A-Level Biology Edexcel A - Topic 6 : Immunity, Infection and Forensics
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
60 Terms
Which 5 factors are used to determine the time of death of a mammal?
• Extent of decomposition
• Stage of succession
• Forensic entomology
• Body temperature
• Degree of muscle contraction.
Describe the stages of decomposition.
1) Autolysis occurs - Enzymes in the gut start to break down the wall of the gut and the surrounding area. As cells die, they release enzymes which help break down tissues.
2) The loss of oxygen in tissues favours the growth of anaerobic bacteria. The bacteria invade tissues and release more enzymes.
----------------------------------------------
After a few hours:
• Cells and tissues are broken down by enzymes and bacteria present before death - turns skin green
Few days-weeks:
• Microorganisms decompose tissues and organs - produces gasses which cause bloating.
• Skin blisters and falls off
Few weeks:
• tissues liquefy and seep into the area around the body causing bloating and deflation
Few months - years:
• Skeleton remains
Decades - centuries:
• Skeleton disintegrates - nothing left
How is extent of decomposition used to determine time of death?
Bodies in similar environmental conditions show regular patterns of decay ( fresh → bloated → decaying → dry). Therefore stage of decomposition can be used to determine how long a body has been dead for.
Which factors affect the extent of decomposition?
• Mild heat - increases rate as enzymes activity increases
• Intense heat - decreases rate as enzymes become denatured
• Humidity - the more humid the quicker the rate. In extremely dry conditions the process can stop completely (e.g. mummies).
• Presence of wounds - increases rate as bacteria are able to enter more easily
How can stage of succession be used to determine time of death?
As the body decays, the species colonising the body change - there is a succession in species. As there is a predictable sequence of ecological succession, analysis of the community of species present can be used to determine time of death.
----------------------------------------------
1) Anaerobic bacteria thrive in the no oxygen and acidic (lactic acid) conditions
2) Certain flies, such as blowflies arrive, they are attracted to the moisture, smell and open wounds. They lay eggs on the carcass.
3) The eggs hatch, maggots eat the skin and tissue of the body, this liquidises certain parts which the adult flies feed on
4) Beetles are attracted, they lay eggs and the grub that hatch eat the maggots
5) Parasitic wasps lay eggs in the beetle and fly larvae
6) Eventually the body dries out and species such as cheese and coffin flies are abundant
7) Dehydration continues, maggots can't survive. Beetles with strong mandibles, such as carcass beetles move in and eat the remaining muscles and connecting tissues
8) Finally mites and moth larvae digest the hair
----------------------------------------------
The season, weather, size and location of the body will influence the type and number of species present.
How can forensic entomology be used to determine time of death?
• Each species of insects has a specific life cycle:
Egg (1 day) → Larva (9 days) → Pupa ( 6 - 12 days) → Adult fly.
• By determining the age of insects on a corpse the time of death can be determined.
• They collect the eggs, larvae and pupa found and let them grow into adults to estimate how long the insects have been there.
• Mostly used for bodies 4 - 14 days old.
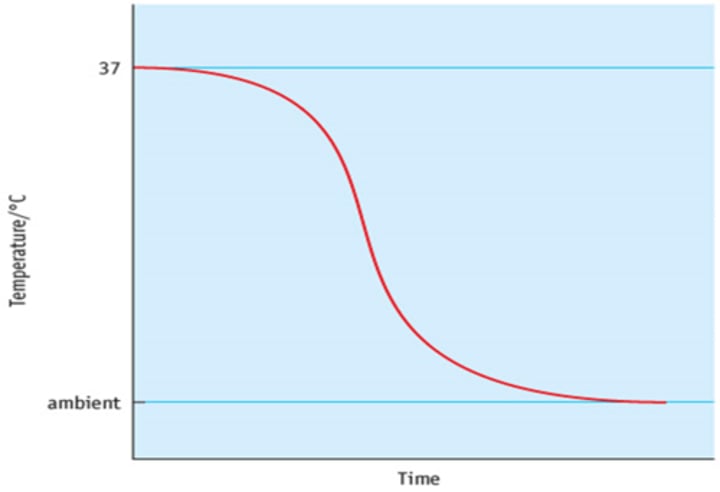
How can body temperature be used to determine time of death?
• After death the temperature of the body begins to decrease from 37°C as exothermic metabolic reactions stop.
• If the temperature of the room is known, it is possible to create a cooling curve to determine the time of death.
• This can only be done within the first 24 hours after death as the body will eventually reach the same temperature as the surroundings (ambient).
Which factors effect the rate of cooling/body temperature?
• Body Size - slows cooling
• Body Position (compact) - slows cooling
• Clothing - slows cooling
• Air Movement - speeds cooling
• Humidity - slows cooling
Describe the process of rigor mortis.
1) Muscles become deprived of oxygen.
2) Anaerobic respiration occurs, causing the build up of lactic acid in muscles.
3) The pH decreases due to the lactic acid, inhibiting the production of ATP by enzymes.
4) Without the presence of ATP, the actin and myosin in muscle fibres stick permanently to each other, meaning the muscles can no longer relax. So they contract, starting with the smaller muscle groups, causing the body to stiffen.
How can degree of muscle contraction (rigor mortis) be used to determine time of death?
• After death muscles begin to stiffen. The extent of rigor mortis can be used to determine time of death.
• Begins about 2 - 4 hours after death
• Full effect is about 6 - 8 hours.
• It passes at about 36 - 48 hours after death
• However, this is only applicable within the first 36 hours of death because the stiffness wears off as muscle fibres begin to break down.
• The warmer the environment the quicker the process of rigor mortis.
What is the role of microorganisms in the decomposition of organic matter and recycling of carbon?
• Bacteria and fungi use enzymes to hydrolyse dead organic matter into smaller molecules that they can use as respiratory substrates.
• During this process carbon dioxide and methane and is released thus recycling carbon.
What is the purpose DNA profiling?
• Genetic identification of organisms
• Determining genetic relationships between organisms
• To identify an individuals risk of developing particular diseases
Describe the process of DNA profiling/fingerprinting.
1) DNA is amplified using PCR (this allows for small samples to be analysed)
2) Fragments of DNA are cut with restriction endonuclease enzymes
3) The fragments are separated and visualised using gel electrophoresis
4) A southern blot is carried out
5) 'Blots' are compared
Describe the process of gel electrophoresis.
• Fragments are dyed with ethidium bromide so they fluoresce under UV light.
• Fragments are loaded into wells of agarose gel.
• The gel is submerged in a buffer solution
• A current is then applied to the gel. DNA is negatively charged so the fragments move towards the positive anode. Fragments of different sizes move differently according to mass so 'bands' will appear. Smaller fragments (fewer STRs) travel faster.
Describe the process of a southern blot.
• An alkaline buffer solution is added to the gel
• A nylon or nitrocellulose membrane/filter is placed onto the gel
• The buffer solution contain DNA fragments is drawn by capillary action into the membrane
• The DNA fragments will then stick to the membrane (visible as 'blots')
• Hybridization - DNA probes (complementary sequences labeled with genes like fluoresce or radioactivity) are added and will bind with the DNA fragments.
• If the DNA probes were radioactive, X-ray film is used to detect the fragments. If the DNA probes were fluorescent, the fragments are viewed under UV light. This resulting image is called a DNA fingerprint/profile
Only those that bound to the probe show up, hence indicating whether this person is related to an individual/the suspect.
How is DNA amplified in PCR (Polymerase Chain Reaction)?
1) A reaction mixture is set up by mixing the DNA sample, primers, free nucleotides and the enzyme DNA polymerase.
2) The mixture is then heated to 90°C - 95°C for 30 seconds to break the hydrogen bonds and therefore separate the two DNA strands.
3) The mixture is then cooled for 20 seconds to a temperature between 50°C - 60°C so that the primers can bind to the DNA strands.
4) The temperature is increased to 70°C - 75°C for at least 1 minute as this is the temperature DNA polymerase works at. DNA polymerase creates a copy of the sample by complementary base pairing using the free nucleotides.
5) This cycle is repeated as many times as wanted/needed in order to gives rise to an amount of DNA which is sufficient to create a DNA profile.
Each PCR cycle doubles the amount of DNA present
Describe the structure of a bacterial cell
Cell Wall - the cell's rigid outer covering made of peptidoglycan. Provides the cell with strength and support.
Slime Capsule - protective slimy layer of polysaccharide which helps the cell to retain moisture and adhere to surfaces.
Plasmid - circular piece/loops of DNA.
Flagellum - a tail-like structure which propels the cell forwards using a corkscrew motion.
Pili - hair-like structures which help the cell to adhere to various surfaces, primarily other bacterial cells.
Ribosomes - The site of protein synthesis.
Mesosomes - infoldings of the inner membrane which contain enzymes required for respiration.
Circular DNA
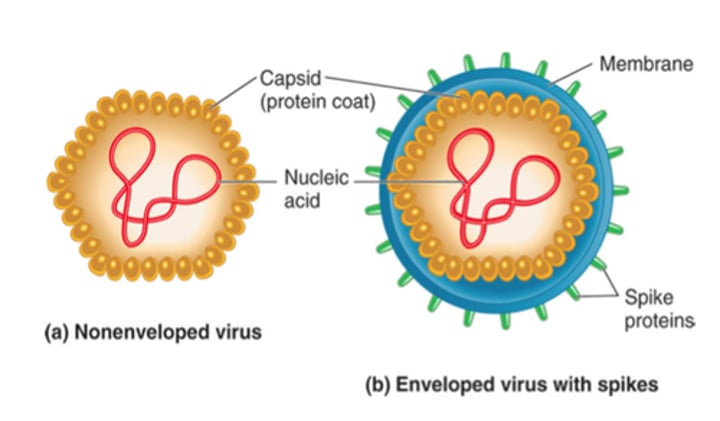
Describe the structure of a virus
Non-enveloped:
• Nucleic acid genome - DNA or RNA (can be either singe or double stranded + can be either linear or circular)
• Viral enzymes e.g. reverse transcriptase
• Surrounded by capsid - a protective protein coat made of capsomeres
----------------------------------------------
Enveloped:
• Nucleic acid genome - DNA or RNA (can be either singe or double stranded + can be either linear or circular)
• Viral enzymes e.g. reverse transcriptase
• Surrounded by matrix protein
• Lipid layer called the envelope derived from cell membrane of host cell
• Attachment proteins on surface
Compare viruses and bacteria
• Bacteria are prokaryotes, viruses are non-living
• Viruses are dependant on host cells to survive, bacteria do not need hosts
• Viruses are significantly smaller than bacteria.
• Bacteria have an average diameter of 0.5-5µm, whereas viruses have a much wider range of sizes and shapes with diameters varying between 20-40nm
• Bacteria have a cell membrane, cell wall and cytoplasm, as well as other organelles
such as ribosomes, plasmids, flagellum and pili. Viruses possess no such structures.
Why are viruses referred to as 'particles' instead of cells?
Acellular & non-living: no cytoplasm, cannot self-reproduce, no metabolism.
What are retroviruses?
Viruses that contain RNA as their genetic information
How does Mycobacterium tuberculosis cause disease?
1) Primary infection - Infects phagocytes in the lungs, triggering an inflammatory response which seals infected phagocytes in waxy-coated tubercles so that the bacteria remain dormant → symptomless
2) When the immune system becomes weakened, the bacteria become active again and destroy lung tissue. This can be fatal.
In some cases, the bacteria can invade glands and the CNS.
What symptoms does TB cause?
• Breathing problems
• Coughing (up blood in sputum)
• Loss of appetite
• Weight loss
• Fever
How is TB transmitted?
• Drinking infected milk
• Through the inhalation of droplets of mucus and saliva from talking, coughing and sneezing.
What factors increase the risk of TB transmission?
• Close contact
• Poor health
• Poor diet
• Overcrowded living conditions
How can you prevent the transmission of TB?
• Improve living standards
• Treat cattle diseases
• Protective clothing
What features has the bacteria Mycobacterium Tuberculosis evolved to help them evade the immune system?
• When engulfed by phagocytes, they produce substances that prevent the lysosome fusing with the vacuole so that they aren't broken down and can multiply undetected in phagocytes
• Disrupts antigen presentation in infected cells, preventing the immune system from recognising and killing infected phagocytes
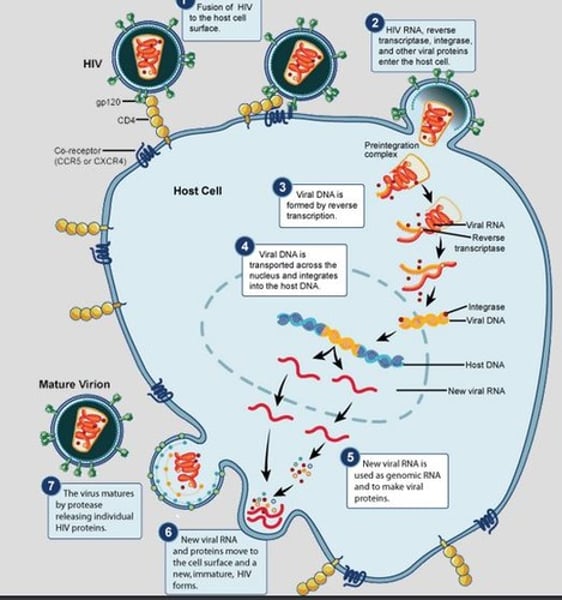
How does HIV infect the body?
1) HIV attaches to the surface of a macrophage (T helper cel), which acts as the host cell - The gp120 protein (on virus surface) binds to the CD4 protein (on host cell membrane).
2) Viral DNA is formed by the enzyme reverse transcriptase.
3) This new DNA moves into the nucleus and integrates into the host cell DNA by the enzyme integrase.
4) Using the host cell machinery, mRNA is synthesised from the new proviral RNA
5) Viral mRNA is translated to make viral enzymes, structural proteins and genomic RNA.
7) The viral genome and structural proteins assemble to form the basic structure of the virus. These move out of the host cell by exocytosis, taking part of the cell membrane with it to form the lipid layer around the virus and thus killing the host cell.
8) The same cycle repeats, reducing the number of T helper cells in the body, weakening immunity
9) AIDS develops when there are too few T helper cells for the immune system to function (usually after 8 - 10 years)
What symptoms are caused by HIV?
These symptoms are known as AIDS:
• Fever
• Headaches
• Fatigue
• Weight loss
• Diarrhoea
• Swollen glands
• Night sweats
• Opportunistic infections (e.g. TB, Pneumonia)
How is HIV transmitted?
HIV is not a very tough virus and therefore cannot survive outside of the body for any significant time. Therefore, it is transmitted through the exchange of body fluids (with the exceptions of saliva and urine):
• Blood - Sharing needles, blood transfusions, cuts and grazes
• Maternal transmission - late stages of pregnancy, breastfeeding
• Vaginal secretions and Semen - unprotected sex
How can you prevent HIV spread?
• Use of condoms
• Clean needles
• Awareness programmes
• Avoiding promiscuity
What features has HIV evolved to help them evade the immune system?
• The protein coat is constantly changing so the immune system cannot target and destroy it
• It reduces the number of immune cells in the body
• Has a high rate of mutation in the genes which code for antigen proteins. This means that the structure of the antigens constantly change so the memory cells won't recognise these new strains. The body will have to produce a primary response for each new strain.
At what point will a patient show a HIV positive result?
3-12 weeks after infection, when HIV antibodies appear in the blood
How can some people be immune to HIV?
They lack the CD4+ receptor on T helper cells that HIV requires for docking.
Why is it difficult to create a vaccine for AIDS?
• Virus mutates rapidly, therefore antigens on the viral surface continually change
• Working on animals to develop vaccines is not possible because HIV only infects humans
• The virus hides itself for years inside macrophages, therefore most vaccines may not work properly
What are the routes a pathogen can enter the body with?
• Vector (organism that transmits infection) - prevented by blood clotting, skin and sebum
• Formites (objects carrying pathogens) - prevented by skin, skin flora and vomiting
• Direct contact (skin-to-skin or exchange of fluids) - prevented by lysozymes, defensive secretions, mucus and skin flora
• Inhalation - prevented by mucus, vomiting, lysozymes and cilia
• Ingestion (contaminated food and drink) - prevented by vomiting, mucus and saliva
• Inoculation (break in the skin by using enzymes or passively
through wounds, hair follicles or sweat glands) - prevented by skin and blood clotting
What physical barriers to infection does the body have?
• Skin - a tough physical barrier consisting of keratin. Also secretes sebum which can kill some microbes
• Stomach Acid (hydrochloric acid) - kills bacteria.
• Gut and skin flora - natural bacterial flora competes with pathogens for food and space.
• Mucus traps bacteria so that it can be removed by the contraction of the cilia or stalled and passed into the digestive system
What are the non-specific responses of the body to infection?
Inflammation:
• Histamines released by damaged white blood cells cause vasodilation. This increases the flow of blood to the infected area and increases permeability of blood vessels. As a result, antibodies, white blood cells and plasma leak out into the infected tissue and attack the pathogen.
• This causes oedema (swelling) and often pain.
Fever:
• The hypothalamus sets body temperature higher. This decreases the speed of pathogen reproduction and increases rate of specific immune response.
Lysozyme action:
Lysozyme (an enzyme found in secretions such as tears, sweat, saliva and mucus) kills bacterial cells by hydrolysing their cell wall
Interferon:
• A chemical released from cells which inhibits the production of viral proteins and therefore prevents from multiplying/replicating
• Promote inflammation
• Activate some immune cells
Phagocytosis:
1) Phagocytes recognise the antigens of a pathogen and attach onto the surface
2) The cytoplasm of the phagocyte moves around the pathogen, engulfing it. This forms a phagosome within the cytoplasm of the phagocyte.
3) A lysosome fuses with the phagosome and the enzymes break down the pathogens
4) The phagocyte then presents the pathogen's antigens on its surface to activate other immune system cells.
Involves neutrophils and monocytes which differentiate into macrophages (a type of phagocyte).
What are the different lymphocytes and their functions?
B lymphocytes (B cells):
• Produced and mature in the bone marrow and are involved in the humoral response
• B effector - differentiate to produce plasma cells which which release antibodies
• B memory cells - remain in the body for months or years, enabling an individual to respond quickly to the same antigen. They are specific to the antigen encountered during the primary immune response.
T lymphocytes (T cells)
• Produced in the bone marrow and mature in the thymus gland
• Involved in both the cell mediated and humoral response
• T helper - activate phagocytes and B cells and aid T killer cells to divide
• T killer - destroy cells with foreign antigens on their surface by releasing perforin and cytotoxins
• T memory/effector - a long lived T cell that has receptors for an antigen due to its encounter with a prior infection or vaccination
What is an APC?
Antigen Presenting Cell - displays foreign antigens with MHC (Major Histocompatibility Complexes) on their surfaces for T cells to recognise
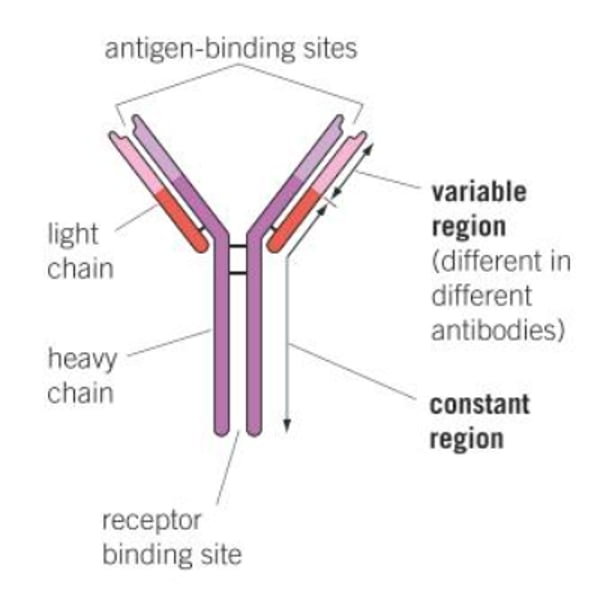
Describe the structure of an antibody
• Antibodies are made of four polypeptide chains: two heavy chains and 2 light chains.
• Each chain has a variable region and a constant region.
• The variable regions have a shape which is complementary to a particular antigen and differ between antibodies. They form the antigen binding sites
• The constant regions allow binding to receptors on immune system cells (e.g. phagocytes) and are the same in all antibodies.
• Disulphide bridges hold the peptide chains together
What are the functions of antibodies?
• Opsonisation - the antibodies act as markers so that phagocytes can easily recognise and destroy the pathogens
• Agglutination - clumps the pathogens together so that phagocytosis occurs much more easily/efficiently
• Neutralisation/Precipitation - bind to the toxins produced by pathogens, and in doing so make them insoluble - hence inactive. The toxin-antibody complexes are then phagocytosed.
• Lysis - breaking open of bacterial cells
• Preventing pathogens from binding to host cells by blocking the cell surface receptors so they cannot attach to and infect host cells.
What are the 2 types of specific immune response?
• The humoral response
• The cell mediated response
Describe the process of the humoral response.
T Helper Activation:
1) Pathogen is engulfed by a macrophage.
2) The surface antigens are passed along the endoplasmic reticulum into a vesicle which are transported to the cell surface membrane. The macrophage acts as an APC and presents the antigens on MHCs.
3) The APC binds to T helper cells with complementary CD4 receptors.
4) The T Helper cell is 'activated' and divides by mitosis to form T memory cells and active T helper cells. The T memory cells remain in the body and become activated if the pathogen is encountered again.
Effector stage:
5) B cell antibodies bind to the complementary antigens of the APC and engulf it by endocytosis.
6) The B cell becomes an APC and presents antigens on MHCs.
7) An activated T helper cell, with a complementary receptor to the antigens, binds to the APC and produces cytokines.
8) Th cytokines produced stimulate the B cell to divide by mitosis and form B memory cells and B effector cells. The B memory cells remain in the body and become activated if the pathogen is encountered again.
9) The B effector cells differentiate into plasma cells which secrete/synthesise antibodies.
10) The antibodies attach to the pathogen, which macrophages identify and then attack.
11) T Suppressor cells stop the immune response.
Describe the process of the cell mediated response
1) Pathogen infects/invades host cells and presents the antigens on MHCs to become an APC
2) T Killer cell with complementary receptor proteins binds to the APC.
3) Cytokines secreted by active T Helper cells stimulate the T Killer cell to divide by mitosis.
4) T Killer cell divides to form active T Killer cells and T Memory cells. The T memory cells remain in the body and become activated if the pathogen is encountered again.
5) The active T Killer cells bind to APCs and secrete perforins which cause pores to form in the cell membrane.
6) The APCs become permeable so water and ions enter causing them to swell, burst and die.
Compare and contrast the humoral response and the cell mediated response.
Similarities:
• Both respond to antigens
• Both require the formation of APCs and the presence of MHCs
• Both involve clonal selection (the activation of only those cells that recognise the antigen)
• Both involve clonal expansion (the proliferation of the cells needed so that there are large numbers)
• Both involve T helper cells
• Both result in the production of memory cells
• Both have a lag period.
Differences:
• The humoral response works against extracellular pathogens (in the blood and tissue fluids) whereas the cell mediated response works against intracellular pathogens (in cells that present antigens).
• The humoral response produces antibodies whereas the cell mediated response produces cytokines and T killer cells.
What is clonal expansion?
When B cells and T cells which are complementary to an antigen undergo rapid mitotic division to form many cloned cells
Compare the primary and secondary immune responses
• Secondary response has a faster rate of antibody production than the primary response
• Secondary response has a. shorter time lag between exposure & antibody production than the primary response
• Secondary response has a higher concentration of antibodies than the primary response
What is passive natural immunity?
Immunity that is acquired by the transfer of antibodies from a mother to a foetus through the placenta or to a baby through breastfeeding.
What is passive artificial immunity?
Immunity that is acquired by the transfer of pre-made antibodies to an individual through an injection.
What is active natural immunity?
Immunity that is acquired from natural infection with/exposure to a live pathogen.
What is active artificial immunity?
Immunity that is acquired by exposure to a dead or weakened version of a pathogen in the form of a vaccine.
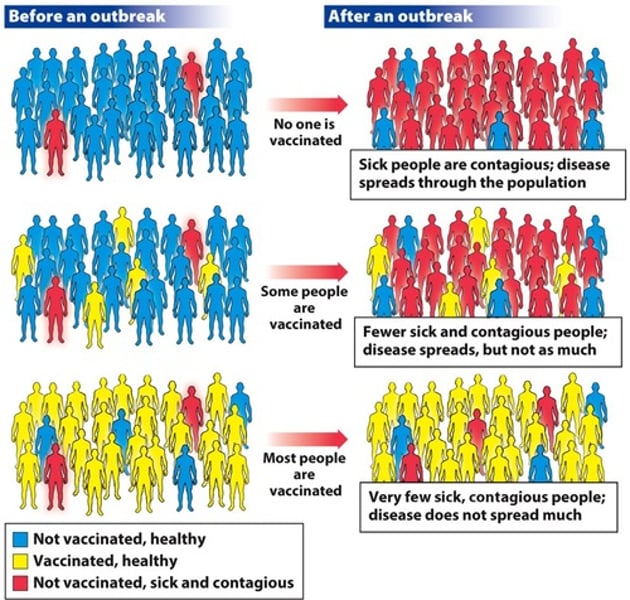
What is meant by heard immunity?
the idea that a population can be protected from a certain disease if a threshold of vaccination is reached.
What are the different types of atibiotics
Bacteriostatic - inhibit the growth of bacteria by stopping protein synthesis and production of nucleic acids so the bacteria can't divide and grow.
Bactericidal - kill bacteria by preventing the formation of peptidoglycan cross-links in bacterial cell walls, causing osmotic lysis (bursting).
What is meant by the term 'evolutionary race' ?
The continual competition over time where infectious agents are evolving better infection mechanisms whilst the hosts are simultaneously evolving better defences.
Why is there an 'evolutionary race' between pathogens and their host?
Host defences are a selection pressure for bacteria. Random genetic mutations may enable bacteria to evade these defences.
Hosts with phylogenetic characteristics that reduce likelihood & symptoms of infection have a selective advantage.
How do some pathogens evade the body's defence systems?
• Antiphagocytic polysaccharide capsules mask antigens
• Leukocidins destroy leukocytes (WBCs)
• Antigen variability reduces effect of opsonisation/agglutination by antibodies
• Use mucinase to destroy mucin
• Use proteases to destroy mucosal secretions, antibodies and antimicrobial peptides
• Use phospholipase to destroy cytoskeleton of phagocytes to prevent fusion with lysosome
• Use urease to produce ammonia in stomach to neutralise hydrochloric acid
• Acid-resistant capsid
Why are some bacteria resistant to antibiotics?
Random genetic mutation, often on plasmid, confers resistance e.g. antigen shape changes. These bacteria have selective advantage and therefore survive in the presence of antibiotics to reproduce and pass on the allele for resistance to offspring.
What code of practice have hospitals put in place to control the spread of antibiotic resistant infections?
• Antibiotics are only prescribed when needed and their course is completed to ensure that all the bacteria are destroyed, and to minimise the selection pressure on bacteria, preventing resistant strains from forming.
• New patients are screened at arrival, isolated and treated if they are infected to prevent the spread of pathogens between patients.
• Strict hygiene regimes are followed (e.g. regular hand washing, use of alcohol based antibacterial gels, bans on wearing of jewellery, ties and long sleeved clothing) which minimises the transmission of pathogens and reduces the number of places that may harbour pathogens
• Isolating patients with resistant diseases, which prevents transmission
Describe how one gene can give rise to more than one protein?
1) DNA is transcribed to make pre-mRNA
2) DNA splicing - enzyme complexes called spliceosomes modify the pre-mRNA by removing introns (non-coding regions) and sometimes some exons (coding regions).
3) The remaining genes/exons are joined back up in different combinations to produce several different mRNA strands.
4) When these differences mRNA strands are translated they produce different amino acid sequences which results in different bonds stabilising the protein's tertiary structure and so more than one protein can be produced from one gene.