A&P 2 Exam 2 (ch. 18-20)
0.0(0)
Card Sorting
1/149
Earn XP
Description and Tags
Last updated 7:31 PM on 2/19/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
150 Terms
1
New cards
autorhythmic fibers
Specialized cardiac muscle fibers
Self-excitable
Repeatedly generate action potentials that trigger heart contractions
2 functions
-Act as pacemaker
-Form conduction system
Self-excitable
Repeatedly generate action potentials that trigger heart contractions
2 functions
-Act as pacemaker
-Form conduction system
2
New cards
metabolism of cardiac muscle
-Aerobic cellular respiration
-Many mitochondria (Lots of mitochondria help process of ATP production (fuel for heart to beat)
-Can use many different fuels (carbs, fatty acids, lactic acid, AAs, ketone bodies)
-Susceptible to failure in ischemic conditions
-Many mitochondria (Lots of mitochondria help process of ATP production (fuel for heart to beat)
-Can use many different fuels (carbs, fatty acids, lactic acid, AAs, ketone bodies)
-Susceptible to failure in ischemic conditions
3
New cards
intercalated disks
link cardiac muscle cells together
4
New cards
desmosomes
mechanical junctions that prevent cells from pulling apart
5
New cards
gap junctions
tunnels between cells for very fast action potential transmission
6
New cards
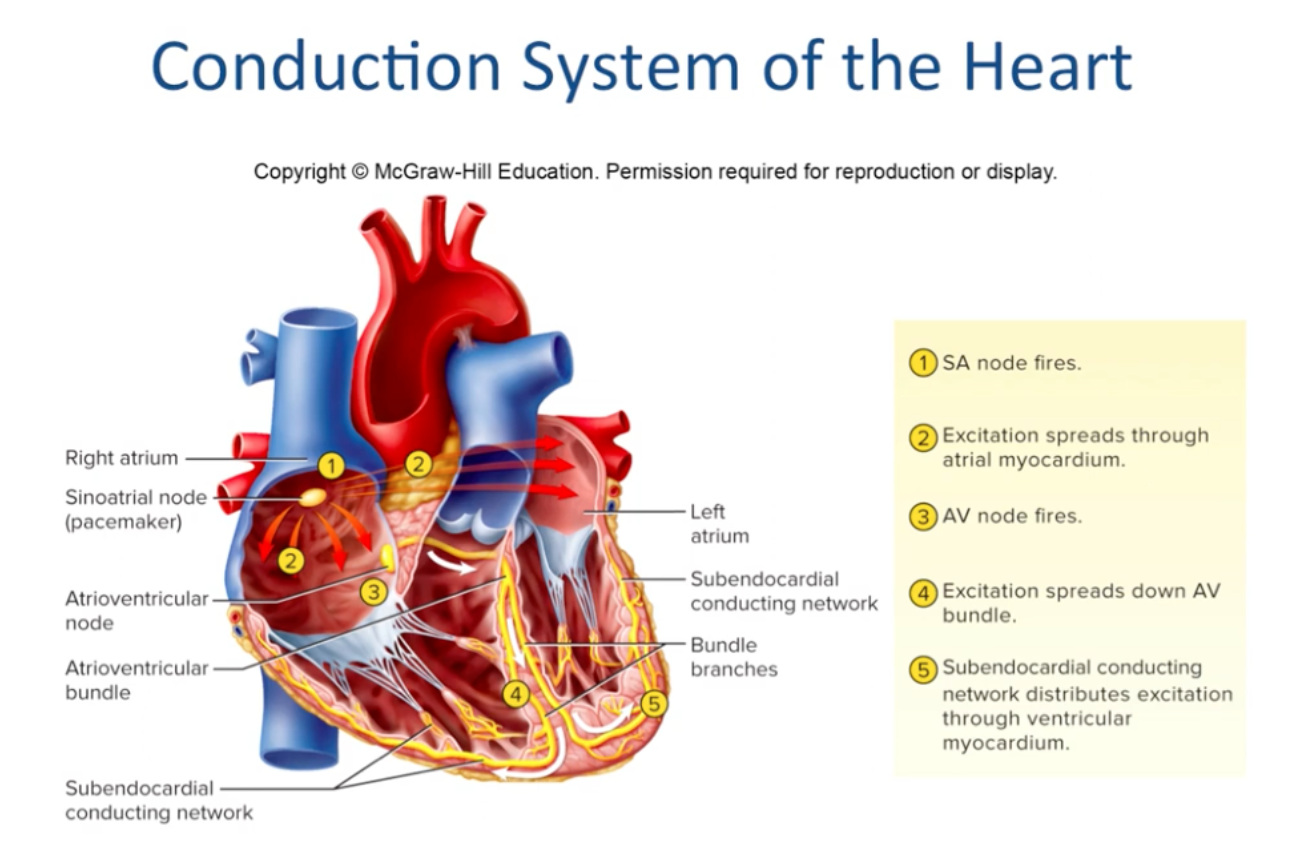
describe the heart's pacemaker and internal electrical conduction system
-Your sinoatrial (SA) node is sometimes called your heart's natural pacemaker. It sends the electrical impulses that start the heartbeat
-The SA node depolarizes and is in charge of establishing heart rate
\***if the SA node is damaged, the AV node can take over but it depolarizes much slower**
-The SA node depolarizes and is in charge of establishing heart rate
\***if the SA node is damaged, the AV node can take over but it depolarizes much slower**
7
New cards
conduction system of the heart
SA node --\> AV node --\> AV bundle --\> right and left AV bundle branches --\> Purkinje fibers (subendocardial conducting network)
8
New cards
what parts of conduction system are responsible for contraction
-signal sent from SA node: contraction of right and left atria
-signal in purkinje fibers (subendocardial conducting network): contraction of right and left ventricles
-signal in purkinje fibers (subendocardial conducting network): contraction of right and left ventricles
9
New cards
nerve supply to the heart
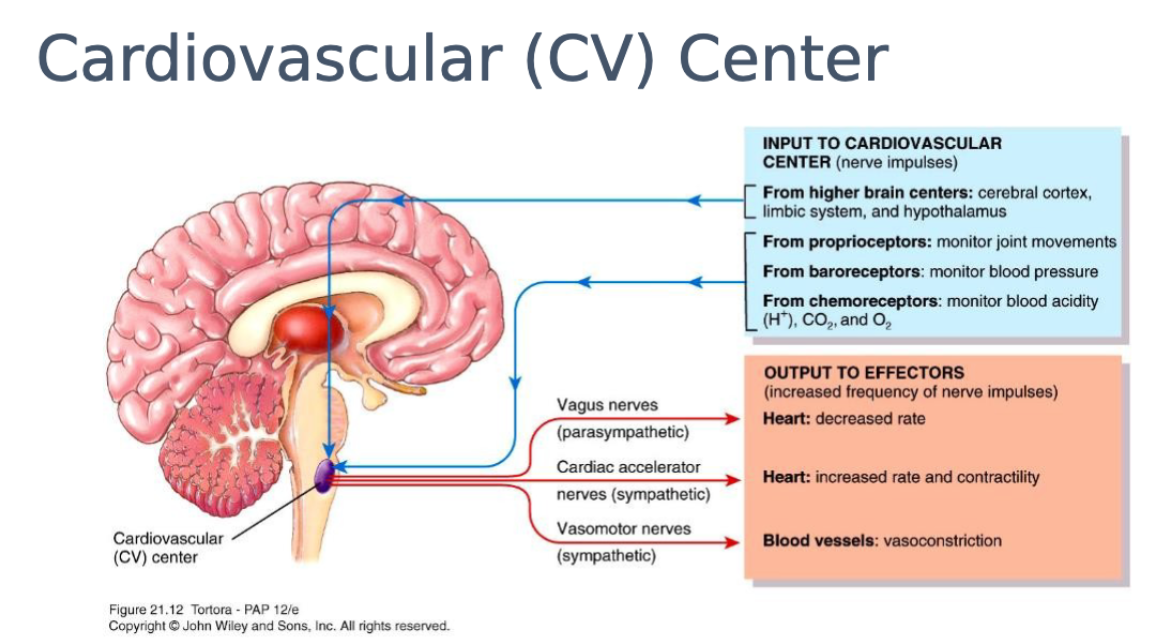
Receives both sympathetic and parasympathetic nerves; Modify heart rate and contraction strength
10
New cards
what establishes fundamental rhythm of the heartbeat
The SA node (APs start here and spread through rest of heart)
normal heartbeat: sinus rhythm
normal heartbeat: sinus rhythm
11
New cards
which nerves increase heart rate
sympathetic
12
New cards
which nerves decrease heart rate
parasympathetic
13
New cards
systole
Contraction of the heart
(occurs immediately following depolarization)
(occurs immediately following depolarization)
14
New cards
diastole
Relaxation of the heart
(occurs immediately following repolarization)
(occurs immediately following repolarization)
15
New cards
sinus rhythm
normal heart beat
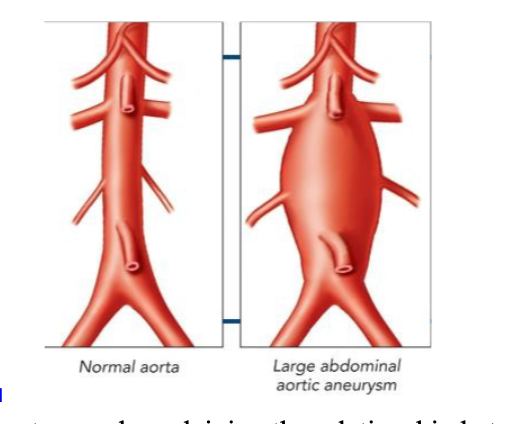
16
New cards
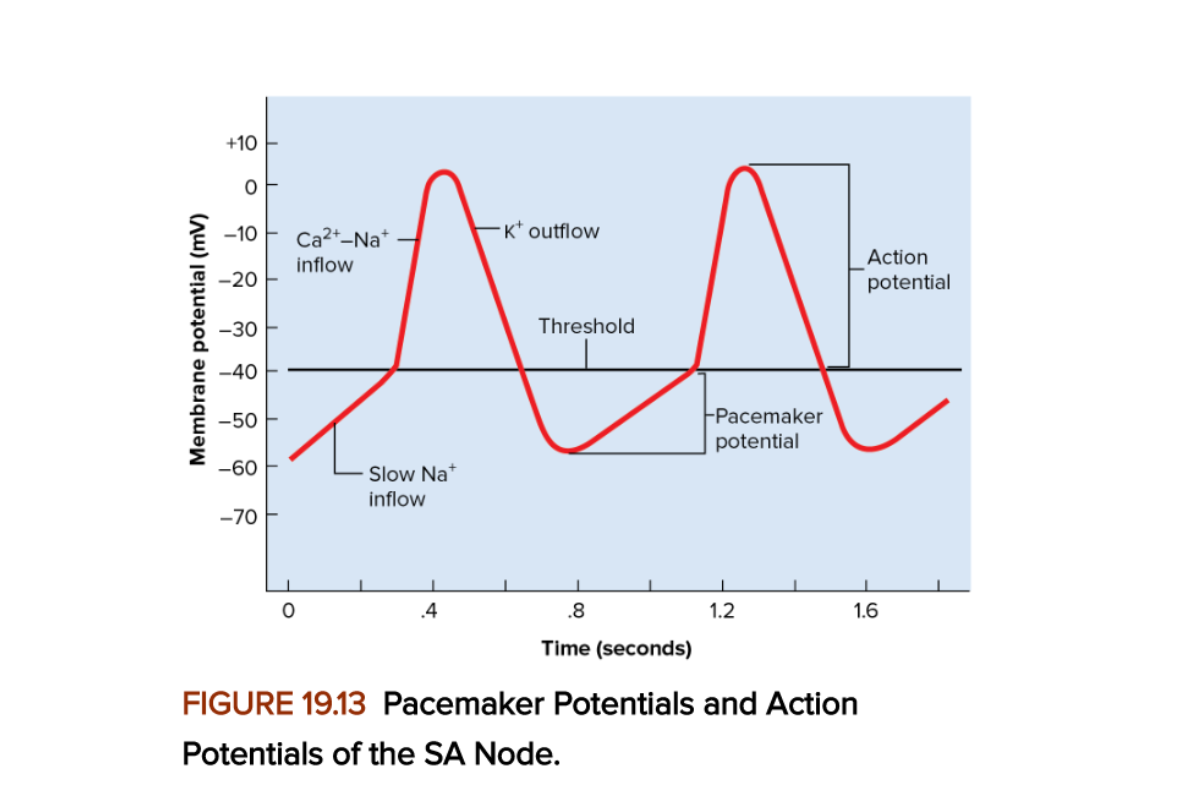
Explain why the SA node fires spontaneously and rhythmically
-The cells of the SA node do not have a stable resting membrane potential
-Their membrane potential starts at about -60mV and drifts upward, showing gradual depolarization called the pacemaker potential (prepotential)
-Results from slow inflow of Na+ without compensating outflow of K+
-Their membrane potential starts at about -60mV and drifts upward, showing gradual depolarization called the pacemaker potential (prepotential)
-Results from slow inflow of Na+ without compensating outflow of K+
17
New cards
Nodal APs
Pacemaker potential: due to Na+ channels opening and K+ channels closing
Depolarization: due to Ca2+ influx
Repolarization: Ca2+ channels inactivate, K+ channels open, K+ rushes out
Depolarization: due to Ca2+ influx
Repolarization: Ca2+ channels inactivate, K+ channels open, K+ rushes out
18
New cards
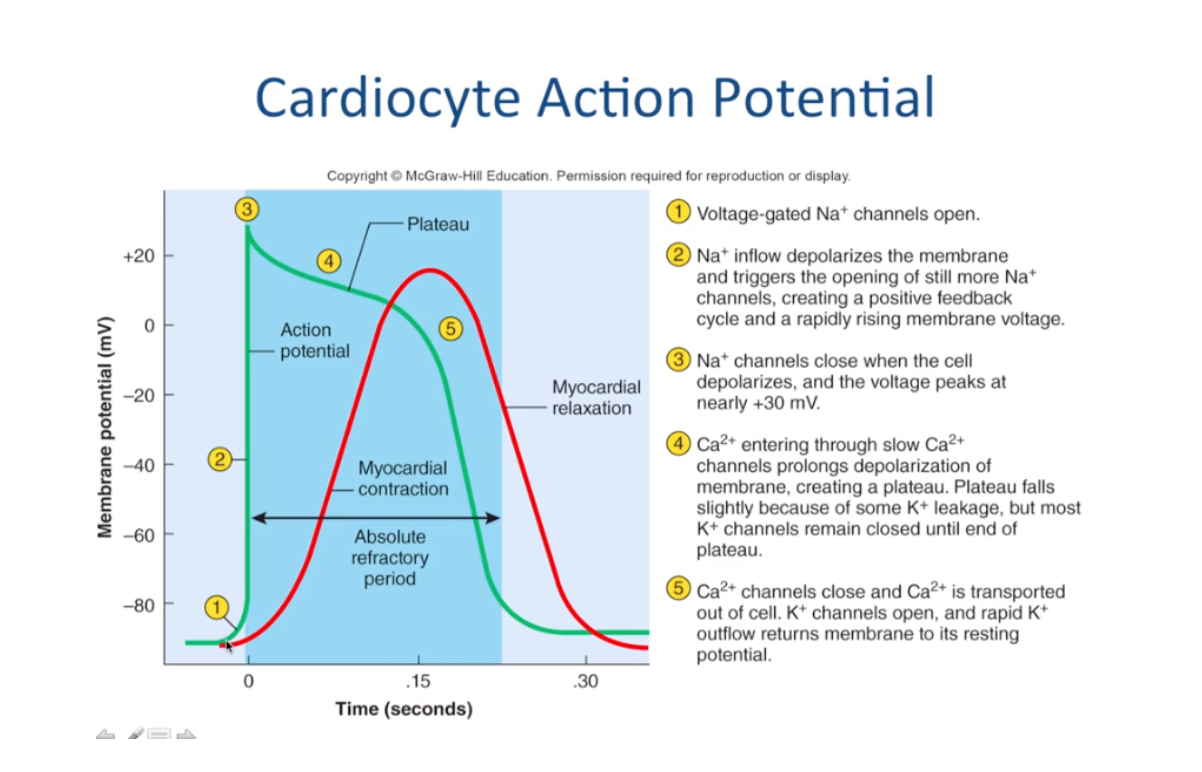
cardiocyte action potential
voltage gated Na+ channels open (depolarization)
Ca2+ channels prolong depolarization of membrane (plateau)
Ca2+ channels close and K+ channels open, rapid K+ outflow (repolarization)
Ca2+ channels prolong depolarization of membrane (plateau)
Ca2+ channels close and K+ channels open, rapid K+ outflow (repolarization)
19
New cards
significance of plateau phase
-allows for longer muscle contraction (allows heart to contract in a steady, uniform, and forceful manner)
-very long refractory period: prevents tetanus in the heart
-very long refractory period: prevents tetanus in the heart
20
New cards
electrocardiogram (ECG)
recording of the electrical changes that occur in the myocardium during a cardiac cycle
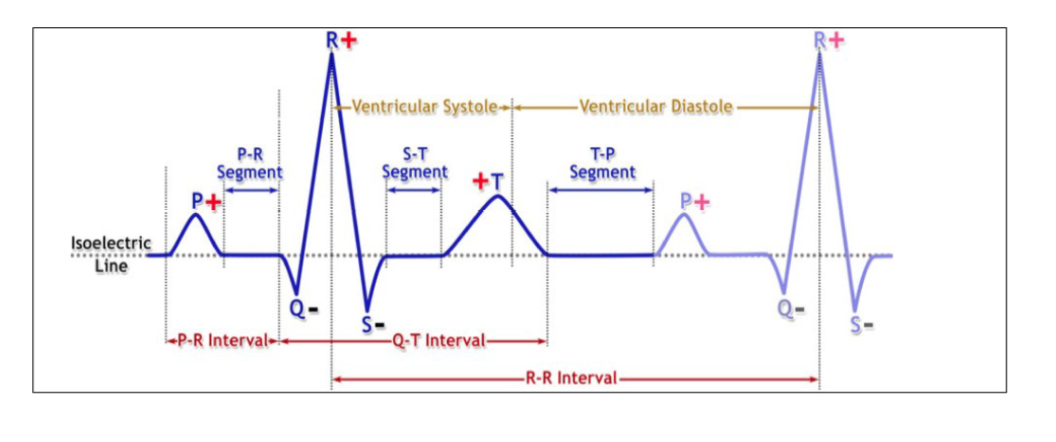
21
New cards
p wave
atrial depolarization
22
New cards
QRS interval
atrial repolarization
23
New cards
QRS complex
ventricular depolarization
24
New cards
T wave
ventricular repolarization
25
New cards
The activity of the conduction system
-Your heart (cardiac) conduction system sends the signal to start a heartbeat.
-It also sends signals that tell different parts of your heart to relax and contract (squeeze). -This process of contracting and relaxing
-It also sends signals that tell different parts of your heart to relax and contract (squeeze). -This process of contracting and relaxing
26
New cards
R-R on ECG
one full cardiac cycle
27
New cards
Arythmias
irregular heart rhythms
(due to defects in the conduction system)
(due to defects in the conduction system)
28
New cards
fibrillation
-'quivering' of the heart due to irregular contracts
-Heart loses effective pump
-Defibrillation by electrically shocking the heart to 'wipe the slate clean'
-Heart loses effective pump
-Defibrillation by electrically shocking the heart to 'wipe the slate clean'
29
New cards
How is blood pressure expressed?
millimeters of mercury (mmHg)
30
New cards
Describe how changes in blood pressure operate the heart valves
-Blood flow through the heart is controlled entirely by pressure changes
(High pressure to low pressure)
-Blood flows down a pressure gradient through any available opening
(The reason why valves are so important)
(High pressure to low pressure)
-Blood flows down a pressure gradient through any available opening
(The reason why valves are so important)
31
New cards
heart sounds
S1 and S2 'lupp-dupp'
Third heart sound (S3): heard in children and adolescents
(If heard in people over 30, may indicate an enlarged and failing heart)
Third heart sound (S3): heard in children and adolescents
(If heard in people over 30, may indicate an enlarged and failing heart)
32
New cards
S1
louder and longer
33
New cards
S2
softer and sharper
34
New cards
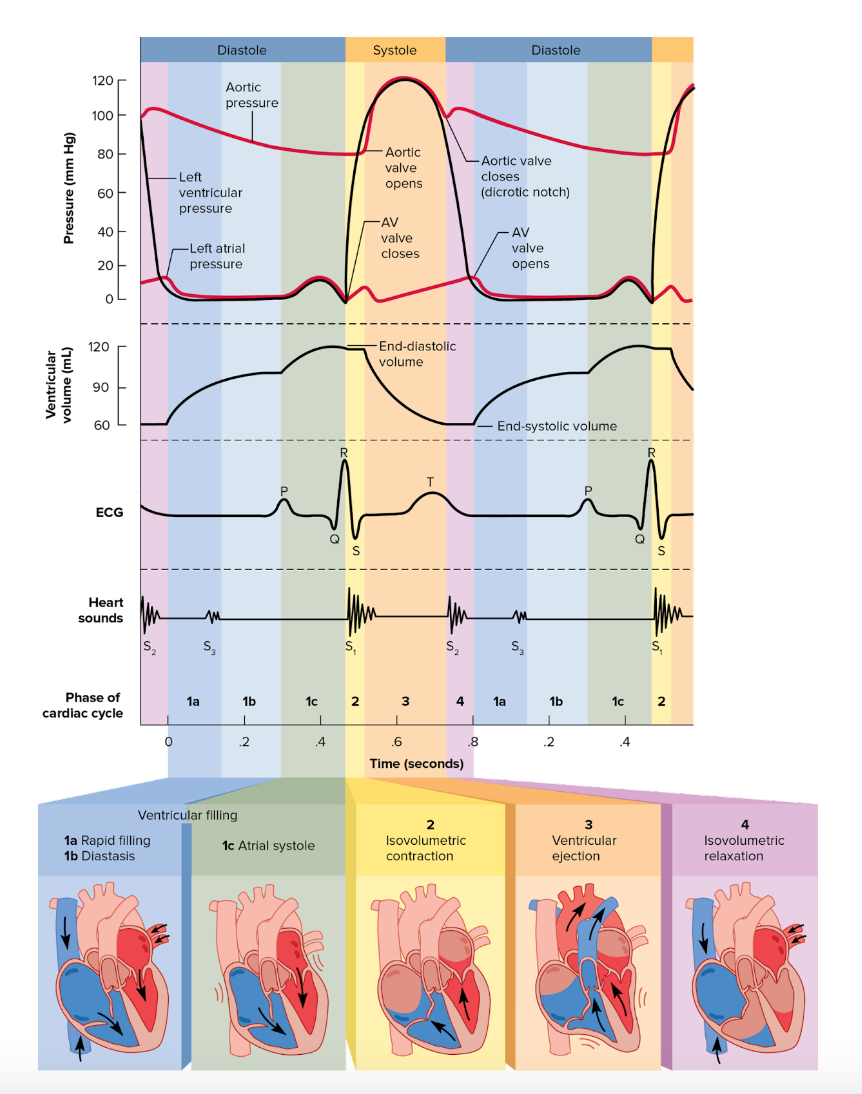
cardiac cycle
a series of pressure changes that occur in the heart
35
New cards
stroke volume (SV)
amount of blood expelled by ventricles (mL)
36
New cards
End Diastolic Volume (EDV)
the amount of blood that is in the ventricles before the heart contracts
2 factors determine EDV:
-Duration of ventricular diastole
-Venous return
2 factors determine EDV:
-Duration of ventricular diastole
-Venous return
37
New cards
End Systolic Volume (ESV)
volume remaining in ventricle at end of systole
38
New cards
stroke volume calculation
EDV-ESV
39
New cards
ventricular filling
-Atria relaxed, blood passively flows into the ventricle
-Depolarization of SA node
-Atria contract, ventricles are relaxed
-More blood fills the ventricles- end-diastolic volume
-Ventricles depolarize
-Atrial diastole
-Depolarization of SA node
-Atria contract, ventricles are relaxed
-More blood fills the ventricles- end-diastolic volume
-Ventricles depolarize
-Atrial diastole
40
New cards
isovolumetric contraction
-Ventricular depolarization causes systole
-Ventricular pressure rises, forces AV valves to shut (now all 4 valves are closed)\-- isovolumetric contraction
-Heart sound S1
-Ventricular pressure rises, forces AV valves to shut (now all 4 valves are closed)\-- isovolumetric contraction
-Heart sound S1
41
New cards
ventricular ejection
-Pressure eventually great enough to force open semilunar valves, blood rushes into aorta and pulmonary trunk
(Stroke volume: volume ejected per beat from each ventricle
Ventricles will not expel all of their blood)
(Stroke volume: volume ejected per beat from each ventricle
Ventricles will not expel all of their blood)
42
New cards
isovolumetic relaxation
-Phase following the T wave
-Ventricles relax, small amount of blood remains
-Ventricular pressure drops, semilunar valves close
--Dicrotic notch: backflow of blood rebounding off aortic SL valve
-During ventricular systole and diastole, atria have been in diastole and filling with blood
--When blood pressure rises high enough, AV valves forced open, ventricular filling begins again
-Ventricles relax, small amount of blood remains
-Ventricular pressure drops, semilunar valves close
--Dicrotic notch: backflow of blood rebounding off aortic SL valve
-During ventricular systole and diastole, atria have been in diastole and filling with blood
--When blood pressure rises high enough, AV valves forced open, ventricular filling begins again
43
New cards
Wiggers Diagram
44
New cards
how is atrial systole related to ventricular filling
Atrial contraction (atrial systole) ejects blood from the atrium and into the ventricle, which is still in diastole, and this completes ventricular filling
45
New cards
AV valves open
atrial pressure greater than ventricular pressure
46
New cards
AV valves close
atrial pressure less than ventricular pressure
47
New cards
SL valves open
pulmonary valve pressure is greater than the aorta and pulmonary trunk
48
New cards
SL valves close
Pulmonary valve pressure is less than aorta and Pulmonary trunk.
49
New cards
Relate the heart sounds to the events of the cardiac cycle
S1- AV valves closing
S2- closing of SL valves
S2- closing of SL valves
50
New cards
Relate the events of the cardiac cycle to the volume of blood entering and leaving the heart.
Ventricular filling: increase of blood in heart
Isovolumetric contraction: decrease of blood in heart
Ventricular ejection: decrease of blood in heart
Isovolumetric relaxation: increase of blood in heart
Isovolumetric contraction: decrease of blood in heart
Ventricular ejection: decrease of blood in heart
Isovolumetric relaxation: increase of blood in heart
51
New cards
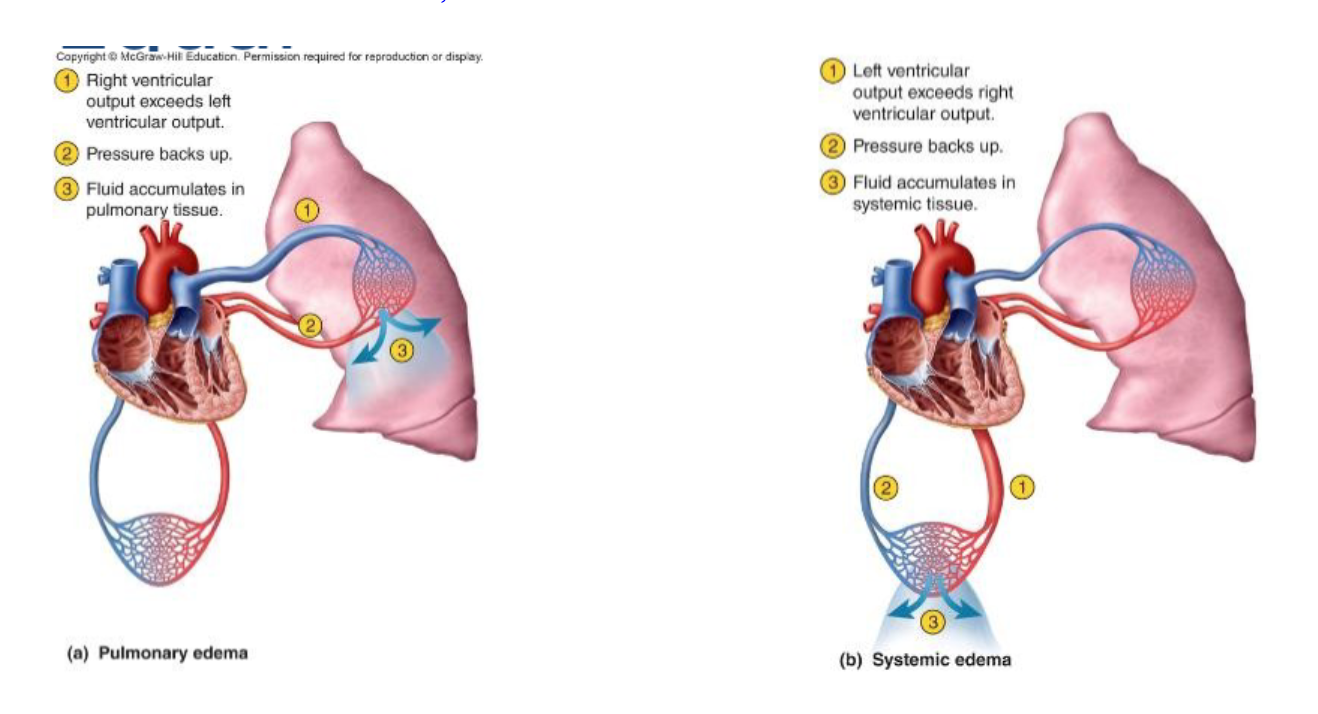
Why is it important that the right and left ventricles have the same stroke volume?
Stroke volumes must be equal
-Fluid accumulation in either circuit due to insufficiency of ventricular pumping leads to congestive heart failure
-Causes: congenital defects in cardiac anatomy, chronic hypertension, myocardial infarction, valvular defects
-Fluid accumulation in either circuit due to insufficiency of ventricular pumping leads to congestive heart failure
-Causes: congenital defects in cardiac anatomy, chronic hypertension, myocardial infarction, valvular defects
52
New cards
mitral valve prolapse (MVP)
improper closure of the mitral valve
(an insufficiency in which one or both mitral valve cusps bulge into the atrium during ventricular contraction)
-Often hereditary
-Affects about 1 in 40 people (especially women)
-Mainly causes no serious dysfunction but can cause chest pain, fatigue, shortness of breath
(an insufficiency in which one or both mitral valve cusps bulge into the atrium during ventricular contraction)
-Often hereditary
-Affects about 1 in 40 people (especially women)
-Mainly causes no serious dysfunction but can cause chest pain, fatigue, shortness of breath
53
New cards
congestive heart failure (CHF)
-fluid accumulation in either circuit due to insufficiency of ventricular pumping
-Common causes: myocardial infarction (MI), chronic hypertension, valvular defects, and congenital birth defects in cardiac anatomy
-Common causes: myocardial infarction (MI), chronic hypertension, valvular defects, and congenital birth defects in cardiac anatomy
54
New cards
left side CHF
(pulmonary edema)
Left ventricle fails to pump effectively, thus backup into the lungs
Left ventricle fails to pump effectively, thus backup into the lungs
55
New cards
right side CHF
systemic edema
Right ventricle fails to pump effectively, thus backup into RA and then into the periphery
Right ventricle fails to pump effectively, thus backup into RA and then into the periphery
56
New cards
Cardiac Output (CO)
:volume of blood ejected from a single ventricle each minute
-Helps keep blood pressure at needed levels and supply brain and vital organs with oxygen-rich blood
-Entire blood volume flows through pulmonary and systemic circuits each minute
-Helps keep blood pressure at needed levels and supply brain and vital organs with oxygen-rich blood
-Entire blood volume flows through pulmonary and systemic circuits each minute
57
New cards
cardiac reserve
difference between maximum cardiac output (CO) and CO at rest
-Average cardiac reserve 4-5 times resting value
-Train athletes can generate 7x resting value
-Average cardiac reserve 4-5 times resting value
-Train athletes can generate 7x resting value
58
New cards
Calculate cardiac output given stroke volume and heart rate.
Cardiac output \= stroke volume (SV) x heart rate (HR)
59
New cards
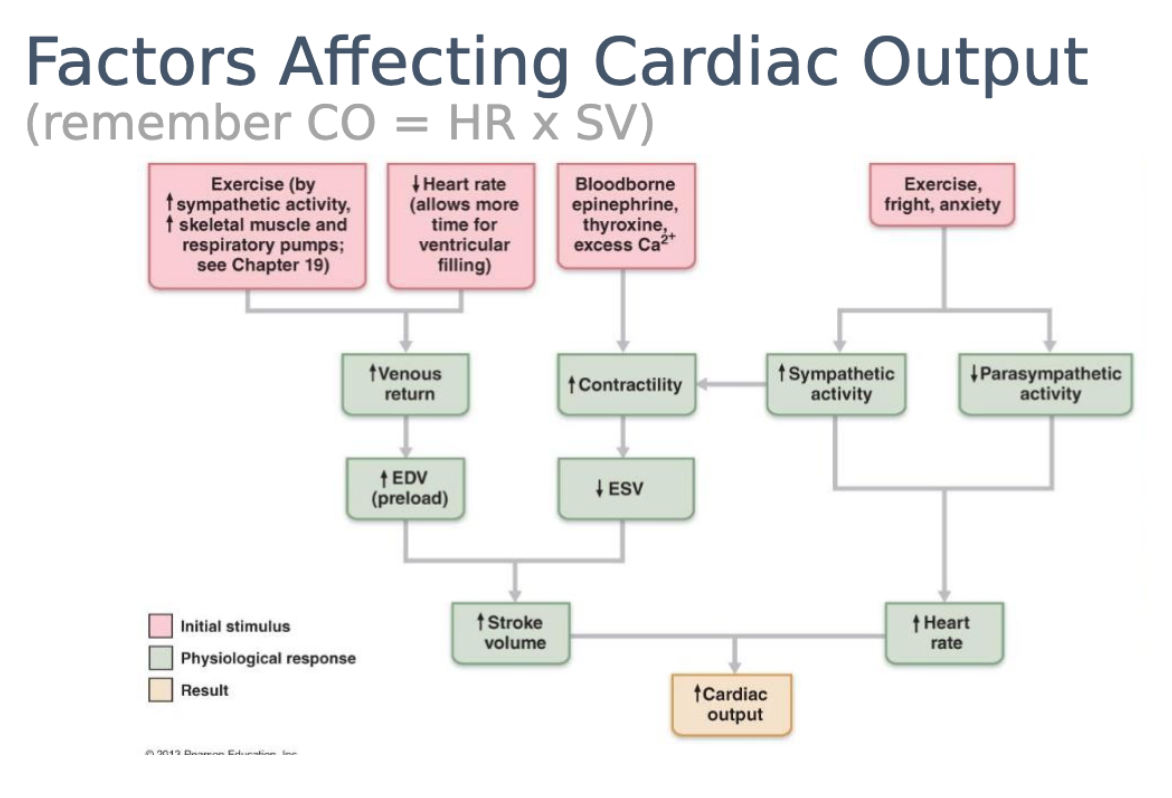
how changes in HR and SV affect CO
Increased heart rate or stroke volume or both will increase cardiac output
Decreased heart rate or stroke volume or both will decrease cardiac output
Decreased heart rate or stroke volume or both will decrease cardiac output
60
New cards
regulation of stroke volume
Preload
Contractility (inotropic agents)
Afterload
Contractility (inotropic agents)
Afterload
61
New cards
Tachycardia
persistent, resting adult heart rate above 100 bpm
(fast heart rate)
(fast heart rate)
62
New cards
bradycardia
persistent, resting adult heart rate below 60 bpm
(slow heart rate)
(slow heart rate)
63
New cards
vagal tone
steady background firing rate of vagus nerves that holds the heart rate down to its usual 70 to 80 bpm at rest (heart naturally beats around 100 bpm)
64
New cards
Procioceptors
in the muscle and joints provide information on changes in physical activity
65
New cards
Baroreceptors
pressure sensors in the aorta and internal carotid arteries
(detect changes in blood pressure)
(detect changes in blood pressure)
66
New cards
chemoreceptors
occur in the aortic arch, carotid arteries, and medulla oblongata
Sensitive to blood pH, CO2 and O2 levels
(More important in respiratory control, but they do influence heart rate)
Sensitive to blood pH, CO2 and O2 levels
(More important in respiratory control, but they do influence heart rate)
67
New cards
positive chronotropic agents
increase heart rate
-Sympathetic nervous system
-Epinephrine, norepinephrine
-Thyroid hormone
-Glucagon
-Nicotine, caffeine
-Hypocalcemia
-Sympathetic nervous system
-Epinephrine, norepinephrine
-Thyroid hormone
-Glucagon
-Nicotine, caffeine
-Hypocalcemia
68
New cards
negative chronotropic agents
-decrease heart rate
-Parasympathetic nervous system
-Acetylcholine
-Hypercalcemia
-Hypokalemia
-Beta blockers
-Parasympathetic nervous system
-Acetylcholine
-Hypercalcemia
-Hypokalemia
-Beta blockers
69
New cards
How would potassium or calcium excess or deficiency affect heart rate?
Excess of deficiency of calcium or potassium would lead to irregular heart beats
70
New cards
preload
degree of stretch on the heart before it contracts
71
New cards
Frank-Starling Law of the Heart
the more the heart fills with blood during diastole, the greater the force of contraction during systole
Preload is proportional to end-diastolic volume (EDV)
Preload is proportional to end-diastolic volume (EDV)
72
New cards
venous return
the volume of blood that returns from the veins to the atria each minute
73
New cards
how does venous return effect preload
Increase in venous return → increase in preload (increase in preload will increase the force at which the heart contracts)
74
New cards
Contractility
strength of contraction at any given preload/muscle length
(Positive inotropic agents: increases contractility
Negative inotropic agents: decreases contractility)
(Positive inotropic agents: increases contractility
Negative inotropic agents: decreases contractility)
75
New cards
positive iontropic agents
increases stroke volume
-Increased preload (myocardial stretch)
-Increased contractility
-Sympathetic nervous system
-Epinephrine, norepinephrine
-Glucagon
-Digitalis
-Nicotine, caffeine
-Hypercalcemia
--Often promote Ca2+ inflow during cardiac AP
-Increased preload (myocardial stretch)
-Increased contractility
-Sympathetic nervous system
-Epinephrine, norepinephrine
-Glucagon
-Digitalis
-Nicotine, caffeine
-Hypercalcemia
--Often promote Ca2+ inflow during cardiac AP
76
New cards
negative iontropic agents
decreases stroke volume
-Reduced preload
-Reduced contractility
-Increased afterload
-Hypocalcemia
--Often decrease available Ca2+
--Calcium channel blockers
-Hyperkalemia
--Increased K+ in interstitial fluid
-Reduced preload
-Reduced contractility
-Increased afterload
-Hypocalcemia
--Often decrease available Ca2+
--Calcium channel blockers
-Hyperkalemia
--Increased K+ in interstitial fluid
77
New cards
calcium effect on stroke volume
excess calcium (hypercalcemia) causes a slow heartbeat, increasing stroke volume. Calcium deficiency (hypocalcemia) causes an increased heart rate, decreasing the stroke volume
78
New cards
potassium effect on stroke volume
excess potassium (hyperkalemia) causes the heart rate to become slow and irregular, increasing the stroke volume
79
New cards
afterload
pressure (resistance in arteries) that must be overcome before semilunar valves can open
(Increase in afterload causes stroke volume to decrease)
(Hypertension and atherosclerosis increase afterload)
(Increase in afterload causes stroke volume to decrease)
(Hypertension and atherosclerosis increase afterload)
80
New cards
Identify the factors that govern cardiac output.
Heart rate, contractility, preload, afterload
81
New cards
cardiovascular center
area of the medulla at which stimulation will activate the sympathetic nervous system to increase blood pressure, heart rate, and the parasympathetic to decrease heart rate
82
New cards
Atrial (Bainbridge) reflex
Due to respiration (deep breathing) increases thoracic pressure which Increases venous return, atria stretch to accommodate blood, this causes increases in heart rate
(An increase in heart rate due to an increase in central venous pressure)
(An increase in heart rate due to an increase in central venous pressure)
83
New cards
Describe some effects of exercise on cardiac output.
-Increases cardiac output
-Muscular activity increases venous return (increasing the preload on the right ventricle and left ventricle)
-Increases heart rate and stroke volume
-Muscular activity increases venous return (increasing the preload on the right ventricle and left ventricle)
-Increases heart rate and stroke volume
84
New cards
factors affecting cardiac output
85
New cards
blood pressure (BP)
the force exerted by blood on a vessel wall
-Measured with a sphygmomanometer
-Depends on: cardiac output, resistance, blood volume
-Measured with a sphygmomanometer
-Depends on: cardiac output, resistance, blood volume
86
New cards
resistance
-Due to viscosity, length, and diameter
-Most important variable as it can change easily due to changes in vessel diameter
-Most important variable as it can change easily due to changes in vessel diameter
87
New cards
vascular resistance
-Opposition to blood flow due to friction between blood and walls of blood vessels
-Vessel diameter
-Blood viscosity
--Ratio of RBCs to plasma and protein concentration
-Total blood vessel length
--400 miles of additional blood vessels for each 2.2lb of fat
-Vessel diameter
-Blood viscosity
--Ratio of RBCs to plasma and protein concentration
-Total blood vessel length
--400 miles of additional blood vessels for each 2.2lb of fat
88
New cards
flow
amount of blood flowing through an organ, tissue or blood vessel in a give time
-Volume of blood \= cardiac output
-CO \= HR x SV
-Volume of blood \= cardiac output
-CO \= HR x SV
89
New cards
flow equation
Flow \= change in pressure/resistance
90
New cards
relationship between flow, change in pressure, and resistance
-Flow is directly proportional to change in pressure (increase in ΔP increases flow)
-Flow is disproportional to resistance (increase in resistance decreases flow)
-Flow is disproportional to resistance (increase in resistance decreases flow)
91
New cards
mean arterial pressure (MAP)
-Mean arterial pressure (MAP)
--Not equal to the mean of systolic and diastolic pressure because diastole lasts longer than systole
-Pulse pressure \= systolic - diastolic pressure
-MAP \= diastolic pressure + ⅓ pulse pressure
--Not equal to the mean of systolic and diastolic pressure because diastole lasts longer than systole
-Pulse pressure \= systolic - diastolic pressure
-MAP \= diastolic pressure + ⅓ pulse pressure
92
New cards
systolic pressure
generated by contraction (systole) of the left ventricle
93
New cards
diastolic pressure
the minimum to which the BP falls when the ventricle in diastole
94
New cards
pulse pressure
difference between systolic and diastolic pressure
95
New cards
blood viscosity (factor that affects resistance)
-Stems mainly from its plasma proteins (albumin) and erythrocytes
-A deficiency of erythrocytes (anemia) or albumin (hypoproteinemia) reduces viscosity and speeds up blood flow
-A deficiency of erythrocytes (anemia) or albumin (hypoproteinemia) reduces viscosity and speeds up blood flow
96
New cards
vessel length (factor that affects resistance)
the greater the vessel length, the less pressure and flow
97
New cards
vessel radius (factor that affects resistance)
-Effects of radius on blood flow stems from the friction of the moving blood against the vessels walls
-Blood usually exhibits smooth, silent laminar flow
-Large vessel radius \= average velocity of flow is high
-Small vessel radius \= lower average velocity
-Blood usually exhibits smooth, silent laminar flow
-Large vessel radius \= average velocity of flow is high
-Small vessel radius \= lower average velocity
98
New cards
angiogenesis
Angio \= blood vessel; genesis \= creation
(Important process in embryonic development as well as postnatal wound healing, etc.)
(Important process in embryonic development as well as postnatal wound healing, etc.)
99
New cards
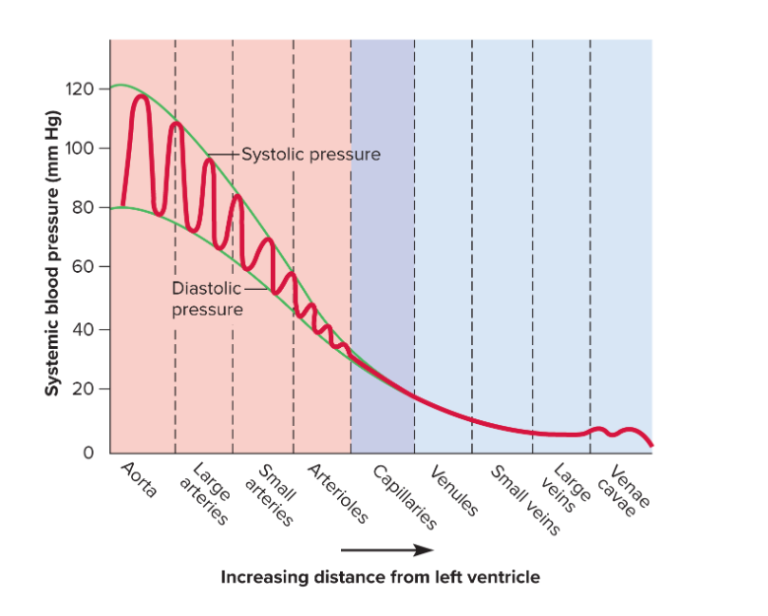
changes in blood pressure relative to distance from heart
Systolic and diastolic pressures are lower and there is less difference between them when they are farther away from the heart
(There is no pulse pressure beyond the arterioles)
(There is no pulse pressure beyond the arterioles)
100
New cards
importance of blood pressure homeostasis
too low: inadequate perfusion of body tissues (ischemia, necrosis)
too high: blood vessel damage (increased risk of aneurysms
too high: blood vessel damage (increased risk of aneurysms