Gram-negative curved bacilli & Coccobacilli
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
80 Terms
What’s a common feature among curved rods?
They’re all Oxidase +
What are the morphological and motility characteristics of V. cholerae
→ Gram-negative, slender bacilli, comma-shaped
→ Darting motility (Vibrio = Vibrate) - Long polar flagellum
How is V. Cholera transmitted?
*Fecal oral route:
→ Food (Shellfish) - Fecally-contaminated water
Describe cholera symptoms
Acute diarrheal disease:
Rice water stools
Dehydration
Hypovolemic shock
Metabolic acidosis
What is the ID50 of Cholera
1011 Cell/mL
What can decrease cholera ID50
If someone has lowered stomach acid (antiacid or PPI) - Vibrios are very sensitive to stomach acid
What are cholera’s virulence factors
Cholera toxin CT
Toxin-coregulated pilus (Type IV pilus for adhesion)
Describe Cholera toxin’s mechanism
It’s a classic AB toxin: B for tropism/ A for activity
Endocytosis → Adenylyl cyclase → cAMP → Cl- and Na+ efflux
What kind of specimens are taken to screen for cholera
Stool samples or mucus flakes BEFORE GIVING ANTIBIOTICS
Morphology and Characteristics of Vibrio cholerae?
Gram-negative, curved bacilli
Non-sporing, non-capsulated
Facultative anaerobe
How is V. cholera cultured
It requires an aerobic alkaline culture medium (pH<8):
Bile Salt Agar (BSA)
Thiosulfate Citrate Bile salts & Sucrose Agar (TCBSA)
Monsur’s Gelatin
Taurocholate Trypticase Tellurite Agar (GTTA)
Vibrio cholera biochemistry
Oxidase + (Rare case of Oxidase-positive sugar fermenters, oxidase negative would otherwise suggest E. Coli/ shigella/ Salmonella)
Suc +
Lac + (late fermenter)
String test +
Uses 0.5% Deoxycholate (a bile salt), which can lyse Vibrio cholerae’s cell wall, which will cause DNA to leak out and give a stringy texture
Cholera Red Reaction +
Peptone water (contains Trp + NO2-) + H2SO4→ V. cholerae should metabolize Trp to indole: Indole + NO2- + H2SO4 → Red coloration
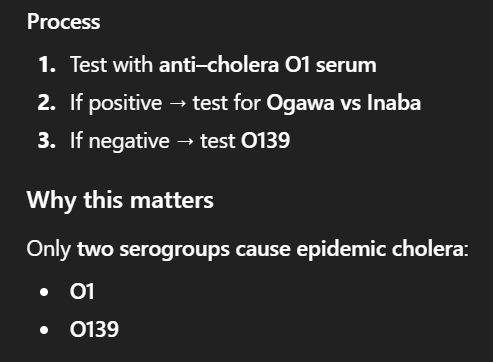
Side agglutination with cholera O subgroup then test for serotypes, cuz only O cause disease (Check image)
Immobilization test using antiserum same concept as agglutination
Phage typing
Vibrio cholera Prophylaxis and treatment
Prophylaxis: Oral vaccines - Immunity for 6-12 months
Treatment: Oral rehydration fluid, antibiotic therapy SECONDARY importance
Vibrio Vulnificus characteristics
G- curved bacillus found in marine environments
Vibrio vulnificus clinical significance
It can cause severe wound infections or septicemia due to exposure to contaminated sea water → Cellulitis that can progress to NF in high-risk patients (Liver disease: Cirrhosis, hemochromatosis)
May require surgical debridement
Campylobacter jejuni characteristics
Curved or spiral-shaped (S-shape) with polar flagella
Campylobacter jejuni biochemistry + Optimal growth conditions
Oxidase +
Microaerophile
Grows best at 42C
Campylobacter jejuni incubation period
2-5 days
Campylobacteriosis symptoms
Bloody diarrhea (Especially in children)
Abdominal cramps
Malaise
Fever
Nausea and vomiting
Usually self-limiting
Campylobacter sources
Raw or undercooked meat and poultry, water, unpasteurized milk, contact with animals (dogs/cats/pigs)
Campylobacteriosis Complictions
GBS (Some serotypes more than others)
Septic arthritis
What is the carriage rate for H. pylori
50% of world population asymptomatically
What exactly does H. pylori colonize
Mainly the antrum of the stomach → Peptic ulcers
What is the probability of carriers developing peptic ulcers
5-10%
Peptic ulcers are risk factors for what conditions?
Gastric adenocarcinoma (1%)
MALT lymphoma (0.1%)
→ First infectious agent associated with cancer development
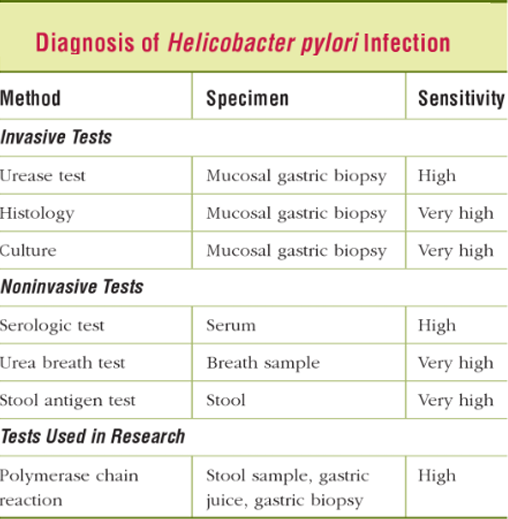
What are some histological diagnostic methods for H. pylori
After gastric biopsy, and transport of media at 4C (very fragile), we can do:
Giemsa (Sensitive & Inexpensive)
Steiner or Warthin-Starry stain (More sensitive but expensive)
Immunohistochemistry
H. pylori culture
Less reliable
H. pylori is quite fastidious, but can be grown on Chocolate Agar (Microaerophilic conditions) and takes about 10 days to grow
Discuss H. pylori serology
We can get positive IgG at ~3 weeks post-infection
However, we can’t differentiate between recent, ancient, and even cured infection (ABs persist after triple therapy)
In pediatrics, we often do stool Ag detection instead of PCR
H. pylori biochemistry
Ox +
Cat +
Urease +++
What non-cultural, non-serological, and non-histological tests can we also use
Molecular → RT-PCR on biopsies and stools
Urease rapid test on biopsies→ 80% Sensitivity, 95% Specificity
13C-Urea breath test → Sensitivity and specificity both >95%
*Note: Must stop TTT treatment before doing urea test (Mainly PPI, it is well-known to reduce sensitivity)
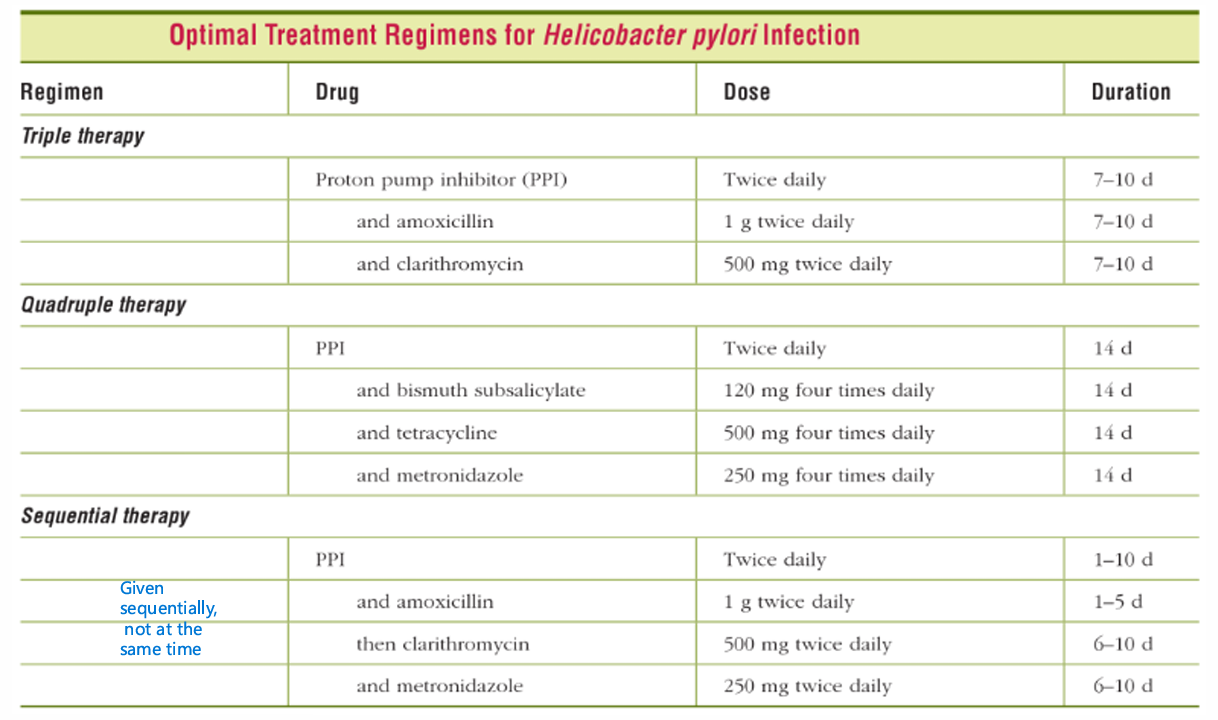
H. pylori Treatment
Triple therapy: PPI + Amoxicillin or Metronidazole (If allergy) + Clarithromycin
Bismuth-based quadruple therapy (When concerned about macrolide resistance)
Fluoroquinolones, Tetracycline, Rifampicin
What are Parvobacteria
Gram-negative, pleomorphic bacteria
These bacteria are usually fastidious and require enriched media for isolation: Blood or chocolate agar
THEY ALL STAIN POORLY IN GRAM STAIN
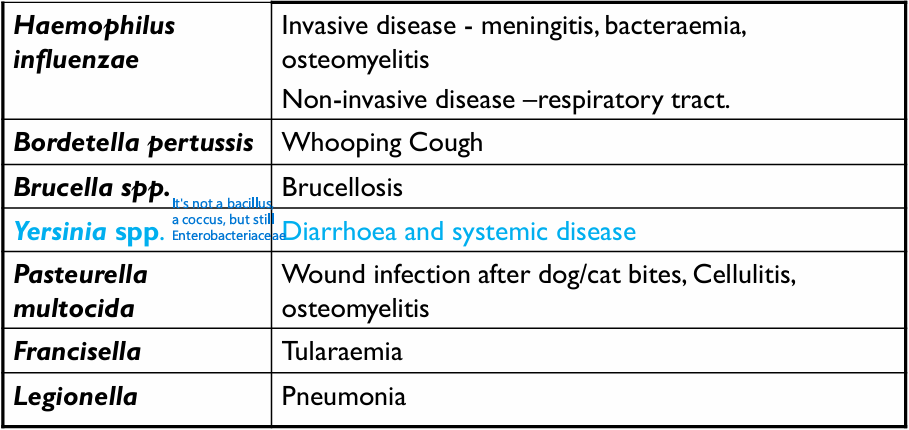
Discuss H. influenzae’s Habitat/ Transmission/ Virulence factors
Habitat: Normal flora of URT and Vagina
Transmission: Respiratory droplets
Virulence factors: Capsule, IgA protease
How do we classify H. influenzae
They are classified according to whether or not they are encapsulated, and if they are encapsulated, then there are 6 capsule types to differentiate between: a to f
What clinical pictures are capsulated strains of H. influenzae’s mostly associated with?
Capsulated strains mainly infect children from 2 months to 3 years of age
Hib specifically can cause meningitis, pneumonia, sepsis, and epiglottitis
Note: Epiglottitis can have a “Cherry red” appearance in children, and a “Thumb sign”
What clinical pictures are unencapsulated strains of H. influenzae’s mostly associated with?
Unencapsulated-Nontypeable H. influenzae are the most common cause of mucosal infections → Otitis Media, Conjunctivitis, Bronchitis
They are also associated with invasive infections
What can other Hemophilus serotypes cause?
H. aegyptius can cause conjunctivitis “pink eye”
H. ducreyi can cause Chancroid
1) What are the treatment guidelines for H. influenzae:
Mucosal infections
Meningitis
2) H. influenzae Prophylaxis
1) * For mucosal infections, treat with Amoxicillin +/− Clavulanic acid.
* For meningitis, Ceftriaxone
2) Give Rifampin for post-exposure prophylaxis
Describe the available vaccines for H. influenzae
We only got the Hib vaccine; it contains Hib’s capsular polysaccharide conjugated to diphtheria toxoid
→ Given between 2 and 18 months of age
How do we culture H. influenzae?
We can either use CSF or blood samples and directly culture them on Blood or Chocolate Agars
* CSF if meningitis suspected (Hib)
* Blood if patient is positive for laryngoepiglottitis, or pneumonia
How do we make the culture medium for H. influenzae more selective?
We add bacitracin to CA, it inhibits many G+ URT bacteria
What are some unique tests that we can use to identify H. influenzae
Satellitism: If you streak S. aureus across a BA or CA, it will provide Factor V, which will help enlarge H. influenzae colonies
X&V: Add factors X and V, they favor H. influenza growth
Describe the basic characteristics of Bordetella, brucella, and francisella
They’re extremely small, Gram-negative, aerobic, non-fermenter (OxidizersName ) coccobacilli, true pathogens (isolation always associated with disease)
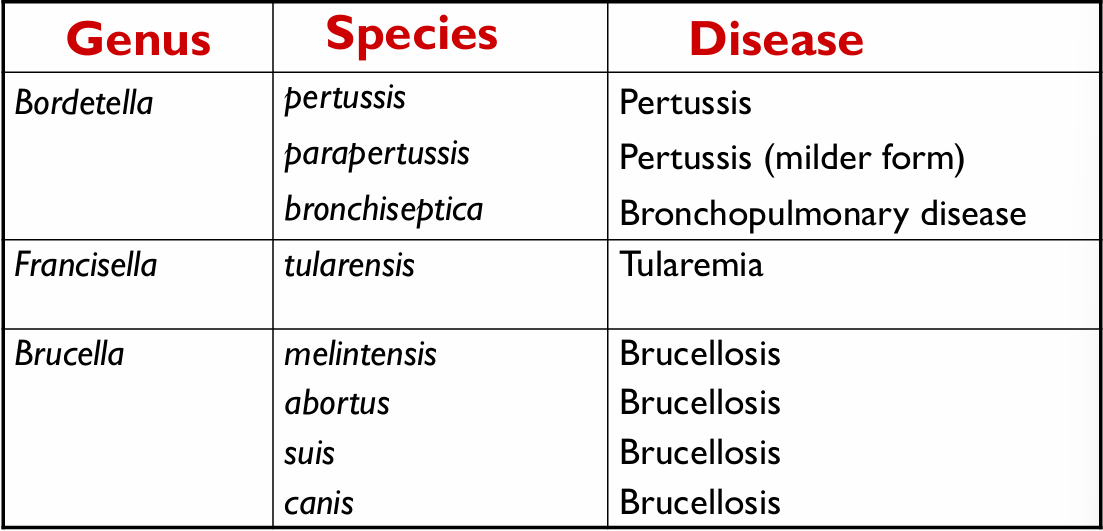
Name all the bordetellas, fracisellas, and brucellas and the diseases they are associated with
Bordetella pertussis: habitat & reservoir, transmission, virulence factors
Habitat & Reservoir: Commensal of the human respiratory tract, healthy carriers are reservoirs - Childhood disease.
Transmission: Direct contact - Respiratory droplets and aerosols
Virulence factors: Pertussis toxin (toxoidable)
What does the pertussis toxin do?
It destroys and dislodges ciliated epithelial cells → Whooping cough
It activates adenylate cyclase by inactivating Gi, the inhibitory subunit
Describe the pertussis cough
Hacking coughs followed by abrupt deep inhalation (Whoop)
Describe the progression of pertussis
Catarrhal stage: Low grade fever, coryza - MAX infectivity
Paroxysmal stage: Whooping cough stage *Note: In adults, causes “100-day cough”
Convalescence stage: Gradual recovery
Lymphocytosis in Catarrhal and paroxysmal stages
Bordetella pertussis specimen and culture
Specimen: Postnasal or Prenasal swab
Culture: Cough plate method/ Charcoal BA (Cephalexin)/ Regan-Lowe agar/ Bordet-Gengou medium → “Split pearls” or “mercury drops” colonies
B. Pertussis treatment and prevention
Treatment
Macrolides, but use TMP-SMX if allergic
Prevention
Tdap - Full strength (teens and adults)
DTaP - Reduced dose (Infants & children)
Legionella pneumophila morphology
Thin, non-capsulated, Gram-negative coccobacilli
Stains poorly (Like most parvobacteria → Use silver stain)
Legionella pneumophila: Habitat, transmission, outbreaks, and diseases
Habitat: Water (air conditioners, cooling systems, and hot water tanks)
Transmission: Contaminated aerosols - NO PERSON-PERSON transmission
Outbreaks: Cruise ships and nursing homes
Diseases:
Legionnaires’ disease: Severe atypical pneumonia (Unilateral lobar pneumonia), fever, GI, and CNS symptoms
Pontiac fever - Mild- flu-like
What are the risk factors for developing legionnaires’ disease over Pontiac fever
Older age, tobacco smoking, chronic lung disease
What kind of immune-evasion mechanisms does legionella have
It can form biofilms (Inside and outside the body), and it can also prevent the fusion of phagosomes with lysosomes in macrophages
Describe Legionella pneumophila diagnostics
Culture: Charcoal yeast extract buffered with iron and cysteine medium
PCR
Detection of ANTIGEN IN URINE
*Note: Labs may show hyponatremia
Treatment for legionella
Macrolides or quinolones
Francisella tularensis appearance
Gram-negative coccobacilli with bipolar staining - Safety pin appearance
What does Francisella tularensis cause?
A plague-like disease of rodents and other small mammals (Rabits, - Reservoirs |||| Ticks and deerflies→ Vectors)
Francisella tularensis treatment
Charcoal yeast extract buffered with iron and cysteine medium
Francisella tularensis treatment
Streptomycin and gentamicin
Francisella tularensis prevention
Avoid insects
Live-attenuated vaccines administered by multiple skin punctures (Like if grass was many needles)
Pasteurella multocida appearance
Gram-negative, nonmotile, coccobacillus
How is Pasteurella multocida transmitted
Through bites and scratched, especially the ones caused by dogs and especially cats.
What clinical manifestations can Pasteurella multicoda cause?
Clinical manifestation depends on the infection site:
Animal bite or scratch: Soft tissue infection (Majority and potentially dangerous)
Can cause rapidly developing cellulitis at the infection site
Chronic local infection
Osteomyelitis
Nasopharyngeal colonization → Infection (Less common)
Laboratory identification of Pasteurella multicoda
Culture
Charcoal yeast agar with buffered cysteine and iron
Small, translucent, non-hemolytic colonies on blood agar
Blood smear
Bipolar staining on blood smear
Pasteurella treatment
Penicillin (P for Pasteurella)
Responds well to many drugs tho
What’s another name for brucellosis
Malta fever
Name the Brucellas and their source
B. abortus - mainly cattle
B. melitensis - sheep & goats
B. suis - pigs
B. canis - dogs
B. melitensis is the most common one worldwide
Brucella is Zoonotically-transmitted, but how exactly?
Brucella is concentrated in animal milk, urine and genital organs.
Transmission:
Orally through unpasteurized milk and raw milk or meat products
Skin → Through abrasions (Farmers and Vets)
Respiratory in lab workers
Conjunctival/ Blood transfusion/ person to person
Note: Possible transplacental transmission
Describe Brucella’s infection process
Very similar to viruses
Entry through mucosas → Macrophage activation and phagocytosis → Intracellular multiplication → Spread to Reticuloendothelial organs through lymphatics → Spread to blood → Spread to any organ
*Note: Forms noncaseating granulomas (Non-necrotic - No white necrotic center)
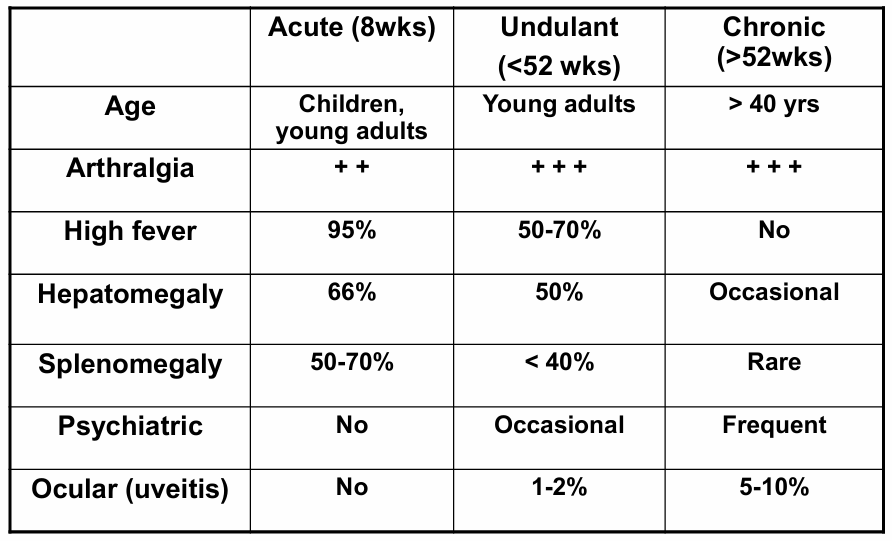
Compare the clinical manifestations of acute, undulant, and chronic brucellosis
Main takeaways from the table
More acute if younger the patient, more chronic the older the patient
Arthralgia in all but more in chronic
Fever associated with acute, and undulant fever is undulant -No chronic
No Hepatomegaly in chronic
Rare splenomegaly in chronic
Psychiatric symptoms more common with chronic
More common ocular symptoms the more chronic
What can you find on a blood test of a patient with brucellosis
We will notice monocytosis, which is characteristic of chronic infections unlike leukocytosis for most acute infections
What are the culture techniques used for brucella?
It usually takes a lot of time (4 weeks), however, BACTALERT, an automated medium, can culture in 2-8 days
Mostly Blood culture, however, we can also do CSF, LN, BMI, pus, synovial fluid
Can we use serology to diagnose Brucella?
Yes, it’s the main diagnosis method (Can also do PCR)
→ Serum agglutination tests for IgG, IgM, and IgA
What is the standard for brucellosis treatment
Doxycycline + Rifampin or Streptomycin
Doxycycline is important cuz brucella can be IC
What are the risk factors for brucellosis relapse
Male se
Inadequate antibiotic treatment
Thrombocytopenia
Describe Gardnerella Vaginalis’s general characteristics
Gram-variable, facultative-anaerobic, non-motile, rod
Describe how Gardnerella vaginalis causes bacterial vaginosis
BV is not an STD but it is common in women who have a lot of sex:
Frequent exposure of the vagina to alkaline pH results in loss of Lactobacillus → further ↑ vaginal pH (>4.5) → Gardnerella-centered anaerobic, polymicrobial biofilm (Allows for Moblincus and Prevotella overgrowth) → amine production causing odor and discharge (fishy odor)
What are the diagnostic methods for BV
Amine-whiff test - Mixing discharge with 10%KOH enhances the fishy odor
Papanicalou test:
Normal: reveals Doederlein bacilli (Lactobacilli)
BV: Reveals cells with stippled appearance along outer margin, Doerderlein bacilli will not be found in BV
What’s the standard treatment for BV?
Metronidazole or clindamycin