Oct 8 Midterm Exam at 1800h followed by TAPED lecture: Honouring Dignity and Autonomy
1/26
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
27 Terms
Professional Identity
The set of attributes, beliefs, values, motives and experiences by which people define themselves in their professional lives – College of Nurses of Ontario
Self-Concept
Pathway to Professional Identity for Nurses
•Initiation:
•pre-existing values and beliefs about nursing and profession; level of education vs clinical experience; contrast btw personal values and socialization – “obedience”.
•Academics:
•identity construction and deconstruction; knowledge about professional values, history, health care system, ethics, skills, role models.
•Clinical Experience:
•key to creating a sense of belonging; sense of being undervalued can be challenging; somewhat removed from “norms”
•Transition to Practice:
•disconnect btw expectation and reality upon graduation; learning curve
•Evolution of identity in health care system:
• constantly developed, deconstructed, and re-developed; changes based on context
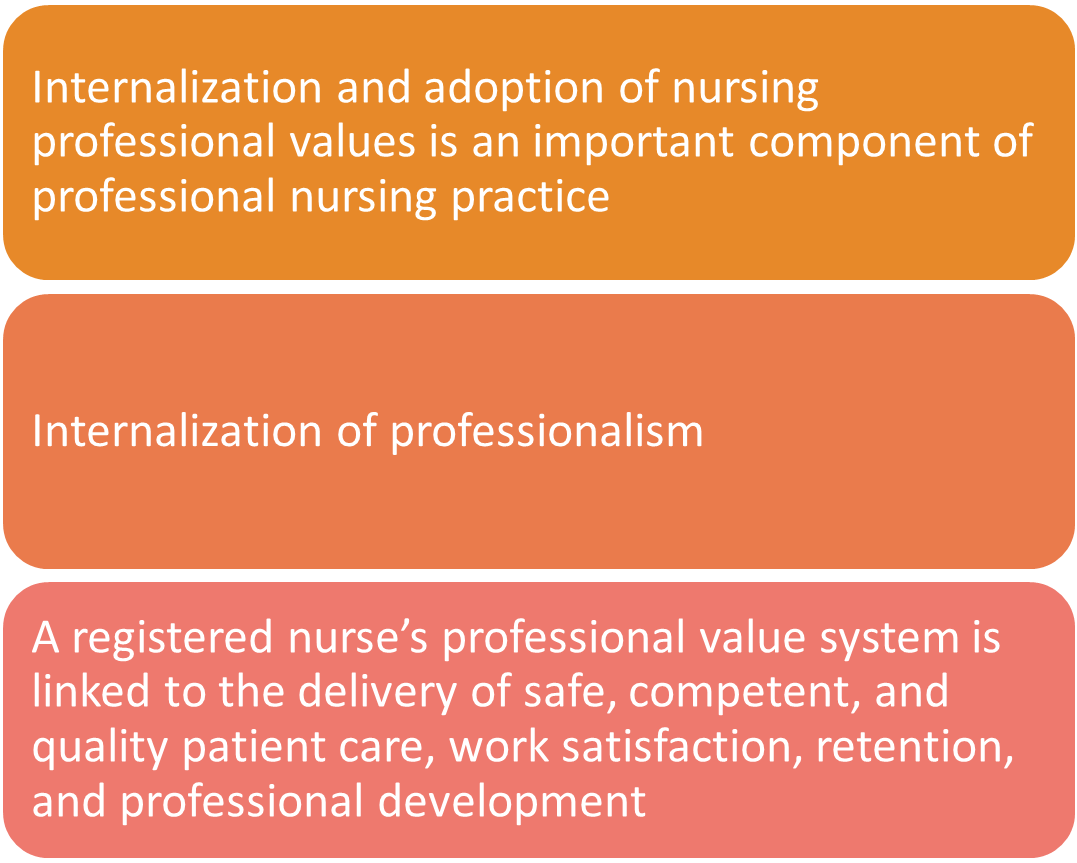
Professional Values
Evolving Profession
•Health care system is dynamic = adaptability
•Changing demands, evolving technology, government policies etc.
•Implementing change = anxiety, fear of failure and resistance to change
Evolving Self
•Those same health care changes, along with day to day nursing impacts our sense of self in relation to professional identity.
•Changes can be gradual and non-intentional.
•Changes are also personal and required for the profession.
Self-Reflective Practice
Gibbs Reflective Cycle
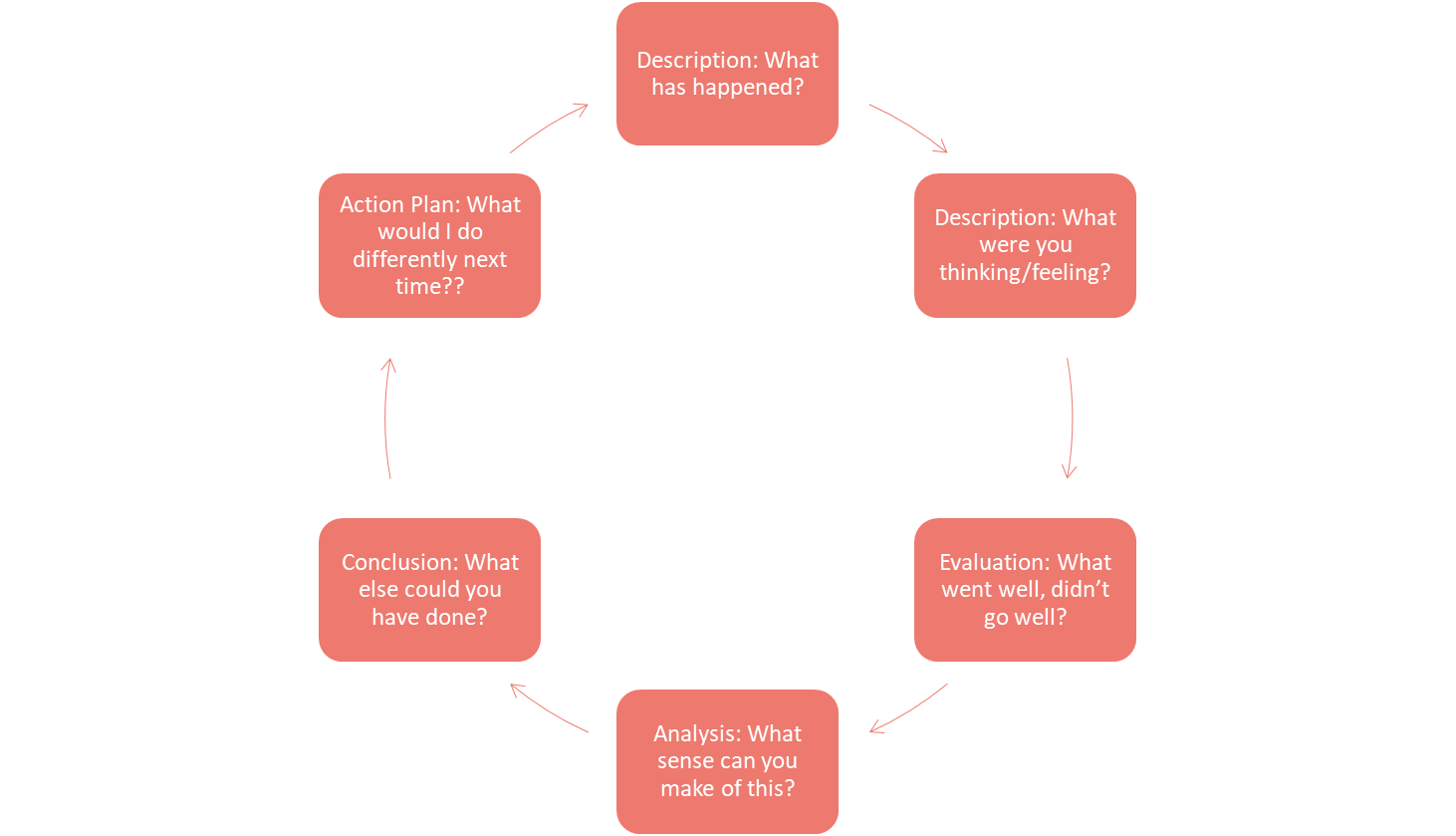
A common method of exploring an experience.
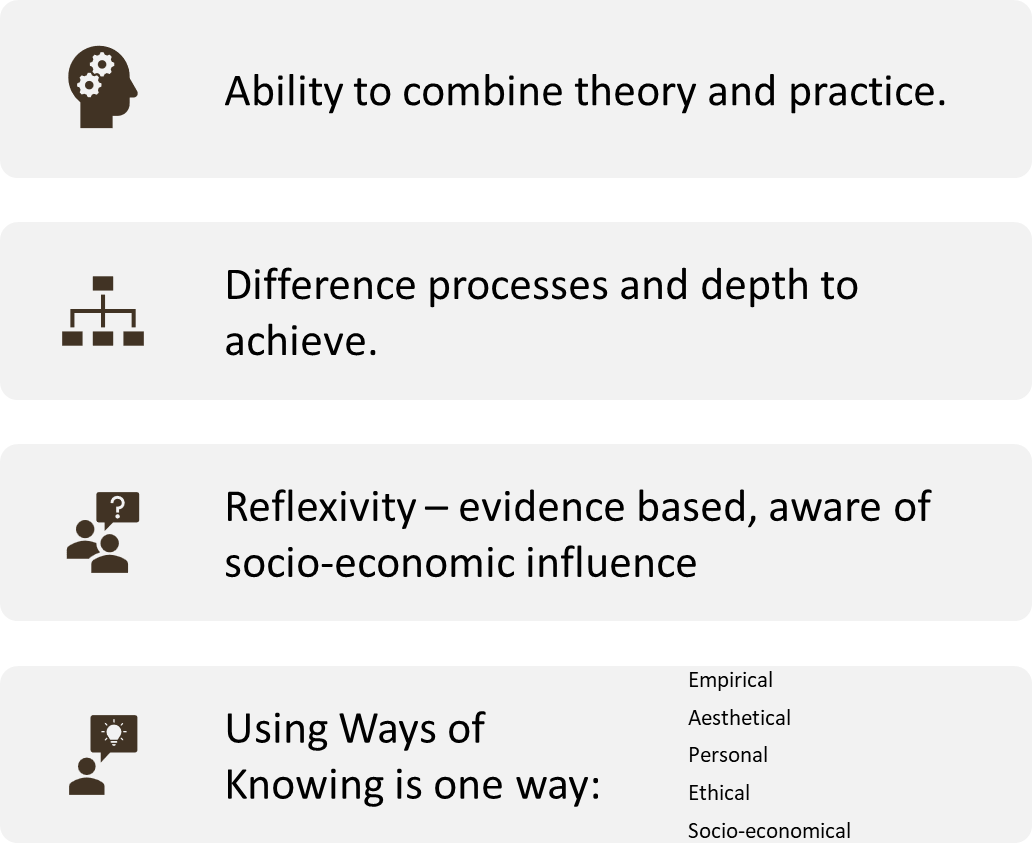
Carper’s Ways of knowing in Nursing
Patterns of knowledge that include:
1.Empirical science,
2.Ethical
3.Personal,
4.Aesthetic, and
5.Sociopolitical knowledge
EEPAS
Value 1
1.1 Nurses respect the inherent dignity and autonomy of all people
1.2 Nurses promote the autonomy and self-determination rights of all people
1.3 Nurses respect client’s preferences and choices through compassionate and ethical conduct
1.4 Nurses uphold the rights of all people to be free from violence
Code of Ethics and Rights of Indigenous Peoples
4.1 Nurses Uphold the Pursuit of Truth and Principles of Reconcilation
§Nurses understand Indigenous people have the right to self determination, self government and human rights.
Human Rights and Health
1.Human rights violations can directly impact a person’s health
2.Violations which impact social, cultural, economic opportunities increase vulnerability to illness
3.Programming that doesn’t consider human rights (or violates human rights) may result in discrimination
Code of Ethics and Human Rights 1
1.1 Nurses respect the inherent dignity and autonomy of all people
Code of Ethics and Human Rights 2
1.4 Nurses uphold the rights of all people to be free from violence:
Code of Ethics and Human Rights 3
5.1 Nurses respect the principles of social justice and social determinates of health to influence health for all people
Macro-Level Othering: Structural
§Conditions for structural othering: organizational culture, work environment and constraints, institutional policies and practices
§People who do not fit into the structures of the system are othered
“difficult to deal with’
“need different care”
Dignity
To feel worth
To treat with humanity
To recognize each person as a unique being
Nurses carry dignity for others and dignity for self and profession
Absolute/Relative Dignity
•Absolute Dignity: inherent, values such as responsibility, freedom, duty, and service.”
•Relative Dignity: bodily, external, esthetic dimension and a physical inner ethical dimension…changeable and is influenced by internal and external factors”
Dignity as Resource
Dignity promotes health and helps to restore health during vulnerability
Dignity as Distinction: individualized attending to the person; accepting the person as a unique and complete person
Dignity as Influence and Participation: support people to be able to participate in their own health and life
Value 1
Nurses promote the autonomy and self-determination rights of all people
Respect the right of individuals to make decisions based on informed consent, within their capacity
Respect the rights of clients to participate in decision making even when rights are limited by law (incapacity)
Nurses provide information and resources to support informed consent
Recognize power differentials that may influence informed consent
Informed Decision-Making
an individual’s right to sufficient information to make decisions about care, treatment and involvement in research.
Consent
The following elements are required for informed consent to be valid
•Capacity to consent:
•Information:
•Voluntariness:
Mature Minors
§The age of majority is 18 years (SK). There is no stipulated age of consent for treatment.
§A person under 18 years of age who is assessed and deemed capable of consenting to treatment (a mature minor) is allowed to make treatment decisions.
§Any person 16 years of age or more who has capacity to make a health care decision can make a directive.
§Age of consent for sexual activity in Canada = 16 years
Informed Consent and Nursing
§Obtaining informed consent is not USUALLY a nursing duty.
§We may WITNESS a signature, but do not legally assume the duty of providing all the information.
§We must ensure that the patients UNDERSTAND!
Implied Consent
“Nurses ensure that nursing care is provided with the person’s informed consent” (CNA, 2017, as cited in P & P, ch. 10)
CRNS & Substitute Decision Maker
§RNs are accountable and accept responsibility for their own actions and decisions, and utilize the Code of Ethics.
§RNs advocate for client’s rights and ensure informed consent, guided by legislation, practice standards and ethics
§RNs assess understanding of informed consent and implement actions when the client is unable to provide informed consent, including involving the involving substitute decision-makers
§RNs demonstrate knowledge of a substitute decision-maker’s role
§RNs, along with other health care providers and substitute decision-makers, consider and respect the best interests of the person and wishes or advance care planning
§Document who the SDM is and decisions made by SDM
1.3 Nurses respect client’s preferences and choices through compassionate and ethical conduct
§Professional obligation to provide care compassionately and ethically
§Support all people to live and die with dignity, work to relieve pain and suffering
§Nurses reflect on moral values and beliefs which are in conflict with a person’s decisions (ex: MAID, abortion care, harm reduction)
§Nurses inform the employer if there is a conflict
§Nurses must ensure the best interest of the client is protected until alternative care is available.
(CNA, 2025)