airway management / mechanical ventilation
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
49 Terms
artificial airway...
emergency choice for insufficient airway
endotracheal tube
Placement of a tube into the trachea
• Oral
• Nasal
- 14 - 21 days of wearing
pts:
- comatose
- upper airway obstruction
- mechanical ventilation
- suctioning secretions
tracheostomy
surgical creation of an opening into the trachea through the neck
- permanent

Fenestrated tracheostomy tube
allows the patient to speak, breathe, or clear secretions from the upper airway.

non fenestrated tube
no holes in tube; air must go around tube to get to upper airway

tracheostomy complications
Tube obstruction
Tube dislodgement and accidental decannulation
laryngeal nerve damage
dysphagia
tracheoesophageal aphasia
tracheodilation and ischemia -> necrosis
Pneumothorax
Bleeding
Infection
tracheostenosis
- if dislodgment, cover the hole and bag the face
indications for tracheostomy
Long-term mechanical ventilation
Frequent suctioning
Protecting the airway
Bypass an airway obstruction
Reduce WOB
intubation
• Process of placing an endotracheal tube to provide a patent airway
• Preparation, sedation, paralysis
Nursing Role:
• Gather supplies/equipment
• Administer medications
• Monitor VS

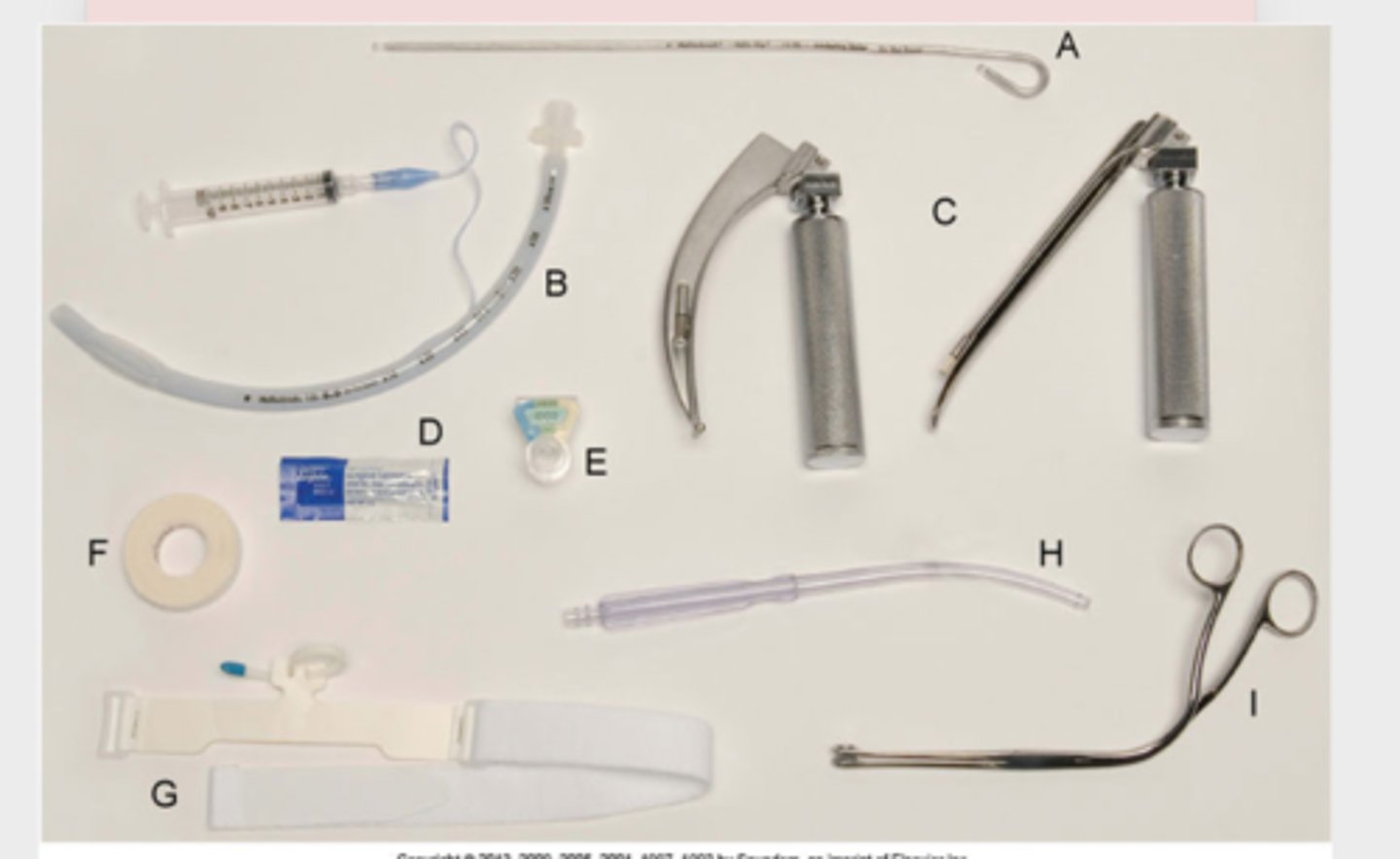
intubation equipment
- o2 flowmeter and o2 tubing
- suction apparatus
- suction catheter
- ambu bag !!!
- laryngoscope
- stylet (obturator for et tube)
- stethoscope
- tape
- syringe
- magil forceps
- towels for position
endotracheal tube cuff pressure
< 20-25 mmHg
< 25 cm H20
if ET cuff pressure if >25 mmHg
- ischemia
- bleeding
- pressure necrosis
if ET cuff pressure if <20 mmHg
- increased risk of aspiration pneumonia
- Longitudinal Folds
- ineffective ventilation
sedation medications
- FENTANYL
- MIDAZOLAM
- ETOMIDATE
- KETAMINE
- PROPOFOL (Diprivan)
PARALYTICS medications (-IUM)
- SUCCINYLCHOLINE
- CISTRACURIUM BESYLATE
- ROCURONIUM
- VECURONIUM
POST-INTUBATION CARE
- respiratory assessment
- secure tube
- proper ventilator settings
- humidified o2, monitoring CO2
- sedation and analgesics
- restraints
- assume all pts can hear you
- correct underlying problem
Oral care - mouth wash, moisturizing lips etc q 12 hrs
Suction PRN - pre and post oxygenation 2 mins
RIGHT AFTER INTUBATION, THE PHYSICIAN ASKS YOU TO LISTEN TO BREATH SOUNDS TO CONFIRM PLACEMENT. YOU HEAR BREATH SOUNDS ON THE RIGHT SIDE BUT NOT THE LEFT. WHAT DO YOU DO?
- might be down the right branch
- pneumothorax
- deflate the endotracheal tube cuff and carefully withdraw the tube by 1 cm
RIGHT AFTER INTUBATION YOU SEE ABDOMINAL MOVEMENT AND DISTENTION WITH EACH BREATH. WHAT DO YOU DO?
- in esophagus, at risk for aspirating
- remove the ETT and immediately begin ventilating the patient with a bag-valve-mask (BVM) using 100% oxygen
care of the patient with an ett
•Maintain tube
•Manage secretions
- semi-fowler's
•Oral care
•Skin integrity
•Foster communication and comfort
•Prevent complications
Suctioning Technique
- In-line (closed) suction catheter/Ballard
- lowest setting (80-120)
• Sustains PEEP
- ALWAYS USE SALINE, NOT WATER
• Pre-oxygenate before and after
Complications:
• Bronchospasms
• Trauma; suctioning too much
COMPLICATIONS FROM INTUBATION
• RESPIRATORY: penumothorax, subq air, trauma
• CARDIAC: bleeding, dysrhythmias,
• TRAUMA: airway
• INFECTION: pneumonia,
• TRACHEAL DAMAGE: vocal cord paralysis, ichemia/necrosis
MECHANICAL VENTILATORS
• Positive pressure breathing device
• Non-invasive (BIPAP) and invasive (ET TUBE)
Indications for mechanical ventilation:
- PaO2 <55 mm Hg
- PaCO2 >50 mm Hg and pH <7.32
- Vital capacity <10 mL/kg
- Negative inspiratory force <25 cm H2O
- FEV1 <10 mL/kg
mechanical manifestation indications for mechanical ventilation
- Apnea or bradypnea
- Respiratory distress with confusion
- Increased work of breathing not relieved by other interventions
- Confusion with need for airway protection
- Circulatory shock
- Controlled hyperventilation (e.g., patient with a severe head injury)
BIPAP
Bilevel positive airway pressure for respiratory support.

vital capacity
the maximum amount of air a person can exhale after taking the deepest possible breath
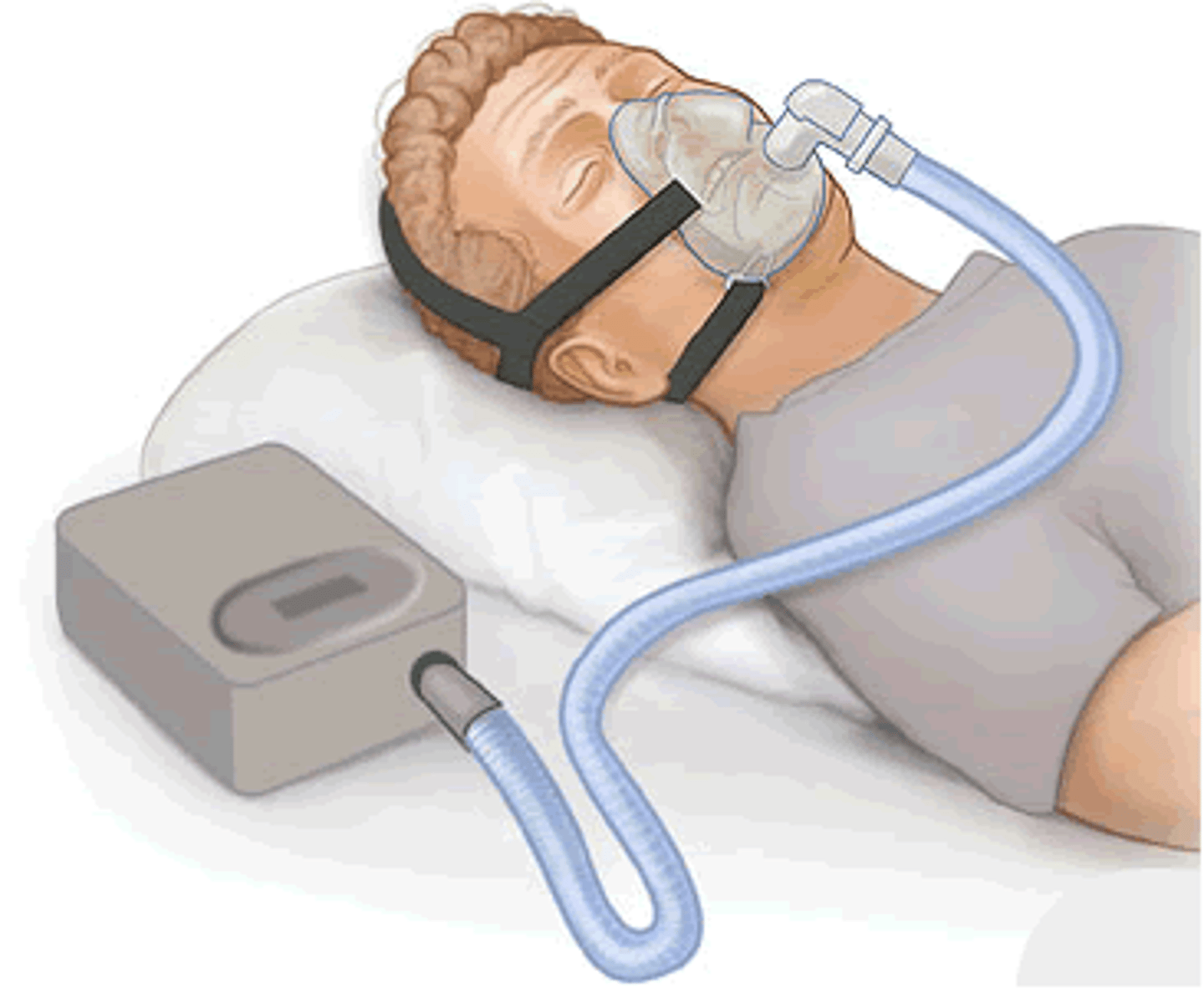
NONINVASIVE POSITIVE-PRESSURE VENTILATION
CPAP/BiPAP
• Given via facemasks
• Decrease the work of breathing
• Decreases risk of nosocomial infections
• Best mode: pressure-controlled
BiPAP indications and contraindications
indications:
- acute or chronic respiratory failure
- acute pulmonary edema
- COPD
- chronic heart failure
- sleep-related breathing disorder
contraindications:
- HX of respiratory arrest
- serious arrythmias
- cognitive impairment
- head/facial trauma
CPAP (Continuous Positive Airway Pressure)
Single positive pressure to airways during respiratory cycle
- Used with mechanical ventilation or leak-proof mask
- Obstructive sleep apnea
BIPAP (Bilevel Positive Airway Pressure)
Pressure during inspiratory and expiratory
- first step before ventilation
- Oxygenation and ventilation
- Back-up rate
º Most common uses:
- severe COPD
- sleep apnea
PEEP
Positive pressure at the end of exhalation to keep alveoli open; good for ARDS
• Maintains recruitment
• Improves oxygenation
• *The higher the PEEP, the greater the risk for acute lung injury and decreased venous return; pneumothorax, tension pneumothorax

VENTILATOR MODES
º Controlled Modes (CMV):
• Pressure Control
• Volume Control
º Support Modes:
• Pressure Support/CPAP
º Combination Modes
• SIMV
(CMV) PRESSURE CONTROL CONTINUOUS MANDATORY VENTILATION
• Set pressure
• Set respiratory rate
• Tidal volume varies
(CMV) VOLUME CONTROL CONTINUOUS MANDATORY VENTILATION
• Preset tidal volume
• Preset respiratory rate
• Pressure varies
• Tidal volume is based off patient's ideal body weight
• 6-10 mL/kg
(COMBINATION) SIMV (SYNCHRONIZED INTERMITTENT MANDATORY VENTILATION)
• Preset tidal volume
• Set respiratory rate
• Patient can breathe spontaneously with no assistance
(SUPPORT) PSV/+CPAP (PRESSURE SUPPORT VENTILATION)
• Weaning mode / spontaneous breathing trial
• Patient initiated breaths
• Set pressure, low PEEP
• Back-up mode and rate set
• ***HAVE TO BE Off sedation!
HIGH PRESSURE VENTILATOR ALARMS
• Coughing
• Occluded airway
• Tubing kinked
• Fighting the ventilator
• Decreased lung compliance
• Pneumothorax, atelectasis, bronchospasm
LOW PRESSURE VENTILATOR ALARMS
• Leak in ventilator tubing
• Disconnected circuit
• Extubation
• Alarm fatigue
MY PATIENT IS ON 100% FIO2 AND KEEP DROPPING THEIR SATS INTO THE LOW 80'S. WHAT DO I DO?
- suction
MY PATIENT HAS ORDERS TO BE ON BIPAP, AND THEIR BREAKFAST TRAY IS HERE. WHAT DO I DO?
- You should not allow the patient to eat or drink anything while using BiPAP, as they might inhale food or liquid into their lungs.
depends on patient, ask respiratory therapist
COMPLICATIONS FROM MECHANICAL VENTILATION
• Decreased cardiac output
• Barotrauma
• Pneumothorax
• Infection
• Delirium/psychosis
• Loss of mobility
• Ventilator dependence
WEANING
• A process of withdrawing the patient from the ventilator
• Physiologically/hemodynamically stable
• Demonstrates spontaneous breathing capability
• Recovering from acute medical problems
• Respiratory failure is sufficiently reversed
• Look at the patient as a whole!
• Patient/family preparation
What amount of FiO2 should my patient be on when weaning?
- 21-25%
- gradually reduces until PaO2 is 70-100%
What is the lowest amount of FiO2 on a mechanical ventilator when weaning?
- 21-25%
Why should I pay attention to my tidal volumes during weaning?
reflects a patient's ability to take sufficiently deep breaths; patients with low aren’t able to breathe as sufficiently
patients that aren't breathing adequately:
- tachypnea
- tachycardia
- reduced tidal volumes
- decreased oxygen saturation
what to do when a patient self-extubates?
- assess, if they need artificial airway, start bagging and call for help
- vital signs, respiratory effort
- assess stridor (upper airways) and oxygenation needs
WHAT DOES MY PATIENT LOOK LIKE IF THEY ARE NOT TOLERATING WEANING?
put patient back on SIMV
- if completely stop breathing, then pressure control/ventilation control
- then putting them back to sleep if it's the worst
- epinephrine breathing treatment
patient self-extubating complications:
- closely monitor for 12 hours if stable.
- consider frequent airway suction, NPO
- hypoxemia
- bradycardia
- hypotension and death
patient self-extubating prevention:
- RESTRAINTS
- sedation
- making sure ballard is above head
EXTUBATION
• Humidified oxygen through facemask once the endotracheal tube is out
• Monitor respiratory status; stridor and dyspnea
• Get your patient to talk
• high-fowlers will help with expansion and secretion removal
• NPO UNTIL CLEARED BY SPEECH
• Educate