2) CVA pathology and medical management
1/74
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
75 Terms
what is a stroke
a sudden onset of a focal neurologic deficit resulting from cerebrovascular disease
Stoke is the ________ leading cause of death in the US?
5th
strokes are _____ and _____
preventable and treatable
prevalence of a stroke increases with
age in both men and women
Transient Ischemic Attack (TIA)
minor stroke
full resolution within 24 hours
ischemic stroke
blockage of blood flow (thrombic/embolic)
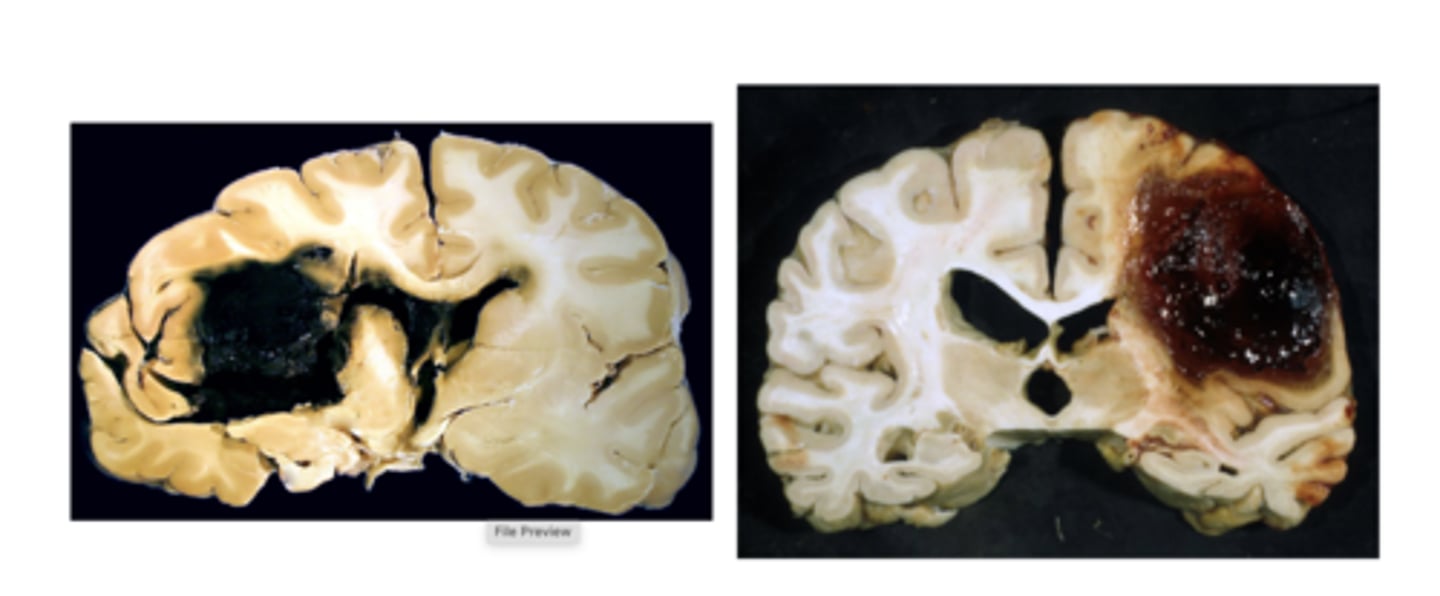
hemorrhagic stroke
intracerebral hemorrhage
Subarachnoid hemorrage
in ischemic strokes, it can be caused by
thrombus or embolus
thrombus
a blood clot attached to the interior wall of an artery or vein
embolus
blood clot that has come loose
a part of a thrombus can come loose
if the embolus gets stuck in the venous side it can cause a
pulmonary embolism
damage from a hemorrhagic stroke can cause
ischemic changes due to pressure on the brain tissue
ischemic CVA mortality
8-12% within the first month
hemorrhagic CVA mortality
37-38% within the first month
stroke risk in the US is nearly twice as high for
non-hispanic black adults than for white adults
mortality risk in the US is highest in
non-Hispanic black adults and pacific islander adults
risk factors for ischemic strokes
hypertension
diabetes
high cholesterol
smoking
heart disease
drug/alcohol use
obesity
risk factors for hemorrhagic strokes
hypertension
increasing age
black ethnicity
low cholesterol with low LDL
loer triglycerides
FAST acronym for stroke
face droop
arm weakness
speech difficulty
time is critical
acute stroke examination (medical)
PMH
meds (anticoagulants)
recent surgeries
vital signs
blood glucose
head CT scan
last known normal
what is the time point that the patient was normal (prior to stroke)
ABC workup for acute stroke
artery, blood, cardiac
when doing a CT scan for a stroke, what are we looking for?
looking for bleeding
signs of stroke - all signs can be seen in 24 hours
hemorrhagic stroke CT scan
there will be a light spot where the bleeding is
ischemic stroke management
thrombolytics
Thrombolytics
Medications that dissolve blood clots
if thrombolytics are used 4.5 hours after symptom onset
there is danger of conversion to hemorrhagic stroke
intra-arterial thrombectomy (IAT)
manual removal of arterial blockage
patient selection is critical for an IAT
less than 6 hours
NIHSS less than 6
ASPECTS less than 6
hemorrhagic stroke presentation
Symptoms are progressive over 48-72 hours
headache
nausea/vomiting
seizure
focal neurologic deficits
herniation syndromes (brain being pushed)
acute ICH (intra-cerebral hemorrhage) management
BP control, reverse coagulopathy, intracranial pressure management, surgical management
surgical management of ischemic CVA
posterior fossa decompression
- performed in the case of a potentially fatal brainstem compression
neurological findings of strokes are going to be impacted by
size of lesion
location of lesion
amount of collateral blood flow
what location of a lesion is better? peripheral or central?
peripheral
unilateral deficits happen due to damage to the
carotid vascular system
bilateral deficits happen due to damage to the
vascular supply to the basilar system
acute stroke symptoms include
weakness
numbness
difficulty with speech
confusion
altered vision - loss of vision
Impaired gait/balance
vertigo
headache
acute stroke symptoms will vary depending on
the location of the pathology
dysarthria
slurred speech, difficulty with articulation
signs of lower motor neuron (LMN) syndrome
flaccid paralysis
muscle atrophy
hyporeflexia
examples of LMN
polio, peripheral
when the UMN is injured, there can be a combination of problems
postive signs - exaggerate normal functions
UMN syndrome postitve signs
Spastic paralysis
hyperreflexia
altered muscle tone
athetosis
dystonia
emergence of primitive reflexes
athetosis
involuntary squirming
dystonia
muscle turning on and stays on
Spastic paraylsis
inability to isolate individual muscle movement
negative signs of UMN syndrome
-fatigue
-dyscoordination
-impaired motor planning and control
ischemic stroke are named for the artery involved
- middle cerebral artery
- anterior cerebral artery
- internal carotid
- posterior cerebral
- vertebral
- basilar
Left middle cerebral artery (MCA) syndrome
R hemiparesis
R sensory loss
aphasia
R visual field cut
left gaze preferance
Right middle cerebral artery (MCA) syndrome
L hemiparesis
L sensory loss
neglect/anosognosia
L visual field cut
right gaze preferance
MCA syndrome is the ________ common location for ischemic stroke
most
what is processed on the lateral side of the left eye, it is processed on the
right side of the brain
what is processed on the medial side of the left eye, it is processed on the
left side of the brain
ACA syndrome (anterior cerebral artery)
contralateral weakness (LE>UE>face)
contralateral sensory loss (LE>UE>face)
abulia (left)
gaze preference
incontinence
central PCA syndrome
visual field cut
thalamic involvement
thalamic involvement in central PCA syndrome
weakness
sensory changes - anesthesia, thalamic pain syndrome
hemiballismus - random movement of limbs
peripheral PCA syndrome
alexia (inability to read) but they can write
amnesia
visual deficits - cortical blindness, visual field cut
basilar artery syndrome
altered mental status
brainstem findings - cranial nerve deficits, weakness, anesthesia
basilar artery syndrome can be catastrophic due to pons damage
tetraplegia
coma
locked-in syndrome
stroke of the cerebullum leads to
nystagmus
dizziness
nausea
ipsilateral ataxia
hemorrhagic strokes are named after their
depth and location
intracranical hemorrhage (ICH)
bleeding from an arterial source into the brain parenchyma
- most fatal of all CVA
subarachnoid hemorrage (SAH)
bleeding into the subarachnoid space between the arachnoid and the pia mater
aneurysms and vascular malformations are
the most common non-traumatic causes of SAH
most common sites for SAH
anterior communicating artery
posterior communicating artery
middle cerebral artery
dangers of SAH
- spewing blood, under high pressure, into brain tissue
- susceptibility to re-rupture
- obstruction of the SA space which can lead to hydrocephalus due to CSF blockage
hemorrhagic CVA syndromes tend to be
less focal than ischemic due to more generalized area of tissue involvement
putaminal hemorrhage
similair to MCA CVA but with greater alteration of consciousness
thalamic hemorrhage
Results in contralateral hemiplegia with disproportionately greater sensory loss
cerebellar hemorrhage
results in ataxia and vestibulopathy
pontine hemorrhage
Offers the poorest prognosis
Tetraplegia and coma
lacunar CVA
characteristics of ischemic and hemorrhagic
symptoms of lacunar CVA
pure motor
pure sensory
ataxic hemiparesis
clumsy hand dysarthria
mixed sensory and motor
three stages of recovery
acute/early
late
chronic
initial improvements
reduction of cerebral edema
absorption of damaged tissues
improved local vascular flow
damaged areas of the brain