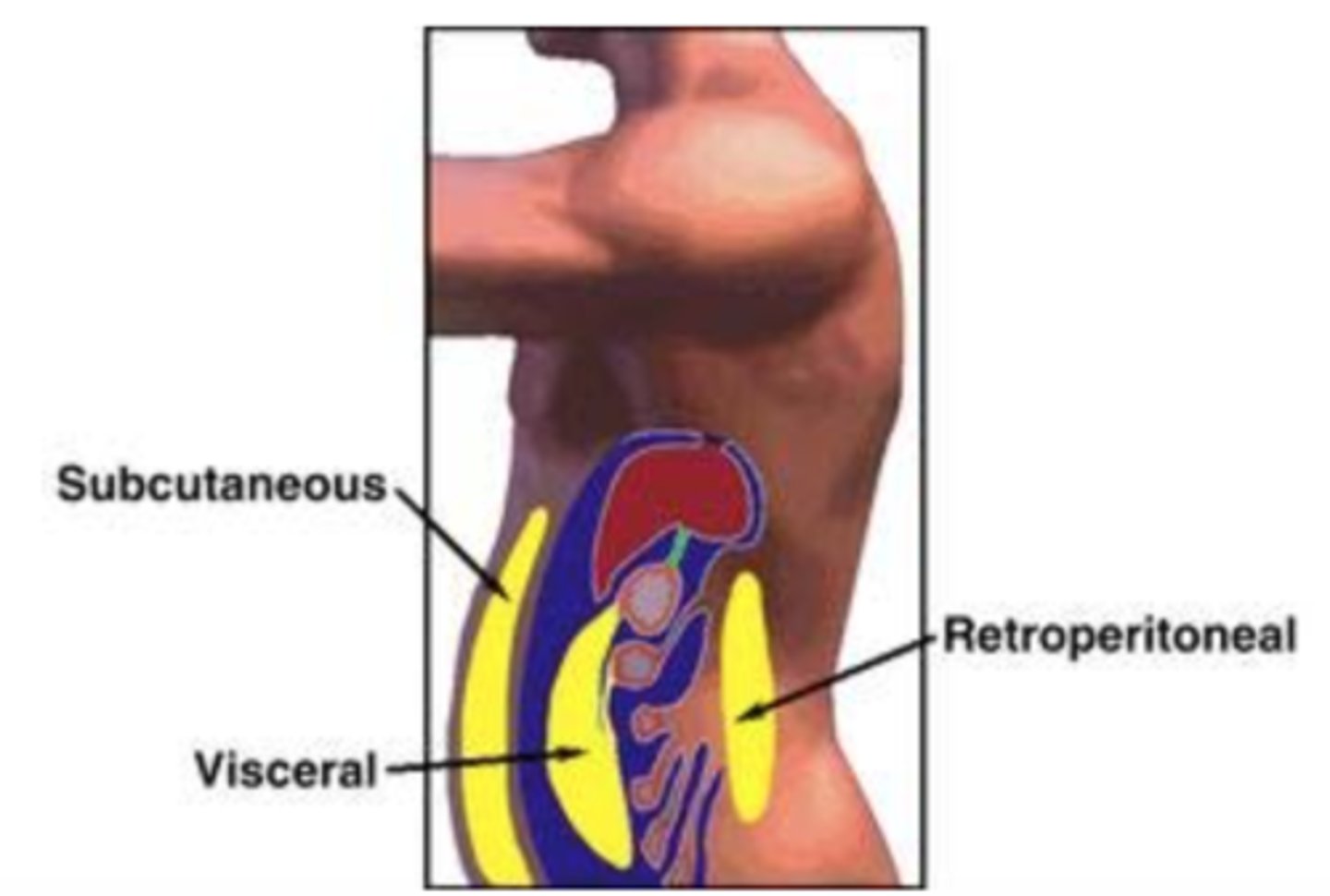
what is the difference between visceral and subcutaneous adipose tissue?
visceral or central is located deep in the abdominal cavity and is more metabolically active
subcutanous or peripheral is located just beneath the skin commonly located in the lower extremities/buttocks
what is the most widely used method to gauge obesity?
BMI
what are the NIH definitions for adult BMI?
Normal
18.5-24.9 kg/m2
Overweight
25-29.9 kg/m2
Obesity
≥ 30 kg/m2
Grade/Class I: 30-34.9 kg/m2
Grade/Class II: 35.39.9 kg/m2
Grade/Class III (Extreme/Morbid/Severe Obesity): ≥ 40 kg/m2
what other anthropomorphic measurements (other than BMI) are useful in accessing metabolic syndromes?
waist circumference
waist to hip ratio
waist to height ratio
why is visceral fat more more susceptible to ↑↑↑ lipolysis?
Insulin receptors in visceral adipose tissue have a lower affinity for insulin which impairs the ability of insulin to suppress lipolysis
Visceral adipose tissue is more sensitive to the stimulatory effects of the counter-regulatory hormones that ↑ blood glucose (usually via glucagon)
what are 2 counter-regulatory hormones that ↑ blood glucose?
epinephrine and cortisol
how can adipokines act as cytokines?
creating a pro-inflammaotry state by drawing macrophages & other inflammatory mediator to various tissue surfaces
Central (visceral) adipose tissue drains directly into the portal vein which exposes liver to ↑ levels of FFA & altered adipokine levels and stimulates the liver to produce what 2 things?
C-reactive protein (CRP)
Fibrinogen
hunger and "overfeeding" is seen in IR due to the shortage of fuel for cellular function and dysfunction of what appetite/satiety hormone?
leptin
what is "pancreatic poop out"?
when the compensatory mechanism of the pancreas producing sufficient insulin to regulate blood glucose fails
explain the process when an insulin resistant person eats food
Food ↑BG → Pancreas secretes Insulin in response to ↑BG → IR prevents insulin & glucose from entering cell → Cells don't have fuel* so you feel hungry & eat more
explain the progression of insulin resistance
postprandial hyperinsulinemia --> fasting hyperinsulinemia --> hyperglycemua and glucose intolerance --> type 2 DM
what are 2 features that can be seen in patients with IR and dyslipidemia? which is an excellent marker of IR?
Hypertriglyceridemia (↑TG)**
Low high-density lipoprotein (↓HDL)
when fasting TG is ~180 mg/dL what is there a predominance of?
sdLDLs
how can hyperinsulinemia and IR lead to hypertension and hyperuricemia?
HTN
Vasoconstriction
Inhibition of NO synthesis & its vasodilatory effects
↑ Activity of the SNS
Salt and water retention
↑ Renal reabsorption (↓ excretion) of Na+
HYPERURICEMIA
↑ Synthesis of uric acid
↑ Renal reabsorption (↓ excretion) of uric acid
how can metabolically active adipose tissue lead to hypertension?
Activation of the RAAS pathway
↓
Salt & water retention angiotensinogen-like substance & vasoconstriction
↓
HTN
in IR there is a predominace of sdLDLS, dysregulated adipokines act as cytokines, and there is metabolically active adipose tissue that all leads to what 2 things?
inflammation and hypercoagulability
what is metabolic syndrome?
Cluster of metabolic abnormalities that increase risk of T2DM and CVD
what is the goal for a patient with metabolic syndrome?
decrease overall cardiac M&M
what is the driving force behind the development of metabolic syndrome?
obesity
what is the pathophysiology of metabolic syndrome?
insulin resistance (HYPERinsulinemia)
name some clinical features of metabolic syndrome
↑ Waist circumference/central adiposity
Adipokine dysregulation
Pro-inflammatory cytokine excess
Insulin resistance (IR)
Impaired glucose tolerance (IGT)
Atherogenic dyslipidemia (↑TG & sdLDLs, ↓HDL)
Hypertension (HTN)
Hyperuricemia
↑ Prothombotic factors (fibrinogen, PAI-1)
Endothelial dysfunction
what is the NCEP/ATP III criteria for metabolic syndrome?
Three or more (≥3) of the following criteria: central obesity, hypertriglyceridemia, low HDL, elevated blood pressure, hyperglycemia
name 3 associated conditions that can be seen with metabolic syndrome?
liver disease, PCOS, obstructive sleep apnea
what is sometimes seen on physical exam in patients with severe insulin resistance? (hyperpigmentation in folded areas)
Acanthosis nigricans

what is the most important component for weight reduction in obesity management?
caloric restriction
what is the most important component for maintenance of weight loss?
physical activity
what are 2 options other than lifestyle intervention for patients with significant obesity? what is the BMI for each?
Weight loss medications
BMI ≥30 kg/m2
Bariatric surgery
BMI ≥40 kg/m2
popular weight loss medications such as ozempic and wegovy are what kind of medications?
GLP-1 receptor agonists (GLP-1 RAs)
what is the first choice for dyslipidemia therapy for a patient with metabolic syndrome?
statins
what is the first choice for hypertensive therapy for a patient with metabolic syndrome?
ACE/ARBs
what are 2 common "insulin-sensitizers" used for hyperglycemia therapy?
Biguanides [metformin (Glucophage®)]
Thiazolidinediones (TZDs)
how frequent should a patient with metabolic syndrome follow up with there provider?
individualized to patient
diabetes mellitus is considered a risk equivalent to what?
coronary artery disease
what is the pathophysiology of type 1 DM? what is required in these patients?
Some insult, or group of insults, leads to complete β-cell destruction & ↑ BG
Exogenous insulin
diabetes type 1A
immune mediated
diabetes type 1B
idiopathic
there are many possible etiologies to type 2 DM. what is the #1 enviornmental?
obesity
what is the basic pathophysiology behind type 2 DM?
insulin resistance
what is the term for a milder atypical form of type 1 DM where there is enough B cell function to not develop ketosis?
latent autoimmune diabetes of adulthood (LADA)
maturity-onset diabetes of the young affects non obese pts <25 years old and is an autosomal _________ trait
dominant
name 3 secondary causes for diabetes
endocrine disorders/tumors
pancreatic disorders
medications
what are some possible signs/symptoms a patient with type 1 diabetes might present with?
Polyuria
Polydipsia
Polyphagia with Weight Loss
Weakness/Fatigue
Recurrent Blurred Vision
Vulvovaginitis/Balanitis (Pruritus)
Peripheral Neuropathy
Nocturnal Enuresis
what are some possible signs/symptoms a patient with type 2 diabetes might present with?
Polyuria
Polydipsia
(Polyphagia with Weight Loss?)
Weakness/Fatigue
Recurrent Blurred Vision
Vulvovaginitis/Balanitis (Pruritus)
Peripheral Neuropathy
(Nocturnal Enuresis?)
Often Asymptomatic
what is considered normal glucose tolerance, impaired glucose tolerance, and diabetes mellitus for a fasting plasma glucose?
norm: <100
impaired: 100-125
DM: ≥ 126
what is considered normal glucose tolerance, impaired glucose tolerance, and diabetes mellitus for a 2-hour postprandial?
norm: <140
impaired: 140-199
DM: ≥ 200
what is considered normal glucose tolerance, impaired glucose tolerance, and diabetes mellitus for a HbA1C?
norm: <5.7%
impaired: 5.6-6.4%
DM: ≥ 6.5%
what is the leading cause of death in type 2 DM?
coronary disease (CAD/MI)
what is a complication of DM that includes PAD, ED, and gangrene?
peripheral vascular disease
you are screening one of your diabetic patients for CV risk factors. they have stage one (≥130/80 mmHg) HTN and dyslipidemia. what are you treating them with?
HTN- ACE or ARB
Lipid - statin
what are DM agents with CV benefit?
SGLT2i, GLP-1RA
what is a leading cause of CKD that accounts for 20% of deaths in patients with DM younger than 40?
diabetic nephropathy
what screening is required at a minimum for diabetic nephropathy?
Annual urine albumin/creatinine ratio (UACR)
what is the treatment fro diabetic nephropathy?
Strict control of blood sugar (SGLT2 inhibitor or GLP-1 RA)
Smoking cessation if applicable
Management of HTN +/- albuminuria
what is the name of the drug for T2D pts w/ CKD + albuminuria on max tolerated doses of ACEi/ARB?
finerenone (Kerendia®)
what is the most common complication of DM?
diabetic neuropathy
what screening should be done annually on all diabetic patients for diabetic neuropathy?
DFE + Monofilament including skin/pulses too
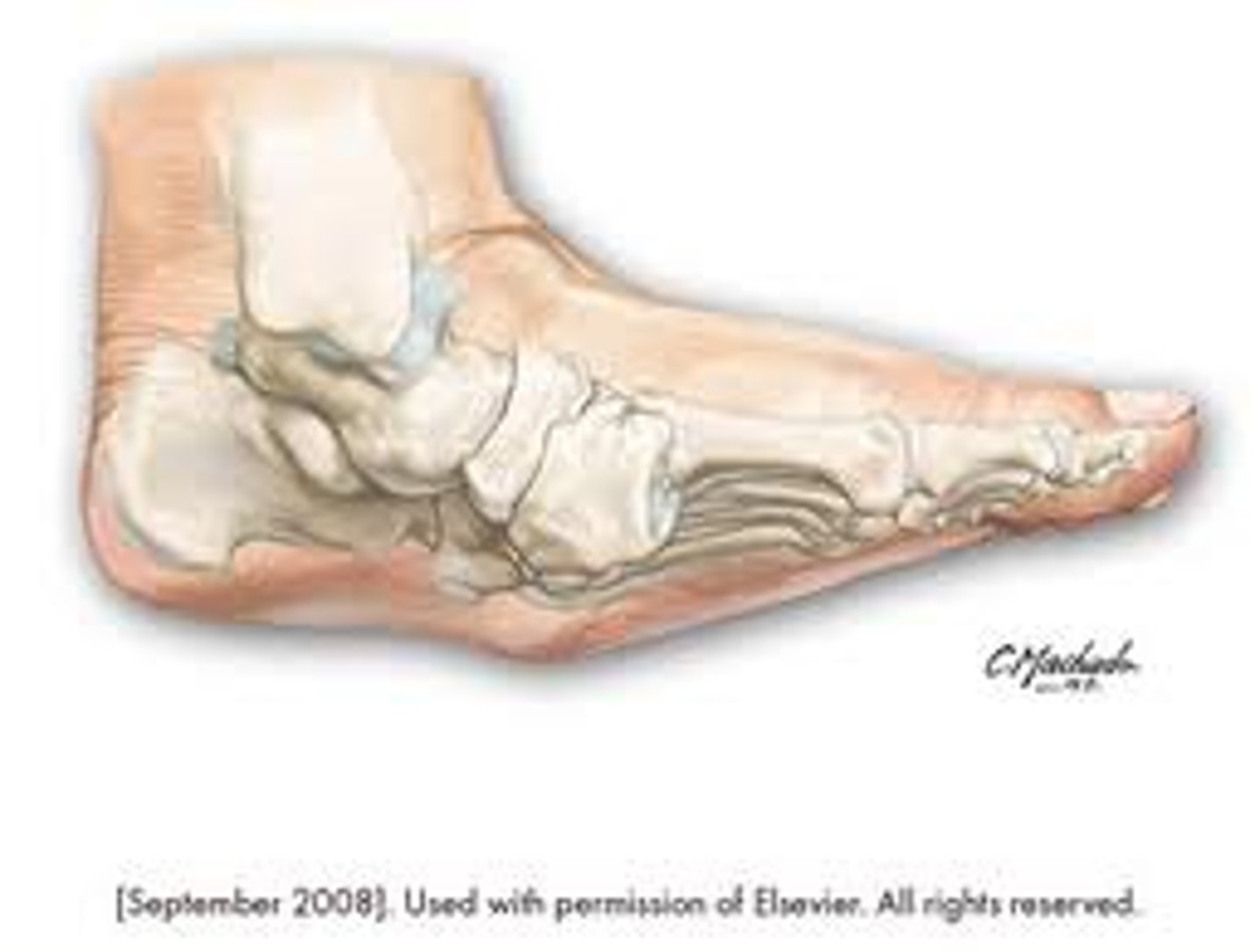
charcot foot
neuropathic fracture/dislocation found in patients with diabetes
what are 2 FDA approved treatment options for neuropathy pain?
pregabalin (Lyrica®) duloxetine (Cymbalta®)
what are 4 central neuropathies that are complications of DM?
Orthostasis
Gastroparesis
Erectile Dysfunction (ED)
Neurogenic Bladder
what are 3 ocular complications of DM?
diabetic cataracts, glaucoma, diabetic retinopathy
what is the difference between nonproliferative and proliferative diabetic retinopathy?
proliferative has nerovascularization
Disseminated granuloma annulare

Diabetic dermopathy

Necrobiosis lipoidica diabeticorum (NLD)

Bullosis diabeticorum
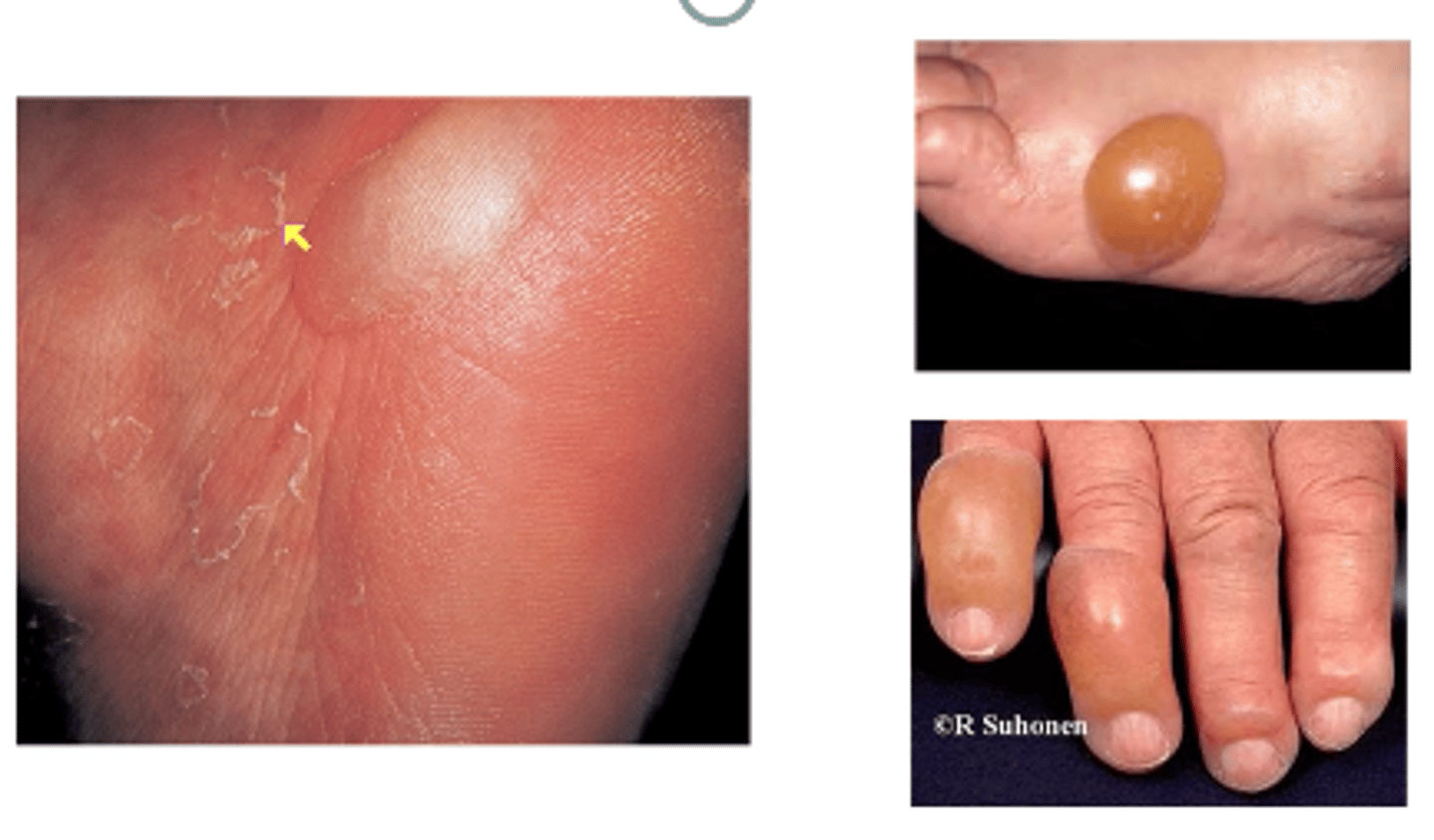
Digital sclerosis

what does a physical exam include for a person with DM?
anything DM can affect which is pretty much everything!
vitals, general, skin, eyes, neck, heart, lungs, abdomen, extremities, neuro, etc
what are the screening recommendations for type 2 DM is asymptomatic adults?
Test ALL adult patients beginning at age 35* (New 2022)
Test adult patients of ANY AGE who have overweight or obesity (BMI ≥25 kg/m2 or ≥23 kg/m2 in Asian Americans) AND have ≥1 additional risk factor(s) for DM
Pts with HIV (2023), on high risk meds (2024*), h/o pancreatitis (2024*)
t/f after a women with gestational diabetes gives birth there is no longer a concern for diabetes
false (should have lifelong testing every 1-3 years)
you test A1C, FPG, and 2-h 75-g OGTT on a patient if normal what then? if confirmed prediabetes then what?
If normal, repeat testing at 3-year intervals; if abnormal, repeat to confirm
If prediabetes, identify and, if appropriate, treat other CVD risk factors – follow yearly at a minimum
what are the screening recommendations for type 2 DM in asymptomatic childern?
Those who have overweight (BMI ≥85th percentile) or obesity (BMI ≥95th percentile) PLUS any 1+ risk factors
what age should you start screening children for type 2 that meet the requirements and how frequent?
age 10 years OR at onset of puberty, whichever comes first
every 3 years at minimum if normal
what test should be done every 3-4 months for diagnosis and regular monitoring and what test should be done annual?
blood testing- HbA1C
urinalysis- urinary albumin/creatinine ratio (UACR)
how can you tell if a patient has type 1 or type 2 DM?
Age at onset
Clinical characteristics like IR and acuity/severity of sxs
Glucosuria +/- ketonuria??
Autoantibody panel
what is the most important obligation of the clinician who provides initial care to a patient with DM?
education of the patient AND the family
what is the mainstay therapy for type 1 DM?
insulin
what is the 1st line therapy for patients with type 2 DM?
metformin
A1C goals must be individualized. according to the ADA what is the goal for most non pregnant patients? what about the AACE?
ADA- 7%
AACE-6.5%