BIOS 3755 Exam 3
0.0(0)
Card Sorting
1/202
Earn XP
Description and Tags
Last updated 1:51 PM on 12/9/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
203 Terms
1
New cards
Which one of the choices is NOT derived from multipotent uncommitted Hematopoietic Stem Cell (HSC)?
- Platelets
- Red blood cells
- T lymphocytes
- B lymphocytes
- Platelets
- Red blood cells
- T lymphocytes
- B lymphocytes
- All of them are derived from stem cells; in fact, a single HSC can reconstitute an entire immune and blood system upon transplant after irradiation
2
New cards
***Compare and contrast the organization/function of circulatory systems: open, closed, single, and double systems***
- Open
- Open
- Blood bathes the organs directly (circulatory fluid is interstitial fluid); blood = interstitial fluid
- Heart opens directly into sinuses that are filled with blood
- May or may not exchange oxygen
--> Has oxygen-carrying pigment but not contained within cells; it's free in the hemolymph
- No oxygen exchange/delivery to cells in insect circulatory system
--> There's a separate system of tubes that reach the cells
- Pump and open tube mechanism
--> Tube is only for open nutrients and removal of wastes
- Low pressure = less energy cost
- Heart opens directly into sinuses that are filled with blood
- May or may not exchange oxygen
--> Has oxygen-carrying pigment but not contained within cells; it's free in the hemolymph
- No oxygen exchange/delivery to cells in insect circulatory system
--> There's a separate system of tubes that reach the cells
- Pump and open tube mechanism
--> Tube is only for open nutrients and removal of wastes
- Low pressure = less energy cost
3
New cards
***Compare and contrast the organization/function of circulatory systems: open, closed, single, and double systems***
- Closed
- Closed
- Blood...
--> Is confined (only found in) to vessels
--> Is distinct from interstitial fluid
-----> Blood and extracellular fluid are 2 separate entities
--> Transports oxygen and carbon dioxide
- Multiple hearts and no lungs in annelid circulatory system
- Gas exchange occurs only through capillaries
- High pressure = more energy cost
- Types: single and double circulation
--> Is confined (only found in) to vessels
--> Is distinct from interstitial fluid
-----> Blood and extracellular fluid are 2 separate entities
--> Transports oxygen and carbon dioxide
- Multiple hearts and no lungs in annelid circulatory system
- Gas exchange occurs only through capillaries
- High pressure = more energy cost
- Types: single and double circulation
4
New cards
***Compare and contrast the organization/function of circulatory systems: open, closed, single, and double systems***
- Single
- Single
- Bony fish, rays, and sharks have single circulation with a 2-chambered heart
- Blood leaving the heart passes through 2 capillary beds before returning
- Problem: Trusting a low pressure fluid movement to push blood throughout the entire system; have to go through the whole system without resupplying
- Blood leaving the heart passes through 2 capillary beds before returning
- Problem: Trusting a low pressure fluid movement to push blood throughout the entire system; have to go through the whole system without resupplying
5
New cards
***Compare and contrast the organization/function of circulatory systems: open, closed, single, and double systems***
- Double
- Double
- Amphibians, reptiles, and mammals
--> Amphibians (3 chambered hearts) have pulmonary return to left atrium (as in mammals) but deoxygenated blood mixes with oxygenated blood in single ventricle
--> Reptiles (Improved 3 chambered hearts) have a septum partially separating the ventricle, which improves separation of pulmonary and systemic circulation
--> Birds and mammals (4 chambered hearts) achieve complete separation of pulmonary and systemic circulation
-----> Provides high rate of oxygen delivery to tissues and corresponding higher levels of activity
- Systemic and pulmonary circulation are partially separated
--> Oxygen-poor blood flows through the pulmonary circuit to pick up oxygen through the lungs
--> Oxygen-rich blood delivers oxygen through the systemic circuit
- Solved the problem of pressure
- Still have the problem of not mixing blood in some organisms
--> Amphibians (3 chambered hearts) have pulmonary return to left atrium (as in mammals) but deoxygenated blood mixes with oxygenated blood in single ventricle
--> Reptiles (Improved 3 chambered hearts) have a septum partially separating the ventricle, which improves separation of pulmonary and systemic circulation
--> Birds and mammals (4 chambered hearts) achieve complete separation of pulmonary and systemic circulation
-----> Provides high rate of oxygen delivery to tissues and corresponding higher levels of activity
- Systemic and pulmonary circulation are partially separated
--> Oxygen-poor blood flows through the pulmonary circuit to pick up oxygen through the lungs
--> Oxygen-rich blood delivers oxygen through the systemic circuit
- Solved the problem of pressure
- Still have the problem of not mixing blood in some organisms
6
New cards
***Describe and identify the functions of the different components of blood***
- Plasma + cells and components
--> Plasma has dissolved...
-----> Proteins: purpose is to generate osmotic differences
--------> Carrier proteins
--------> Antibodies
-----> Nutrients
-----> Inorganic substances
-----> Metabolic wastes
--------> Urea
-----> Hormones
--> Cells and components include...
-----> Red blood cells (erythrocytes), more than 99%
--------> Made in bone marrow
--------> Enucleated
--------> 120 day life cycle
--------> About 1% of red blood cells are renewed every day
--------> Billrubin is generated when broken down (gives yellow color to urine)
--------> Most Fe is recycled back to bone marrow
--------> Lack of sufficient red blood cells causes anemia
-----------> Sickle-cell anemia
---------------> Abnormal hemoglobin that makes red blood cells sickle-shaped (both copies of DNA have the sickle-cell gene), making it less efficient
-----------> Iron deficiency
-----------> Bone marrow failure
-----------> Hemorrhage
-----------> Blood cell production issues
-----> White blood cells (leukocytes)
--------> Made in bone marrow
--------> Key part in immunity
--------> Have nuclei
--------> Numbers and types can hint at infections
-----> Platelets
- Luminol
--> Reacts with Fe in hemoglobin in red blood cells to fluoresce under black light
- Hematocrit
--> 45% of blood volume that is red blood cells (i.e. erythrocytes)
--> 55% is plasma
--> The rest is leukocytes and platelets, making a buffy coat
--> Plasma has dissolved...
-----> Proteins: purpose is to generate osmotic differences
--------> Carrier proteins
--------> Antibodies
-----> Nutrients
-----> Inorganic substances
-----> Metabolic wastes
--------> Urea
-----> Hormones
--> Cells and components include...
-----> Red blood cells (erythrocytes), more than 99%
--------> Made in bone marrow
--------> Enucleated
--------> 120 day life cycle
--------> About 1% of red blood cells are renewed every day
--------> Billrubin is generated when broken down (gives yellow color to urine)
--------> Most Fe is recycled back to bone marrow
--------> Lack of sufficient red blood cells causes anemia
-----------> Sickle-cell anemia
---------------> Abnormal hemoglobin that makes red blood cells sickle-shaped (both copies of DNA have the sickle-cell gene), making it less efficient
-----------> Iron deficiency
-----------> Bone marrow failure
-----------> Hemorrhage
-----------> Blood cell production issues
-----> White blood cells (leukocytes)
--------> Made in bone marrow
--------> Key part in immunity
--------> Have nuclei
--------> Numbers and types can hint at infections
-----> Platelets
- Luminol
--> Reacts with Fe in hemoglobin in red blood cells to fluoresce under black light
- Hematocrit
--> 45% of blood volume that is red blood cells (i.e. erythrocytes)
--> 55% is plasma
--> The rest is leukocytes and platelets, making a buffy coat
7
New cards
3 essential components of true circulatory systems (open or closed)
- Includes
1. Pump
2. Vessels
3. Blood
- Requirements
1. Circulatory fluid for nutrients and/or gas exchange
2. Set of tubes for fluid transport
3. Muscular pump for fluid movement
1. Pump
2. Vessels
3. Blood
- Requirements
1. Circulatory fluid for nutrients and/or gas exchange
2. Set of tubes for fluid transport
3. Muscular pump for fluid movement
8
New cards
Human circulatory system is...
Closed
9
New cards
Only ___ blood cells have DNA in them
White (NO RED!!!)
10
New cards
What is the adaptive advantage of having a double circulation and three-chambered heart of amphibians, over the single circuit and two-chambered heart of fish?
Oxygenated blood can return to the heart for additional pumping before going to systemic flow (i.e. the main purpose of having double circulation)
11
New cards
Pulmonary circuit
Flow to/from lungs
12
New cards
Systemic circuit
Flow to/from rest of body
13
New cards
Arteries
Vessels carrying blood away from the heart; high pressure towards capillaries
14
New cards
Veins
Vessels carrying blood towards the heart; low pressure from capillaries
15
New cards
Capillaries
Tiny, thin-walled vessels connecting arterioles to venules; capillaries have slow blood flow and low blood pressure to permit gas/nutrient exchange between blood and interstitial fluid
16
New cards
Fish circulatory system
- 1 circuit
- 2-chambered heart (single atrium and single ventricle)
- Blood leaving the heart passes through both gill and systemic capillaries before going back to heart
- Drawback: you have to go through whole circuit without an extra push
- Some fish have lungs that have 2 atrium and 1 ventricle (lungfish)
--> 1 receives oxygenated blood from lung, other deoxygenated blood from body
--> Body mixes
- 2-chambered heart (single atrium and single ventricle)
- Blood leaving the heart passes through both gill and systemic capillaries before going back to heart
- Drawback: you have to go through whole circuit without an extra push
- Some fish have lungs that have 2 atrium and 1 ventricle (lungfish)
--> 1 receives oxygenated blood from lung, other deoxygenated blood from body
--> Body mixes
17
New cards
Amphibian circulatory system
- 2 circuit
- 3-chambered heart
--> 2 atrium and 1 ventricle
- 1st evolution of separating the pulmonary and systemic circuits
--> This separation allows for deoxygenated blood and oxygenated blood to mix less
- In amphibians, the pulmonary and systemic circuits are partially separated
--> Have pulmonary return to left atrium (as in mammals) but deoxygenated blood mixes with oxygenated blood in single ventricle
- 3-chambered heart
--> 2 atrium and 1 ventricle
- 1st evolution of separating the pulmonary and systemic circuits
--> This separation allows for deoxygenated blood and oxygenated blood to mix less
- In amphibians, the pulmonary and systemic circuits are partially separated
--> Have pulmonary return to left atrium (as in mammals) but deoxygenated blood mixes with oxygenated blood in single ventricle
18
New cards
Turtles, lizards, snakes (reptiles) circulatory system
- 2 circuit
- 3-chambered improved heart
- The reptilian ventricle is party divided by a septum to direct oxygenated blood to the body and the deoxygenated blood to the lungs; still some mixing, but the ventricles are starting to separate more
--> Improves separation of pulmonary and systemic circulation
- 3-chambered improved heart
- The reptilian ventricle is party divided by a septum to direct oxygenated blood to the body and the deoxygenated blood to the lungs; still some mixing, but the ventricles are starting to separate more
--> Improves separation of pulmonary and systemic circulation
19
New cards
Crocodilians circulatory system
- 2 circuit
- 4-chambered heart
- 4-chambered heart
20
New cards
Bird circulatory system
- 2 circuit
--> 2 pumps that operate in parallel
- 4-chambered heart
- Birds and mammals have 4-chambered hearts; their pulmonary and systemic circuits are totally separate
--> System provides high rate of oxygen delivery to tissues and corresponds to higher levels of activity
--> No mixing of oxygenated and deoxygenated
- Pulmonary circuit = blood goes to lung
- Systemic circuit = blood goes to body
--> 2 pumps that operate in parallel
- 4-chambered heart
- Birds and mammals have 4-chambered hearts; their pulmonary and systemic circuits are totally separate
--> System provides high rate of oxygen delivery to tissues and corresponds to higher levels of activity
--> No mixing of oxygenated and deoxygenated
- Pulmonary circuit = blood goes to lung
- Systemic circuit = blood goes to body
21
New cards
Mammal circulatory system
- 2 circuit
--> 2 pumps that operate in parallel
- 4-chambered heart
- Birds and mammals have 4-chambered hearts; their pulmonary and systemic circuits are totally separate
--> System provides high rate of oxygen delivery to tissues and corresponds to higher levels of activity
--> No mixing of oxygenated and deoxygenated
- Pulmonary circuit = blood goes to lung
- Systemic circuit = blood goes to body
- Mammalian cardiovascular system
--> Veins carry blood into the heart under low pressure from capillaries
--> Arteries carry blood away from the heart under high pressure towards capillaries
--> Capillaries have slower blood flow and lower blood pressure and permit gas/nutrient exchange between blood and interstitial fluid
- Mammalian hearts are 2 pumps operating in parallel
--> Right side of the heart receives venous blood from systemic circulation and pumps it to the lungs (pulmonary part)
--> Left side of the heart receives venous blood from the lungs and pumps it to the body (systemic part)
--> 2 pumps that operate in parallel
- 4-chambered heart
- Birds and mammals have 4-chambered hearts; their pulmonary and systemic circuits are totally separate
--> System provides high rate of oxygen delivery to tissues and corresponds to higher levels of activity
--> No mixing of oxygenated and deoxygenated
- Pulmonary circuit = blood goes to lung
- Systemic circuit = blood goes to body
- Mammalian cardiovascular system
--> Veins carry blood into the heart under low pressure from capillaries
--> Arteries carry blood away from the heart under high pressure towards capillaries
--> Capillaries have slower blood flow and lower blood pressure and permit gas/nutrient exchange between blood and interstitial fluid
- Mammalian hearts are 2 pumps operating in parallel
--> Right side of the heart receives venous blood from systemic circulation and pumps it to the lungs (pulmonary part)
--> Left side of the heart receives venous blood from the lungs and pumps it to the body (systemic part)
22
New cards
Veins always carry deoxygenated blood
- False
- Pulmonary arteries carry deoxygenated blood
- Pulmonary veins do the opposite job of your pulmonary arteries; they collect oxygen-rich blood and carry it from your lungs to your heart
- No other vein will be as oxygenated as this one ^
- Pulmonary arteries carry deoxygenated blood
- Pulmonary veins do the opposite job of your pulmonary arteries; they collect oxygen-rich blood and carry it from your lungs to your heart
- No other vein will be as oxygenated as this one ^
23
New cards
___ ventricle has the thickest wall
Left; sends blood all the way to the body
24
New cards
Systole
- Contraction of the ventricles/chambers of the heart to drive blood into the aorta and pulmonary artery
- Ventricles contract (AV valves shut) at the start of systole and relax (semi-lunar valves shut) at the end of systole
--> Shutting of AV valves gives a LUB sound
--> Shutting of semi-lunar valves gives a DUB sound
- At the end of systole, you have a drop in pressure in the left ventricle (as it's pumped into the aorta)
- Ventricles contract (AV valves shut) at the start of systole and relax (semi-lunar valves shut) at the end of systole
--> Shutting of AV valves gives a LUB sound
--> Shutting of semi-lunar valves gives a DUB sound
- At the end of systole, you have a drop in pressure in the left ventricle (as it's pumped into the aorta)
25
New cards
Diastole
- Relaxation of ventricles
- Will result in increase in volume of blood in left ventricle
- Will result in increase in volume of blood in left ventricle
26
New cards
One-Way valves
- Flaps of connective tissue that prevents backflow of blood when the cardiac cycle is in sequence of contraction (pumping the heart) and relaxation (filling the heart)
- Thus throughout systole, blood only flows in 1 direction
- 4 one-way valves in the circulatory system
--> 2 atrioventricular ones that close during systole to prevent backflow of blood from ventricles into the atria during ventricular contraction
--> 2 semilunar valves that close at the beginning of diastole to prevent backflow of blood from arteries into the ventricles
- Thus throughout systole, blood only flows in 1 direction
- 4 one-way valves in the circulatory system
--> 2 atrioventricular ones that close during systole to prevent backflow of blood from ventricles into the atria during ventricular contraction
--> 2 semilunar valves that close at the beginning of diastole to prevent backflow of blood from arteries into the ventricles
27
New cards
Mammalian heart: pulmonary and systemic circulation
- Pulmonary
1. Blood returns to heart from body, enters right atrium
2. Blood enters right ventricle
3. Blood is pumped from right ventricle to lungs
4. Blood returns to left atrium from lungs
- Systemic
4. Blood returns to left atrium from lungs
5. Blood enters left ventricle
6. Blood is pumped from left ventricle to body
1. Blood returns to heart from body, enters right atrium
1. Blood returns to heart from body, enters right atrium
2. Blood enters right ventricle
3. Blood is pumped from right ventricle to lungs
4. Blood returns to left atrium from lungs
- Systemic
4. Blood returns to left atrium from lungs
5. Blood enters left ventricle
6. Blood is pumped from left ventricle to body
1. Blood returns to heart from body, enters right atrium
28
New cards
There are no values at the point where venous blood flows into the atria (i.e. veins into the atria)
True
29
New cards
Atrioventricular valves
- One-way valves that separate atria (upper part of the heart) from ventricles and prevent blood from flowing backward into atria during ventricular contraction
- Right and left AV valves
- Right and left AV valves
30
New cards
Semilunar valves
- One-way valves that separate ventricles from arteries, and prevent blood from flowing backwards into ventricles during ventricle relaxation
- Pulmonary and aortic valve
- Pulmonary and aortic valve
31
New cards
Systole: ventricle ejection
- Blood flows out of ventricle
- Atria relaxed
- Ventricles contract
- AV valves: Closed
- Aortic and pulmonary valves: Open
- Atria relaxed
- Ventricles contract
- AV valves: Closed
- Aortic and pulmonary valves: Open
32
New cards
Diastole: ventricular filling
- Blood flows into ventricles
- Atria relaxed
- Ventricles relaxed
- AV valves: Open
- Aortic and pulmonary valves: Closed
- Atria relaxed
- Ventricles relaxed
- AV valves: Open
- Aortic and pulmonary valves: Closed
33
New cards
Diastole: ventricular filling (atrial contraction)
- Blood flows into ventricles
- Atria contraction
- Ventricles relaxed
- AV valves: Open
- Aortic and pulmonary valves: Closed
- Atria contraction
- Ventricles relaxed
- AV valves: Open
- Aortic and pulmonary valves: Closed
34
New cards
___ supports the valves responsible for one-way flow of blood
Coronary skeleton; the skeleton is composed of dense fibrous connective tissue, which is good for support but also a barrier to conduction of action potentials (necessary for a coordinated contraction)
35
New cards
Lungfish heart
- Has 2 atria
--> 1 receiving oxygenated blood from the lung
--> 1 receiving deoxygenated blood from the body
- Lungs evolved from non-gill structures (swim bladder or similar organ)
- Direct return of blood to heart from lung
--> 1 receiving oxygenated blood from the lung
--> 1 receiving deoxygenated blood from the body
- Lungs evolved from non-gill structures (swim bladder or similar organ)
- Direct return of blood to heart from lung
36
New cards
Systole: isovolumetric ventricular contraction
- Atria relaxed
- Ventricles contract
- AV valves: Closed
- Aortic and pulmonary valves: Closed
- Ventricles contract
- AV valves: Closed
- Aortic and pulmonary valves: Closed
37
New cards
Diastole: isovolumetric ventricular relaxation
- AV valves: Open
- Aortic and pulmonary valves: Closed
- Aortic and pulmonary valves: Closed
38
New cards
***Elaborate on the electrical wiring and ion movements of different parts in the heart***
- Cannot activate sequentially (top to bottom)
--> When you squeeze from the top, your blood will want to go to the bottom of the heart (this is NOT where the exit is)
-----> Would result in a bunch of blood at the tip of the heart (tip=bottom) with nowhere to go
--> Electrical signal must be squeezed from the bottom to get out to the top of the heart (where the exit is)
- Neural wiring
1. SA node starts at the top of the right atrium
2. At the top of the septum, we wait for atria to contract
3. Signal goes from SA --> AV node; here, atria contracts
4. Signal goes to --> Bundle of His (which bifrocates into left and right bundles)
5. Signal goes to --> Tip of the heart
6. Purkinje fibers contract all the ventricles from the bottom up
- Complete flow of blood through the heart
--> Starts with pulmonary circuit
1. Pulmonary veins bring blood to the left atrium
2. Left atrium --> Left ventricle
3. Left ventricle --> Systemic aorta
4. Systemic aorta --> Systemic vein
5. Systemic vein --> Right atrium
6. Right atrium --> Right ventricle
7. Right ventricle --> Send to lungs by pulmonary artery
--> Ends with pulmonary circuit
--> When you squeeze from the top, your blood will want to go to the bottom of the heart (this is NOT where the exit is)
-----> Would result in a bunch of blood at the tip of the heart (tip=bottom) with nowhere to go
--> Electrical signal must be squeezed from the bottom to get out to the top of the heart (where the exit is)
- Neural wiring
1. SA node starts at the top of the right atrium
2. At the top of the septum, we wait for atria to contract
3. Signal goes from SA --> AV node; here, atria contracts
4. Signal goes to --> Bundle of His (which bifrocates into left and right bundles)
5. Signal goes to --> Tip of the heart
6. Purkinje fibers contract all the ventricles from the bottom up
- Complete flow of blood through the heart
--> Starts with pulmonary circuit
1. Pulmonary veins bring blood to the left atrium
2. Left atrium --> Left ventricle
3. Left ventricle --> Systemic aorta
4. Systemic aorta --> Systemic vein
5. Systemic vein --> Right atrium
6. Right atrium --> Right ventricle
7. Right ventricle --> Send to lungs by pulmonary artery
--> Ends with pulmonary circuit
39
New cards
***Relate the electrical activity of the heart to its contraction***
- Myogenic initiation of contraction
--> SA node is pacemaker of heart, initiates depolarization
-----> Autorhythmic and sets resting rate of heart contractions
-----> Unlike other excitable cells, there is no spike in Na+ influx at the beginning of the action potential; the rapid depolarization is from Ca++ entering the cell, followed by delayed efflux of K+
-----> Na+ channels open when membrane potential is 60mV
--------> Na+ influx occurs constantly (channels always open) ==> slow depolarization
-----> K+ diminishes as membrane potential rises
-----> SA node cells depolarize to threshold starting another action potential
--> Fibers connect SA node to Bundle of His
--> Depolarization propagates from Bundle of His along Purkinje fibers in the ventricular muscle mass (note fine network extending throughout ventricles)
- Electrical activation of the heart
1. Signal originates at SA node
--> Pacemaker cells at the SA node initiate depolarization (electrical impulses) to stimulate contraction
-----> Its frequency overrides frequencies of all other autorhythmic muscle cells in the heart, allowing it to set the rate and timing for cardiac muscle contraction (e.g. heart rate)
2. Signal spreads over atria; atria contract
--> Branching network within cardiac muscle, the intercalated discs (specialized gap junctions), allow pulse to spread quickly
--> This transmits depolarization from the SA node and atria to the Bundle of His (which bifurcates into a left and right bundle)
-----> Left is more extensive than right, b/c the left ventricle is more muscular (and those muscles provide more resistance to AP conduction), so more more fibers are needed
3. Signal delays at AV node
--> The AV node delays ventricular contraction slightly while ventricles fill
4. Signal spreads down conducting fibers to bottom of ventricles; ventricles contract
--> Highest amount of electrical activity (in mV)
--> Purkinje fibers spread up through the walls of the ventricle to depolarize them
5. Ventricles relax
--> SA node is pacemaker of heart, initiates depolarization
-----> Autorhythmic and sets resting rate of heart contractions
-----> Unlike other excitable cells, there is no spike in Na+ influx at the beginning of the action potential; the rapid depolarization is from Ca++ entering the cell, followed by delayed efflux of K+
-----> Na+ channels open when membrane potential is 60mV
--------> Na+ influx occurs constantly (channels always open) ==> slow depolarization
-----> K+ diminishes as membrane potential rises
-----> SA node cells depolarize to threshold starting another action potential
--> Fibers connect SA node to Bundle of His
--> Depolarization propagates from Bundle of His along Purkinje fibers in the ventricular muscle mass (note fine network extending throughout ventricles)
- Electrical activation of the heart
1. Signal originates at SA node
--> Pacemaker cells at the SA node initiate depolarization (electrical impulses) to stimulate contraction
-----> Its frequency overrides frequencies of all other autorhythmic muscle cells in the heart, allowing it to set the rate and timing for cardiac muscle contraction (e.g. heart rate)
2. Signal spreads over atria; atria contract
--> Branching network within cardiac muscle, the intercalated discs (specialized gap junctions), allow pulse to spread quickly
--> This transmits depolarization from the SA node and atria to the Bundle of His (which bifurcates into a left and right bundle)
-----> Left is more extensive than right, b/c the left ventricle is more muscular (and those muscles provide more resistance to AP conduction), so more more fibers are needed
3. Signal delays at AV node
--> The AV node delays ventricular contraction slightly while ventricles fill
4. Signal spreads down conducting fibers to bottom of ventricles; ventricles contract
--> Highest amount of electrical activity (in mV)
--> Purkinje fibers spread up through the walls of the ventricle to depolarize them
5. Ventricles relax
40
New cards
***Determine which part of the ECG corresponds to what motion of the heart***
- ECG is a graph of voltage vs time of the electrical activity of the heart (voltage vs. time) measured using electrodes placed on the skin, based on skin conductance
--> Non-invasive
--> These electrodes detect the small electrical changes that are a consequence of cardiac muscle depolarization followed by repolarization during each cardiac cycle (heartbeat)
- Changes in the normal ECG pattern occur in numerous cardiac abnormalities, including
--> Cardiac rhythm disturbances
--> Inadequate coronary artery blood flow
--> Electrolyte disturbances
- The ECG
--> P wave
-----> Atrial excitation; comes from atria contracting
-----> Atrial action potential; atria begins depolarizing (signal from SA node causes atria to contract)
-----> At the end of the P wave, atrial depolarization is complete
-----> After P wave, there is a delay caused by AV node (PR segment)
--> QRS complex
-----> Waiting period and initiation of ventricles
-----> Depolarization of ventricles (ventricle excitation) @Q-R; begins at the same time as the atria repolarization (atrial relaxation), but progresses superiorly and masks it
-----> Ventricular action potential
--------> Ventricular depolarization begins at apex of the heart and progresses superiorly as atria repolarize
-----> Ventricular depolarization is complete by the end of the QRS complex
-----> After S, the ventricles finish contracting (ST segment)
--> T wave
-----> End of ventricle contraction
-----> Ventricular repolarization begins at apex and progresses superiorly as atria repolarizes
-----> Once complete, heart is ready for next cycle
- The ECG reveals electrical regulation of the heart
1. SA node (pacemaker)
--> SA node initiates signal for atrial excitation
2. AV node
--> Here, atrial excitation is complete
--> AV node delays signal
3. Bundle branches; heart apex
4. Purkinje fibers
--> Bundle of His and Perkinje fibers transmit electrical signal and coordinate contraction
--> Non-invasive
--> These electrodes detect the small electrical changes that are a consequence of cardiac muscle depolarization followed by repolarization during each cardiac cycle (heartbeat)
- Changes in the normal ECG pattern occur in numerous cardiac abnormalities, including
--> Cardiac rhythm disturbances
--> Inadequate coronary artery blood flow
--> Electrolyte disturbances
- The ECG
--> P wave
-----> Atrial excitation; comes from atria contracting
-----> Atrial action potential; atria begins depolarizing (signal from SA node causes atria to contract)
-----> At the end of the P wave, atrial depolarization is complete
-----> After P wave, there is a delay caused by AV node (PR segment)
--> QRS complex
-----> Waiting period and initiation of ventricles
-----> Depolarization of ventricles (ventricle excitation) @Q-R; begins at the same time as the atria repolarization (atrial relaxation), but progresses superiorly and masks it
-----> Ventricular action potential
--------> Ventricular depolarization begins at apex of the heart and progresses superiorly as atria repolarize
-----> Ventricular depolarization is complete by the end of the QRS complex
-----> After S, the ventricles finish contracting (ST segment)
--> T wave
-----> End of ventricle contraction
-----> Ventricular repolarization begins at apex and progresses superiorly as atria repolarizes
-----> Once complete, heart is ready for next cycle
- The ECG reveals electrical regulation of the heart
1. SA node (pacemaker)
--> SA node initiates signal for atrial excitation
2. AV node
--> Here, atrial excitation is complete
--> AV node delays signal
3. Bundle branches; heart apex
4. Purkinje fibers
--> Bundle of His and Perkinje fibers transmit electrical signal and coordinate contraction
41
New cards
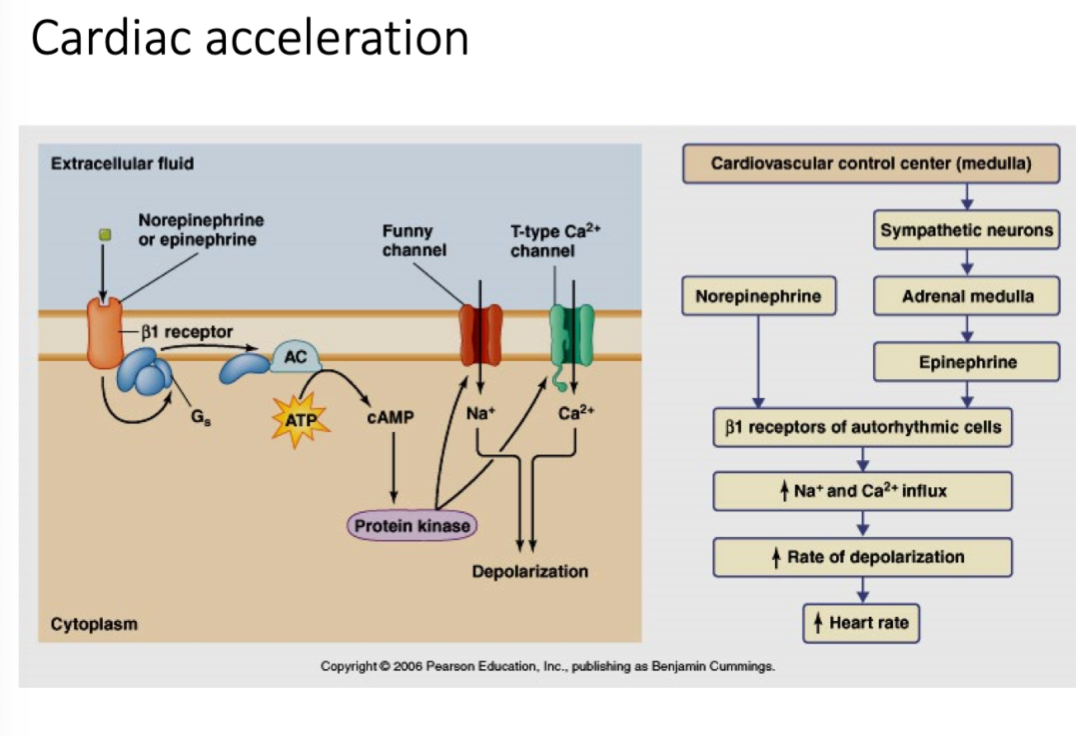
***Compare and contrast the acceleration and deceleration pathways for the heart rate***
- Acceleration
- Acceleration
- Uses sympathetic neurons (caused by sympathetic stimulation)
- Norepinephrine
- Epinephrine
- Beta receptors of autorhythmic cells
- Accelerator nerve decreases length of diastole
--> Opens more Na+ and Ca++ channels
-----> Na+ and Ca++ influx
--------> Increased rate of depolarization (faster)
- Increased heart rate
- Norepinephrine
- Epinephrine
- Beta receptors of autorhythmic cells
- Accelerator nerve decreases length of diastole
--> Opens more Na+ and Ca++ channels
-----> Na+ and Ca++ influx
--------> Increased rate of depolarization (faster)
- Increased heart rate
42
New cards
***Elaborate on blood pressure and blood velocity in different vessels throughout the circulatory system***
- The Cardiac Cycle
--> Blood vessels help regulate blood pressure and velocity
-----> Pressure determines the open/shut status of valves, which determines the volume of blood in the ventricles
--------> At the beginning of systole:
-----------> AV valves shut to prevent backflow of blood from ventricles into atria
-----------> Semilunar valves open shortly afterward to allow deoxygenated blood from RV to enter pulmonary artery
--------> At the beginning of diastole:
-----------> Semilunar valves shut to prevent backflow of blood from aorta into ventricles
-----------> AV valves open shortly afterward to allow oxygenated blood from LA to enter LV
- Heart rate is under autonomic control, adjusting heart rate to maintain sufficient blood pressure and flow to all organs
- Baroreceptors sense changes in blood pressure
--> Baroreceptor reflex
-----> Cardiac output (volume of blood leaving left ventricle) increases
--------> Increase in heart rate and stroke volume (amount of blood ejected from ventricles)
-----> Arterioles in non-critical tissues (skin and intestines) constrict
--------> Diverts blood flow to more critical organs
-----> Veins constrict, decreasing overall volume
--------> Over half the blood in the circulatory system is contained within veins
- The role of muscle: contraction of arterial and venous smooth muscle helps regulate blood pressure and velocity in closed systems
- The pressure of blood flow is highest in: arteries > capillaries > veins
--> Elasticity of artery and arteriole walls is important as it...
-----> Stores energy during systole
-----> Maintains pressure on arterial side of circulation during diastole, thus keeping flow unidirectional
--> Veins have thin walls
-----> Thus, they have low resistance
- The velocity of blood flow is highest in: arteries > veins > capillaries
--> Pressure and velocity of blood drops rapidly in capillary beds, important features preventing rupture of capillaries and fostering exchange as blood transits the bed
--> Velocity decreases in capillaries b/c the total area increases (i.e. the "lake effect")
- Laminar flow and vessel radius
--> Large radius = average velocity of flow is high
-----> Faster flow because there is less friction dragging the blood
--> Small radius = average velocity of flow is low
-----> Why flow is slower in capillaries; the diameter is smaller there
- Arterioles regulate blood flow through capillaries
--> Local vasoconstriction: same volume of blood in smaller cross sectional area will increase speed and blood pressure
-----> Creates small area
-----> Increases blood velocity and pressure
--> Local vasodilation: same volume of blood in larger cross sectional area will decrease speed and blood pressure
-----> Creates larger area
-----> Decreases blood velocity and pressure
--> Blood vessels help regulate blood pressure and velocity
-----> Pressure determines the open/shut status of valves, which determines the volume of blood in the ventricles
--------> At the beginning of systole:
-----------> AV valves shut to prevent backflow of blood from ventricles into atria
-----------> Semilunar valves open shortly afterward to allow deoxygenated blood from RV to enter pulmonary artery
--------> At the beginning of diastole:
-----------> Semilunar valves shut to prevent backflow of blood from aorta into ventricles
-----------> AV valves open shortly afterward to allow oxygenated blood from LA to enter LV
- Heart rate is under autonomic control, adjusting heart rate to maintain sufficient blood pressure and flow to all organs
- Baroreceptors sense changes in blood pressure
--> Baroreceptor reflex
-----> Cardiac output (volume of blood leaving left ventricle) increases
--------> Increase in heart rate and stroke volume (amount of blood ejected from ventricles)
-----> Arterioles in non-critical tissues (skin and intestines) constrict
--------> Diverts blood flow to more critical organs
-----> Veins constrict, decreasing overall volume
--------> Over half the blood in the circulatory system is contained within veins
- The role of muscle: contraction of arterial and venous smooth muscle helps regulate blood pressure and velocity in closed systems
- The pressure of blood flow is highest in: arteries > capillaries > veins
--> Elasticity of artery and arteriole walls is important as it...
-----> Stores energy during systole
-----> Maintains pressure on arterial side of circulation during diastole, thus keeping flow unidirectional
--> Veins have thin walls
-----> Thus, they have low resistance
- The velocity of blood flow is highest in: arteries > veins > capillaries
--> Pressure and velocity of blood drops rapidly in capillary beds, important features preventing rupture of capillaries and fostering exchange as blood transits the bed
--> Velocity decreases in capillaries b/c the total area increases (i.e. the "lake effect")
- Laminar flow and vessel radius
--> Large radius = average velocity of flow is high
-----> Faster flow because there is less friction dragging the blood
--> Small radius = average velocity of flow is low
-----> Why flow is slower in capillaries; the diameter is smaller there
- Arterioles regulate blood flow through capillaries
--> Local vasoconstriction: same volume of blood in smaller cross sectional area will increase speed and blood pressure
-----> Creates small area
-----> Increases blood velocity and pressure
--> Local vasodilation: same volume of blood in larger cross sectional area will decrease speed and blood pressure
-----> Creates larger area
-----> Decreases blood velocity and pressure
43
New cards
What is happening at the heart at step 4
- Signal spread in ventricles
- Signal spreads down conducting fibers to bottom of ventricles resulting in the ventricles contracting
- Signal spreads down conducting fibers to bottom of ventricles resulting in the ventricles contracting
44
New cards
What is happening at the heart at step 3
Signal pause at AV node
45
New cards
Arterial pressure
Pressure in arteries away from the heart
46
New cards
Venous pressure
Pressure in the vena cava
47
New cards
Sympathetic stimulation ___ heart rate
Increases
48
New cards
Parasympathetic stimulation ___ heart rate
Decreases
49
New cards
Arteries posses ___ elastic layers and walls than veins
Thicker; must handle blood coming in through the heart at a high pressure situation, whereas venules have thin walls and low resistance
50
New cards
Veins have ___ while arteries don't
Semi-lunar veins
51
New cards
What brings back the venule blood to the heart
- Skeletal muscles + valves
--> Not the smooth muscles of the blood vessels
--> Movement of skeletal muscles helps to press/squeeze against veins, pushing blood back to heart (muscles contract and blood can only go in 1 direction)
- Negative pressure applied by the heart
- Circulating blood pushing in the back (i.e. pressure applied by circulating blood going to tissues)
--> Not the smooth muscles of the blood vessels
--> Movement of skeletal muscles helps to press/squeeze against veins, pushing blood back to heart (muscles contract and blood can only go in 1 direction)
- Negative pressure applied by the heart
- Circulating blood pushing in the back (i.e. pressure applied by circulating blood going to tissues)
52
New cards
Capillaries are ___ and extremely ___
Small; thin walled
53
New cards
Lake effect
- Drop in velocity as the total area increases
- Velocity of blood flow is inverse to the total cross sectional area of the blood vessels; as the total cross sectional area increases, the velocity of flow decreases
- Blood flow is slowest in the capillaries to allow time for the exchange of gases and nutrients
- Velocity of blood flow is inverse to the total cross sectional area of the blood vessels; as the total cross sectional area increases, the velocity of flow decreases
- Blood flow is slowest in the capillaries to allow time for the exchange of gases and nutrients
54
New cards
Which step in heart contraction results in QRS peak
Ventricular depolarization
55
New cards
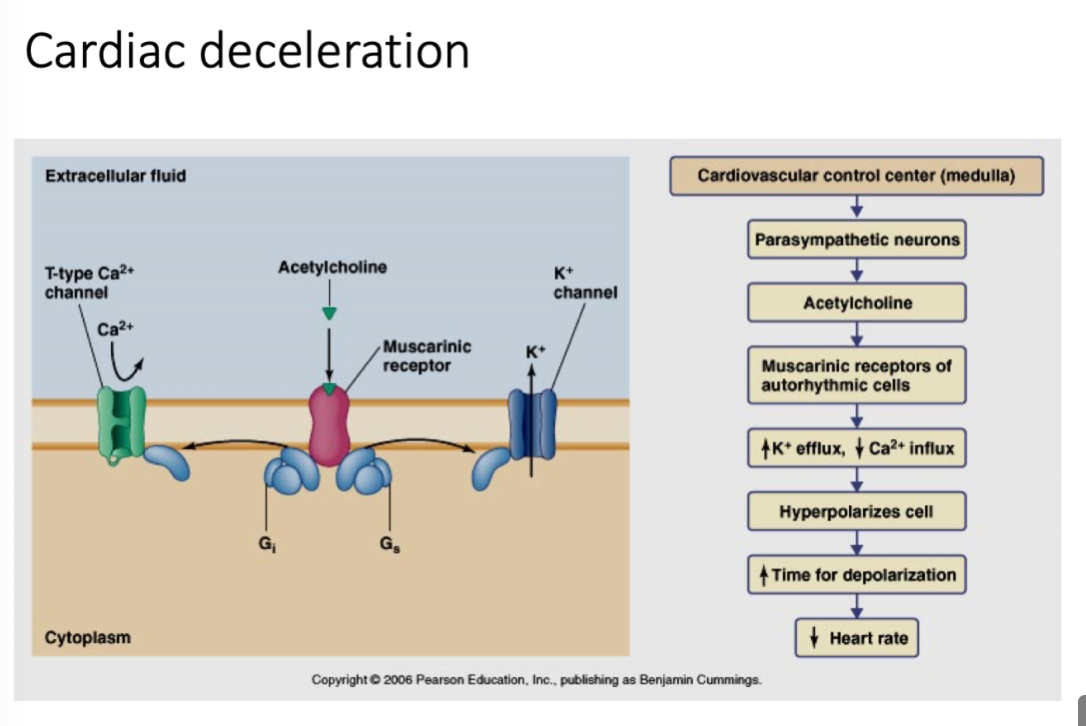
***Compare and contrast the acceleration and deceleration pathways for the heart rate***
- Deceleration
- Deceleration
- Uses parasympathetic neurons (caused by parasympathetic stimulation)
- Acetylcholine
- Muscarinic receptors of autorhythmic cells
- Vagus nerve increases length of diastole
--> Closes more Ca++ channels, opens more K+ channels
-----> Hyperpolarization
--------> Increased time for depolarization (prolonged)
- Decreased heart rate
- Acetylcholine
- Muscarinic receptors of autorhythmic cells
- Vagus nerve increases length of diastole
--> Closes more Ca++ channels, opens more K+ channels
-----> Hyperpolarization
--------> Increased time for depolarization (prolonged)
- Decreased heart rate
56
New cards
***Elaborate on the exchange happening between blood and interstitial fluid through the capillaries***
- Hemodynamics: Regulating patterns of flow
--> Aorta: large and small arteries are high flow/high pressure conduits for blood
--> Control of blood flow into capillaries occurs via pre-capillary sphincters, that are small bands of smooth muscle controlled by the autonomic nervous system
--> The capillaries are small, only a single cell in thickness, and allow for fine regulation of blood flow to specific tissues according to physiological needs
- Controlling blood flow and pressure
--> Flow of blood to specific tissues is controlled by autonomic nervous system via a network of smooth muscles called pre-capillary sphincters
-----> These muscles can constrict or relax, either completely cutting off circulation or flooding specific tissues with blood
-----> Can respond immediately to physiological demands placed on the body
- Arterioles regulate blood flow through capillaries
--> Local vasoconstriction
--> Local vasodilation
- Capillaries are leaky
--> Hydraulic pressure forces bulk flow of fluid outward at the arteriole end of the capillary
--> Large molecules remain, increasing osmotic concentration of blood; coupled with dropping blood pressure in the capillary as it progresses toward the venule results in a net inward flow of fluid
--> About 15% of blood volume exits in the capillary beds
--> Aorta: large and small arteries are high flow/high pressure conduits for blood
--> Control of blood flow into capillaries occurs via pre-capillary sphincters, that are small bands of smooth muscle controlled by the autonomic nervous system
--> The capillaries are small, only a single cell in thickness, and allow for fine regulation of blood flow to specific tissues according to physiological needs
- Controlling blood flow and pressure
--> Flow of blood to specific tissues is controlled by autonomic nervous system via a network of smooth muscles called pre-capillary sphincters
-----> These muscles can constrict or relax, either completely cutting off circulation or flooding specific tissues with blood
-----> Can respond immediately to physiological demands placed on the body
- Arterioles regulate blood flow through capillaries
--> Local vasoconstriction
--> Local vasodilation
- Capillaries are leaky
--> Hydraulic pressure forces bulk flow of fluid outward at the arteriole end of the capillary
--> Large molecules remain, increasing osmotic concentration of blood; coupled with dropping blood pressure in the capillary as it progresses toward the venule results in a net inward flow of fluid
--> About 15% of blood volume exits in the capillary beds
57
New cards
***Differentiate between various types of capillaries and their locations***
- Capillaries contribute to interstitial fluid and lymph
1. Continuous:
- Lowest permeability
- Found in muscle, brain, lungs, connective tissues, exocrine glands
2. Fenestrated:
- Intermediate permeability
- Found in kidneys, intestines, endocrine glands
- Has pores
3. Sinusoidal:
- Very permeable
- Found in liver, bone marrow, spleen, lymph nodes, adrenal cortex
- Has a paracellular gap
- Junctions between endothelial cells determine the permeability of capillary beds
1. Continuous:
- Lowest permeability
- Found in muscle, brain, lungs, connective tissues, exocrine glands
2. Fenestrated:
- Intermediate permeability
- Found in kidneys, intestines, endocrine glands
- Has pores
3. Sinusoidal:
- Very permeable
- Found in liver, bone marrow, spleen, lymph nodes, adrenal cortex
- Has a paracellular gap
- Junctions between endothelial cells determine the permeability of capillary beds
58
New cards
***Appreciate the lymphatic system's role in circulation***
- Excess fluid in interstitial space enters lymphatic duct
--> Lymph ducts ensure extra fluid doesn’t stay in the tissue and is returned back to the circulatory system
- Where does the extra 15% of blood volume go?
--> The fluid (lymph) which accumulates in the interstitial spaces is collected into small ducts (lymphatic vessels)
-----> These drain into larger lymphatic ducts which merge into thoracic duct and drain into vena cava adjacent to the heart
--------> Returning lymph to general circulation
- Lymphatic System
--> Lymphatic circulation includes lymph nodes with high level of lymphocytes, an important part of the immune system
--> Why do your lymph nodes swell during infection??
-----> Pathogens are fighting white blood cells in lymph nodes
--> Lymph carries pathogens to the nodes where they are destroyed or stimulate production of antibodies to fight infection
- Lymphokinetic Motion and Pressure Gradient
--> Blood capillaries --> interstitial fluid --> lymph capillaries --> lymph veins --> lymph ducts --> large circ. veins
- Failure of lymph to return to circulation is not a good thing
--> E.g. Nematode microfilaria worms spread by biting insects causes a very debilitating disease in tropical regions
--> E.g. Elephantiasis: When lymph cannot return to the heart; when extra fluid is not moved out of tissues, painful and debilitating swelling occurs
--> Lymph ducts ensure extra fluid doesn’t stay in the tissue and is returned back to the circulatory system
- Where does the extra 15% of blood volume go?
--> The fluid (lymph) which accumulates in the interstitial spaces is collected into small ducts (lymphatic vessels)
-----> These drain into larger lymphatic ducts which merge into thoracic duct and drain into vena cava adjacent to the heart
--------> Returning lymph to general circulation
- Lymphatic System
--> Lymphatic circulation includes lymph nodes with high level of lymphocytes, an important part of the immune system
--> Why do your lymph nodes swell during infection??
-----> Pathogens are fighting white blood cells in lymph nodes
--> Lymph carries pathogens to the nodes where they are destroyed or stimulate production of antibodies to fight infection
- Lymphokinetic Motion and Pressure Gradient
--> Blood capillaries --> interstitial fluid --> lymph capillaries --> lymph veins --> lymph ducts --> large circ. veins
- Failure of lymph to return to circulation is not a good thing
--> E.g. Nematode microfilaria worms spread by biting insects causes a very debilitating disease in tropical regions
--> E.g. Elephantiasis: When lymph cannot return to the heart; when extra fluid is not moved out of tissues, painful and debilitating swelling occurs
59
New cards
***Synthesize on different ways of blood returning to heart via veins***
- What brings back the venule blood to heart
--> Skeletal muscles + valves
-----> Not the smooth muscles of the blood vessels
-----> Valves make sure blood moves 1 way
-----> Contraction of skeletal muscle is responsible for return flow of blood to the heart from the lower extremities (the heart cannot produce enough pressure to accomplish this feat!)
-----> When you move, you create pressure
--------> Pressure goes through the valves, pushing fluid forward in 1 way
--> Negative pressure applied by the heart
-----> Valves in veins and lymphatic ducts are arranged to only allow fluid flow towards the heart
-----> When surrounding muscles contract, valves allow flow towards heart and prevent backflow towards tissues
--> Circulating blood pushing in the back
--> Skeletal muscles + valves
-----> Not the smooth muscles of the blood vessels
-----> Valves make sure blood moves 1 way
-----> Contraction of skeletal muscle is responsible for return flow of blood to the heart from the lower extremities (the heart cannot produce enough pressure to accomplish this feat!)
-----> When you move, you create pressure
--------> Pressure goes through the valves, pushing fluid forward in 1 way
--> Negative pressure applied by the heart
-----> Valves in veins and lymphatic ducts are arranged to only allow fluid flow towards the heart
-----> When surrounding muscles contract, valves allow flow towards heart and prevent backflow towards tissues
--> Circulating blood pushing in the back
60
New cards
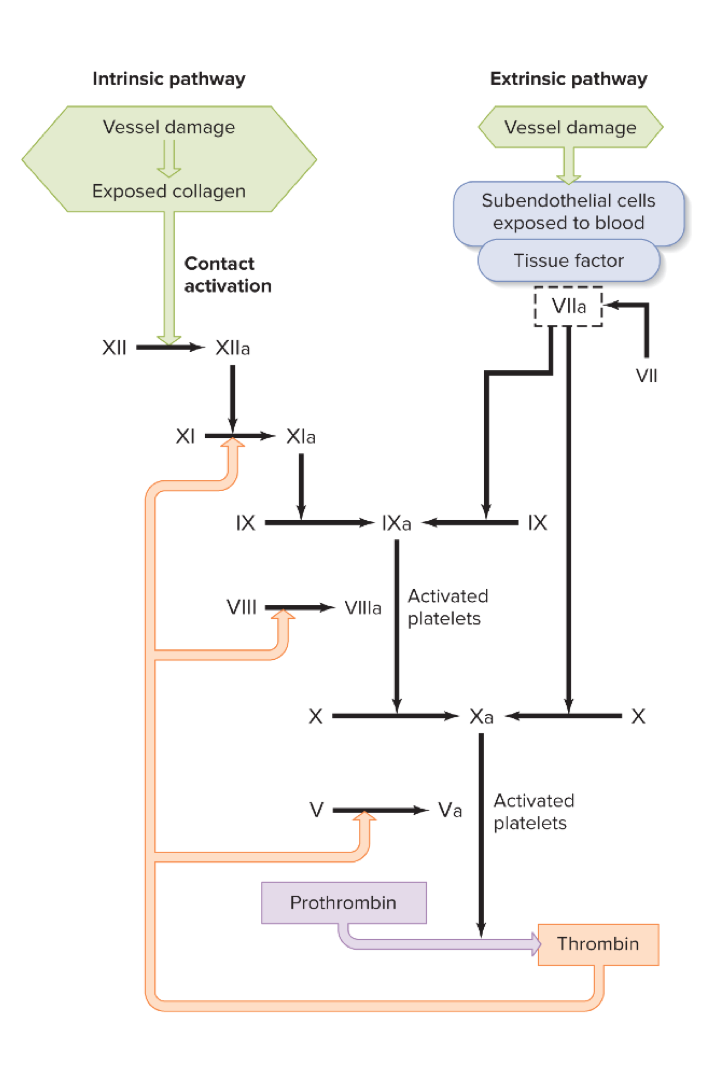
***Elaborate on how clotting occurs only in specific locations and differentiate between extrinsic and intrinsic pathways***
- Platelets
--> Megakaryocytes continuously cleave off fragments called platelets, which circulate
--> Platelets play critical role in blood clotting process (self sealing in case of leaks)
- Clotting
--> Factors released by damaged cells in the vessel wall attract platelets, which forms the initial plug
--> Proteins dissolved in plasma are converted from soluble to insoluble form only in the region of the platelets
--> After the rupture is healed, new and healthy cells release an enzyme that dissolves the fibrin mesh
1) Step 1: Platelet plug
2) Step 2: Fibrin meshwork; permanent stop until wound is healed; then it dissolves
--> Fibrin mesh traps blood cells in it as well
-----> Blood clots are fibrin proteins trapping red blood cells in between fibrin molecules
- Clotting Cont.
--> Clotting is well controlled in our body because the unwanted blood clotting can be deadly
--> We want a system that can form clot quickly when needed but not spontaneously plug up our vessels
--> A cascade system is evolved in blood clotting, which convert soluble fibrinogen to insoluble fibrin only under proper stimulation
- 2 pathways
--> Intrinsic and extrinsic converge on the activation of thrombin from its inactive precursor, prothrombin
- Cascade of plasma enzyme activations (positive feedback loop)
--> Vessel damage
-----> Exposure of blood to subendothelial tissue
--------> Inactive plasma protein
-----------> Enzyme
--------------> Inactive plasma protein
-----------------> Enzyme
--------------------> Prothrombin
-----------------------> Thrombin
--------------------------> Loose fibrin (soluble fibrinogen)
--------------------------> Stabilized fibrin (insoluble fibrin)
--> Megakaryocytes continuously cleave off fragments called platelets, which circulate
--> Platelets play critical role in blood clotting process (self sealing in case of leaks)
- Clotting
--> Factors released by damaged cells in the vessel wall attract platelets, which forms the initial plug
--> Proteins dissolved in plasma are converted from soluble to insoluble form only in the region of the platelets
--> After the rupture is healed, new and healthy cells release an enzyme that dissolves the fibrin mesh
1) Step 1: Platelet plug
2) Step 2: Fibrin meshwork; permanent stop until wound is healed; then it dissolves
--> Fibrin mesh traps blood cells in it as well
-----> Blood clots are fibrin proteins trapping red blood cells in between fibrin molecules
- Clotting Cont.
--> Clotting is well controlled in our body because the unwanted blood clotting can be deadly
--> We want a system that can form clot quickly when needed but not spontaneously plug up our vessels
--> A cascade system is evolved in blood clotting, which convert soluble fibrinogen to insoluble fibrin only under proper stimulation
- 2 pathways
--> Intrinsic and extrinsic converge on the activation of thrombin from its inactive precursor, prothrombin
- Cascade of plasma enzyme activations (positive feedback loop)
--> Vessel damage
-----> Exposure of blood to subendothelial tissue
--------> Inactive plasma protein
-----------> Enzyme
--------------> Inactive plasma protein
-----------------> Enzyme
--------------------> Prothrombin
-----------------------> Thrombin
--------------------------> Loose fibrin (soluble fibrinogen)
--------------------------> Stabilized fibrin (insoluble fibrin)
61
New cards
Aorta
Large and small arteries are high flow/
62
New cards
***Apply the Law of Partial Pressures to predict direction of gas movement in solution***
- In a mixture, each component will exert its own partial pressure
- The partial pressure of a gas in a mixture is largely independent of the other gas components present
- Fick's Law of Diffusion; rate of diffusion
= Use this to grab as much as you can from the environment and expel CO2 out of the environment
= k x A x (P2-P1)/D
--> k = gas diffusion constant
--> A = Area for gas exchange
--> P2-P1 = Difference in partial pressure of gas on either side of diffusion barrier
--> D = Distance (thickness of diffusion barrier)
- All gases will diffuse in the largest amounts when (human lungs check off all these boxes!)
--> Surface area available for exchange is large
--> Diffusion barrier is small (respiratory surface is thin)
--> Partial pressure gradient across surface is large
- Partial Pressure of Oxygen
--> Declines with altitude
--> PpO2 = atmospheric pressure X 0.209
--> External concentration of oxygen declines but composition of air always remains constant
--> As you ascend, there is less pressure but always same composition of air
--> Ratio of oxygen doesn't change, but the amount of air available for you to breathe in decreases as you go higher
- The partial pressure of a gas in a mixture is largely independent of the other gas components present
- Fick's Law of Diffusion; rate of diffusion
= Use this to grab as much as you can from the environment and expel CO2 out of the environment
= k x A x (P2-P1)/D
--> k = gas diffusion constant
--> A = Area for gas exchange
--> P2-P1 = Difference in partial pressure of gas on either side of diffusion barrier
--> D = Distance (thickness of diffusion barrier)
- All gases will diffuse in the largest amounts when (human lungs check off all these boxes!)
--> Surface area available for exchange is large
--> Diffusion barrier is small (respiratory surface is thin)
--> Partial pressure gradient across surface is large
- Partial Pressure of Oxygen
--> Declines with altitude
--> PpO2 = atmospheric pressure X 0.209
--> External concentration of oxygen declines but composition of air always remains constant
--> As you ascend, there is less pressure but always same composition of air
--> Ratio of oxygen doesn't change, but the amount of air available for you to breathe in decreases as you go higher
63
New cards
***Explain the functional adaptations of gas exchange surfaces in animals using Fick's Law (surface area, distance, concentration gradients and perfusion)***
- Fick's Law: (kA(P2-P1))/D
--> k = gas diffusion constant
--> A = area for gas exchange
--> P2-P2 = difference in partial pressure of gas on either side of diffusion barrier
--> D = distance (thickness of diffusion barrier)
- Physical adaptions of gas exchange surfaces
1) Maximizes surface area (increase A)
2) Minimize cross-membrane thickness (decrease D)
3) Ventilate! Keep C1 as large as possible
4) Perfuse! Keep C2 on interior as low as possible
--> Big difference in partial pressure between 2 surfaces = more diffusion coming through
-----> By breathing in and out we keep C1 at a maximum
--> k = gas diffusion constant
--> A = area for gas exchange
--> P2-P2 = difference in partial pressure of gas on either side of diffusion barrier
--> D = distance (thickness of diffusion barrier)
- Physical adaptions of gas exchange surfaces
1) Maximizes surface area (increase A)
2) Minimize cross-membrane thickness (decrease D)
3) Ventilate! Keep C1 as large as possible
4) Perfuse! Keep C2 on interior as low as possible
--> Big difference in partial pressure between 2 surfaces = more diffusion coming through
-----> By breathing in and out we keep C1 at a maximum
64
New cards
***Compare and contrast the structure/function of gills, tracheae, and avian lungs***
- Fish gills
--> Maximizes area and minimizes thickness
--> Large surface area
--> Low resistance to water flow
--> Continuous water flow = ventilation
-----> Constantly moving water around and across their gills
-----> Water pumped continuously across gills with a buccal pump; coupled with a valve flap at rear of mouth, providing 1-way flow of water
--> Blood vessels have countercurrent mechanisms = perfusion
-----> Deoxygenated blood enters gill lamella on downstream edge- flows against flow of water- exits lamella on upstream edge (countercurrent flow)
--------> Maximizes diffusion rate
--> Structure of gills:
-----> Larger surface area then rest of body
-----> Removes 80% of oxygen while lungs remove 25%
-----> Adapted to extract oxygen from an oxygen poor environment
-----> Respiratory surfaces are so tiny that red blood cells flow singularly in close contact (single cell thickness) with O2 in water (very efficient!)
- Tracheal
--> Insect tracheal systems decouples respiration from circulation
-----> Circulatory system doesn't move CO2 and oxygen but are used for moving nutrients (e.g. moving glucose into the cells)
--> Insects: Open circulation with blood (hemolymph) bathing organs
--> Trachea: Tubes that carry air throughout body; where gas diffusion occurs
-----> Though to be the limiting factor in insect size
-----> Contractions of abdominal muscles forces air in and out of tracheal system
-----> Extensive, branching internal tube system in insects
--------> Direct exchange with body cells
-----------> Circulatory system is not involved
-----> Trachea and trachioles are conduits for air movement; diffusion occurs in smaller and thin-walled air capillaries
--> Internal tube system that has direct exchange with body cells and is open to the external environment through narrow tubes to retain moisture
--> Spiracles: Air enters spiracles and goes through the trachea allowing oxygen to diffuse throughout the body
-----> Spiracles can be closed to minimize the loss of water by evaporation
- Avian Lungs
--> Faster metabolic rate than mammals, as they are always flying/being active
--> 1-way flow of air through respiratory system
--> Trachea split into many interconnected parabronchi
--> Gas exchange occurs in a rich air capillary network interconnecting parabronchi
--> Air flows unidirectionally through parabronchi
-----> In human lungs, air can flow through both directions (which is problematic and not as efficient as bird lungs)
--> Trachea bypasses lungs and enters air sacs behind
-----> Air sacs permit 1-way flow: trachea bypasses the lungs almost entirely and enters 2 large air sacs behind the lungs
--> Gas exchange occurs during inhalation and exhalation
-----> Crosscurrent flow
--> Little "dead space" of unused air
-----> When birds breathe in, they utilize all the oxygen that went into your body
--------> Need this because their hearts beat a lot faster and they have a higher metabolism + at higher altitudes, there is less oxygen available to them
--> Avian lung ventilation
1. During inhalation, air flows through the trachea and enters posterior air sacs
2. During exhalation, air leaves posterior air sacs and enters parabronchi in posterior of lungs
3. During next inhalation, air moves into parabronchi in anterior of lung & to anterior air sacs
4. During next exhalation, air moves out of anterior air sacs, through trachea, to atmosphere
--> Maximizes area and minimizes thickness
--> Large surface area
--> Low resistance to water flow
--> Continuous water flow = ventilation
-----> Constantly moving water around and across their gills
-----> Water pumped continuously across gills with a buccal pump; coupled with a valve flap at rear of mouth, providing 1-way flow of water
--> Blood vessels have countercurrent mechanisms = perfusion
-----> Deoxygenated blood enters gill lamella on downstream edge- flows against flow of water- exits lamella on upstream edge (countercurrent flow)
--------> Maximizes diffusion rate
--> Structure of gills:
-----> Larger surface area then rest of body
-----> Removes 80% of oxygen while lungs remove 25%
-----> Adapted to extract oxygen from an oxygen poor environment
-----> Respiratory surfaces are so tiny that red blood cells flow singularly in close contact (single cell thickness) with O2 in water (very efficient!)
- Tracheal
--> Insect tracheal systems decouples respiration from circulation
-----> Circulatory system doesn't move CO2 and oxygen but are used for moving nutrients (e.g. moving glucose into the cells)
--> Insects: Open circulation with blood (hemolymph) bathing organs
--> Trachea: Tubes that carry air throughout body; where gas diffusion occurs
-----> Though to be the limiting factor in insect size
-----> Contractions of abdominal muscles forces air in and out of tracheal system
-----> Extensive, branching internal tube system in insects
--------> Direct exchange with body cells
-----------> Circulatory system is not involved
-----> Trachea and trachioles are conduits for air movement; diffusion occurs in smaller and thin-walled air capillaries
--> Internal tube system that has direct exchange with body cells and is open to the external environment through narrow tubes to retain moisture
--> Spiracles: Air enters spiracles and goes through the trachea allowing oxygen to diffuse throughout the body
-----> Spiracles can be closed to minimize the loss of water by evaporation
- Avian Lungs
--> Faster metabolic rate than mammals, as they are always flying/being active
--> 1-way flow of air through respiratory system
--> Trachea split into many interconnected parabronchi
--> Gas exchange occurs in a rich air capillary network interconnecting parabronchi
--> Air flows unidirectionally through parabronchi
-----> In human lungs, air can flow through both directions (which is problematic and not as efficient as bird lungs)
--> Trachea bypasses lungs and enters air sacs behind
-----> Air sacs permit 1-way flow: trachea bypasses the lungs almost entirely and enters 2 large air sacs behind the lungs
--> Gas exchange occurs during inhalation and exhalation
-----> Crosscurrent flow
--> Little "dead space" of unused air
-----> When birds breathe in, they utilize all the oxygen that went into your body
--------> Need this because their hearts beat a lot faster and they have a higher metabolism + at higher altitudes, there is less oxygen available to them
--> Avian lung ventilation
1. During inhalation, air flows through the trachea and enters posterior air sacs
2. During exhalation, air leaves posterior air sacs and enters parabronchi in posterior of lungs
3. During next inhalation, air moves into parabronchi in anterior of lung & to anterior air sacs
4. During next exhalation, air moves out of anterior air sacs, through trachea, to atmosphere
65
New cards
Which of the following describes a scenario where diffusion rate is highest
- Small surface area
- Thick membrane
- High partial pressure differences on either side of a membrane
- None of the above
- Small surface area
- Thick membrane
- High partial pressure differences on either side of a membrane
- None of the above
High partial pressure differences on either side of a membrane
66
New cards
Which one of the structures is the MAIN contributor for the blood returning to the heart through veins?
- Skeletal muscles
- Negative pressure from heart pumping
- Smooth muscles of the veins
- Circulating blood pushing in the back
- Valves
- Skeletal muscles
- Negative pressure from heart pumping
- Smooth muscles of the veins
- Circulating blood pushing in the back
- Valves
Valves
67
New cards
Functions of the respiratory system
- Defense against inhaled pathogens
- CO2 removal
- Blood oxygenation
- Speech formation
- Blood pH regulation
- Traps and dissolves small blood clots
- Removes or adds chemical messengers to the blood
- Oxygen and carbon dioxide exchange between blood and atmosphere
- CO2 removal
- Blood oxygenation
- Speech formation
- Blood pH regulation
- Traps and dissolves small blood clots
- Removes or adds chemical messengers to the blood
- Oxygen and carbon dioxide exchange between blood and atmosphere
68
New cards
Which of the following is not a part of inspiration?
- The intercostal muscles pull the ribs outward
- The rib cage moves up and out
- The diaphragm contracts and moves down
- Air rushes into the lungs
- The pressure in the lungs increases
- The intercostal muscles pull the ribs outward
- The rib cage moves up and out
- The diaphragm contracts and moves down
- Air rushes into the lungs
- The pressure in the lungs increases
The pressure in the lungs increases
69
New cards
Which of the below contributes highest % for CO2 removal from tissues?
- Bound to hemoglobin (as carboaminohemaglobin)
- Diffuse away from tissues to the atmosphere
- Dissolved in blood as CO2 gas
- Converted to bicarbonate in blood
- Bound to hemoglobin (as carboaminohemaglobin)
- Diffuse away from tissues to the atmosphere
- Dissolved in blood as CO2 gas
- Converted to bicarbonate in blood
Converted to bicarbonate in blood
70
New cards
***Describe respiratory system anatomy, the alveoli structure, and function of surfactants***
- Branches of respiratory system:
--> Trachea
--> Bronchi
--> Bronchioles
--> Terminal bronchioles
--> Respiratory bronchioles
-----> Where CO2/O2 exchange starts
--> Alveolar ducts
--> Alveolar sacs
-----> Majority of exchange happens here
- Alveoli
--> Thin walls to increase diffusion
--> Think back to Fick's Law
-----> Distance and area don't change
-----> Partial pressure of O2 in blood is what changes in physiological situations
--> All to increase efficiency of gas
--> Lots of surfactant in alveolus
--> Almost entirely covered in blood vessels (sac of air covered with blood vessels that do the exchange)
--> Rich capillary network surrounds the alveolus, allowing close contact of blood for gas exchange to occur
--> Elastic and compliant
-----> Expand during inhalation (elastic)
-----> Return to original shape during exhalation (compliant)
- Function of Surfactants (detergent-like molecule)
--> Secreted and lines interior of alveoli
--> Helps prevent collapse by reducing surface tension (to a greater extent in smaller alveoli)
-----> Equalizes pressure in different-sized alveoli, so there is no pressure gradient between smaller and larger ones
--> Without surfactant, air would flow from the smaller to larger
--> With surfactant, air would flow from high partial pressure to low pressure
-----> As a result, smaller alveoli do not collapse into bigger alveoli
-----> Breaks surface tension so that the pressure is equal between the 2 chambers; with no air flow, both get sufficient air
--> Mix of phospholipid and protein
--> Increases lung compliance
-----> Makes it easier for the lung to change size and volume
--> Deep breath = increases secretion by stretching secreting cells
--> Production in fetal lung occurs in late gestation
-----> Stimulated by cortisol
-----> Premature babies have less lung capacity, as they don't have many surfactants
--> Trachea
--> Bronchi
--> Bronchioles
--> Terminal bronchioles
--> Respiratory bronchioles
-----> Where CO2/O2 exchange starts
--> Alveolar ducts
--> Alveolar sacs
-----> Majority of exchange happens here
- Alveoli
--> Thin walls to increase diffusion
--> Think back to Fick's Law
-----> Distance and area don't change
-----> Partial pressure of O2 in blood is what changes in physiological situations
--> All to increase efficiency of gas
--> Lots of surfactant in alveolus
--> Almost entirely covered in blood vessels (sac of air covered with blood vessels that do the exchange)
--> Rich capillary network surrounds the alveolus, allowing close contact of blood for gas exchange to occur
--> Elastic and compliant
-----> Expand during inhalation (elastic)
-----> Return to original shape during exhalation (compliant)
- Function of Surfactants (detergent-like molecule)
--> Secreted and lines interior of alveoli
--> Helps prevent collapse by reducing surface tension (to a greater extent in smaller alveoli)
-----> Equalizes pressure in different-sized alveoli, so there is no pressure gradient between smaller and larger ones
--> Without surfactant, air would flow from the smaller to larger
--> With surfactant, air would flow from high partial pressure to low pressure
-----> As a result, smaller alveoli do not collapse into bigger alveoli
-----> Breaks surface tension so that the pressure is equal between the 2 chambers; with no air flow, both get sufficient air
--> Mix of phospholipid and protein
--> Increases lung compliance
-----> Makes it easier for the lung to change size and volume
--> Deep breath = increases secretion by stretching secreting cells
--> Production in fetal lung occurs in late gestation
-----> Stimulated by cortisol
-----> Premature babies have less lung capacity, as they don't have many surfactants
71
New cards
***Elaborate on pressure changes during an inhalation exhalation cycle and predict issues in the system***
- We exhale, not because of pumping, but because an increase in pressure pushes air out
- Summary: The intrapleural space decreases in pressure, and along with contraction of the diaphragm causes a "negative pressure" that pulls air in. Then, that difference in pressure between intrapleural space and alveoli decreases and the intrapleural space pressure becomes slightly more positive; when this happens in combination with the diaphragm relaxing, air flows out of the lungs
- How does the diaphragm work?
--> As diaphragm is pulled, the lungs fills up
--> Diaphragm creates negative pressure
-----> Increasing volume of the area drops pressure
--> Lungs are going to try to expand and fill up the air
1. Beginning of inspiration: pressure in pleural space is lower, so that later the lung expands as air flows in
- Patm = 0
- Palv = 0
- Pip (intrapleural fluid) = -4
- Still have negative pressure
- Lowest pressure is in the intrapleural cavity, which causes some pulling down and inspiration
2. Mid-inspiration (not pumping air in; flows by pressure): pleural space pressure is even lower, so lung continues to expand
- Patm = 0
- Palv = -1
- Pip = -6
- Elastic recoil force spring is constantly loaded; negative pressure fights against it
- Inspiratory muscles expand the space, making more negative pressure
--> Results in air flowing in
--> The walls of your lungs will try to fight against this ^
- The more negative pressure you make, you make resistance force
- Diaphragm is pulling down and causing pressure to come down even more and the pressure within the intrapleural cavity to decrease even more
- This muscle force, in addition to the pressure change from breathing in, causes the alveolar pressure to decrease slightly
3. End of inspiration/beginning expiration
- Patm = 0
- Palv = 0
- Pip = -7
- Lung capacity stops
- No flow afterward because that pressure difference is now moved into the intrapleural space
- Diaphragm has contracted all the way and the maximum amount of air has entered the lungs (as indicated by the large differences in pressure)
- Although recoil force is starting, the force of the diaphragm pulling down has prevented air from escaping yet
4. Mid-expiration
- Patm = 0
- Palv = 1
- Pip = -5 (less negative)
- Alveolar > atmosphere, so air flows out
--> A positive air pressure compared to the outside with push air out
- As you exhale, your lungs become smaller again
- The force from the diaphragm has stopped as it has relaxed
- The difference in pressures between the intrapleural space and alveoli has decreased, so air flows out
- Issues in the system
--> Breakdown of alveolar walls and overexpansion of alveoli (damaged and enlarged alveoli in emphysema)
-----> Surfactant isn't the issue
-----> Volume is greater
-----> Loss of surface area and density of capillaries
-----> Larger alveoli causes the blood vessels not be able to fully cover the alveoli (i.e. loss of coverage of vessels)
--------> Breathe in more
--------> Difficulty breathing
--------> Lower efficiency of O2 uptake
--> Pneumothorax
-----> Alveoli burst and lung collapse
--------> Via excess pressure or infection
--------> Or breach of thoracic wall (puncture injury)
-----> Intrapleural pressure equals/exceed air pressure within alveoli
-----> Successful reinflating of the lung requires removal of the air filling the intrapleural space via a tube inserted through the chest wall
- Summary: The intrapleural space decreases in pressure, and along with contraction of the diaphragm causes a "negative pressure" that pulls air in. Then, that difference in pressure between intrapleural space and alveoli decreases and the intrapleural space pressure becomes slightly more positive; when this happens in combination with the diaphragm relaxing, air flows out of the lungs
- How does the diaphragm work?
--> As diaphragm is pulled, the lungs fills up
--> Diaphragm creates negative pressure
-----> Increasing volume of the area drops pressure
--> Lungs are going to try to expand and fill up the air
1. Beginning of inspiration: pressure in pleural space is lower, so that later the lung expands as air flows in
- Patm = 0
- Palv = 0
- Pip (intrapleural fluid) = -4
- Still have negative pressure
- Lowest pressure is in the intrapleural cavity, which causes some pulling down and inspiration
2. Mid-inspiration (not pumping air in; flows by pressure): pleural space pressure is even lower, so lung continues to expand
- Patm = 0
- Palv = -1
- Pip = -6
- Elastic recoil force spring is constantly loaded; negative pressure fights against it
- Inspiratory muscles expand the space, making more negative pressure
--> Results in air flowing in
--> The walls of your lungs will try to fight against this ^
- The more negative pressure you make, you make resistance force
- Diaphragm is pulling down and causing pressure to come down even more and the pressure within the intrapleural cavity to decrease even more
- This muscle force, in addition to the pressure change from breathing in, causes the alveolar pressure to decrease slightly
3. End of inspiration/beginning expiration
- Patm = 0
- Palv = 0
- Pip = -7
- Lung capacity stops
- No flow afterward because that pressure difference is now moved into the intrapleural space
- Diaphragm has contracted all the way and the maximum amount of air has entered the lungs (as indicated by the large differences in pressure)
- Although recoil force is starting, the force of the diaphragm pulling down has prevented air from escaping yet
4. Mid-expiration
- Patm = 0
- Palv = 1
- Pip = -5 (less negative)
- Alveolar > atmosphere, so air flows out
--> A positive air pressure compared to the outside with push air out
- As you exhale, your lungs become smaller again
- The force from the diaphragm has stopped as it has relaxed
- The difference in pressures between the intrapleural space and alveoli has decreased, so air flows out
- Issues in the system
--> Breakdown of alveolar walls and overexpansion of alveoli (damaged and enlarged alveoli in emphysema)
-----> Surfactant isn't the issue
-----> Volume is greater
-----> Loss of surface area and density of capillaries
-----> Larger alveoli causes the blood vessels not be able to fully cover the alveoli (i.e. loss of coverage of vessels)
--------> Breathe in more
--------> Difficulty breathing
--------> Lower efficiency of O2 uptake
--> Pneumothorax
-----> Alveoli burst and lung collapse
--------> Via excess pressure or infection
--------> Or breach of thoracic wall (puncture injury)
-----> Intrapleural pressure equals/exceed air pressure within alveoli
-----> Successful reinflating of the lung requires removal of the air filling the intrapleural space via a tube inserted through the chest wall
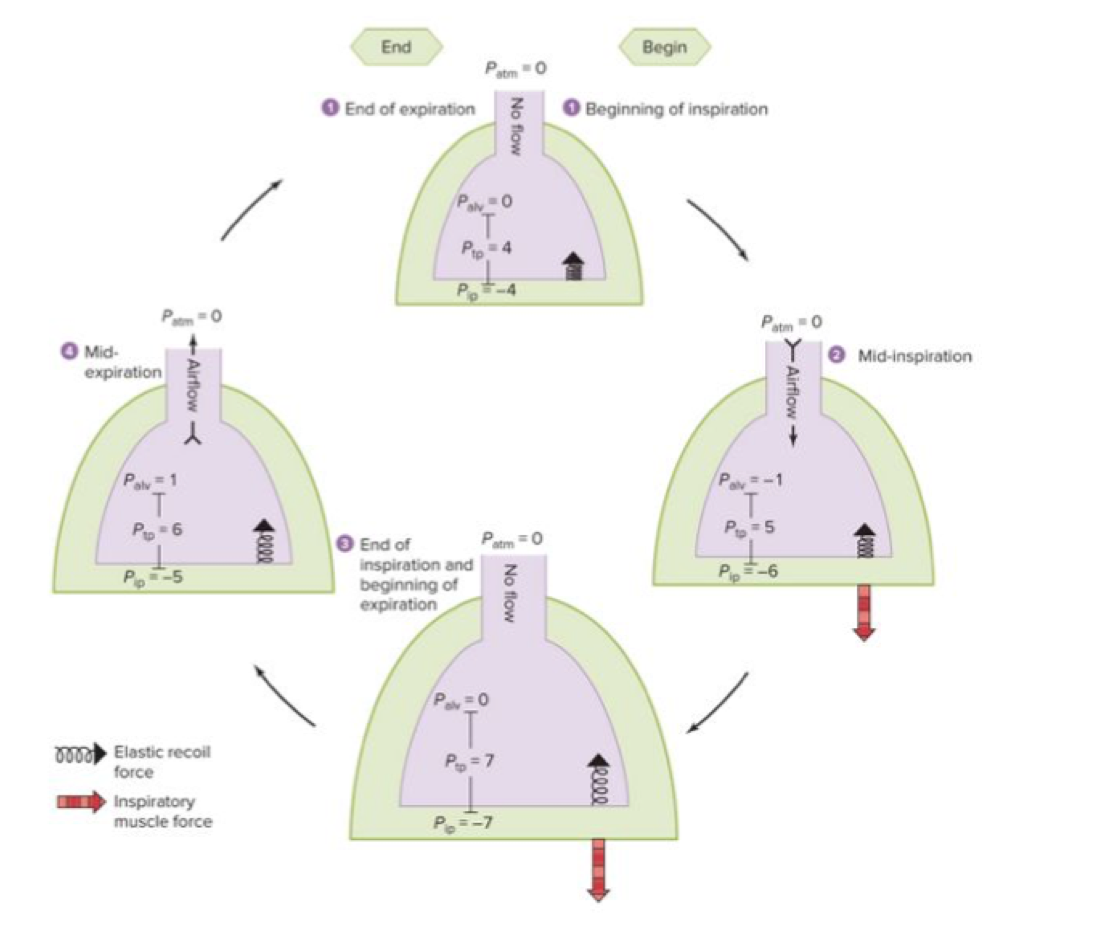
72
New cards
***Define dead space***
- Air left over from preceding breath
--> You don't ever push everything out, so in the anatomical dead space, there's air left over from preceding breath
- No exchange happens in conducting airways
- We have so much air (150mL~) not being used; it's lost to the anatomic dead spaces
--> In our mouth, nose, trachea, etc.
--> You don't ever push everything out, so in the anatomical dead space, there's air left over from preceding breath
- No exchange happens in conducting airways
- We have so much air (150mL~) not being used; it's lost to the anatomic dead spaces
--> In our mouth, nose, trachea, etc.
73
New cards
***Describe the reversible binding of O2 to hemoglobin (dissociation curves)***
- Hemoglobin is the oxygen-carrying molecule in vertebrates
--> Can carry 4 O2 for 1 hemoglobin
- 2 critical features
1. Cooperative binding: promotes oxygen loading and unloading
--> Becomes more likely to bind once one is bound
--> Large amount of O2 are delivered to resting and exercising tissues
2. pH sensitivity (Bohr effect)
--> Increased acidity: increases release of O2 at any PO2
--> An increase in temperature signifies an increase in activity and there's increased oxygen delivery to tissue (a shift to the right of the oxygen-hemoglobin equilibrium curve)
--> Can carry 4 O2 for 1 hemoglobin
- 2 critical features
1. Cooperative binding: promotes oxygen loading and unloading
--> Becomes more likely to bind once one is bound
--> Large amount of O2 are delivered to resting and exercising tissues
2. pH sensitivity (Bohr effect)
--> Increased acidity: increases release of O2 at any PO2
--> An increase in temperature signifies an increase in activity and there's increased oxygen delivery to tissue (a shift to the right of the oxygen-hemoglobin equilibrium curve)
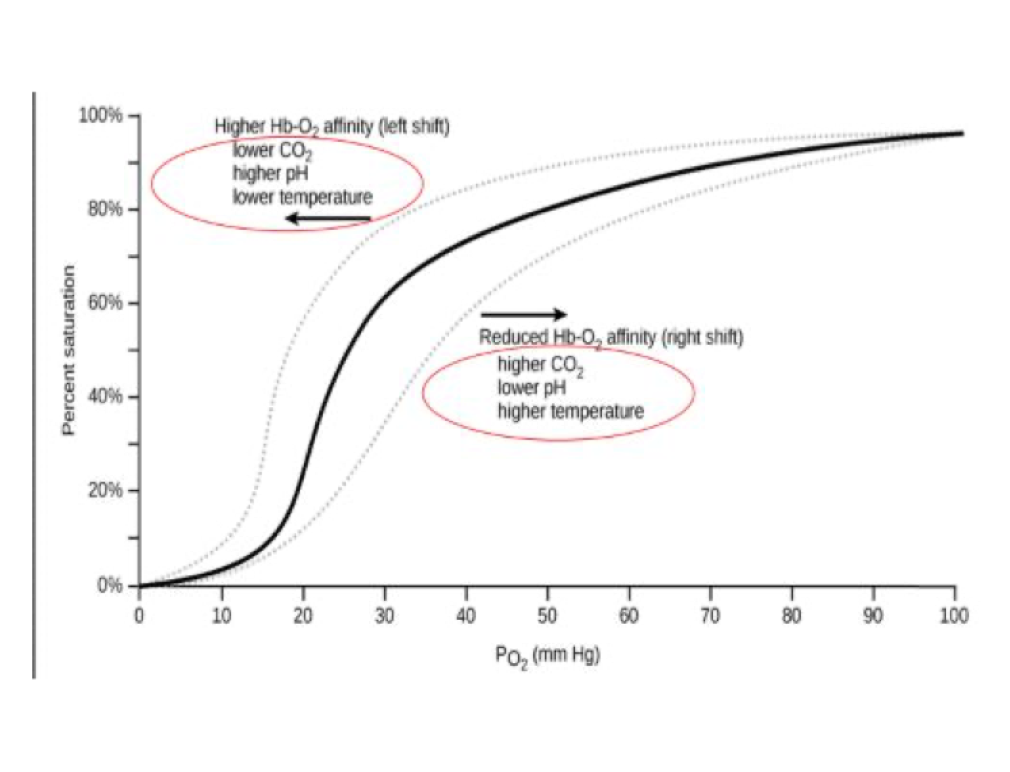
74
New cards
***Predict the effects of pH, temperature, and CO2 concentrations on hemoglobin affinity for O2***
- Factors that lead to an increased Hb-O2 affinity (left shift)
--> No (or decreased) DPG
--> Lower CO2
--> Lower acidity (higher pH)
--> Lower temperature
--> Fetal Hb
- Factors that lead to a reduced Hb-O2 affinity (right shift)
--> Added DPG
--> Higher CO2
--> Higher acidity (lower pH)
--> Higher temperature
--> No (or decreased) DPG
--> Lower CO2
--> Lower acidity (higher pH)
--> Lower temperature
--> Fetal Hb
- Factors that lead to a reduced Hb-O2 affinity (right shift)
--> Added DPG
--> Higher CO2
--> Higher acidity (lower pH)
--> Higher temperature
75
New cards
***Elaborate on how gases are exchanged in alveoli and tissues based on partial pressures and define ventilation-perfusion matching***
- Oxygen exchange happens very quickly, leaving a buffer in the healthy capillaries
--> So when you have diseased lungs that became inflamed and thicker, you aren't as impacted as much
- Ventilation-perfusion matching
1. Supply less blood flow to poorly ventilated areas, thus diverting blood flow to well-ventilated areas
2. Redirect air away from diseased or damaged alveoli and toward healthy alveoli
- Due to disease or blockage
--> Body senses this through pulmonary blood
-----> Blood circulation system responds with vasoconstriction of pulmonary vessels
--> So when you have diseased lungs that became inflamed and thicker, you aren't as impacted as much
- Ventilation-perfusion matching
1. Supply less blood flow to poorly ventilated areas, thus diverting blood flow to well-ventilated areas
2. Redirect air away from diseased or damaged alveoli and toward healthy alveoli
- Due to disease or blockage
--> Body senses this through pulmonary blood
-----> Blood circulation system responds with vasoconstriction of pulmonary vessels
76
New cards
***Differentiate between different methods of how CO2 is transferred in blood***
- Transporting CO2
--> CO2 has HIGHER solubility in blood than O2
--> When CO2 is converted to bicarbonate ion, it serves as a pH buffer and keeps pCO2 low so that CO2 travels from TISSUES to BLOOD cells
-----> Bicarbonate is the primary buffer system in blood and serves to limit pH changes
--> 10% is dissolved in blood in gas form
--> 25-30% is bound to hemoglobin
--> 60-65% is converted to bicarbonate by carbonic anhydrase
--> Haldane effects describes the transport function of blood for CO2 (after blood has flowed through capillaries and is returning to the heart in veins; it is venous return and has a higher content of CO2): Blood carries more CO2 in deoxygenated state than in oxygenated blood
-----> Oxygenated blood has a lower amount of CO2
-----> Deoxygenated blood has a higher amount of CO2
--> CO2 has HIGHER solubility in blood than O2
--> When CO2 is converted to bicarbonate ion, it serves as a pH buffer and keeps pCO2 low so that CO2 travels from TISSUES to BLOOD cells
-----> Bicarbonate is the primary buffer system in blood and serves to limit pH changes
--> 10% is dissolved in blood in gas form
--> 25-30% is bound to hemoglobin
--> 60-65% is converted to bicarbonate by carbonic anhydrase
--> Haldane effects describes the transport function of blood for CO2 (after blood has flowed through capillaries and is returning to the heart in veins; it is venous return and has a higher content of CO2): Blood carries more CO2 in deoxygenated state than in oxygenated blood
-----> Oxygenated blood has a lower amount of CO2
-----> Deoxygenated blood has a higher amount of CO2
77
New cards
***Recognize blood's buffering mechanisms for other ions***
- When CO2 is converted to bicarbonate ion, it serves as a pH buffer and keeps pCO2 low so that CO2 travels from TISSUES to BLOOD cells
- Bicarbonate is the primary buffer system in blood and serves to limit pH changes
- Bicarbonate is the primary buffer system in blood and serves to limit pH changes
78
New cards
***Elaborate on how humans regulate breathing and what is the stimulus during exercise and differentiate between respiratory acidosis and alkalosis***
- Regulating breathing
--> Conscious override of breathing
--> Fundamental breathing rate and depth is controlled by sensory receptors sensitive to CO2
-----> Found in the brainstem and pO2 found in the aortic arch and carotid sinuses
--> Brainstem contains pacemaker neurons similar to those in the heart
-----> This is within the ventral and dorsal respiratory group within the medulla oblongata
--> Central chemoreceptors on ventral surface of medulla are bathed in cerebrospinal fluid, and very sensitive to changes in pCO2
--> You will not have coordinated breathing without pons
--> Pneumotaxic center is receiving all sensory input on pCO2 and pO2- when pCO2 is too high because you're not breathing enough or pO2 is too low because you're not breathing enough but cannot give coordinated commands
--> Peripheral chemoreceptors on aortic arch and carotid sinuses are exposed to blood, and sensitive to pO2, but require large changes in pO2 to stimulate response
--> Conscious override of breathing
--> Fundamental breathing rate and depth is controlled by sensory receptors sensitive to CO2
-----> Found in the brainstem and pO2 found in the aortic arch and carotid sinuses
--> Brainstem contains pacemaker neurons similar to those in the heart
-----> This is within the ventral and dorsal respiratory group within the medulla oblongata
--> Central chemoreceptors on ventral surface of medulla are bathed in cerebrospinal fluid, and very sensitive to changes in pCO2
--> You will not have coordinated breathing without pons
--> Pneumotaxic center is receiving all sensory input on pCO2 and pO2- when pCO2 is too high because you're not breathing enough or pO2 is too low because you're not breathing enough but cannot give coordinated commands
--> Peripheral chemoreceptors on aortic arch and carotid sinuses are exposed to blood, and sensitive to pO2, but require large changes in pO2 to stimulate response
79
New cards
Which one is NOT an essential nutrient?
- Vitamins
- Essential amino acids
- Essential fatty acids
- Minerals
- Essential oils
- Vitamins
- Essential amino acids
- Essential fatty acids
- Minerals
- Essential oils
Essential oils
80
New cards
***Describe the steps of mechanical and chemical digestion***
- 4 stages of food processing
1. Ingestion of nutrients
--> Goes through mechanical digestion to reduce smaller bits of food in order to be swallowed
2. Digestion of large macromolecules into building blocks (monomers)
--> Chemical digestion turns food into smaller molecules which are able to enter the body cells
3. Absorption of monomers from gut into internal environment
4. Elimination of metabolic waste through liver secretions
- Other functions of the digestive system
--> Removal of non-absorbable ingested stuff
--> Metabolic transformation of fuel molecules and detoxification of foreign substances in liver
--> Fighting infectious microorganisms in your gut
- Steps of human digestive system (mechanical + chemical)
1. Mouth
--> Site of mechanical and chemical processing
-----> Tongue manipulates food so that teeth can chew food
-----> Saliva digests carbs
--------> Saliva also contains mucin, a wetting agent that helps make the bolus slide more easily
--------> Chemical digestion of certain food is done by salivary amylase & lipase
--------> Consists of:
-----------> Mucin: protects mouth and lubricates
-----------> Buffers: protects tooth decay
-----------> Antibacterial agents
-----------> Salivary amylase
---------------> Begins the process of digesting starch, breaking off disaccharides
-----------> Salivary lipase
---------------> Begins process of digesting fats (into glycerol and free fatty acids)
--> Swallowing: coordinated movement of the epiglottis and glottis to prevent food from entering windpipe
--> Peristalsis: rhythmic waves of contraction of smooth muscles in the wall of the canals of the digestive tract
2. Esophagus
--> Transports food
3. Stomach
--> Site of mechanical and chemical processing
-----> Digests proteins
--> Large muscular organ with a deeply folded lining
--> Gastric glands are within folds and have 3 major cell types:
-----> Chief cells secrete pepsinogen (activated by low pH to form pepsin, a powerful enzyme)
-----> Mucus cells secrete mucus that lubricates and protects lining of the stomach
-----> Parietal cells secrete hydrochloric acid (HCl), which activates the pepsinogen
4. Small intestine
--> Site of last major stages of digestion and absorption
--> Site of chemical processing and absorption
-----> Digests proteins, fats, carbs
-----> Absorbs nutrients and water
--> 3 regions
1. Duodenum
-----> Acid chyme from stomach enters and mixes with
--------> Bile (aids in absorption of fats)
--------> Intestinal juices and additional digestive enzymes
--------> Pancreatic juice (hydrolytic enzymes and bicarbonate buffer)
2. Jejunum
3. Ileum
--> Small intestine has a large surface area due to the microvilli and villi on the intestinal lumen, which allows greater nutrient absorption
--> In the 1st part of the small intestine
-----> Acid chyme from stomach enters and mixes with:
--------> Bile (aids in absorption/emulsification of fats)
--------> Intestinal juice and additional digestive enzymes
--------> Pancreatic juice (hydrolytic enzymes and bicarbonate buffer)
--> The pancreas produces proteases, protein-digesting enzymes that are activated once they enter the duodenum
5. Large intestine
--> Absorbs water and forms feces
-----> Contains symbiotic bacteria
--> Shorter (than small intestine)
--> Greater diameter
--> Lower in surface area than small intestine
--> Main function is reabsorption (of water and salts)
--> Home to an abundant and diverse community of bacteria which provide an important source of vitamins (biotin, folic acid, nearly all of your vitamin K, and several B vitamins), they exclude competing and potentially pathogenic bacteria
-----> Not the case for stomach or small intestine
--> 4 major regions
-----> Ascending
-----> Transverse
-----> Descending colon
-----> Rectum
6. Appendix
--> Contains immune tissue
--> Harbors symbiotic bacteria
7. Anus
--> Eliminates feces
- Human digestive system accessory organs
--> Salivary glands
-----> Secrete enzymes that digest carbs
-----> Supply lubricating mucus
--> Liver
-----> Secretes molecules that aid in fat digestion
--> Gallbladder
-----> Stores secretions from liver
-----> Empties into small intestine
--> Pancreas
-----> Secretes enzymes and other materials into small intestine
-----> Produces proteases, protein-digesting enzymes that are activated once they enter the duodenum
1. Ingestion of nutrients
--> Goes through mechanical digestion to reduce smaller bits of food in order to be swallowed
2. Digestion of large macromolecules into building blocks (monomers)
--> Chemical digestion turns food into smaller molecules which are able to enter the body cells
3. Absorption of monomers from gut into internal environment
4. Elimination of metabolic waste through liver secretions
- Other functions of the digestive system
--> Removal of non-absorbable ingested stuff
--> Metabolic transformation of fuel molecules and detoxification of foreign substances in liver
--> Fighting infectious microorganisms in your gut
- Steps of human digestive system (mechanical + chemical)
1. Mouth
--> Site of mechanical and chemical processing
-----> Tongue manipulates food so that teeth can chew food
-----> Saliva digests carbs
--------> Saliva also contains mucin, a wetting agent that helps make the bolus slide more easily
--------> Chemical digestion of certain food is done by salivary amylase & lipase
--------> Consists of:
-----------> Mucin: protects mouth and lubricates
-----------> Buffers: protects tooth decay
-----------> Antibacterial agents
-----------> Salivary amylase
---------------> Begins the process of digesting starch, breaking off disaccharides
-----------> Salivary lipase
---------------> Begins process of digesting fats (into glycerol and free fatty acids)
--> Swallowing: coordinated movement of the epiglottis and glottis to prevent food from entering windpipe
--> Peristalsis: rhythmic waves of contraction of smooth muscles in the wall of the canals of the digestive tract
2. Esophagus
--> Transports food
3. Stomach
--> Site of mechanical and chemical processing
-----> Digests proteins
--> Large muscular organ with a deeply folded lining
--> Gastric glands are within folds and have 3 major cell types:
-----> Chief cells secrete pepsinogen (activated by low pH to form pepsin, a powerful enzyme)
-----> Mucus cells secrete mucus that lubricates and protects lining of the stomach
-----> Parietal cells secrete hydrochloric acid (HCl), which activates the pepsinogen
4. Small intestine
--> Site of last major stages of digestion and absorption
--> Site of chemical processing and absorption
-----> Digests proteins, fats, carbs
-----> Absorbs nutrients and water
--> 3 regions
1. Duodenum
-----> Acid chyme from stomach enters and mixes with
--------> Bile (aids in absorption of fats)
--------> Intestinal juices and additional digestive enzymes
--------> Pancreatic juice (hydrolytic enzymes and bicarbonate buffer)
2. Jejunum
3. Ileum
--> Small intestine has a large surface area due to the microvilli and villi on the intestinal lumen, which allows greater nutrient absorption
--> In the 1st part of the small intestine
-----> Acid chyme from stomach enters and mixes with:
--------> Bile (aids in absorption/emulsification of fats)
--------> Intestinal juice and additional digestive enzymes
--------> Pancreatic juice (hydrolytic enzymes and bicarbonate buffer)
--> The pancreas produces proteases, protein-digesting enzymes that are activated once they enter the duodenum
5. Large intestine
--> Absorbs water and forms feces
-----> Contains symbiotic bacteria
--> Shorter (than small intestine)
--> Greater diameter
--> Lower in surface area than small intestine
--> Main function is reabsorption (of water and salts)
--> Home to an abundant and diverse community of bacteria which provide an important source of vitamins (biotin, folic acid, nearly all of your vitamin K, and several B vitamins), they exclude competing and potentially pathogenic bacteria
-----> Not the case for stomach or small intestine
--> 4 major regions
-----> Ascending
-----> Transverse
-----> Descending colon
-----> Rectum
6. Appendix
--> Contains immune tissue
--> Harbors symbiotic bacteria
7. Anus
--> Eliminates feces
- Human digestive system accessory organs
--> Salivary glands
-----> Secrete enzymes that digest carbs
-----> Supply lubricating mucus
--> Liver
-----> Secretes molecules that aid in fat digestion
--> Gallbladder
-----> Stores secretions from liver
-----> Empties into small intestine
--> Pancreas
-----> Secretes enzymes and other materials into small intestine
-----> Produces proteases, protein-digesting enzymes that are activated once they enter the duodenum
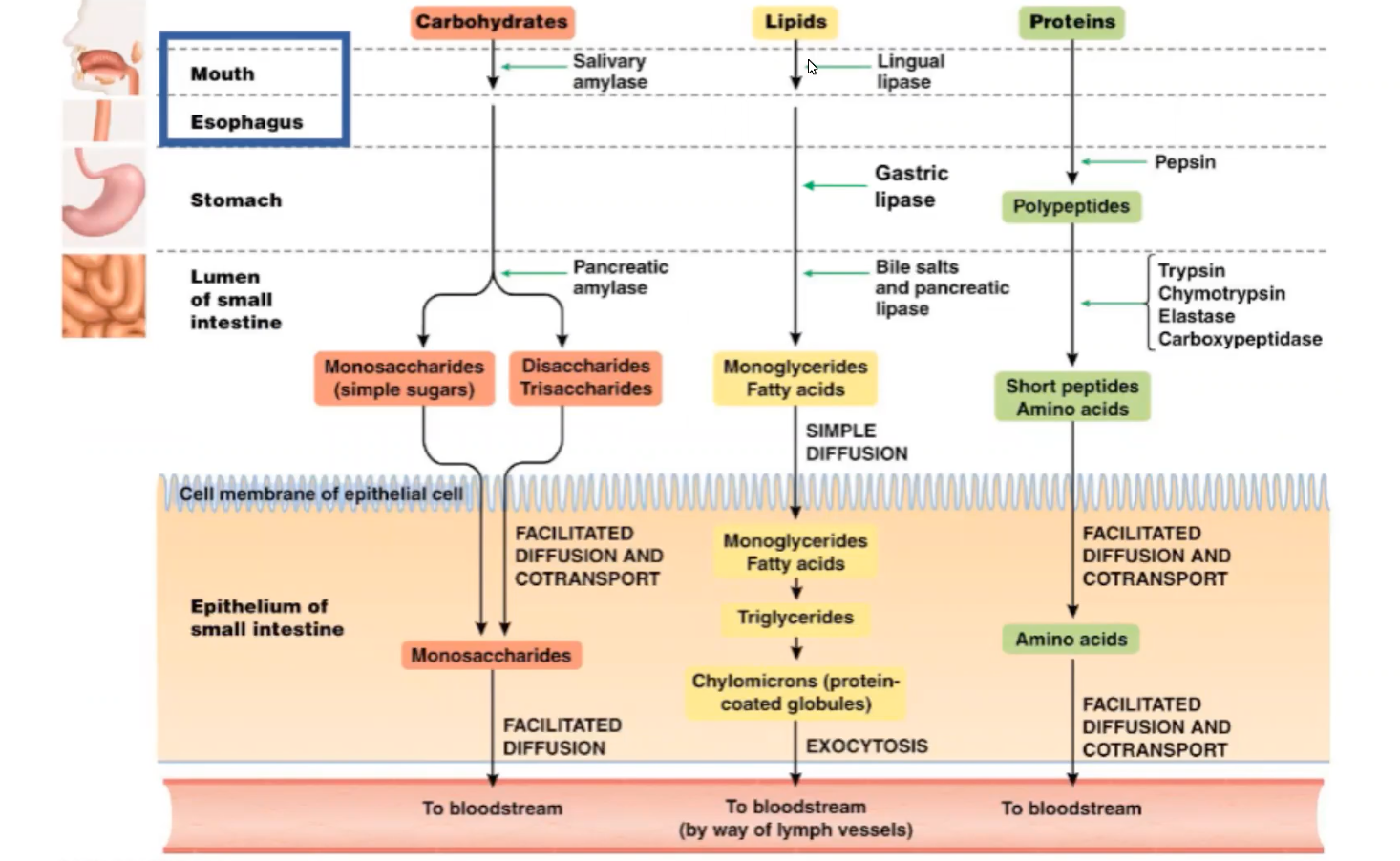
81
New cards
***Describe nutrient absorption in the human digestive system***
- Stomach
--> Absorbs some glucose
- Small intestine
--> Absorbs most glucose
- Large intestine
--> Water, vitamin K, short-chain fatty acids
--> Absorbs some glucose
- Small intestine
--> Absorbs most glucose
- Large intestine
--> Water, vitamin K, short-chain fatty acids
82
New cards
***Elaborate on neural and hormonal regulation of digestion***
- Neural control of digestion
- Hormonal control of digestion
--> Amino acids or fatty acids in the duodenum trigger the release of CHOLECYSTOKININ (CCK), which stimulates the release of digestive enzymes from the pancreas and bile from the gallbladder to stimulate a contraction of smooth muscles to get bile into the small intestine
--> ENTEROGASTRONE secreted by the duodenum inhibits peristalsis and acid secretion by the stomach, thereby slowing digestion when acid chyme rich in fats enters the duodenum
--> GASTRIN from the stomach recirculates via the bloodstream back to the stomach, where it stimulates the production of gastric juices
--> Secreted by the duodenum, SECRETIN stimulates the pancreas to release sodium bicarbonate, which neutralizes acid chyme from the stomach
- Hormonal control of digestion
--> Amino acids or fatty acids in the duodenum trigger the release of CHOLECYSTOKININ (CCK), which stimulates the release of digestive enzymes from the pancreas and bile from the gallbladder to stimulate a contraction of smooth muscles to get bile into the small intestine
--> ENTEROGASTRONE secreted by the duodenum inhibits peristalsis and acid secretion by the stomach, thereby slowing digestion when acid chyme rich in fats enters the duodenum
--> GASTRIN from the stomach recirculates via the bloodstream back to the stomach, where it stimulates the production of gastric juices
--> Secreted by the duodenum, SECRETIN stimulates the pancreas to release sodium bicarbonate, which neutralizes acid chyme from the stomach
83
New cards
Eukaryotic cells obtain ___ and expel ___
O2; CO2
84
New cards
Arteries have ___, but veins do not
Valves
85
New cards
AV valves shut = ventricles ___
Contracting
86
New cards
Semi-lunar valves shut = ventricles ___
Relaxing
87
New cards
Avoiding tetany
- Plateau phase of the cardiac AP helps prevent tetany
--> Caused by Ca++ influx
- Delayed repolarization gives the myocytes time to fully relax
--> Caused by Ca++ influx
- Delayed repolarization gives the myocytes time to fully relax
88
New cards
Frank-Starling Law of the Heart
- Increased end-diastolic volume/venous return = increased systolic stroke volume/work
--> I.e. The more blood that fills the heart during diastole, the more force that is used to pump out blood during systole
- This is analogous to the relationship between skeletal muscle stretch and contraction force
--> More filling of the LV = more stretching of the ventricular muscles = more force applied to push all blood out
--> I.e. The more blood that fills the heart during diastole, the more force that is used to pump out blood during systole
- This is analogous to the relationship between skeletal muscle stretch and contraction force
--> More filling of the LV = more stretching of the ventricular muscles = more force applied to push all blood out
89
New cards
The Fetal Heart
- Lungs are nonfunctional during fetal development as all gas exchange occurs at the placenta
- Fetal heart has 2 bypasses for blood to avoid pulmonary circuit
1. Formane ovale
--> Allows deoxygenated blood to go directly from right to left atrium, avoiding pulmonary circuit
2. Ductus arteriosus
--> Allows deoxygenated blood to go from pulmonary artery to the aorta
- Without a pulmonary circuit, the fetal heart is functionally more or less a 3-chambered heart
- Fetal heart has 2 bypasses for blood to avoid pulmonary circuit
1. Formane ovale
--> Allows deoxygenated blood to go directly from right to left atrium, avoiding pulmonary circuit
2. Ductus arteriosus
--> Allows deoxygenated blood to go from pulmonary artery to the aorta
- Without a pulmonary circuit, the fetal heart is functionally more or less a 3-chambered heart
90
New cards
*** Elaborate on nervous system control of blood flow***
- Pre-capillary sphincters, bands of smooth muscle cells controlled by the autonomic nervous system, adjusts blood flow into capillaries
- Can provide immediate responses to physiological conditions
- Can restrict flow to a particular tissue
- Can provide immediate responses to physiological conditions
- Can restrict flow to a particular tissue
91
New cards
Blood pressure is highest on ___ end and constantly goes ___
- Artery; down
- At the arterial end of a capillary, blood pressure is greater than osmotic pressure, and fluid flows out of the capillary into the interstitial fluid
--> As the fluid flows out and the large molecules remain, the osmotic pressure in capillary increases as it progresses toward the venule
- At the venule end of a capillary, blood pressure is less than osmotic pressure, and fluid flows from the interstitial fluid into the capillary
- At the arterial end of a capillary, blood pressure is greater than osmotic pressure, and fluid flows out of the capillary into the interstitial fluid
--> As the fluid flows out and the large molecules remain, the osmotic pressure in capillary increases as it progresses toward the venule
- At the venule end of a capillary, blood pressure is less than osmotic pressure, and fluid flows from the interstitial fluid into the capillary
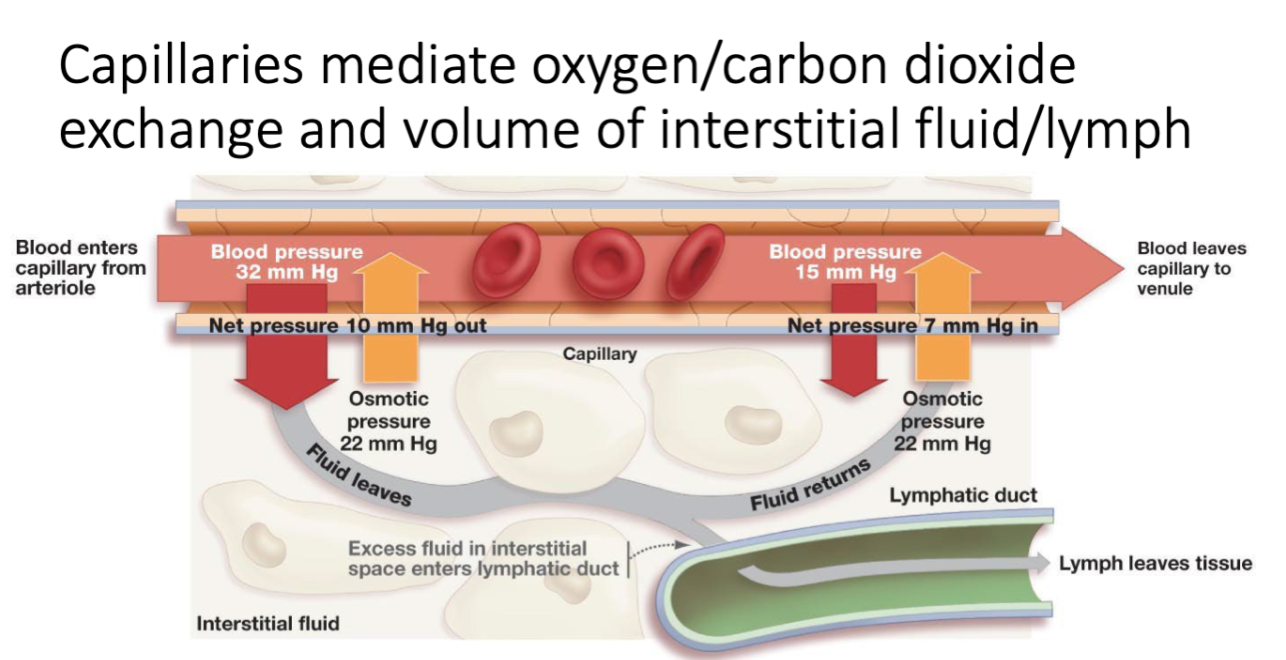
92
New cards
Osmotic pressure is in which direction?
- Osmotic pressure is trying to draw water in, but the high blood pressure is pushing water
- Net movement of water is out
- Outward flow happens the majority of the time, whereas inward flow only happens at the end
- Net movement of water is out
- Outward flow happens the majority of the time, whereas inward flow only happens at the end
93
New cards
Ideal Gas Law
Pv = nRT
- P: pressure
- v: volume (liter)
- n: moles of gas present
- R: ideal gas constant
- T: absolute temperature
- P: pressure
- v: volume (liter)
- n: moles of gas present
- R: ideal gas constant
- T: absolute temperature
94
New cards
O2 has ___ solubility; it's ___ to acquire from air than from water
- Low; easier
- Fish must work hard to diffuse oxygen from water
- Fish must work hard to diffuse oxygen from water
95
New cards
Availability of oxygen declines with ___ temperature; in ___ temperatures, you can dissolve much more gas
Increasing; lower
96
New cards
Metabolic rate/demand for oxygen, for aquatic animals, ___ with temperature; this is a problem since the availability of oxygen ___ with increasing temperature
Increases; declines
97
New cards
Solubility of oxygen ___ with increasing salinity of seawater
Decreases
98
New cards
Demand for oxygen or metabolic rate ___ when active
Increases (i.e. left side of the curve)
99
New cards
At ___ temperatures, there is a limit of how active you can be
Warmer; insufficient oxygen to support demand rate
100
New cards
Fish have higher physiological stress in ___ water
Warm