R2
1/254
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
255 Terms
FEV1
how much air can be forcefully exhaled in one second
FEV1/FVC
percentage of total air capacity
What is intermittent asthma (STEP 1)?
daytime ≤2 days per week
nighttime ≤2x per month
SABA use is ≤2 days per week
no activity limitations
FEV1 > 80% predicted
FEV1/FVC normal
0-1 per year exacerbations
What is Mild persistent asthma (STEP 2)?
daytime >2 days per week/ not daily
nighttime 3-4x per month
SABA use is >2 days per week/ not daily; or >1x/day
minor limitations
FEV1 > 80%
FEV1/FVC normal
>2 per year exacerbations
What is Moderate Persistent asthma (STEP 3)?
daytime daily
nighttime >1x/week but not nightly
SABA use is daily
some limitations
FEV1 = 60-80% of predicted
FEV1/FVC reduced 5%
≥2 per year exacerbations
What is severe persistent asthma (STEP 4)?
sx’s throughout day
nighttime 7x/week
SABA use several times per day
extremely limitations
FEV1 = <60%
FEV1/FVC reduced >5%
>2 per year exacerbations
With each follow up visit, what should be done?
inhaler technique
priming and cleaning technique
step up maintain or step down
Vaccines for asthma?
flu
Pneumovax 23 (age 2-64)
How often would you have to use the SABA in order to indicate worsening asthma control?
>2 days per week
Asthma triggers
smoke, pollution, SO2, NO, high humidity, exercise (EIA), irritants, emotion, upper respiratory infection (URI), Cold air, GERD, aspirin (ASA), NSAIDs
Asthma cascade
Exposure to allergens or irritants triggers the inflammatory cascade involving a variety of inflammatory cells
Inflammation leads to bronchoconstriction, hyper responsiveness, edema of the airways
Leads to limited airflow
Asthma cascade image
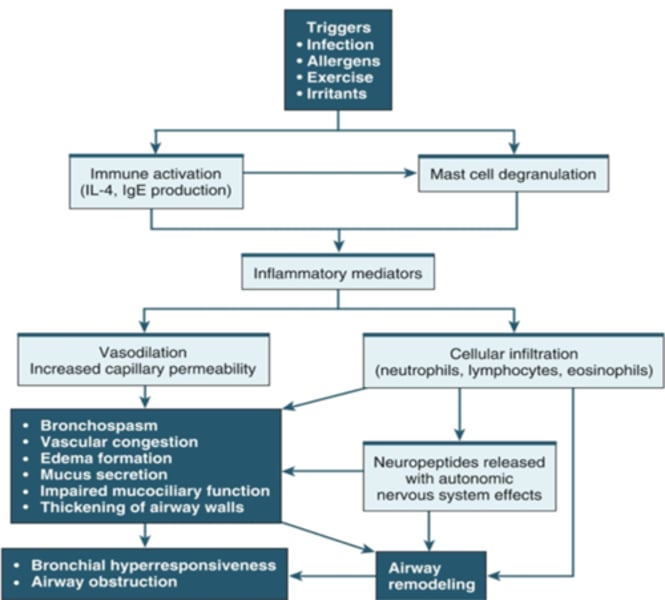
Inflammatory mediator effects
Blood vessels vasodilate, increased capillary permeability (runny nose)
Nerve cells (itching)
Smooth muscle cells (bronchial spasms and narrowed airway)
Goblet cells (mucus production)
Inhaled Corticosteroids (ICS) clinical effect
Reduce inflammation in the lumen
Early phase response - Asthma
30 to 60 minutes after exposure to Allergen/irritant
Mast cells release inflammatory mediators
Leukotrienes, histamine, cytokines, prostaglandins, nitric oxide
Increase mucus prouction, vasodilation an vascular permeability begins
o Increased permeability can cause edema, thickening and narrowing airway wall
o Can also compromise epithelial integrity, reduce mucus clearance, promote formation of exudative plugs
Late phase response - Asthma
4 to 6 hours after initial attack
Cytokine production (epithelial cells, Th2) d/t T cell activation
Recruitment of eosinophils, CD4+ T cells, basophils, neutrophils, and macrophages;
less intense bronchoconstriction while increase in airway hyperresponsiveness and airway inflammation and further edema
Airway remodeling
Structural changes in the broccchial walls from chronic inflammation
Changes include fibrosis, smooth muscle hypertrophy, mucus hyper secretion, Angiogenesis
Progressive loss of lung function not fully reversible, results in persistent asthma
Drug therapy
1) SABA - short acting beta adrenergic agonist - albuterol
2) LABA - Long acting beta to adrenergic agonist - corticosteroids - salmeterol
3) methylxanthines
4) anti-cholinergic (used more with COPD)
5) leukotriene modifiers - montelukast
6) Monoclonal antibodies - anti IgE
7) oral corticosteroid (OCS)
SABA - short acting beta adrenergic agonist
Simulate beta 2 receptors and bronchioles to produce Bronchodilation
Onset in minutes, duration 4 - 8 hours
Most effective for acute bronchospasm
Can be taken as a preventative for exercised induced asthma
LABA - Long acting beta adrenergic agonist
Inhaled
Effects in 30 minutes and last for over 12 hrs
Used daily to control asthma, not for acute attacks
Taken twice daily
Use for one to two weeks from maximum effect
THE MOST EFFECTIVE FOR LONG TERM CONTROL
LABA ARs
tremor, nervousness, h/a dry mouth, dry cough nausea, throat irritation
Symptoms can be reduced using a spacer and gargling after admin
Anticholinergics clinical effects
Promotes bronchodilation by preventing muscle around bronchi from tightening
Less effective than SABA
not used in regular management, use for severe acute attack
Leukotriene modifiers
Prophylactic use, produce both bronchodilator and anti-inflammatory effects
Not for acute attacks
Monoclonal antibodies
Prevents IgE from attaching to mast cells preventing release of chemical mediators.
Subcutaneous admin every 2 to 4 weeks for moderate to severe asthma
AR - risk for anaphylaxis
Characteristics of asthma
Lower airway disorder negatively impacts oxygenation, ventilation, gas exchange
Chronic and progressive
Obstructive pulmonary disease, results in air trapping
Diagnosis
History, physical, spirometry, pulmonary function test, chest x-ray, pulse symmetry, arterial blood gases (ABGs)
symptoms alone can be used to diagnose
pulmonary function tests (PFTs)
battery of studies/maneuvers. Measuring the ventilation mechanics of the lungs: airway function, lung volume, and the capacity of the lungs to exchange oxygen and carbon dioxide efficiently
Asthma related to allergy symptoms
May include:
Signs of chronic rhinitis, nasal edema, nasal polyps, rhinorrhea, oropharyngeal erythema
Risk factors
Genetics
Atopy - genetic predisposition to develop IgE-mediated response to common allergens
Immune response - babies immune system must be conditioned to function properly, exposure to microbes
Asthma Impairment criteria
Frequency of symptoms
Night time awakenings
SABA use for symptoms
Interference with normal activity
Lung function
PEFR (peak expiratory flow rate)
Shows the amount and rate of air that can be forcefully breathed out of the lungs.
Treatment for mild to moderate asthma
Inhaled bronchodilators and oral corticosteroids
Monitor vital signs
Outpatient monitoring
Follow up with healthcare provider
Severe attack symptoms
Alert and oriented but focused on breathing
Tachycardia, tachypnea (breath greater than 30 a minute)
Accessory muscle use, sits forward, sniffing position
Wheezing
PEFR Less than 50% predicted or personal best
Recurring symptoms interfere with ADLs
Feeling of impending doom
Silent chest
Severe attack treatment
Emergency department, hospital admission
Supplemental O2 and oximetry
PaO2 greater than 60 mmHg or O2 sat below 93%
Monitor PEFR, ABGs, vital signs
Bronchodilators, oral corticosteroids
LAMA
Long acting muscarinic antagonist
Final step 5 in GINA treatment protocol of asthma
ICS-formoterol place in threapy
As needed: offers a therapeutic alternative to maintenance low-dose ICS plus SABA
Maintenance and reliever therapy (MART)
Budesonide/formoterol
Low dose ICS
Markedly reduces hospitalizations and deaths
Very effective in preventing severe exacerbations, reducing symptoms, improving lung function, and preventing exercise induced bronchospasm
Early treatment with ICS associated with better lung function if symptoms have been present for 2 to 4 years
Treatment follow up
Review response after 2 to 6 weeks then every 6 months if controlled.
Consider step down when asthma has been well-controlled for three months
In adolescence and adults ICS should not be stopped completely
Asthma action plan - green zone
Doing well: no symptoms, participate in usual activities,
peak flow results greater than 80% of personal best,
remain on medication
Action plan yellow zone
Cough, Wheeze, chest tightness or SOB; or
Waking at night d/t asthma; or
Can do Some but not all activitites
PEFR 60—79% of best
Action plan - red zone
Medical alert!
Symptomatic and medications not helping,
cannot do usual activities,
Sx’s are same or worsen after 24 h in yellow zone
PEFR < 50% of personal best.
Call the doctor now, ambulance, get to the hospital
Asthma and COVID-19
Not at a increased risk of acquiring COVID-19
Not at risk of severe COVID-19 if well-controlled mild to moderate asthma
If well-controlled not at increased risk of death
Death risk increased in people who recently needed oral corticosteroids (OCS)
There have not been increased asthmatic exacerbations during the pandemic
Fluticasone
Flovent HFA (MDI), Flovent Diskus (DPI)
ipatropium brand
atrovent HFA
salmeterol
Serevent Diskus
Tiotropium brand
spiriva
Umeclidinium/vilanterol
Anoro Ellipta
levalbuterol brand
xopenex HFA
albuterol brand
proventil HFA
ventolin HFA
Fluticasone/umeclidinium/vilanterol
Trelegy Ellipta
formoterol + budesonide brand
symbicort
Tiotropium/olodatero
Stiolto Respimat
beclomethasone brand
qvar redihaler
formoterol + mometasone brand
dulera
Glycopyrrolate/formoterol
Bevespi Aerosphere
Fluticasone/salmeterol
Advair Diskus, Advair HFA
B2 agonist MOA
increases cAMP which causes smooth muscle relaxation
anticholinergic MOA
decreases cGMP which causes smooth muscle relaxation
methylxanthine MOA
several MOA... thought to inhibit PDE III and PDE IV --> inc cAMP, inc CA++ influx, dec prostoglandins
corticosteroid MOA
inhibit inflammatory response
PDE 4 inhib MOA
inhibits PDE 4 --> inc cAMP which relaxes bronchial smooth muscle
ipratropium MOA
SA anticholinergic
albuterol MOA
SABA
Tiotropium MOA
LAMA anticholinergic
Umeclidinium MOA
LAMA anticholinergic
Glycopyrrolate MOA
LA anticholinergic
Levalbuterol MOA
SABA
Formoterol MOA
LABA
Salmeterol MOA
LABA
Theophylline MOA
methylxanthine
budesonide MOA
ICS
Fluticasone MOA
ICS
Methylprednisolone MOA
systemic CS
roflumilast MOA
PDE 4 inhib
Which LABAs have a 12hr DoA
salmeterol
arformoterol
formoterol
The inflammation and bronchoconstriction associated with asthma is reversible/irreversible
reversible
What 2 tests help diagnose asthma
spirometry
peak expiratory flow
Spirometry measures _____ and ____
Forced Vital Capacity
FEV1
What is Forced Vital Capacity
maximum volume of air exhaled after taking a deep breath
Bronchodilator reversibility is documented when FEV1 increases by more than ___% from baseline
12%
PEF is measured by what
Peak flow meter
With moderate and severe asthma severity, how much is FEV1/FVC reduced
at least 5% (greater than 5% in severe)
T/F
Exercise should be avoided as much as possible in pts with exercise induced bronchospasm
False
When a pt is using a SABA to control their asthma, when would you consider Stepping up therapy
if they need to use it >2day/wk
In addition to acute asthma symptoms, what else are SABAs used to control
exercise-induced bronchospasm (EIB)
Which drug class is the mainstay and taken on a daily basis to treat asthma
inhaled corticosteroids (ICS)
How should LABAs be used in treating asthma
in combo with ICS
NEVER used alone is asthma
Asthma Treatment Algorithm:
Step 1: Intermittent asthma
SABA prn
Asthma Treatment Algorithm:
Step 2: mild-persistent asthma
Daily low-dose ICS &PRN SABA
or
PRN concomitant ICS & SABA
Alt: Daily LTRA & PRN SABA OR cromolyn or theophylline & PRN SABA
Asthma Treatment Algorithm:
Step 3: moderate persistent asthma
Daily & PRN combo low-dose ICS formoterol
Asthma Treatment Algorithm:
Step 4: severe persistent asthma
Daily & PRN combo medium-dose ICS-formoterol
Alt: med dose ICS-LABA OR daily med dose ICS + LAMA, and PRN SABA, or daily med dose ICS + LTRA, theophylline, zileuton or same plus saba
Asthma Treatment Algorithm:
Step 5: severe persistent asthma
Daily med-high dose ICS-LABA + LAMA and PRN SABA
ALT: Daily medium-high dose ICS-LABA or dally high-dose ICS + LTRA. and PRN SABA
Asthma Treatment Algorithm:
Step 5
Daily high dose ICS-LABA + PO CS + PRN SABA
SABA MOA
B2 agonist--> bronchodilation
What are the SABAs
albuterol
levalbuterol
Side effects of SABA
nervousness
tremor
tachycardia/palpitation
dec K+
cough
rhinitis
nausea
SABA warnings
caution in:
CVD
glaucoma
DM
angina
Salmeterol BBW
inc risk of asthma related death; should only be used in pts who are on ICS
ICS common side effects
hoarseness, cough, sore throat, oral candidiasis (rinse mouth); pneumonia in COPD