L11 AN2102 -Pelvic Organs II – Ovaries, Tubes, Uterus, Vagina, Blood, Innervation, Ectopic
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
58 Terms
What are the two functions of the ovaries?
• Exocrine – release of oocytes (≈1 every 28 days)
• Endocrine – secretion of estrogen and progesterone
Are the ovaries intraperitoneal or retroperitoneal?
Intraperitoneal, but most of the ovary is not covered by peritoneum.
Why is most of the ovary not covered by peritoneum?
So ovulation is not blocked — the oocyte must be released freely.
What does the ligament of the ovary connect?
The ovary to the uterine horn.
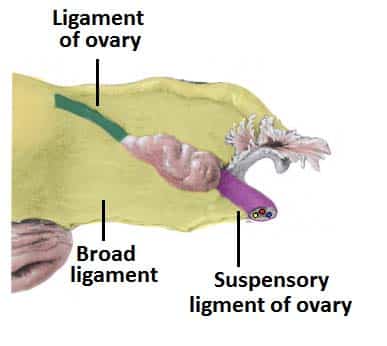
What travels inside the suspensory ligament of the ovary?
• Ovarian artery
• Ovarian vein(s)
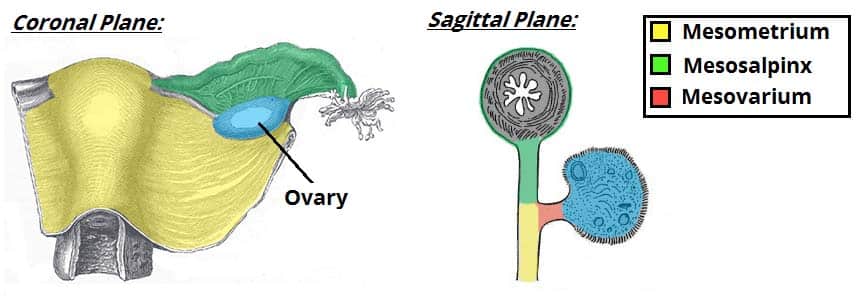
What is the mesovarium?
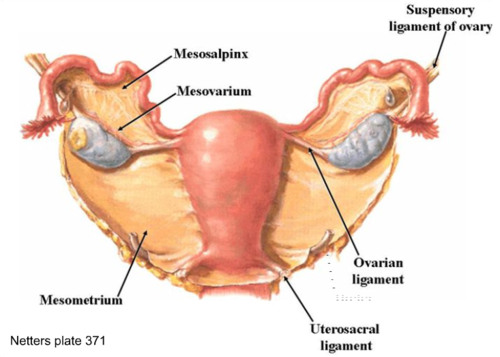
A peritoneal fold attaching to the anterior border of the ovary; part of the broad ligament.
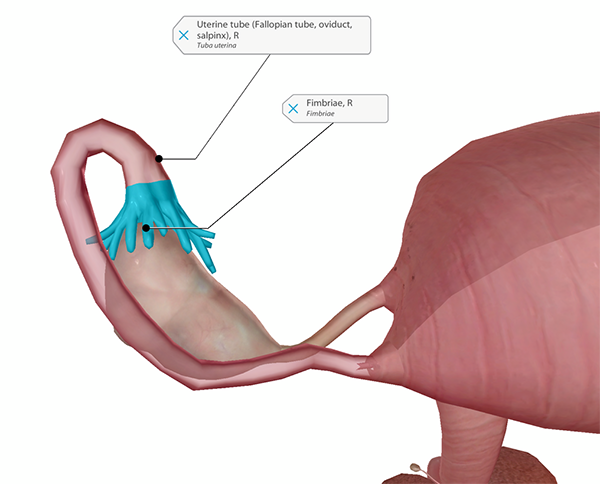
What is the ovarian fimbria?
A long fimbria connecting tube to ovary, helping capture the oocyte.
What are the four parts of the uterine tube (lateral → medial)?
infundibulum → Ampulla → Isthmus → Intramural (uterine) part.
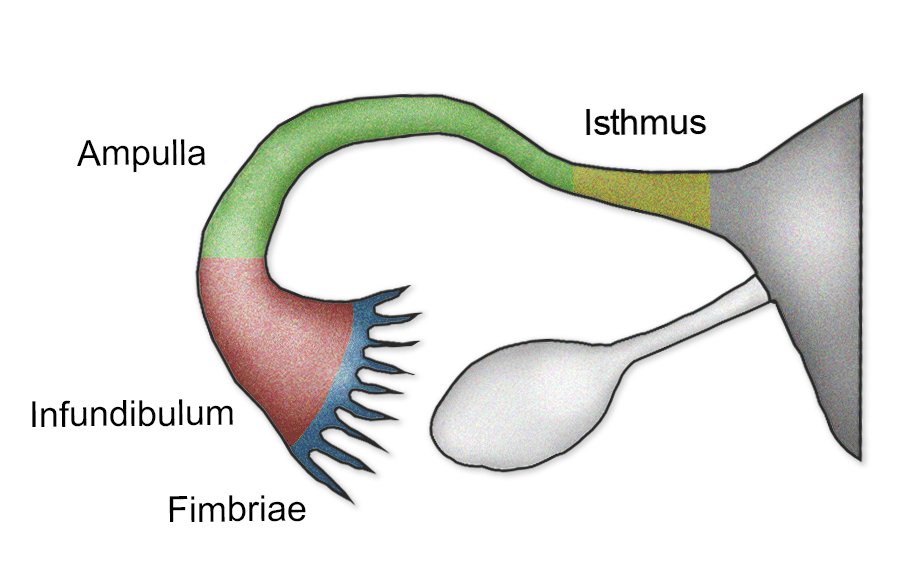
What happens in the ampulla of the uterine tube?
Fertilization.
Why is the isthmus a common site for ectopic pregnancy?
Narrow lumen + scarring (PID) → embryo gets trapped.
What risk is associated with the intramural (uterine) part of the tube?
Dangerous interstitial ectopic pregnancy → uterine rupture around 3–4 months.
happens in the intramural part of the tube, which is surrounded by thick, vascular myometrium. This delays rupture until 3–4 months, but when rupture happens, it causes massive hemorrhage due to tearing of uterine wall and involvement of both uterine and ovarian blood supplies.
What is the mesosalpinx?
Upper part of the broad ligament supporting the uterine tube.
What are the two normal angles of the uterus?
• Anteverted – vagina–cervix angle opens forward
• Anteflexed – cervix–body angle opens forward
What structures maintain uterine position?
Pelvic peritoneum, broad ligament, round ligaments.
![Figure, Uterine Tubal Anatomy and Ligaments...] - StatPearls - NCBI Bookshelf](https://www.ncbi.nlm.nih.gov/books/NBK499970/bin/uterusLigaments.jpg)
What happens in uterine prolapse?
Uterus descends into/through vagina due to weakened support.
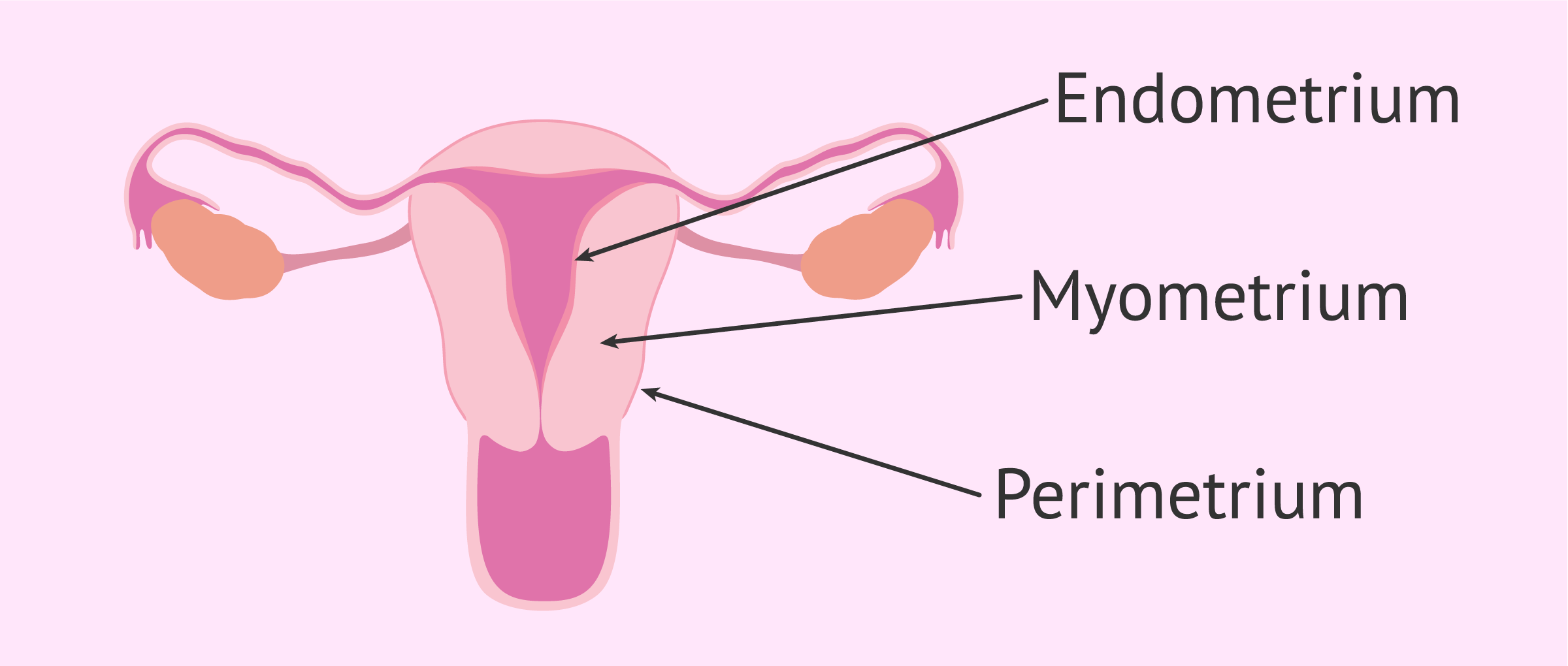
What are the layers of the uterine body?
Endometrium + Myometrium.
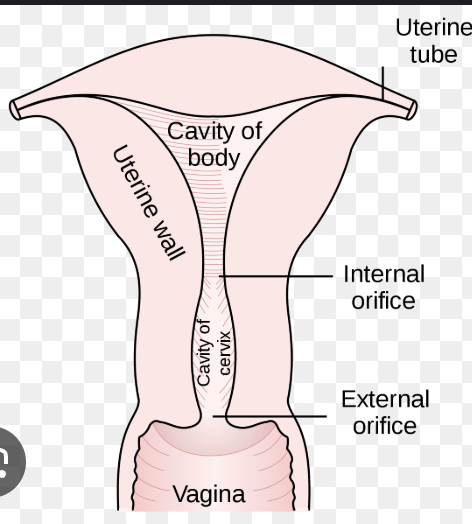
What connects the uterine cavity to the vagina?
Cervical canal via the external os.
What is the rectouterine pouch (Pouch of Douglas)?
The deepest peritoneal space in females, behind the uterus.
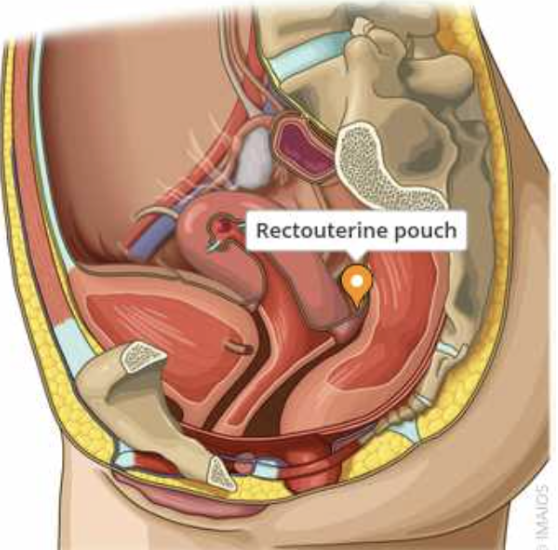
How is culdocentesis performed?
clinical procedure where a needle is inserted through the posterior vaginal fornix into the rectouterine pouch (pouch of Douglas) to check for free fluid in the pelvis.
What forms the vaginal fornices?
The pelvic vagina attaching around the cervix
:background_color(FFFFFF):format(jpeg)/images/article/vaginal-fornix/78zS2YZofs8s54GHfIuIJQ_7ZkkZyAZ5wsuqc66Wk9qg_Fornix_vaginae_01.png)
Why is the posterior fornix clinically important?
It gives access to the rectouterine pouch (culdocentesis).
What structure lies anterior to the pelvic vagina?
Bladder and urethra.
What lies posterior to the pelvic vagina?
Rectum (ampulla).
What artery supplies the ovaries?
Ovarian artery (direct from abdominal aorta)
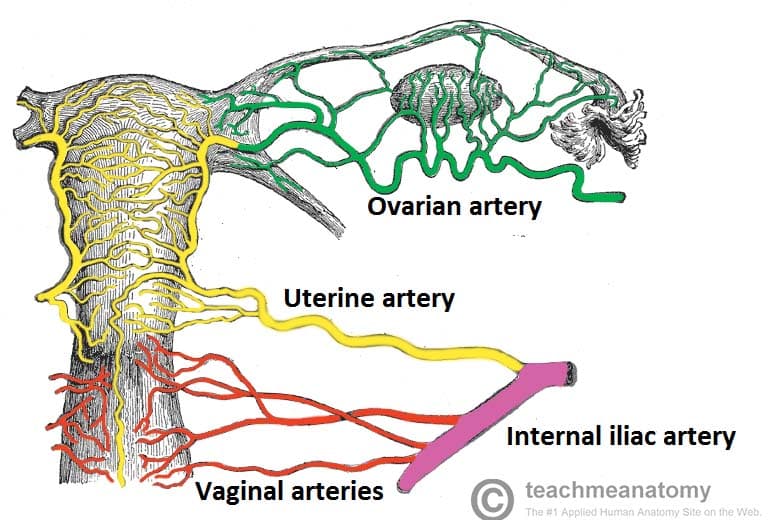
What artery supplies the uterus?
Uterine artery (from internal iliac).
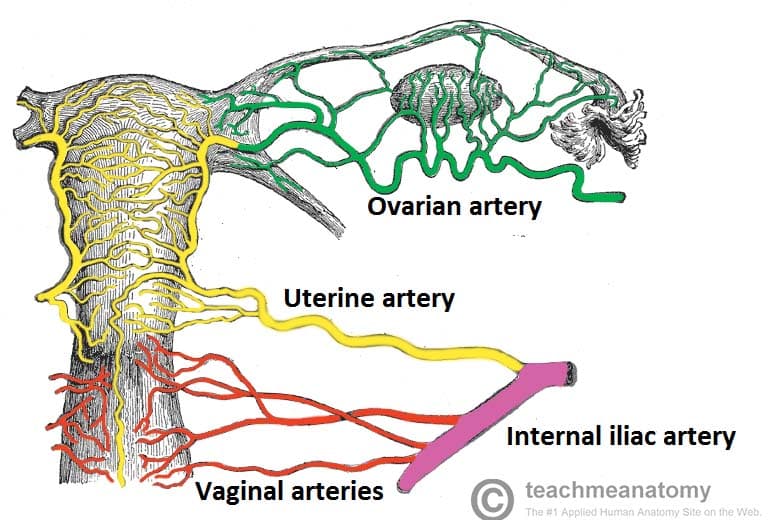
What artery gives branches to the uterine tubes?
Ovarian artery (tubal branches)
• Ascending uterine artery (tubal branches)

What vessels supply the superior bladder in both sexes?
Superior vesical arteries (from patent umbilical artery).
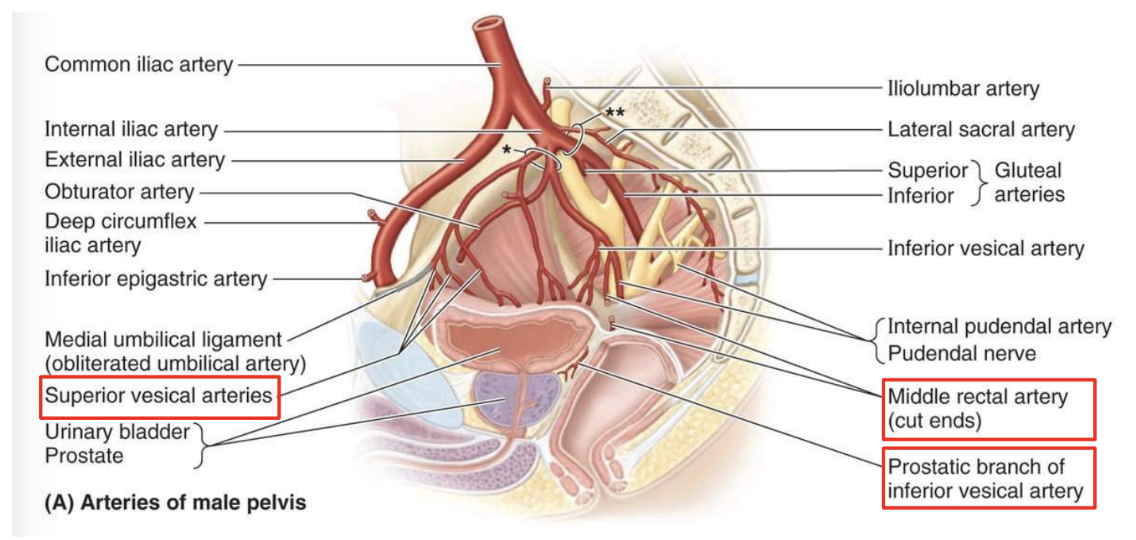
What artery supplies the inferior bladder + prostate in males?
Inferior vesical artery.
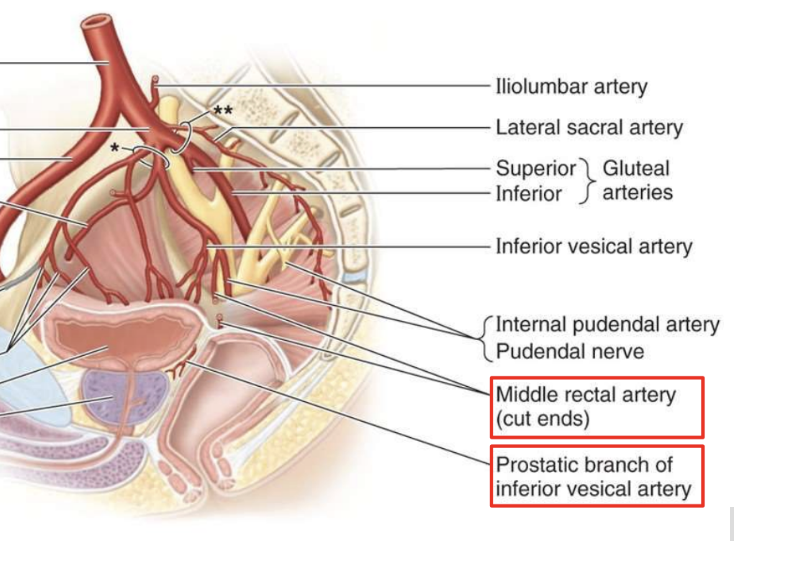
What artery replaces the inferior vesical artery in females?
Uterine artery.
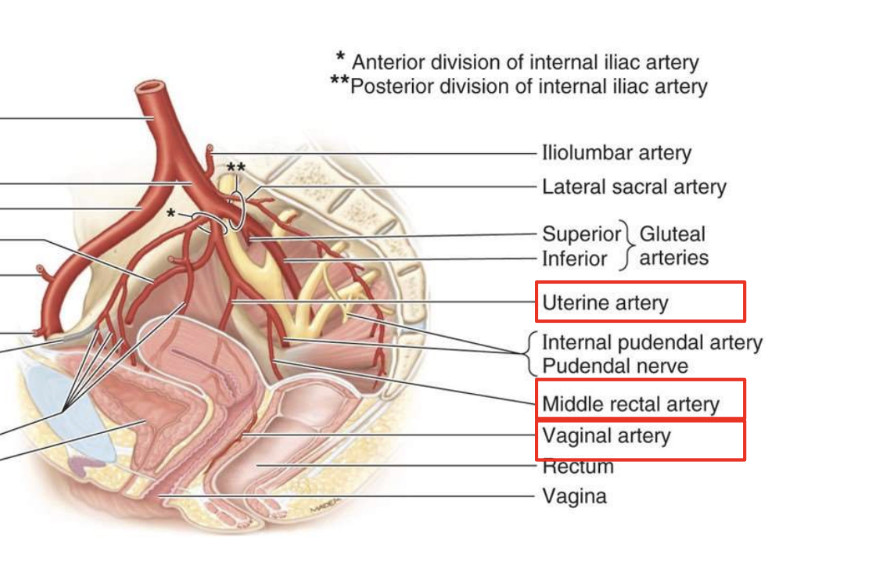
What does the middle rectal artery supply?
Middle rectum + rectal ampulla. (from internal iliac)
:background_color(FFFFFF):format(jpeg)/images/library/13516/1000.png)
Where do pelvic venous plexuses drain that allows spread of cancer to the spine?
Internal vertebral venous plexus (Batson’s plexus), which is valveless.
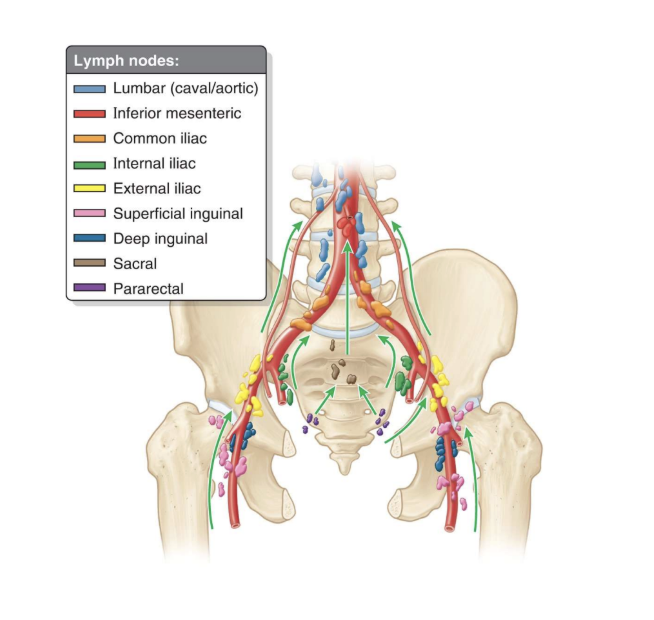
What is the lymphatic pathway from pelvic organs?
Internal iliac → Common iliac → Lumbar nodes → Cisterna chyli → Thoracic duct.
Which spinal cord levels give rise to sympathetic fibers for pelvic organs?
L1-L2
Which specific region of the spinal cord contains the sympathetic cell bodies?
The intermediolateral (IML) cell column of L1–L2.
Are sympathetic fibers to pelvic organs preganglionic or postganglionic when they leave L1–L2?
They are preganglionic when they leave the spinal cord.
Through which nerves do sympathetic fibers leave the lumbar sympathetic chain?
![PDF] Clinical anatomy of the splanchnic nerves | Semantic Scholar](https://figures.semanticscholar.org/4662eec7fef4399313a9b268d3eed956a10e14dd/3-Figure3-1.png)
Lumbar splanchnic nerves.
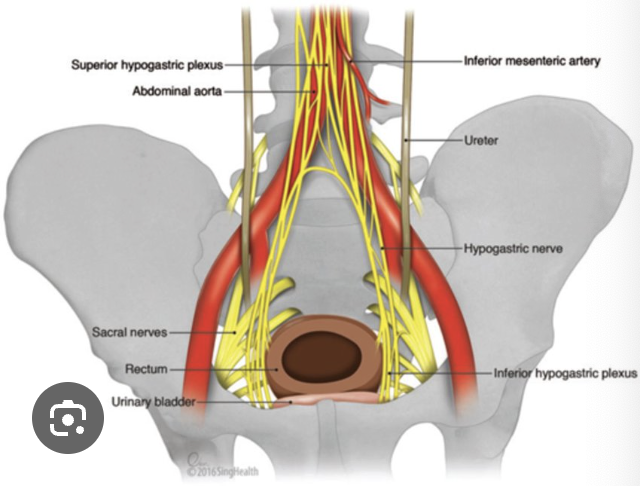
What major autonomic plexus in the pelvis first receives lumbar splanchnic fibers?
The superior hypogastric plexus.
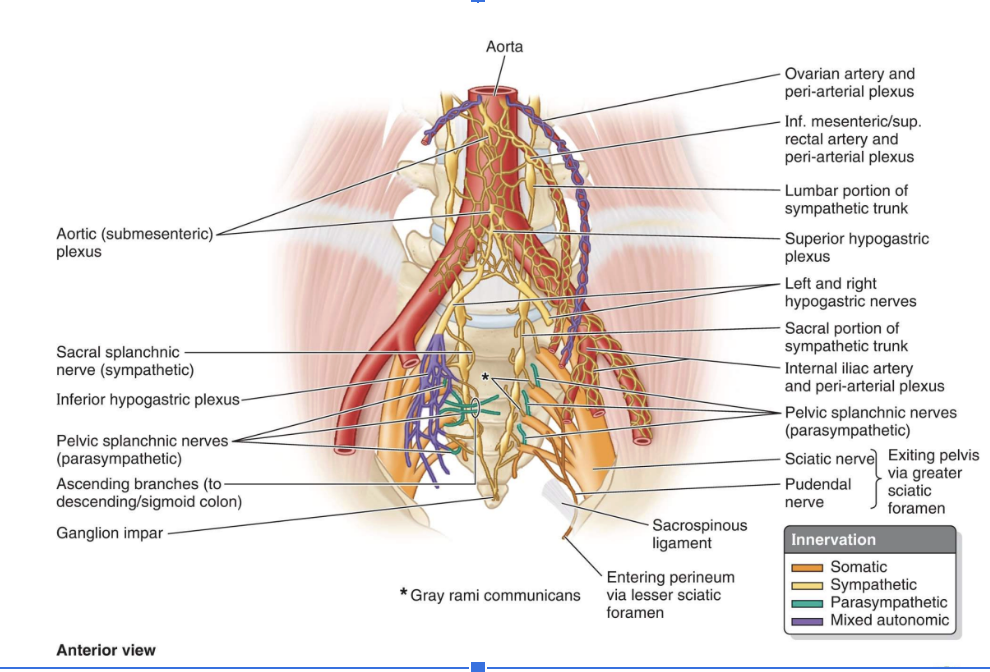
How do sympathetic fibers descend from the superior hypogastric plexus into the pelvis?
Through the hypogastric nerves.
:background_color(FFFFFF):format(jpeg)/images/article/hypogastric-nerve/AtiYThhA42W6YEDxLWwLA_hypogastric_nerve.png)
Where do sympathetic fibers finally distribute to individual pelvic organs?
From the inferior hypogastric plexus.
What sympathetic functions occur in the pelvis (examples)?
Contracts internal urethral & internal anal sphincters.
Relaxes detrusor muscle (inhibits urination).
Vasoconstriction of pelvic vessels.
Why does pelvic pain from organs ABOVE the pelvic pain line refer to L1–L2 dermatomes?
Because visceral pain afferents follow sympathetic fibers back to L1–L2.

Which pelvic organs receive sympathetic fibers from L1–L2?
Bladder, uterus, vagina, prostate, seminal vesicles, and the distal ureter.
Why can pelvic pathology cause groin or lower abdominal pain?
Because visceral pain afferents from pelvic organs (above the pelvic pain line) travel with sympathetics to L1–L2, and the brain refers the pain to those dermatome
Which dermatomes correspond to L1 and L2?
L1: inguinal/groin region
L2: upper medial thigh
From which spinal levels does parasympathetic innervation to pelvic organs arise?
S2–S4, via the pelvic splanchnic nerves.
Do pelvic splanchnic nerves pass through the sympathetic chain?
No. They travel directly from the ventral rami of S2–S4 into the inferior hypogastric plexus.
Where do parasympathetic fibers enter to reach pelvic organs?
They enter the inferior hypogastric plexus and then supply organs directly.
What are the major parasympathetic functions in the pelvis?
Contracts detrusor muscle → urination.
Relaxes internal urethral sphincter (in males).
Increases rectal motility.
Supplies erectile tissues → vasodilation → erection (“point”).
Regulates distal colon and pelvic viscera.
Why can pelvic pathology produce sacral, perineal, or lower back pain?
Because visceral afferents from organs below the pelvic pain line follow parasympathetics to S2–S4, referring pain to those dermatomes.
Which dermatomes correspond to S2–S4?
The perineum, sacral region, and lower back.
How does the pelvic pain line explain labor pain patterns?
Uterine contractions → L1–L2 referral → lower abdominal pain.
Cervical dilation → S2–S4 referral → sacral back pain.
What is an ovarian ectopic pregnancy?
Implantation on the ovary due to failure to capture the oocyte.
What is an infundibular ectopic pregnancy?
Implantation in the infundibulum; may detach into peritoneum.
Where do most ectopic pregnancies occur?
Ampulla.
Why is an isthmic ectopic pregnancy dangerous?
The lumen is very narrow → rapid rupture → massive hemorrhage.
What is an interstitial (intramural) ectopic pregnancy?
Embryo implants where tube enters uterine wall → expands until uterine rupture at 3–4 months.
What happens in a cervical ectopic pregnancy?
Implantation in cervical canal → often lost as cervix dilates.
What does a Pap smear test sample? what does it screen for?
Cells from around the external os.
screens for Cervical dysplasia and cervical carcinoma.